Abstract
Background
Coarctation of the aorta (COA) is associated with reduced aortic distensibility and systemic hypertension (HTN). 60–85% of COA patients have a bicuspid aortic valve (BAV). It is not known if the presence of a BAV accentuates the aortopathy and HTN in CoA patients. We examined whether patients with COA and a BAV had lower aortic distensibility by CMR, and a higher prevalence of systemic HTN compared with COA patients with a tricuspid aortic valve (TAV).
Methods
In successfully repaired COA patients excluding those with residual COA, ascending aorta (AAO) and descending aorta (DAO) distensibility was calculated by CMR. HTN was assessed using standard pediatric and adult criteria.
Results
Among 215 COA patients (median age 25.3 years), 67% had a BAV, and 33% had a TAV. Median AAO distensibility z-score was lower in the BAV group (− 1.2 versus − 0.7; p = 0.014) but DAO distensibility was similar in BAV and TAV patients. HTN prevalence was similar in BAV (32%) and TAV groups (36%, p = 0.56). On multivariable analysis controlling for confounders, HTN was not associated with BAV but was associated with male gender (p = 0.003) and older age at follow-up (p = 0.004).
Conclusions
In young adults with treated COA, those with a BAV had stiffer AAO compared to those with a TAV, but DAO stiffness was similar. HTN was not related to BAV. These results suggest that although the presence of a BAV in COA exacerbates the AAO aortopathy, it does not exacerbate the more generalized vascular dysfunction and associated HTN.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Coarctation of the aorta (COA) is a common form of congenital heart disease with an incidence of 1 in 3000–4000 live births [1, 2]. COA is not a simple mechanical narrowing and is associated with reduced aortic distensibility and generalized vascular dysfunction, which leads to a high prevalence of systemic hypertension, left ventricular hypertrophy, ischemic heart disease, and stroke despite successful repair [3,4,5,6,7,8,9,10,11,12]. Reduced aortic distensibility has been associated with higher aorto-carotid wave transmission, which may contribute to cerebral aneurysms and stroke [9]. 60–85% of patients with COA have a bicuspid aortic valve (BAV) [13,14,15,16]. BAV patients also have reduced ascending aortic (AAO) distensibility, independent of COA [17, 18]. Since COA and BAV are both associated with abnormal vascular properties, it is not known if the presence of a BAV accentuates the reduced AAO distensibility seen in COA and if this additional abnormality increases the already high risk of systemic hypertension, compared to COA patients with a BAV. Therefore, we examined whether patients with COA and a BAV had lower aortic distensibility by CMR, and a higher prevalence of systemic hypertension compared with COA patient with a tricuspid aortic valve (TAV).
Methods
A retrospective review of existing clinical data at Boston Children’s Hospital from January 2005 until December 2019 was performed. Demographic, clinical, and surgical data were abstracted from the medical records. The Department of Cardiology’s Scientific Review Committee and the Boston Children’s Hospital’s Committee on Clinical Investigation approved this retrospective review of existing clinical data and waived the requirement for informed consent.
Subjects
Children and adults with COA who had undergone CMR between 2005 and 2019 with available images to measure aortic distensibility were included. Subjects with the following were excluded: unicuspid aortic valve, associated complex congenital heart defects (aside from simple septal defects and patent ductus arteriosus), genetic syndromes, connective tissue disorder, significant recurrent COA (upper to lower extremity systolic blood pressure gradient > 20 mm Hg), severe aortic valve stenosis (by echocardiography, within 1 year of the CMR), severe aortic regurgitation (CMR regurgitation fraction > 40%), and history of surgery involving the aortic root or ascending aorta. Sievers classification was used to describe the types of BAV [19]. For patients who had reintervention on the aortic arch, classification of the type and age at repair was based on the first arch intervention.
CMR imaging
CMR examinations were performed for clinical indication using a commercially available whole-body scanner (Achieva; Philips Healthcare, Best, The Netherlands). When subjects had multiple available examinations, the most recent examination was used for analysis. In young patients who could not cooperate with breathing instructions, the examination was performed under general anesthesia. Brachial artery blood pressure was measured in the right arm before each examination in the supine position using commercial oscillometric blood pressure recorders. Electrocardiogram (ECG)-gated 2-dimensional cine steady-state free precession imaging of the left ventricular outflow tract in 2 orthogonal planes was performed that were then used to plan a stack of cine steady-state free precession (SSFP) images in the short axis of the AAO and the descending aorta (DAO) as previously described. Aortic valve morphology (BAV or TAV) was determined on a stack of cine SSFP images in the short axis of the aortic root.
CMR image analysis
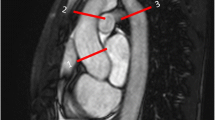
Cine steady-state free precession CMR images were analyzed at 2 locations (AAO and thoracic DAO, Fig. 1) to calculate parameters of stiffness as previously reported [17, 20]. At each location, the cross-sectional area was measured by a single observer using manual planimetry at both peak systole and end-diastole. Images were cross-referenced with 2 long axis planes to select the appropriate short-axis slice perpendicular to the aorta. Aortic stiffness was assessed using the following parameters as previously described [20, 21].
a Planimetry of the AAO and DAO to measure the CSA in both systole and diastole; b Cross-reference synchronized image of the oblique coronal left ventricular outflow tract used to select the slice that crosses the AAO at the widest perpendicular point at the level of the right pulmonary artery; c Cross-reference synchronized image of the oblique sagittal long-axis aortic arch perpendicular point at the level of the right pulmonary artery; d Cross-reference synchronized image of left ventricular outflow tract long-axis. AAO ascending aorta, CSA cross-sectional area, DAO descending
Images were analyzed using commercially available software Cvi42 version 5.10 (Circle Cardiovascular Imaging Inc. Calgary, AB, Canada). For AAO distensibility data, z scores were calculated using previously published normative data reported by Voges et al. [22].
Blood pressure measurements
All available blood pressure recordings following repair were abstracted from the patient’s medical record. Following standard practice at our institution, right arm blood pressure (BP) was recorded while seated using commercial oscillometric blood pressure devices and size-appropriate cuffs. Four-extremity BP was recorded in the supine position. Arm-leg BP difference was calculated as the difference between the systolic (SBP) in the right arm and the leg with the higher SBP. The most recent recording of arm-leg BP difference was used to exclude patients with significant residual coarctation. Patients satisfying standard pediatric (for patients < 18 years of age: systolic and/or diastolic BP ≥ 95th percentile for age, gender and height) or adult (for patients ≥ 18 years of age: systolic BP ≥ 130 and/or diastolic BP ≥ 80 mm Hg) criteria for resting right arm hypertension on 2 separate outpatient visits were labeled as having systemic hypertension [23, 24]. Patients currently on anti-hypertensive medication were classified as having hypertension only if they satisfied standard criteria for hypertension on 2 separate outpatient visits prior to initiation of treatment. Patients who had transient post-procedure hypertension (with or without antihypertensive treatment), that resolved with normal BP recordings on at least two subsequent outpatient visits (without antihypertensive treatment) were not classified as having hypertension. For the purposes of analysis, patients with well-controlled hypertension were treated the same as those with poorly controlled or newly diagnosed hypertension.
Statistical analysis
Wilcoxon rank-sum test was used to compare aortic stiffness parameters between COA patients with BAV and COA patients with TAV. Logistic regression models using hypertension as the outcome and predictor variable BAV were fit with and without the adjustment for AAO and DAO distensibility to examine whether the distensibility measures affected these relationships. Statistical analysis was performed using commercially available software (Stata version 15.0; StataCorpLP, College Station, Texas).
Results
Subjects
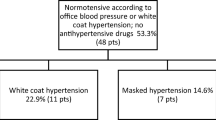
Details of included and excluded subjects are summarized in Fig. 2. Subject characteristics of included patients are summarized in Table 1. The study population consisted of children and young adults, with a median age of 25.3 years at last follow-up (interquartile range (IQR): 18.8, 34.3). As expected, a majority (67%) of patients had a BAV. Subjects with BAV and TAV were similar with respect to most characteristics including gender, age and type of repair, age at follow-up, and medication use. As expected, aortic stenosis and regurgitation were more common in the BAV group and BAV patients had a larger median AAO diameter z-score. 56/215 (26%) subjects had at least one reintervention on their aortic arch (transcatheter or surgical). The majority of subjects in both groups were on antihypertensive medication, with only minor differences in medication use between groups.
Aortic stiffness parameters
CMR derived aortic stiffness parameters at the AAO and DAO are summarized in Table 2 and Fig. 3. BAV patients had a stiffer AAO compared to TAV patients. However, at the DAO, the differences in stiffness between groups were less prominent with similar distensibility values.
Hypertension
The overall prevalence of hypertension was 33% and as seen in Table 2 and Fig. 3, the prevalence of hypertension was similar in BAV and TAV patients. As seen in Table 3, factors associated with hypertension on univariate analysis included male gender, age at follow-up, age at treatment, lower DAO strain, and lower DAO distensibility, but not BAV. On multivariable analysis (Table 4), we explored two separate models, one including AAO distensibility z-score, and the other including DAO distensibility. In both models, no association was found between BAV and hypertension, even after controlling for possible confounders. The only factors independently associated with hypertension included male sex and older age at follow-up.
Discussion
In this CMR study comparing aortic stiffness and hypertension prevalence in successfully repaired COA patients with or without a BAV, we found that although BAV patients have reduced AAO distensibility compared to those with a TAV, DAO distensibility and the prevalence of hypertension are similar in both groups.
Aortic stiffness parameters
Prior studies have demonstrated increased AAO stiffness after successful COA repair [7, 25,26,27,28]. Similarly, patients with a BAV have been shown to have increased AAO stiffness [17, 18]. Because BAV is common in patients with COA, in this study we explored the hypothesis that the presence of BAV exacerbates AAO aortopathy in COA patients. Our results confirm this hypothesis by showing that patients with repaired COA who also have a BAV demonstrate reduced AAO distensibility compared to COA patients with a TAV. Several independent pathogenetic mechanisms for the increased aortic stiffness in COA and BAV have been proposed [26, 28,29,30,31]. It is likely that a coexistence of these pathogenetic mechanism in patients with both COA and BAV is responsible for the higher aortic stiffness seen in this group. In a smaller group of COA patients, Ghorbani et al. also recently reported that BAV was associated with lower AAO distensibility [32].
In contrast to AAO distensibility, DAO distensibility was not significantly different in COA patients with or without a BAV. This is consistent with prior reports showing that abnormalities in aortic stiffness are mostly confined to the AAO in both COA and BAV patients [17, 26]. In COA patients, this may be because the pre-stenotic AAO is subject to higher pressure prior to repair, while the DAO is protected from higher pressure. Similarly, BAV aortopathy and its other effects including dilation are mostly confined to the AAO, and therefore the DAO remains unaffected.
Hypertension
Consistent with prior reports in successfully repaired COA patients, hypertension identified using current pediatric and adult practice guidelines was common (33%) in our study population. Despite the worse AAO distensibility in BAV patients, the prevalence of hypertension was similar in COA patients with or without a BAV. Further, in multivariable models exploring factors associated with hypertension, the presence of a BAV was not significantly associated with hypertension. These findings suggest that although the presence of BAV exacerbates the AAO aortopathy in COA patients, it does not contribute to hypertension. To our knowledge, this is the first study to examine this question. The only factors independently associated with hypertension were male sex and older age. It should however be noted that AAO distensibility in BAV patients deteriorates rapidly with aging, as previously reported by our laboratory [17]. Since our study cohort included mostly children and young adults, it is possible that in older patients with a stiffer AAO, BAV may play a more significant role in the pathogenesis of HTN. This requires further evaluation in future studies including older patients.
Limitations
Several limitations of this work are worth considering. First, our study was limited by the retrospective study design. Second, although we used well established CMR methods for assessing aortic distensibility, it should be noted that peripheral systolic blood pressures may not accurately reflect central aortic pressure. Further, due to the retrospective study design, blood pressure was not measured simultaneous with aortic stiffness measurement.
Conclusions
In young adults with adequately treated COA, those with BAV had a stiffer AAO compared to those with a TAV, but DAO stiffness was similar. In addition, prevalence of hypertension was not related to BAV. These results suggest that although the presence of a BAV in COA exacerbates the AAO aortopathy in a localized fashion, it does not exacerbate the more generalized vascular dysfunction and associated hypertension.
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Grech V. Diagnostic and surgical trends, and epidemiology of coarctation of the aorta in a population-based study. Int J Cardiol. 1999;68:197–202.
Loffredo CA, Chokkalingam A, Sill AM, Boughman JA, Clark EB, Scheel J, Brenner JI. Prevalence of congenital cardiovascular malformations among relatives of infants with hypoplastic left heart, coarctation of the aorta, and d-transposition of the great arteries. Am J Med Genet Part A. 2004;124aa:225–30. https://doi.org/10.1002/ajmg.a.20366.
Rog B, Okolska M, Dziedzic-Oleksy H, Salapa K, Rubis P, Kopec G, Podolec P, Tomkiewicz-Pajak L. Arterial stiffness in adult patients after coarctation of aorta repair and with bicuspid aortic valve. Acta Cardiol. 2018. https://doi.org/10.1080/00015385.2018.1530084.
Tanous D, Benson LN, Horlick EM. Coarctation of the aorta: evaluation and management. Curr Opin Cardiol. 2009;24:509–15. https://doi.org/10.1097/HCO.0b013e328330cc22.
Swan L, Kraidly M, Vonder Muhll I, Collins P, Gatzoulis MA. Surveillance of cardiovascular risk in the normotensive patient with repaired aortic coarctation. Int J Cardiol. 2010;139:283–8. https://doi.org/10.1016/j.ijcard.2008.10.043.
Quennelle S, Powell AJ, Geva T, Prakash A. Persistent aortic arch hypoplasia after coarctation treatment is associated with late systemic hypertension. J Am Heart Assoc. 2015. https://doi.org/10.1161/JAHA.115.001978.
Martins JD, Zachariah J, Selamet Tierney ES, Truong U, Morris SA, Kutty S, de Ferranti SD, Guarino M, Thomas B, Oliveira D, et al. Impact of treatment modality on vascular function in coarctation of the aorta: the LOVE—COARCT Study. J Am Heart Assoc. 2019;8: e011536. https://doi.org/10.1161/JAHA.118.011536.
Cohen M, Fuster V, Steele PM, Driscoll D, McGoon DC. Coarctation of the aorta. Long-term follow-up and prediction of outcome after surgical correction. Circulation. 1989;80:840–5. https://doi.org/10.1161/01.cir.80.4.840.
Kowalski R, Lee MGY, Doyle LW, Cheong JLY, Smolich JJ, d’Udekem Y, Mynard JP, Cheung MMH. Reduced Aortic distensibility is associated with higher aorto-carotid wave transmission and central aortic systolic pressure in young adults after coarctation repair. J Am Heart Assoc. 2019;8: e011411. https://doi.org/10.1161/JAHA.118.011411.
Meijs TA, Minderhoud SCS, Muller SA, de Winter RJ, Mulder BJM, van Melle JP, Hoendermis ES, van Dijk APJ, Zuithoff NPA, Krings GJ, et al. Cardiovascular morbidity and mortality in adult patients with repaired aortic coarctation. J Am Heart Assoc. 2021;10: e023199. https://doi.org/10.1161/JAHA.121.023199.
Pickard SS, Gauvreau K, Gurvitz M, Gagne JJ, Opotowsky AR, Jenkins KJ, Prakash A. Stroke in adults with coarctation of the aorta: a national population-based study. J Am Heart Assoc. 2018. https://doi.org/10.1161/JAHA.118.009072.
Pickard SS, Gauvreau K, Gurvitz M, Gagne JJ, Opotowsky AR, Jenkins KJ, Prakash A. A National population-based study of adults with coronary artery disease and coarctation of the aorta. Am J Cardiol. 2018. https://doi.org/10.1016/j.amjcard.2018.08.051.
Smith DE, Matthews MB. Aortic valvular stenosis with coarctation of the aorta, with special reference to the development of aortic stenosis upon congenital bicuspid valves. Br Heart J. 1955;17:198–206.
Rinnstrom D, Engstrom KG, Johansson B. Subtypes of bicuspid aortic valves in coarctation of the aorta. Heart Vessels. 2014;29:354–63. https://doi.org/10.1007/s00380-013-0370-x.
Teo LL, Cannell T, Babu-Narayan SV, Hughes M, Mohiaddin RH. Prevalence of associated cardiovascular abnormalities in 500 patients with aortic coarctation referred for cardiovascular magnetic resonance imaging to a tertiary center. Pediatr Cardiol. 2011;32:1120–7. https://doi.org/10.1007/s00246-011-9981-0.
Clair M, Fernandes SM, Khairy P, Graham DA, Krieger EV, Opotowsky AR, Singh MN, Colan SD, Meijboom EJ, Landzberg MJ. Aortic valve dysfunction and aortic dilation in adults with coarctation of the aorta. Congenit Heart Dis. 2014;9:235–43. https://doi.org/10.1111/chd.12109.
Perez-Casares A, Dionne A, Gauvreau K, Prakash A. Rapid ascending aorta stiffening in bicuspid aortic valve on serial cardiovascular magnetic resonance evaluation: comparison with connective tissue disorders. J Cardiovasc Magn Reson. 2021;23:11. https://doi.org/10.1186/s12968-021-00716-5.
Boonyasirinant T, Rajiah P, Flamm SD. Abnormal aortic stiffness in patients with bicuspid aortic valve: phenotypic variation determined by magnetic resonance imaging. Int J Cardiovasc Imaging. 2018. https://doi.org/10.1007/s10554-018-1433-y.
Sievers HH, Schmidtke C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg. 2007;133:1226–33. https://doi.org/10.1016/j.jtcvs.2007.01.039.
Prakash A, Adlakha H, Rabideau N, Hass CJ, Morris SA, Geva T, Gauvreau K, Singh MN, Lacro RV. Segmental aortic stiffness in children and young adults with connective tissue disorders: relationships with age, aortic size, rate of dilation, and surgical root replacement. Circulation. 2015;132:595–602. https://doi.org/10.1161/CIRCULATIONAHA.114.014934.
Cavalcante JL, Lima JA, Redheuil A, Al-Mallah MH. Aortic stiffness: current understanding and future directions. J Am Coll Cardiol. 2011;57:1511–22. https://doi.org/10.1016/j.jacc.2010.12.017.
Voges I, Jerosch-Herold M, Hedderich J, Pardun E, Hart C, Gabbert DD, Hansen JH, Petko C, Kramer HH, Rickers C. Normal values of aortic dimensions, distensibility, and pulse wave velocity in children and young adults: a cross-sectional study. J Cardiovasc Magn Reson. 2012;14:77. https://doi.org/10.1186/1532-429X-14-77.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017. https://doi.org/10.1542/peds.2017-1904.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199–269. https://doi.org/10.1016/j.jacc.2017.11.005.
de Divitiis M, Pilla C, Kattenhorn M, Zadinello M, Donald A, Leeson P, Wallace S, Redington A, Deanfield JE. Vascular dysfunction after repair of coarctation of the aorta: impact of early surgery. Circulation. 2001;104:I165-170.
Kuhn A, Baumgartner D, Baumgartner C, Horer J, Schreiber C, Hess J, Vogt M. Impaired elastic properties of the ascending aorta persist within the first 3 years after neonatal coarctation repair. Pediatr Cardiol. 2009;30:46–51. https://doi.org/10.1007/s00246-008-9280-6.
Ou P, Celermajer DS, Jolivet O, Buyens F, Herment A, Sidi D, Bonnet D, Mousseaux E. Increased central aortic stiffness and left ventricular mass in normotensive young subjects after successful coarctation repair. Am Heart J. 2008;155:187–93. https://doi.org/10.1016/j.ahj.2007.09.008.
Vogt M, Kuhn A, Baumgartner D, Baumgartner C, Busch R, Kostolny M, Hess J. Impaired elastic properties of the ascending aorta in newborns before and early after successful coarctation repair: proof of a systemic vascular disease of the prestenotic arteries? Circulation. 2005;111:3269–73. https://doi.org/10.1161/CIRCULATIONAHA.104.529792.
Sievers HH, Sievers HL. Aortopathy in bicuspid aortic valve disease—genes or hemodynamics? or Scylla and Charybdis? Eur J Cardiothorac Surg. 2011;39:803–4. https://doi.org/10.1016/j.ejcts.2011.02.007.
Girdauskas E, Borger MA, Secknus MA, Girdauskas G, Kuntze T. Is aortopathy in bicuspid aortic valve disease a congenital defect or a result of abnormal hemodynamics? A critical reappraisal of a one-sided argument. Eur J Cardiothorac Surg. 2011;39:809–14. https://doi.org/10.1016/j.ejcts.2011.01.001.
Barker AJ, Markl M. The role of hemodynamics in bicuspid aortic valve disease. Eur J Cardiothorac Surg. 2011;39:805–6. https://doi.org/10.1016/j.ejcts.2011.01.006.
Ghorbani N, Muthurangu V, Khushnood A, Goubergrits L, Nordmeyer S, Fernandes JF, Lee CB, Runte K, Roth S, Schubert S, et al. Impact of valve morphology, hypertension and age on aortic wall properties in patients with coarctation: a two-centre cross-sectional study. BMJ Open. 2020;10: e034853. https://doi.org/10.1136/bmjopen-2019-034853.
Funding
Funding provided by Chiang Mai University hospital (Chiang Mai, Thailand).
Author information
Authors and Affiliations
Contributions
KS analyzed the images, collected the CMR and clinical data, and prepared the manuscript. KG helped with study design, performed the statistical analyses, and helped revise the manuscript. AP helped with study design, interpretation of data, manuscript preparation, and overall study supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Department of Cardiology’s Scientific Review Committee and the Boston Children’s Hospital’s Committee on Clinical Investigation approved this retrospective review of existing clinical data and waived the requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saengsin, K., Gauvreau, K. & Prakash, A. Comparison of aortic stiffness and hypertension in repaired coarctation patients with a bicuspid versus a tricuspid aortic valve. J Cardiovasc Magn Reson 25, 31 (2023). https://doi.org/10.1186/s12968-023-00941-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12968-023-00941-0