Abstract
Background
Methamphetamine-associated cardiomyopathy (MA-CMP) is an increasingly recognised aetiology of cardiomyopathy. Cardiovascular magnetic resonance (CMR) is a specialised cardiac imaging modality commonly used in assessment of cardiomyopathy. We aimed to identify specific CMR features associated with MA-CMP.
Methods
A retrospective cohort study of CMR scans was performed in a single centre between January 2015 and December 2020. Thirty patients with MA-CMP who had undergone CMR were identified. MA-CMP was defined as those with a history of significant methamphetamine use hospitalised with acute decompensated heart failure (other causes of cardiomyopathy excluded). A retrospective analysis of index admission CMRs was performed. All studies were performed on a 1.5 T CMR scanner.
Results
The mean age of MA-CMP patients was 43.7 ± 7.5 years, and 86.7% were male. The mean left ventricular (LV) volume obtained in this cohort was consistent with severe LV dilatation (LV end-diastolic volume (334 ± 99 ml); LV end-systolic volume: 269 ± 98 ml), whilst the right ventricular (RV) volume indicated moderate-to-severe dilatation (RV end-diastolic volume: 272 ± 91 ml; RV end-systolic volume: 173 ± 82 ml). Mean LV ejection fraction (20.9 ± 9.2%) indicated severe LV dysfunction, with moderate-to-severe RV dysfunction also detected (RV ejection fraction: 29.4 ± 13.4%). 22 patients (73.3%) had myocardial late gadolinium enhancement (LGE), of which 59.1% were located in the mid-wall, with all of these involving the interventricular septum. 22.7% displayed localised regions of sub-endocardial LGE in a variety of locations, and 18.2% had transmural regions of LGE that were located in the inferior and inferolateral segments. 6 patients (20%) had intracardiac thrombus (4 LV, 2 both LV and RV).
Conclusion
MA-CMP was associated with severe biventricular dilatation and dysfunction, with a high prevalence of intraventricular thrombus. This cohort study highlights that MA-CMP patients have a high prevalence of CMR findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The growth in methamphetamine usage worldwide continues to present increasing societal and healthcare challenges. With the escalation of its usage in a variety of social demographics, methamphetamine-associated cardiomyopathy (MA-CMP) has become an increasingly recognised aetiology of cardiomyopathy, particularly amongst younger patients presenting to emergency departments with heart failure (HF) symptoms and are found to have newly detected ventricular dysfunction [1,2,3,4]. The consequence of this disease process is development of HF with reduced ejection fraction (HFrEF) from severe ventricular dilatation and left ventricular (LV) dysfunction [5]. This clinical entity has substantially increased in its recognition and incidence over the past 15 years with a substantial increase in hospitalisations [6].
Although there has been a number of observational studies of this cohort [4, 5, 7,8,9,10], the complex aetiology of MA-CMP remains unclear, and the cardiovascular magnetic resonance (CMR) findings have yet to be characterised. CMR is a specialised cardiac imaging modality commonly used in assessment of cardiomyopathy with the potential for accurate biventricular volume measurement, calculation of ejection fraction, tissue characterisation and detection of intracardiac thrombus. We aimed to characterise the clinical and CMR features associated with MA-CMP. This is of particular importance as a significant burden of MA-CMP may be reversible with early intervention and complete drug abstinence [11,12,13]
Methods
Study population
A retrospective cohort study was performed of a population of patients with MA-CMP. Patients were identified at the Central Adelaide Local Health Network (CALHN, in Adelaide, South Australia), via a search of the HF database and searching through discharge summaries, utilising electronic medical records from the period between January 2015 and December 2020, to identify all patients with MA-CMP. MA-CMP was defined as those with a history of regular, long-term methamphetamine use, who had required inpatient cardiology admission with acute decompensated HF and had no other identifiable causes of cardiomyopathy. Specifically, coronary artery disease, primary valvular disease (either native or prosthetic valves), active hyperthyroidism, idiopathic, viral, alcohol, chemotherapy or hypertension-related cardiomyopathy were excluded where identified. If there was a history of alcohol or other significant drug use, it was assessed whether methamphetamine was the primary drug of dependence for participant inclusion. Patients were also excluded if they had no available CMR imaging, including those that could not tolerate CMR due to contraindications and/or claustrophobia. All studies were performed on a 1.5 T CMR scanner (Siemens Healthineers, Erlangen, Germany) with Gadovist (Bayer Healthcare, Berlin, Germany), the administered intravenous contrast agent.
Data collection
Clinical and demographic data collected included age at time of index admission/diagnosis, sex, ethnicity, known route of methamphetamine ingestion, duration and/or cessation of methamphetamine use, use of tobacco products, excessive alcohol consumption, and other drug abuse, as well as medical comorbidities (hypertension, diabetes mellitus, hyperlipidaemia, atrial fibrillation/flutter, chronic kidney disease or ischaemic heart disease). Therapies patients were receiving for MA-CMP were also recorded along with patient compliance. CMR parameters collected included: LV end-diastolic volume (LVEDV), LV end-systolic volume (LVESV), LV ejection fraction (LVEF), right ventricular (RV) end-diastolic volume (RVEDV), RV end-systolic volume (RVESV), RV ejection fraction (RVEF, %), presence and location of late gadolinium enhancement (LGE) and presence of intra-cardiac thrombus, according to published standards [14].
Statistical analysis
All continuous variables were presented as mean ± SD as appropriate to distribution. Categorical variables were expressed as number and percentage. Outcomes which did not follow the normal distribution, as assessed via plotting, were expressed as mean and range, with means tested using Mann–Whitney U. For all tests, significance was accepted as a p value < 0.05. All statistical analyses were conducted using SPSS (version 27, Statistical Package for the Social Sciences, International Business Machines, Inc., Armonk, New York, USA). The CALHN Human Research Ethics Committee of the Royal Adelaide Hospital approved the study protocol and waived informed consent.
Results
A total of 4,700 consecutive patients with a history of HF were identified during the study period. After exclusion criteria were applied, 30 patients were included in the cohort. Cohort selection flowchart is shown in Fig. 1.
The year of diagnosis was recorded with an increase in incidence evident across the data collection period, both within the population with CMR imaging performed, and those without, as seen in Fig. 2.
Table 1 outlines the baseline information for this cohort. Most MA-CMP patients were in their fifth decade of life and predominantly male. The average duration of methamphetamine use was 13.4 years, with a comparable portion who were chronic intravenous users (43.3%); whilst others smoked (53.3%), inhaled (6.7%) or had a mixture of consumption methods (13.3%).
Many MA-CMP patients had concurrent heavy tobacco use (80%), and a portion had a previous or current history of excess alcohol use (40%) and/or marijuana use (50%). Comorbidities were present within the cohort, with overall 33.3% possessing a history of hypertension, 10% diabetes mellitus, 10% hyperlipidaemia, 3.3% chronic kidney disease and 3.3% with prior ischaemic heart disease. No patients had a history of cardiac rhythm disorders.
CMR parameters are presented in Table 2. The mean LV volume obtained of the participants included was consistent with severe LV dilatation (LVEDV 334 ± 99 ml; LVESV: 269 ± 98 ml), whilst the mean RV volume indicated moderate-to-severe RV dilatation (RVEDV: 272 ± 91 ml; RVESV: 173 ± 82 ml). LVEF (20.9 ± 9.2%) indicated severe LV dysfunction, with moderate-to-severe RV dysfunction also detected (RVEF: 29.4 ± 13.4%) in all MA-CMP patients.
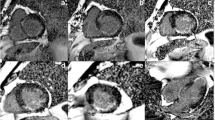
Table 3 demonstrates the findings related to presence and location of LGE on CMR. Twenty-two patients (73.3%) had myocardial LGE, of which 59.1% were located in the mid-wall, with all of these involving the interventricular septum. 22.7% displayed localised regions of sub-endocardial LGE in a variety of locations and 18.2% had transmural regions of LGE that were located in the inferior and inferolateral segments. Several case studies are shown in Fig. 3 to highlight these features.
Presence and location of LGE (3 studies). A Study 1: Mid wall linear LGE (septal); short axis image. B Study 2: Focal transmural LGE at apical inferolateral segment; 4 chamber image. C Study 3: Subendocardial LGE at basal infero-lateral segment; 3 chambers view. D Study 3: Transmural LGE at basal infero-lateral segment; short axis image
Six patients (20%) had intracardiac thrombus. Of these cases, 66.7% were in the LV and 33.3% were biventricular. Figure 4 demonstrates one of the cases in which the burden was limited to the LV. Multiple, irregular large LV thrombi appeared on the horizontal long-axis view at the apex and were circular appearing at the apex on the vertical long-axis view. They had an irregular appearance involving the basal-to-mid anterior segments, with some tracking along the mid anterior segment.
Follow-up data were available on 24 of the 30 patients (80%) included in this cohort using echocardiography. Complete cessation of methamphetamine use and compliance to HF pharmacotherapy was advised to all included participants in this cohort during their index admission. Of the cohort of 11 patients who ceased methamphetamine, all (100%) complied with their medication regime. This compared with only 5 out of the 13 patients taking prescribed medications who continued to use methamphetamine following diagnosis. Over a median follow-up of 6 months (IQR 3.0 to 6.5 months) from index admission, improvement in cardiac function, specifically a LVEF increase of > 5%, was observed in participants who achieved complete cessation of their methamphetamine use compared to those who reduced or remained consistent in their consumption (p-value = 0.003). The presence of baseline LGE on CMR, however, did not show a significant impact on change in follow up LVEF. Additionally, whilst there were variable cessation rates in both patients with and without LGE, a two-way ANOVA test indicates that only cessation is statistically significant (p-value = 0.009), independent of LGE. These figures are presented in Tables 4, 5 and 6.
Given the potential of alcohol abuse being a confounder and contributor to cardiomyopathy in this population, the relationship of alcohol abuse on ventricular volumes, LVEF and RVEF (at baseline), as well as recovery in ventricular function was measured. Whilst there was a small trend to increased volumes in those with a history of alcohol abuse (Table 7), this was not significant. In addition, Fig. 5 highlights that a history of prior alcohol use did not affect rates of improvement in ventricular function with methamphetamine cessation, as patients who ceased methamphetamine use did not also cease alcohol use.
Follow up LVEF data for 24 MA-CMP patients comparing the effect of methamphetamine cessation (circles) with continual use (diamonds), with participants with a history of alcohol abuse further visualised in red in both groups. Mean data ± 2 standard deviations for both groups are also plotted for further comparison
Discussion
CMR has evolved as an essential investigative tool in evaluation of cardiomyopathy due to its accurate quantification of biventricular volumes and ejection fraction as well as tissue characterisation [15]. In addition, detection of specific patterns of LGE and assessment of its burden does assist in assessment of risk for arrhythmias and prognosis in non-ischaemic cardiomyopathy. In this retrospective study of an important HF group, we identified a number of adverse prognostic markers on CMR in patients with MA-CMP.
LV dilation and contractile impairment is a significant predictor of adverse outcomes in dilated cardiomyopathy [16]. In addition, RV dilatation and left atrial dilatation also confer significant prognostic value in cardiomyopathy [17, 18]. Our retrospective study has demonstrated a substantial degree of LV and RV dilatation as measured on CMR. A follow-up CMR study assessing the effects of medical therapy and prognosis relating to degree of ventricular dilatation would provide further insights into prognosis of MA-CMP.
The mechanisms of ventricular dilatation specifically in MA-CMP warrant discussion. MA-CMP development is postulated to be a secondary to an interplay of direct and indirect mechanistic pathways. Directly, amphetamines promote free radical production resulting in direct cellular injury, apoptosis via increased p53 activity, mitochondrial dysfunction, altered gene expression and defective intracellular haemostasis. Contractile dysfunction develops from disrupted electrical–mechanical coupling [19]. In susceptible individuals, long-term use results low-grade inflammation and consequent myocyte loss with replacement fibrosis. Indirectly, amphetamine does potentiate heightened sympathetic nervous system activity, which can also induce coronary and microvascular spasm, resulting in acute ischaemia [20,21,22]. These mechanisms consequently may result in the development of significantly dilated cardiac chambers, systolic dysfunction, and clinical presentation of the heart failure syndrome [5, 23, 24].
LGE is an effective, well-validated and reproducible method of detecting myocardial fibrosis and other pathologies such as infarction, infiltration and inflammation. An abundance of CMR clinical studies have demonstrated correlation with adverse events (including sudden cardiac death in non-ischaemic cardiomyopathy [25,26,27]. The incidence of LGE in our population of MA-CMP was quite high (76.3%), and the pattern of LGE identified in our cohort was heterogenous. This implies varied pathological processes that may occur with MA-CMP including chronic stress precipitating mid-wall fibrosis, micro-embolic phenomena and possibly areas of low-grade chronic inflammation. The majority of patients (56.5%) had evidence of mid-wall LGE, indicating that chronic inflammation and resultant mid-wall fibrosis is likely to be the predominant mechanism for developing of cardiomyopathy. However, 21.7% of the patients included had evidence of sub-endocardial LGE and 21.7% had transmural LGE, both of which can typically be indicative of prior myocardial infarction. In the population included, all patients had obstructive coronary artery disease excluded at coronary angiography which supports the hypothesis of these patients having possible coronary arterial spasm or myocardial infarction with non-obstructive coronary arteries (MINOCA) as the aetiology. The presence and burden of LGE detected on CMR in the non-ischaemic population has been demonstrated to be a powerful imaging biomarker in predicting adverse outcomes and response to medical therapy [28]. In addition, a previous study of 30 patients undergoing endomyocardial biopsy in MA-CMP has reported the presence of fibrosis on biopsy representing an adverse relationship with recovery of ventricular function [5]. Therefore, in the population of MA-CMP where individual clinical factors may render some patients challenging for device implantation, the further prognostic information from LGE assessment may assist in important clinical decision making with regard to implanted cardiodefibrillator (ICD) placement and may also assist with pharmacotherapy selection as well as discussions with patients regarding long-term prognosis.
The incidence of ventricular thrombi was also a highly relevant clinical finding in the population studied. Intra-cardiac thrombi carry significant clinical risk with embolization and its detection has a profound impact in management by mandating therapeutic anticoagulation [29]. Intra-cardiac thrombi have been observed in other studies assessing the MA-CMP population [5]. Our study revealed a 20% incidence of ventricular thrombus with MA-CMP, observed in mixed patterns of LGE. Given the potential clinical catastrophic consequences, this finding necessitates an adequately thorough exclusion for ventricular thrombus with patients with MA-CMP that undergo cardiac imaging.
CMR sequences that were not available in our cohort but would be of value in a future study include native T1 mapping, post contrast T1 mapping and patterns in tissue tracking measuring LV, RV and left atrial strain. Data from these sequences would provide further mechanistic and prognostic insights into the entity of MA-CMP, specifically around the incidence of diffuse fibrosis, long-axis LV function and left atrial function.
Dedicated left atrial volume acquisition may also have provided additional data in this patient population given the prognostic value of atrial dilatation in cardiomyopathy.
Study limitations
Limitations of our study include the obligatory weaknesses associated with a retrospective observational design performed via reviewing medical records which may have resulted in a degree of selection bias. In addition, there was a lack of a control group of non-ischaemic cardiomyopathy which was chosen not to be included due to the heterogeneity of various aetiologies of non-ischaemic cardiomyopathy. Genetic testing for familial dilated cardiomyopathy was also not available in our cohort, however, there was no identified familial cardiomyopathy included in the studied population. Data was gathered from a single healthcare network and may not be as applicable to other populations. However, this limitation is offset by the advantages of this single tertiary centre including uniformity in clinical practice, data acquisition and consistency in CMR study interpretation.
A significant cohort of the population included also had a history of alcohol abuse (~ 40%). However, patients included were assessed on review of the medical records as to what was their predominant drug of abuse and dependence. Patients only with predominant MA abuse were included in our study, but alcohol certainly may have been a contributor to development of a cardiomyopathy in those with a history of alcohol abuse which does represent a potential confounder to the findings reported. Importantly, there was no statistically significant difference in the baseline ventricular volumes in those with previous alcohol abuse, compared to those who did not.
The population selected for this cohort had a significant and long-history of methamphetamine abuse. However, the intensity of methamphetamine use is difficult to quantify in this patient population, particularly when clinical data is retrieved retrospectively from reviewing electronic medical records. Therefore, the study does represent a reasonably heterogenous population of methamphetamine users, with variable methods and levels of consumption.
Conclusions
To our knowledge, this is the largest series of MA-CMP that has been characterised with CMR. This study demonstrated that MA-CMP is associated with significant biventricular dilatation and systolic dysfunction, a high incidence of LGE and a 20% incidence of intra-cardiac thrombus, which was sometimes biventricular. The MA-CMP population possessed heterogenous patterns of LGE detected, most frequently observed in the mid-wall and interventricular septum. Follow-up data of this cohort revealed that abstinence from methamphetamine use following diagnosis of MA-CMP was associated with a greater improvement in LVEF. Future studies with larger cohorts, as well as outpatient cohorts, are required to corroborate these findings and to investigate their follow-up imaging for further recovery of cardiac function.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CMR:
-
Cardiovascular magnetic resonance
- HF:
-
Heart failure
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle/left ventricular
- LVEDV:
-
Left ventricular end-diastolic volume
- LVEDVI:
-
Left ventricular end-diastolic volume index
- LVEF:
-
Left ventricular ejection fraction
- LVESV:
-
Left ventricular end-systolic volume
- LVESVI:
-
Left ventricular end-systolic volume index
- MA-CMP:
-
Methamphetamine-associated cardiomyopathy
- RV:
-
Right ventricle/right ventricular
- RVEDV:
-
Right ventricular end-diastolic volume
- RVEDVI:
-
Right ventricular end-diastolic volume index
- RVEF:
-
Right ventricular ejection fraction
- RVESV:
-
Right ventricular end-systolic volume
- RVESVI:
-
Right ventricular end-systolic volume index
References
Thomas IC, Nishimura M, Ma J, Dickson SD, Alshawabkeh L, Adler E, et al. Clinical characteristics and outcomes of patients with heart failure and methamphetamine abuse. J Card Fail. 2020;26(3):202–9.
Reddy PKV, Ng TMH, Oh EE, Moady G, Elkayam U. Clinical characteristics and management of methamphetamine-associated cardiomyopathy: state-of-the-art review. J Am Heart Assoc. 2020;9(11): e016704.
Zhao SX, Kwong C, Swaminathan A, Gohil A, Crawford MH. Clinical characteristics and outcome of methamphetamine-associated pulmonary arterial hypertension and dilated cardiomyopathy. JACC Heart Fail. 2018;6(3):209–18.
Yeo KK, Wijetunga M, Ito H, Efird JT, Tay K, Seto TB, et al. The association of methamphetamine use and cardiomyopathy in young patients. Am J Med. 2007;120(2):165–71.
Schürer S, Klingel K, Sandri M, Majunke N, Besler C, Kandolf R, et al. Clinical characteristics, histopathological features, and clinical outcome of methamphetamine-associated cardiomyopathy. JACC Heart Failure. 2017;5(6):435–45.
Dickson SD, Thomas IC, Bhatia HS, Nishimura M, Mahmud E, Tu XM, et al. Methamphetamine-associated heart failure hospitalizations across the United States: geographic and social disparities. J Am Heart Assoc. 2021;10(16): e018370.
Ito H, Yeo KK, Wijetunga M, Seto TB, Tay K, Schatz IJ. A comparison of echocardiographic findings in young adults with cardiomyopathy: with and without a history of methamphetamine abuse. Clin Cardiol. 2009;32(6):E18–22.
Richards JR, Harms BN, Kelly A, Turnipseed SD. Methamphetamine use and heart failure: prevalence, risk factors, and predictors. Am J Emerg Med. 2018;36(8):1423–8.
Wang TKM, Kueh SA, Sutton T, Gabriel R, Lund M, Looi JL. Poor outcomes in methamphetamine-associated cardiomyopathy-a growing health issue in New Zealand. N Z Med J. 2019;132(1502):55–66.
Wijetunga M, Seto T, Lindsay J, Schatz I. Crystal methamphetamine-associated cardiomyopathy: tip of the iceberg? J Toxicol Clin Toxicol. 2003;41(7):981–6.
Lopez JE, Yeo K, Caputo G, Buonocore M, Schaefer S. Recovery of methamphetamine associated cardiomyopathy predicted by late gadolinium enhanced cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2009;11(1):46.
Pujol-López M, Ortega-Paz L, Flores-Umanzor Eduardo J, Perea Rosario J, Bosch X. Magnetic resonance as an alternative to endomyocardial biopsy to predict recoverability of left ventricular function in methamphetamine-associated cardiomyopathy. JACC Heart Failure. 2017;5(11):853–4.
Islam MN, Kuroki H, Hongcheng B, Ogura Y, Kawaguchi N, Onishi S, et al. Cardiac lesions and their reversibility after long term administration of methamphetamine. Forensic Sci Int. 1995;75(1):29–43.
Petersen SE, Aung N, Sanghvi MM, Zemrak F, Fung K, Paiva JM, et al. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J Cardiovasc Magn Reson. 2017;19(1):18.
Parsai C, O’Hanlon R, Prasad SK, Mohiaddin RH. Diagnostic and prognostic value of cardiovascular magnetic resonance in non-ischaemic cardiomyopathies. J Cardiovasc Magn Reson. 2012;14(1):54.
Japp AG, Gulati A, Cook SA, Cowie MR, Prasad SK. The diagnosis and evaluation of dilated cardiomyopathy. J Am Coll Cardiol. 2016;67(25):2996–3010.
Bourantas CV, Loh HP, Bragadeesh T, Rigby AS, Lukaschuk EI, Garg S, et al. Relationship between right ventricular volumes measured by cardiac magnetic resonance imaging and prognosis in patients with chronic heart failure. Eur J Heart Fail. 2011;13(1):52–60.
Gulati A, Ismail TF, Jabbour A, Ismail NA, Morarji K, Ali A, et al. Clinical utility and prognostic value of left atrial volume assessment by cardiovascular magnetic resonance in non-ischaemic dilated cardiomyopathy. Eur J Heart Fail. 2013;15(6):660–70.
Giv MJ. Exposure to amphetamines leads to development of amphetamine type stimulants associated cardiomyopathy (ATSAC). Cardiovasc Toxicol. 2017;17(1):13–24.
Kevil CG, Goeders NE, Woolard MD, Bhuiyan MS, Dominic P, Kolluru GK, et al. Methamphetamine use and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2019;39(9):1739–46.
Chen JP. Methamphetamine-associated acute myocardial infarction and cardiogenic shock with normal coronary arteries: refractory global coronary microvascular spasm. J Invasive Cardiol. 2007;19(4):E89–92.
He SY, Matoba R, Fujitani N, Sodesaki K, Onishi S. Cardiac muscle lesions associated with chronic administration of methamphetamine in rats. Am J Forensic Med Pathol. 1996;17(2):155–62.
Lord KC, Shenouda SK, McIlwain E, Charalampidis D, Lucchesi PA, Varner KJ. Oxidative stress contributes to methamphetamine-induced left ventricular dysfunction. Cardiovasc Res. 2010;87(1):111–8.
Karch SB. The unique histology of methamphetamine cardiomyopathy: a case report. Forensic Sci Int. 2011;212(1–3):e1–4.
Perazzolo Marra M, De Lazzari M, Zorzi A, Migliore F, Zilio F, Calore C, et al. Impact of the presence and amount of myocardial fibrosis by cardiac magnetic resonance on arrhythmic outcome and sudden cardiac death in nonischemic dilated cardiomyopathy. Heart Rhythm. 2014;11(5):856–63.
Iles L, Pfluger H, Lefkovits L, Butler MJ, Kistler PM, Kaye DM, et al. Myocardial fibrosis predicts appropriate device therapy in patients with implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. J Am Coll Cardiol. 2011;57(7):821–8.
Kuruvilla S, Adenaw N, Katwal AB, Lipinski MJ, Kramer CM, Salerno M. Late gadolinium enhancement on cardiac magnetic resonance predicts adverse cardiovascular outcomes in nonischemic cardiomyopathy: a systematic review and meta-analysis. Circ Cardiovasc Imaging. 2014;7(2):250–8.
Leong DP, Chakrabarty A, Shipp N, Molaee P, Madsen PL, Joerg L, et al. Effects of myocardial fibrosis and ventricular dyssynchrony on response to therapy in new-presentation idiopathic dilated cardiomyopathy: insights from cardiovascular magnetic resonance and echocardiography. Eur Heart J. 2012;33(5):640–8.
Cruz Rodriguez JB, Okajima K, Greenberg BH. Management of left ventricular thrombus: a narrative review. Ann Transl Med. 2021;9(6):520.
Acknowledgements
The authors gratefully acknowledge contributions from Tim Pearson for querying the databases at Royal Adelaide Hospital.
Funding
No financial assistance or funding was provided for this research article.
Author information
Authors and Affiliations
Contributions
MBS designed the research concept, interpreted the data, was a major contributor in writing the manuscript and acted as corresponding author. FT collected and analysed the patient data and was a major contributor in writing the manuscript. DS planned the analytical approach and helped to evaluate and edit the manuscript. KT, PS and DMK helped to evaluate the manuscript. KTW assisted in data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
CALHN Human Research Ethics Committee (CALHN HREC). CALHN Reference Number: 14152. The CALHN HREC determined that the waiver request meets the requirements of section 2.3.10 of the NHMRC National Statement. Waiver of consent has been granted for access to all electronic and hard medical records for the above project. The project is authorised by CALHN Research Services for conduct at the Royal Adelaide Hospital and The Queen Elizabeth Hospital. The CALHN HREC is constituted in accordance with the NHMRC National Statement on the Ethical Conduct of Human Research (2007).
Consent for publication
The images displayed within the manuscript are entirely unidentifiable with no details on any individuals reported. Therefore, no consent for images published has been obtained for this manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Stokes, M.B., Thoi, F., Scherer, D.J. et al. Cardiovascular magnetic resonance imaging characteristics in patients with methamphetamine-associated cardiomyopathy. J Cardiovasc Magn Reson 24, 67 (2022). https://doi.org/10.1186/s12968-022-00898-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12968-022-00898-6