Abstract
Cathepsin C (CTSC) is a lysosomal cysteine protease constitutively expressed at high levels in the lung, kidney, liver, and spleen. It plays a key role in the activation of serine proteases in cytotoxic T cells, natural killer cells (granzymes A and B), mast cells (chymase and tryptase) and neutrophils (cathepsin G, neutrophil elastase, proteinase 3) underscoring its pivotal significance in immune and inflammatory defenses. Here, we comprehensively review the structural attributes, synthesis, and function of CTSC, with a focus on its variants implicated in the etiopathology of several syndromes associated with neutrophil serine proteases, including Papillon–Lefevre syndrome (PLS), Haim–Munk Syndrome (HMS), and aggressive periodontitis (AP). These syndromes are characterized by palmoplantar hyperkeratosis, and early-onset periodontitis (severe gum disease) resulting in premature tooth loss. Due to the critical role played by CTSC in these and several other conditions it is being explored as a potential therapeutic target for autoimmune and inflammatory disorders. The review also discusses in depth the gene variants of CTSC, and in particular their postulated association with chronic obstructive pulmonary disease (COPD), COVID-19, various cancers, anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis, sudden cardiac death (SCD), atherosclerotic vascular disease, and neuroinflammatory disease. Finally, the therapeutic potential of CTSC across a range of human diseases is discussed.
Similar content being viewed by others
Introduction
Cathepsin C (syn. CatC, CTSC), also known as dipeptidyl peptidase I (DPPI), is a lysosomal cysteine protease belonging to the papain-like cysteine peptidases family. As a critical component of the immune system, CTSC plays a dominant role in immune defenses, antimicrobial activity, inflammation, and programmed cell death (apoptosis) [1]. CTSC activates key pro-inflammatory serine proteases, such as neutrophil elastase, cathepsin G, proteinase 3, neutrophil serine protease 4, mast cell chymase, tryptase, and granzymes A and B, highlighting its essential role in maintaining health [2,3,4,5,6,7]. Dysregulation of CTSC is linked to various inflammatory diseases, including chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, and COVID-19-related acute respiratory distress syndrome (ARDS), making it a potential therapeutic target due to its role in exacerbating inflammation and tissue damage [8, 9]. Additionally, variants in the CTSC gene (OMIM*602365) are also associated with genetic disorders characterized by severe periodontal disease, including Papillon–Lefevre syndrome (PLS, MIM#245000), Haim–Munk syndrome (HMS, MIM#245010), and aggressive periodontitis (AP, MIM#170650) [10]. However, not all cases of aggressive periodontitis are linked with a variation in CTSC.
Despite the multifaceted role of CTSC family in human health and disease there are no contemporary reviews on this subject. Hence, the focus of this review is to explore in detail the molecular biology maturation and substrate specificity of CTSC and its activities, the role of CTSC in immune defense mechanisms and in activating diverse serine proteases. This is followed by an account of CTSC associated syndromes such as HMS, PLS, and AP wherein a strong element of oro-facial diseases is found. The final section deals with its possible translational value and the clinical utility in therapeutics.
Cathepsin family and activities
Protease, also known as peptidase, is an enzyme that hydrolyzes peptide bonds [11]. Peptidase can be classified by a cleavage location into an endopeptidase that cleaves internal peptide bonds and an exopeptidase (aminopeptidases and carboxypeptidases) that cleaves the amino- or carboxyl-terminal bonds in the polypeptide chain. The peptidase can also be classified by its principal catalytic residues in active sites such as cysteine, serine, threonine, aspartic, glutamic, metallo, and mixed [11, 12] though some categories contain families with two or more catalytic types [7, 12, 13].
The all-encompassing term “Cathepsins” denotes many intracellular proteases that belong to various catalytic classes. For example, CTSD and CTSE are aspartic proteases; CTSG and CTSA are serine proteases, and CTSC, B, L, S, H, K, O, X(Z), V, F, and W are cysteine proteases which mostly are endopeptidase while a few such as CTSX and CTSC are exopeptidases [14].
Papain-like cysteine proteases in mammals have a molecular weight of approximately 20–35 kDA which are small enzymes, though CTSC is an exception to this rule. It has a molecular weight around 200 kDa [15,16,17]. Cysteine cathepsins normally consist of a single peptide, a propeptide, and a catalytic unit with the latter representing the mature proteolytically active form [7].
Cathepsins are initially produced as inactive proenzymes with a signal peptide by ribosomes associated with the cellular endoplasmic reticulum (ER). This signal peptide directs the zymogen to be recruited into the ER-Golgi pathway. Subsequently, the signal peptide is cleaved out [13]. Following the initial steps, cathepsins undergo maturation processes and post-translational glycosylations [18]. The pre-part of the molecules is required for intracellular trafficking to the lysosomal region, which is accomplished by mannose-6-phosphate receptors. The proenzymes of cathepsins undergo conversion into their active forms within late endosomes and lysosomes, facilitated by autocatalysis under acidic pH conditions [13]. On the other hand, other enzymes can activate CTSC by cleavage. However, the autocatalytic activation does not occur from CTSC and CTSX because due to their strict exopeptidase activity [19, 20]. In the case of CTSC, its activation relies on the activity of other endopeptidases, such as CTSL and CTSS (Fig. 1) [21].
Schematic illustration of lysosomal cathepsin maturation. Cathepsins are initially synthesized as inactive preproenzymes with a N-terminal signal peptide, guiding them through the rough endoplasmic reticulum (RER). The signal peptide is cleaved in the ER lumen, after which they are directed via the mannose-6-phosphate (Man-6-P) receptor pathway to the lysosome through the trans-Golgi network. Procathesins dissociate from the Man-6-P receptor within late endosomes. Finally, Cathepsins undergo auto-catalysis or cleavage by other proteases to attain their mature form
Cathepsin activities are regulated by cell-type-specific mechanisms, exogenous factors, endogenous inhibitors such as cystatin (A, B, C, D, F), and other proteins including serpins, kininogens, and alpha2-macroglobulin. The maturation and post translational processing of cathepsins is influenced by other enzymes, pH in the endosomal/lysosomal compartment, and environmental pH [18]. Cathepsins degrade various proteases or polypeptides and are involved in lysosomal bulk protein degradation. For example, CTSK and CTSV are potent elastase and CTSK has special specificity in collagen degradation. CTSC cleaves various neutrophil serine proteases including neutrophil elastase [18]. In addition, cathepsins are associated with many disorders such as atherosclerosis, cardiomyopathy, adiposity, osteoporosis, rheumatoid arthritis, metastasis, fibrosis, emphysema, asthma, and neuropathic pain [7].
Cathepsin C gene (CTSC)
The CTSC gene, in mammals, is predominantly expressed in the lungs, spleen, kidneys, liver, placenta, inflammatory tissues as well as in neutrophils, mast cells, monocytes, macrophages, along with their precursors [7, 22, 23]. CTSC is a highly conserved lysosomal cysteine dipeptidyl aminopeptidase required for the activation of pro-inflammatory neutrophil serine proteases (NSPs) including neutrophil elastase (NE), CTSG, proteinase 3 (PR3), neutrophil serine protease 4 (NSP4) and also mast cell chymase, tryptase, and granzymes A and B [2,3,4,5,6,7].
The structure of CTSC and its maturation process
CTSC is originally synthesized as a 55-kDa monomeric single-chain pro-enzyme, separated into four regions including an exclusion domain (Asp1-Gly119), a propeptide (Thr120-His206), a heavy chain (Leu207-Arg370), and a light chain (Asp371-Leu439) [19] (Fig. 2A). The maturation process of CTSC comprises a series of structural transformations of these four regions.
The structure of Pro-CTSC and the Process, maturation, and crystal structure of cathepsin CTSC. A The structure of Pro-CTSC is defined by distinct domains including the exclusion domain, the propeptide, and the papain-like structure region, encompassing both the heavy chain and the light chain. The exclusion domain is involved in modulating substrate specificity and stability. The propeptide is an inhibitory segment regulating enzyme activity, typically removed during maturation and activation. In the papain-like structure region, the heavy chain holds catalytic residues for proteolysis, resembling papain proteases and the light chain aids substrate binding and stability. B The maturation and structural details of cathepsin C (CTSC) involve a series of steps. Initially, the pro-CTSC monomer (modified from Protein Data Bank (PDB) entry ID: 6IC7) undergoes processing to form the pro-CTSC dimer (PDB ID: 4OEL). This dimerization process involves the convergence of two individual pro-CTSC monomers, resulting in the creation of a functional dimeric architecture, an arrangement that ensures the proper functionality of the enzyme. The pro-CTSC dimer is further processed to yield the mature CTSC enzyme (PDB ID: 61C7) with the ability to effectively participate in the degradation of proteins. C Schematic representation of the active site of papain-like peptidases modified for CTSC. The enzyme exhibited substrate binding sites labeled from S3 to S2', while substrate residues denoted by blue circles marked from P2 to P2'. An arrow indicates the cleavage site
Initially synthesized as an inactive zymogen in dimeric form, CTSC undergoes further processing to attain maturity. Upon maturation, it adopts a compact tetramer structure, with each monomer housing heavy and light chain active sites resembling a papain-like structure (Fig. 2B) [19, 20, 24]. Mature CTSC comprises four identical monomers, interconnected by non-covalent interactions, with fully exposed active site clefts. The active site consists of the heavy chain and the light chain on the outer surface of the protein complex [1]. The heavy chain of each monomer consists of the catalytic Cys234 on the central α-helix. The catalytic dyad acts as a key catalytic residue and is formed by the reactive residue of Cys234 from the heavy chain and His381 in the light chain forming a thiolate-imidazolium ion pair. Mature CTSC is a tetrameric structure of a marginally flattened sphere in a diameter ~ 80 Å along with a spherical cavity which has a diameter ~ 20 Å in the center. The molecule has tetrahedral symmetry with its axis coinciding with the crystal symmetry axis of the I222 space group. The asymmetric part of the crystal presents a monomer. Each monomer is composed of three domains: 2 papain-like structures which have a catalytic unit and 1 exclusion domain. The papain-like structures consist of N-terminal heavy chain and C-terminal light chain. The exclusion domain, not having analogy with papain-like protease, provides the tetrahedral structure and enhances the active site cleft’s extensions, so it creates features that endow CTSC activity [25] (Fig. 2B).
The known crystal structures of CTSC are complex with peptide-based inhibitors forming the substrate binding pockets [26, 27]. The S1 site is located at the active site entrance and the S2 site is a hydrophobic pocket containing chloride ion and two water molecules [1]. The S1 site comprises a broad area located in an exposed surface of the molecule that can accommodate large and hydrophobic amino acid residues. The exclusion domain is responsible for the aminopeptidase activity by blocking the S2 site providing a key interaction with the substrate through the Asp1 side chain and making it only accessible to the N-terminus of its substrates (Fig. 2C) [17]. The carboxylic group of the Asp1 side chain is responsible for the anchoring of the N-terminal amino group of CTSC substrates [27]. The Asp1 also interferes with the binding of the positively charges side chains of arginine and lysine residues at S2 site. The three amino acids residues (Asp1, Cys234, His381) which together form a catalytic ternary complex, is responsible for identifying the type of substrate, limiting the length of the cleaved polypeptide, and cleaving the polypeptide [1]. Moreover, the CTSC active site is also blocked beyond S2 binding site by the N-termini of exclusion domain, beta-hairpin, and carbohydrate ring which attach to Asn5 and interfere substrate access. Based on the structure and the active site interaction, the exclusion domain is thought to be derived from a metallic-protease inhibitor which behaves as a partial block of entry into the cleft [17].
Substrate specificity
CTSC acts as a dipeptidyl aminopeptidase with broad substrate specificity. CTSC cleaves two-residue units until it reaches a stop sequence. The protonation of the N-terminal amino group is required for the hydrolysis, using dipeptide AMC substrates. The S1 site has an affinity for compounds with a hydrophobic structure while the S2 pocket has an affinity for smaller aliphatic or hydrophobic with basic structures [1]. CTSC exhibits optimal aminopeptidase activity in slightly acidic pH conditions and is activated by chloride ions at a pH below 7 [28].
Subcellular localization and secretion
CTSC is ubiquitous and is mainly located in the lysosomal or endosomal compartments of cells. Because of its colocalization with active neutrophil serine proteases in the Golgi apparatus, the activation process of granular proteases most likely starts in this compartment. Active CTSC along with in vitro differentiated neutrophil-like cells is found to be stored in cytoplasmic granules in promyelocytic HL60 precursor cells [20]. Pro-CTSC is mainly secreted by the Golgi apparatus into the extracellular milieu. When there are chemical or physiological stimuli, active CTSC is excreted into the extracellular milieu with other lysosomal enzymes by neutrophils, mast cells and lymphocytes [7].
CTSC associated syndromes: Haim–Munk syndrome (HMS), Papillon–Lefevre syndrome (PLS), and aggressive periodontitis (AP)
CTSC plays an essential role in the host defense against bacteria and the pathogenic aberration in the CTSC gene leads to an impaired host response to microbes, resulting in infections and inflammatory diseases [1, 29]. In the following section we review some of the key diseases associated with CTSC. Interestingly over 120 CTSC associated maladies have been reported as shown in Table 1. Most notable of these are with Haim–Munk Syndrome (HMS; MIM #245010), Papillon–Lefevre syndrome (PLS;MIM #245000), and juvenile/aggressive periodontitis (AP; MIM #170650) [10]. The latter two diseases are of particular interest as they have afflictions with the orofacial complex.
Haim–Munk syndrome (HMS)
This is a rare autosomal recessive disorder. The development of red, scaly thickened patches of skin on the palms of the hands and soles of the feet (palmoplantar hyperkeratosis) characterizes HMS. Frequent pus-producing skin infections, hypertrophy of the fingernails and toenails (onychogryphosis), and periodontitis, which often results in premature tooth loss, are also commonly reported [10, 30, 31]. Additional features associated with the disorder may include flat feet (pes planus), abnormally long and slender fingers and toes (arachnodactyly), and loss of bone tissue at the ends of the fingers and/or toes (acroosteolysis) [29].
Papillon–Lefevre syndrome (PLS)
PLS is a rare autosomal recessive disorder characterized by palmoplantar hyperkeratosis and aggressively progressing periodontitis affecting both the primary and permanent dentition. It typically becomes apparent at 1–5 years old, but commonly coincides with the eruption of primary teeth [32]. The gingivae (gums) in these patients are usually inflamed during the eruption of primary teeth, followed by a rapid destruction of periodontium and a premature loss of the deciduous dentition. Nevertheless, the gingiva heals uneventfully after the exfoliation of the primary teeth. Then, the periodontal inflammation recurs after the eruption of permanent teeth, and without proper dental intervention, most permanent teeth are lost by the age of 16 years [33].
The PLS patients exhibit signs of gingivitis, periodontitis, stomatitis, and probably regional adenopathy. Additional findings associated with PLS may include frequent pyogenic skin infections, nail dystrophy, hyperhidrosis, arachnodactyly, and intracranial calcification [10, 31, 34, 35]. Among the various palmoplantar keratoderma conditions, only PLS and HMS are linked to periodontal destruction. Numerous studies have indicated that PLS and HMS represent phenotypic variants of a common disorder resulting from variants in CTSC [36, 37].
Aggressive periodontitis (AP)
Aggressive periodontitis (AP), also referred as Juvenile periodontitis [38], is a disease of the tooth supporting tissues involving the periodontal pocket and the attached gums (Fig. 3A), and its basic etiology is yet unknown. AP is characterized by early onset and aggressive periodontal tissue loss including several teeth, but other symptoms associated with CTSC such as palmoplantar keratosis are not found in AP. Multiple factors have been suggested for the disease including biallelic variants in CTSC [39,40,41,42].
Clinical features of aggressive periodontitis and mechanisms of CTSC in periodontal destruction. A Oral features of a 7-year-old patient with generalized aggressive periodontitis. B The involvement of CTSC in periodontal tissue destruction is mediated through several mechanisms. Two key scenarios are likely co-contributors for aggressive periodontitis within the context of PLS, which entail the persistense of the key periodontal pathogens (such as Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis) and the continuous recruitment of neutrophils. These may trigger an exaggerated immune response and activate innate immune cells, including neutrophils, leading to chronic inflammation and the production of inflammatory mediators that can activate CTSC within the periodontal niche. Additionally, in the context of PLS-associated periodontitis, the uncontrolled recruitment of neutrophils might also lead to excessive release of proteases, including CTSC. This unrestrained protease activity can contribute to the degradation of connective tissue and alveolar bone matrix, disrupting the delicate balance between tissue destruction and repair, leading to the progressive periodontal tissue destruction observed in aggressive periodontitis
Mechanisms of periodontal tissue destruction in PLS and AP
The failure of the host antimicrobial peptide systems, such as LL37, NE, CatG, and the neutrophil extracellular trap (NET)-complexed proteases to remove pathogenic bacteria are thought to be a major cause of periodontitis in the PLS patients [7]. Comprehensive analysis of the impact of CTSC deficiency on NSPs activity and neutrophil function, on the other hand, has revealed a far more complex and interconnected series of events, including neutrophil dysfunction and tissue destruction seen at the disease active sites [43]. The neutrophils of the PLS patients still have an ability to destroy bacteria by producing ROS, hypochlorous acid, and antimicrobial peptides [2, 7, 44]. It appears that the defects seen in PLS neutrophils are caused by a long-term exposure to a microbial stimulus, such as those of chronic periodontitis and chronic skin infection.
The four key periodontopathic bacteria Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Fusobacterium nucleatum, and Treponema denticola have an important role in the progression of periodontal destruction [45]. Occurrence of antibodies to key toxin of Actinobacillus actinomycetemcomitans in some members of an extended family with PLS provides clues [45] to the possibility of limited neutrophil antimicrobial ability in this disease. It appears therefore, bacterial pathogens may persist leading to dysfunctional immune-inflammatory stimulation within periodontal tissues in PLS [7]. Other than periodontal disease, the PLS patients also experience dermatological disorders that are characterized by significant neutrophil infiltration in the afflicted tissues [7].
Other explanations seem likely to underpin the etiology of aggressive periodontitis in PLS. First is the relentless recruitment of primed and/or activated neutrophils to the oral tissues [7]. Studies on CXCL8 and MIP1α, both potent neutrophil chemoattractants, reveal them to be the NSP targets for inactivation [46, 47]. MIP1α also activates osteoclasts [48]. This provides an insight into a more complex role for neutrophils in coordinating immune responses. NSPs have an important role in regulating additional neutrophil recruitment by silencing the inducers of neutrophil accumulation. MIP1α may stimulate the persistent recruitment of neutrophils to inflamed periodontal tissues in the absence of NSP activity. Second is the persistence of pathogenic species in PLS due to insufficient bacterial killing. Rather than causing immediate tissue damage, pathogens are more likely to trigger indirect tissue damage mediated by neutrophil dysfunction. The continuous recruitment of neutrophils by the pathogenic stimulus results in an excess of ROS and pro-inflammatory cytokines, leading to connective tissue destruction and loss of periodontium Fig. 3B) [7]. However, the intricacies of these mechanisms are multifaceted and interconnected and there are additional aspects such as extracellular matrix remodeling and dysregulated immune response to consider.
To summarize, some cases of AP, and PLS seem to be a result of pathogenic variants of CTSC. The insufficiency of NSPs causes the neutrophil dysfunction and seems to reduce bacterial clearance during infection, to generate a destructive pro-inflammatory environment within periodontal tissue, to increase ROS and cytokine production, and eventually to abrogate downregulation of CXCL8 and MIP1α, leading to tissue destruction and alveolar bone loss.
Variants of the CTSC gene associted with diseases
Over 100 documented cases have been identified with variants of the CTSC gene, all of which have consistently exhibited the hallmark features of PLS, characterized by the presence of palmoplantar keratoderma and severe, early-onset, or aggressive periodontitis. According to the new classification of periodontal diseases of 2018 aggressive periodontitis would be classified as a stage IV, grade C generalized periodontitis [49]. The terminology used to describe the periodontal manifestations in these patients vary among studies, but collectively signifies exceptionally severe and early-onset periodontitis. A summary of all studies detailing CTSC variants is provided in Table 1 [36, 39, 50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98].
Missense variants are the most prevalent, followed by an equal occurrence of nonsense and insertion-deletion variants. Splice-site variants are infrequent, while gross deletion variants and regulatory variants are rare. Interestingly, we observed that three families where individuals carrying biallelic CTSC variant displayed solely the features of periodontitis, without palmoplantar keratoderma. These cases encompass:
-
1)
A Jordanian family identified with a homozygous variant c.1040A > G, p.Tyr347Cys[99],
-
2)
A patient with compound heterozygous variant c.815G > A, p.Arg272His; c.1235A > G p.Tyr412Cys [56], and
-
3)
A Turkish family with homozygous c.302G > C, p.Trp101Ser who also had additional features such as hypodontia, taurodontism, molar incisor hypomineralization, and language delay [55]. These cases are noteworthy as they challenge the typical diagnostic pattern of PLS.
Conversely, there exist instances of individuals presenting with typical palmoplantar keratoderma but lacking severe periodontitis. For instance, a Japanese patient with a homozygous nonsense variant c.315dup, p.Lys106fs displayed a distinctive trait of maintaining all permanent teeth beyond the age of 40 years, in contrast to the premature tooth loss typically linked to PLS [83]. This delayed onset of periodontitis has also been documented in previous cases of PLS [100, 101]. Variability in phenotypic presentation and the severity of periodontitis have been noted among patients carrying the same variant [36, 53, 61]. Additionally, some patients may manifest other systemic abnormalities, including recurrent bacterial skin infections, multiple cutaneous abscesses, ventricular septal defects, language delay, iron deficiency anemia, as well as other orodental findings such as missing teeth [29, 55, 102]. These highlight the diverse array of clinical manifestations associated with various CTSC, revealing novel insights into the unexplored roles of CTSC in both health and disease.
Therapeutic use
Given below is a comprehensive account of some of the major and minor illnesses that are associated with CTSC. Namely,
-
PLS
-
Chronic inflammatory lung disease
-
COVID-19
-
Cancers
-
The anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis
-
Sudden cardiac death (SCD)/ atherosclerosis/ cardiovascular disease
-
Neuroinflammatory diseases
Papillon–Lefevre syndrome (PLS)
The available treatments for PLS, whether oral or dermatological, remain constrained, occasionally leading to toxic effects such as those caused by the application of topical steroids. However, recent investigations have unveiled novel molecular pathways and potential pharmacological targets for managing PLS. One study, for instance, observed disparities in azurophil granule proteins between PLS patients and healthy subjects through proteomic analysis and western blotting [58]. The method involved subcellular fractionation of neutrophils from PLS patients and controls, pooling fractions based on marker protein distribution into azurophil granules (α band), specific granules (β1 band), gelatinase granules (β2 band), and light membranes (γ band). Western blotting revealed the absence of serine protease and eosinophil peroxidase. Proteome profiling showed significantly decreased quantities of serine proteases (NE, CTSG, PR3, azurocidin) in PLS neutrophils. Furthermore, it appears that neutrophils from PLS patients exhibit an inability to form NETs, which are essential components of the immune response [58, 103]. In recent years, the experimental research has shown that the metabolic and autophagic dysfunction of CTSC-deficiency fibroblasts in PLS can be corrected by recombinant CTSC (rCTSC) [104].
The fibroblasts of PLS patients showed a significant decrease in the rate of proliferation and mitochondrial energetics, and an impairment of autophagic flux shown by elevated expression levels of both LC3-II and p62/SQSTM1. This was investigated using a BafA1 assay and ultrastructural examination [104, 105]. Moreover, oxidative stress has been related to the pathophysiology of PLS [74]. Increased ROS generation along with decreased antioxidant defenses was observed in the fibroblasts from PLS patients, resulting in lysosomal instability and membrane permeabilization [106]. PLS fibroblasts treated with rCTSC in three different doses showed a statistically significant, dose-dependent reduction in the proliferation rate, observed at 24, 48, 72, and 120 h. Additionally, there was a partial recovery of CTSC enzymatic activity after treatment with rCatC for 120 h. Furthermore, increased expression levels of LC3-II and p62/SQSTM1, indicating improvement of autophagic flux, and reduced IL-1b, indicating decreased inflammasome activation have also been noted [104]. The available data indicates that recombinant cathepsin administration can be a promising therapeutic approach for the management of PLS.
A deficiency in CTSC activity, as seen in PLS, does not impact patient survival despite its clear pathophysiological consequences. Clinical observations suggest that pharmacological inhibition of CTSC, which mimics the phenotypic effects seen in PLS, might be a viable therapeutic strategy. Specifically, transient or partial inhibition of CTSC in bone marrow progenitor cells could potentially modulate serine protease activity, offering therapeutic benefits in chronic inflammatory lung diseases characterized by robust neutrophil infiltration, granulomatosis with polyangiitis (GPA) and other neutrophil-mediated autoimmune disorders [7].
A clinical trial (NCT01116934) investigated whether PLS patients compensate for their impaired CTSC activity by overproducing proinflammatory cytokines, thereby promoting neutrophil recruitment. Cytokine profiles were compared between PLS patients and healthy controls following stimulation with lipopolysaccharide (LPS) and a combination of interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α). Although a slight elevation in certain cytokines was observed in PLS patients, these differences did not reach statistical significance. Consequently, the study did not establish a definitive link between increased cytokine production and CTSC deficiency in PLS, suggesting that cytokine profiles in blood cultures may not be a reliable diagnostic marker for this condition [107]. Further research and clinical trials are needed for a better understanding.
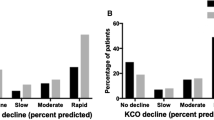
Chronic obstructive pulmonary diseases (COPD)
COPD is caused by hyperactive inflammatory defense mechanisms that are triggered by a combination of factors such as genetics, pollutants, and microbes. There are many putative relationships between CTSC and chronic inflammatory lung diseases [7]. For instance mature CTSC have been detected in sputa of patients with neutrophil dominant chronic inflammatory lung disease such as COPD, cystic fibrosis, bronchiectasis, and neutrophilic asthma, and macrophage dominant chronic inflammatory lung diseases such histiocytosis X, desquamative interstitial pneumonia, and sarcoidosis [7, 20].
In these neutrophil-driven inflammatory pulmonary diseases, circulating neutrophils have numerous activated NSPs that can be activated by CTSC, causing tissue destruction [7]. Indeed, the amount of CTSC has a correlation with the quantity of neutrophils [20]. In addition, a deficiency of alpha-1 antitrypsin (AAT), the NSPs inhibitor, in plasma can lead to COPD/emphysema and other diseases [7, 108]. In chronic lung inflammation, dying neutrophils may irreversibly damage lung tissue [7]. Available data indicates a close correlation between the neutrophil quantity and CTSC so much so that the latter could be used as a biomarker of neutrophil-induced pulmonary inflammation. This implies that control of NSPs may be a promising therapeutic strategy for regulating the progression of chronic inflammatory pulmonary diseases.
COVID-19
The global pandemic of COVID-19 is a protean infection caused by the newly discovered coronavirus SARS-CoV-2 but predominantly affects the respiratory tract [109]. The affected individuals present with a wide array of afflictions ranging from asymptomatic disease, mild to moderate symptoms, and severe illness that can be lethal, presenting as acute respiratory distress syndrome (ARDS) comprising respiratory failure, acute lung injury, and edema.
The pathology leading to severe illness of COVID-19 is incompletely understood but the accumulating data indicate that the disease is precipitated by an exaggerated response of the innate immune system (immunological storm) leading to severe irreversible lung injury and respiratory failure [109].
In a recent study, Fassan et al. observed significant overexpression of CTSC in the lung tissue of COVID-19 patients, as evaluated by immunohistochemistry [110]. Neutrophils seem to play a crucial role in hyperinflammation leading to lung injury, due to the release of reactive oxygen species via elastase-related serine proteases activity. Hence NE-related serine proteases, that have been identified as potential pharmacological targets in neutrophilic inflammatory disorders, appear to be an attractive therapeutic target for managing COVID-19.
Cancers
A plethora of recent discoveries indicate CTSC expression in many cancers such as colorectal cancer, hepatocellular carcinoma, squamous cell carcinoma, and glioma [111,112,113,114]. Being a novel area of exploration there are many facets that are awaiting investigation in this context including the genealogy of cancer, stages of tumor progression, and related pathobiology [115,116,117].
It is known that CTSC has an important role in the proliferation of colorectal cancer cells mediated by autophagy [118]. Apoptosis of colorectal cancer cells can be induced by inhibiting CTSC with the CTSC inhibitor (GFDMK). This treatment triggers endoplasmic reticulum stress-mediated JNK phosphorylation, as validated by western blot analysis. Additionally, it leads to mitochondrial cytochrome c translocation and a decrease in mitochondrial membrane potential (MMP), as analyzed by Rhodamine 123 fluorescence staining [111]. CTSC promotes hepatocellular carcinoma cell (HCC) proliferation and metastasis by acting as a cancer-promoting factor [112]. In the skin, CTSC controls the infiltration of immune cells in skin tumors and promote angiogenesis in squamous cell carcinoma [119].
Other interesting recent discoveries appertaining to this issue include increased anticancer potential of curcumin in colorectal cancer both in vitro and in vivo due to CTSC silencing. It has been proposed that CTSC inhibition could be a new chemotherapeutic technique that may be employed in conjunction with established anti-cancer drugs [120]. Furthermore, there is a report on decursin, a natural chemical from Angelica gigas, which decrease gastric cancer cell growth, and promote cell cycle arrest in vitro, by lowering CTSC expression [121].
Furthermore, CTSC has a dual role in attracting neutrophils to metastatic and stimulating neutrophils to form NETs. Inhibiting CTSC reduces lung metastases and promotes breast cancer in mice. Lung metastasis in mice is successfully inhibited by targeting CTSC with AZD7986, a specific and powerful CTSC inhibitor. Conversely, overexpression of CTSC enhances lung metastasis [114]. The fact that CTSC is strongly associated with tumor development is clear from the foregoing although the underlying mechanisms are yet to be explored.
The anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis
ANCA-associated vasculitis (AAV) is an autoimmune disease characterized by inflammation of the small blood vessels. It has been subgrouped into three main variants: microscopic polyangiitis (MPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
NSPs are proven to contribute to AAV, as neutrophils and monocytes are the only cells that express ANCA auto antigens proteinase 3 (PR3) and myeloperoxidase (MPO) [122]. CTSC proteolytically activates the pro-neutrophil serine proteases in the bone marrow which contributes to the production of mature NE [123]. The membrane-bound proteinase 3 (mPR3) expressed by myeloid cells is the main target antigen of ANCA. By binding to mPR3, ANCA triggers an activation cascade, resulting in a secretion of the active PR3 causing vascular damage.
CTSC from zymogens also activates the proteolytic function of NSPs, including PR3. Therefore, many new upcoming studies are based on the therapeutic effects associated with the pharmacological inhibition of CTSC in reducing PR3 and the severity of AAV and granulomatosis with polyangiitis [123]. In a study by Jerke et al. (2019), the blockade of CTSC using CTSC inhibitors was found to reduce NSP protein levels and their proteolytic activation [123]. Subsequently, they delved into the genetic deficiency effect of CTSC in PLS patients, revealing a significant reduction in total NSPs within neutrophils and monocytes, without impacting neutrophil differentiation [122]. Notably, no signs of generalized immunodeficiency were observed in the studied PLS patients, implying that CTSC influences NSP activation but not immune cell differentiation [124]. The study has been replicated using human stem cells. Pharmacological inhibition of CTSC in neutrophils via an inhibitor resulted in lowered NSPs and membrane PR3 levels. This reduction corresponded to a decreased neutrophil-induced glomerular microvascular endothelial cell damage in both scenarios [122]. However, as shown in other lysosomal disorders, a short-term therapeutic inhibition can result in neutrophil dysfunction and periodontitis [124, 125].
Sudden cardiac death (SCD)/ atherosclerosis/ cardiovascular disease
SCD is defined as death due to a cardiovascular cause that occurs within 1 h of the onset of symptoms [126]. The most common pathological basis of SCD is coronary atherosclerosis [127,128,129] Studies have shown a relationship between CTSC and both SCD and atherosclerotic vascular disease [102]. A recent study using quantitative proteomics to analyze protein alterations in the human left anterior descending coronary artery showed significantly increased CTSC expression in coronary heart disease (CHD) and sudden cardiac death (SCD) compared to a control group. This finding was validated using western blotting and immunohistochemistry [102]. Hence it appears that CTSC is likely to be a good predictive marker of SCD with a promising potential in differential diagnosis of CHD and SCD. However, the small sample size is a limitation of the latter study. Another study has also shown upregulated CTSC gene and protein expression in atherosclerotic lesions [130]. In summary, CTSC seems to be a good molecular marker of the inflammatory response associated with atherosclerosis and SCD.
Neuroinflammatory diseases
CTSC is also considered to be a promising therapeutic target in preventing neuroinflammatory disorders. The data for this emanates from several studies. First, CTSC levels are altered in the pathological tissues derived from the mouse brain and it appears to be involved in neuroinflammation. The expression of CTSC in mouse brains has shown that it is not expressed in the healthy brain tissues but is significantly increased in pathological brain tissue. The activated microglia of the mouse brain were the most immunopositive for CTSC in these studies [131]. Another study on the association of CTSC expression and neuroinflammation induced by lipopolysaccharide (LPS) injections has shown varying CTSC expression levels in mouse neurons and microglia at different time points, post-injection. Further, in vitro, studies have also shown LPS, cytokines IL-6, and IL-1β -induced CTSC expression in microglial cells in a dose-dependent manner. A demyelinating mouse model induced by cuprizone also show leukocyte infiltration, and expression of glia-derived chemokine CXCL2 associated with CTSC expression [132].
Another study of CTSC in a cryogenic traumatic brain injury has shown that CTSC aggravates neuroinflammation by up-regulating CCL2 and CXCL2 expression in neurons and neuroglia [133]. Also, a study of acute and chronic stress-induced mice models has shown that CTSC overexpression leading to inflammation, neurochemical disturbance, and aggravated depressive behavior [94]. In summary, there is a substantial body of data to suggest a key contributory role of CTSC in neuroinflammation and hence it appears to be a promising therapeutic candidate for mitigating the progression of neuroinflammatory disease.
Current clinical trials, challenges, and future directions for CTSC inhibitors
CTSC has emerged as a promising pharmacological target for modulating neutrophil-driven inflammation and related pathologies. Preclinical studies utilizing murine models of inflammation have demonstrated the protective effects of CTSC knockdown, supporting its potential as a therapeutic target. The inhibition of CTSC activity is hypothesized to effectively reduce neutrophil extracellular trap (NET) formation, a key driver of inflammation in various diseases [7]. Given its association with several inflammatory conditions, CTSC inhibition is being explored as a therapeutic strategy, with multiple inhibitors under development at different stages of clinical trials.
GSK-2793660: This irreversible CTSC inhibitor was evaluated in a Phase I clinical trial (NCT02058407) for cystic fibrosis, non-cystic fibrosis bronchiectasis, and ANCA-associated vasculitis. While it demonstrated efficacy in reducing neutrophil serine protease (NSP) activity, its clinical application was limited by epidermal desquamation [134, 135].
AZD7986 (Brensocatib): This non-covalent CTSC inhibitor has shown promise in treating non-cystic fibrosis bronchiectasis. Ongoing clinical trials (NCT02653872, NCT05673603, NCT05517525, NCT06178783, NCT05652257, NCT06344728, NCT05344508, NCT05965570, NCT05090904, NCT05826574) are assessing its safety and efficacy. Phase II trials have demonstrated reduced NSP activity in bronchiectasis patients, correlating with clinical improvement. Brensocatib has also exhibited anti-metastatic effects in preclinical breast cancer models [1, 135, 136].
IcatCXPZ-01: This novel CTSC inhibitor prevents the maturation of NSP zymogens. Preclinical studies in non-human primates have shown almost complete elimination of NSPs in white blood cells, indicating its potential as a therapeutic agent [135, 136].
The development of CTSC inhibitors faces several challenges. Ensuring specificity is crucial, as off-target effects could lead to undesirable side effects. Research is concentrated on creating highly selective inhibitors that have minimal impact on other cathepsins or essential cellular functions. Additionally, delivering CTSC inhibitors effectively to target tissues is a significant challenge. Strategies such as targeted drug delivery systems and formulation optimization are being investigated to enhance bioavailability and reduce systemic side effects.
The insights gained from CTSC research have significant implications for clinical practice. Measuring CTSC activity levels in blood or tissue samples at certain time points might serve as a diagnostic tool for identifying individuals at risk for or currently experiencing inflammatory diseases. Additionally, CTSC activity levels may correlate with disease severity and predict response to therapy, suggesting that they could be useful as prognostic indicators for guiding treatment decisions and personalizing therapy. CTSC inhibitors could be utilized as targeted therapies, specifically addressing the inflammatory pathways involved in various diseases, potentially leading to more effective and less toxic treatments compared to broad-spectrum anti-inflammatory agents. This approach could enable early intervention, potentially mitigating disease progression, and improving patient outcomes. Understanding individual variations in CTSC activity and response to inhibitors could pave the way for personalized medicine, allowing for tailored treatment regimens and reducing reliance on conventional therapies.
Conclusion
The foregoing review elucidates the multifaceted role of CTSC in various biological phenomena and its putative role in both health and disease. The complex structure and the versatile functionality of CTSC underscore its role in activation of granule-associated proteases, impacting not only the immune response but also tissue homeostasis. The extensive involvement of CTSC in diseases such as PLS, HMS, and AP reveals its intricate interplay in regulating neutrophil activity and NSP zymogen activation, which in turn influences such disease progression. While promising, the field of CTSC inhibition for inflammatory diseases remains ripe for exploration. Several key knowledge gaps remain. For instance, a deeper understanding of the precise mechanisms by which CTSC inhibition modulates NET formation in different disease contexts is crucial. Furthermore, the long-term safety and efficacy of CTSC inhibitors require comprehensive evaluation. Future investigations should explore the potential for personalized approaches, tailoring CTSC inhibition strategies to specific patient populations and disease subtypes. By addressing these research priorities, we can accelerate the translation of CTSC inhibitors into effective therapies for inflammatory disorders.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Shen XB, Chen X, Zhang ZY, Wu FF, Liu XH. Cathepsin C inhibitors as anti-inflammatory drug discovery: challenges and opportunities. Eur J Med Chem. 2021;225: 113818. https://doi.org/10.1016/j.ejmech.2021.113818.
Perera NC, Schilling O, Kittel H, Back W, Kremmer E, Jenne DE. NSP4, an elastase-related protease in human neutrophils with arginine specificity. Proc Natl Acad Sci USA. 2012;109(16):6229–34. https://doi.org/10.1073/pnas.1200470109.
Pham CT. Neutrophil serine proteases: specific regulators of inflammation. Nat Rev Immunol. 2006;6(7):541–50. https://doi.org/10.1038/nri1841.
AhYoung AP, Eckard SC, Gogineni A, Xi H, Lin SJ, Gerhardy S, et al. Neutrophil serine protease 4 is required for mast cell-dependent vascular leakage. Commun Biol. 2020;3(1):687. https://doi.org/10.1038/s42003-020-01407-0.
Pham CT, Ley TJ. Dipeptidyl peptidase I is required for the processing and activation of granzymes A and B in vivo. Proc Natl Acad Sci U S A. 1999;96(15):8627–32. https://doi.org/10.1073/pnas.96.15.8627.
Adkison AM, Raptis SZ, Kelley DG, Pham CT. Dipeptidyl peptidase I activates neutrophil-derived serine proteases and regulates the development of acute experimental arthritis. J Clin Invest. 2002;109(3):363–71. https://doi.org/10.1172/jci13462.
Korkmaz B, Caughey GH, Chapple I, Gauthier F, Hirschfeld J, Jenne DE, et al. Therapeutic targeting of cathepsin C: from pathophysiology to treatment. Pharmacol Ther. 2018;190:202–36. https://doi.org/10.1016/j.pharmthera.2018.05.011.
Palmér R, Mäenpää J, Jauhiainen A, Larsson B, Mo J, Russell M, et al. Dipeptidyl peptidase 1 inhibitor AZD7986 induces a sustained, exposure-dependent reduction in neutrophil elastase activity in healthy subjects. Clin Pharmacol Ther. 2018;104(6):1155–64. https://doi.org/10.1002/cpt.1053.
Keir HR, Long MB, Abo-Leyah H, Giam YH, Vadiveloo T, Pembridge T, et al. Dipeptidyl peptidase-1 inhibition in patients hospitalised with COVID-19: a multicentre, double-blind, randomised, parallel-group, placebo-controlled trial. Lancet Respir Med. 2022;10(12):1119–28. https://doi.org/10.1016/s2213-2600(22)00261-2.
de La Dure-Molla M, Fournier BP, Manzanares MC, Acevedo AC, Hennekam RC, Friedlander L, et al. Elements of morphology: standard terminology for the teeth and classifying genetic dental disorders. Am J Med Genet Part A. 2019;179(10):1913–81. https://doi.org/10.1002/ajmg.a.61316.
Rawlings ND. Twenty-five years of nomenclature and classification of proteolytic enzymes. Biochim Biophys Acta Proteins Proteom. 2020;1868(2): 140345. https://doi.org/10.1016/j.bbapap.2019.140345.
Rawlings ND, Barrett AJ, Finn R. Twenty years of the MEROPS database of proteolytic enzymes, their substrates and inhibitors. Nucleic Acids Res. 2016;44(D1):D343–50. https://doi.org/10.1093/nar/gkv1118.
Sijwali P, Nivya MA. Cysteine proteases. In: Joseph J, editor. Encyclopedia of biological chemistry III. 3rd ed. Amsterdam: Elsevier; 2021. p. 270–9.
Cathepsins KH. In: Enna SJ, Bylund DB, editors. xPharm: the comprehensive pharmacology reference. New York: Elsevier; 2007. p. 1–4.
Lecaille F, Kaleta J, Brömme D. Human and parasitic papain-like cysteine proteases: their role in physiology and pathology and recent developments in inhibitor design. Chem Rev. 2002;102(12):4459–88. https://doi.org/10.1021/cr0101656.
Turk B, Turk D, Turk V. Protease signalling: the cutting edge. Embo J. 2012;31(7):1630–43. https://doi.org/10.1038/emboj.2012.42.
Turk D, Janjić V, Stern I, Podobnik M, Lamba D, Dahl SW, et al. Structure of human dipeptidyl peptidase I (cathepsin C): exclusion domain added to an endopeptidase framework creates the machine for activation of granular serine proteases. Embo J. 2001;20(23):6570–82. https://doi.org/10.1093/emboj/20.23.6570.
Bühling F. Cysteine proteases, cathepsins. In: Laurent GJ, Shapiro SD, editors. Encyclopedia of respiratory medicine. Oxford: Academic Press; 2006. p. 594–9.
Dahl SW, Halkier T, Lauritzen C, Dolenc I, Pedersen J, Turk V, Turk B. Human recombinant pro-dipeptidyl peptidase I (cathepsin C) can be activated by cathepsins L and S but not by autocatalytic processing. Biochemistry. 2001;40(6):1671–8. https://doi.org/10.1021/bi001693z.
Hamon Y, Legowska M, Hervé V, Dallet-Choisy S, Marchand-Adam S, Vanderlynden L, et al. Neutrophilic Cathepsin C is maturated by a multistep proteolytic process and secreted by activated cells during inflammatory lung diseases. J Biol Chem. 2016;291(16):8486–99. https://doi.org/10.1074/jbc.M115.707109.
Turk B, Turk D, Dolenc I, Turk V. Chapter 448—Dipeptidyl-Peptidase I. In: Rawlings ND, Salvesen G, editors. Handbook of proteolytic enzymes, 3rd Edition. Academic Press; 2013. p. 1968–74.
Ishidoh K, Muno D, Sato N, Kominami E. Molecular cloning of cDNA for rat cathepsin C. Cathepsin C, a cysteine proteinase with an extremely long propeptide. J Biol Chem. 1991;266(25):16312–7. https://doi.org/10.1016/S0021-9258(18)55298-4.
Rao NV, Rao GV, Hoidal JR. Human dipeptidyl-peptidase I: gene characterization, localization, and expression. J Biol Chem. 1997;272(15):10260–5. https://doi.org/10.1074/jbc.272.15.10260.
Korkmaz B, Lesner A, Letast S, Mahdi YK, Jourdan ML, Dallet-Choisy S, et al. Neutrophil proteinase 3 and dipeptidyl peptidase I (cathepsin C) as pharmacological targets in granulomatosis with polyangiitis (Wegener granulomatosis). Semin Immunopathol. 2013;35(4):411–21. https://doi.org/10.1007/s00281-013-0362-z.
Olsen JG, Kadziola A, Lauritzen C, Pedersen J, Larsen S, Dahl SW. Tetrameric dipeptidyl peptidase I directs substrate specificity by use of the residual pro-part domain. FEBS Lett. 2001;506(3):201–6. https://doi.org/10.1016/S0014-5793(01)02911-8.
Furber M, Tiden AK, Gardiner P, Mete A, Ford R, Millichip I, et al. Cathepsin C inhibitors: property optimization and identification of a clinical candidate. J Med Chem. 2014;57(6):2357–67. https://doi.org/10.1021/jm401705g.
Mølgaard A, Arnau J, Lauritzen C, Larsen S, Petersen G, Pedersen J. The crystal structure of human dipeptidyl peptidase I (cathepsin C) in complex with the inhibitor Gly-Phe-CHN2. Biochem J. 2007;401(3):645–50. https://doi.org/10.1042/bj20061389.
Cigic B, Pain RH. Location of the binding site for chloride ion activation of cathepsin C. Eur J Biochem. 1999;264(3):944–51. https://doi.org/10.1046/j.1432-1327.1999.00697.x.
Yu H, He X, Liu X, Zhang H, Shen Z, Shi Y, Liu X. A novel missense variant in cathepsin C gene leads to PLS in a Chinese patient: a case report and literature review. Mol Genet Genomic Med. 2021;9(7): e1686. https://doi.org/10.1002/mgg3.1686.
Pahwa P, Lamba AK, Faraz F, Tandon S. Haim-Munk syndrome. J Indian Soc Periodontol. 2010;14(3):201–3. https://doi.org/10.4103/0972-124x.75919.
Albandar JM, Susin C, Hughes FJ. Manifestations of systemic diseases and conditions that affect the periodontal attachment apparatus: case definitions and diagnostic considerations. J Periodontol. 2018;89(S1):S183–203. https://doi.org/10.1002/JPER.16-0480.
Dhanrajani PJ. Papillon-Lefevre syndrome: clinical presentation and a brief review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(1):e1-7. https://doi.org/10.1016/j.tripleo.2009.03.016.
Ullbro C, Crossner CG, Nederfors T, Alfadley A, Thestrup-Pedersen K. Dermatologic and oral findings in a cohort of 47 patients with Papillon–Lefèvre syndrome. J Am Acad Dermatol. 2003;48(3):345–51. https://doi.org/10.1067/mjd.2003.197.
Sreeramulu B, Shyam ND, Ajay P, Suman P. Papillon–Lefèvre syndrome: clinical presentation and management options. Clin Cosmet Investig Dent. 2015;7:75–81. https://doi.org/10.2147/ccide.S76080.
Hattab FN, Rawashdeh MA, Yassin OM, al-Momani AS, al-Ubosi MM. Papillon–Lefèvre syndrome: a review of the literature and report of 4 cases. J Periodontol. 1995;66(5):413–20. https://doi.org/10.1902/jop.1995.66.5.413.
Hart TC, Hart PS, Michalec MD, Zhang Y, Firatli E, Van Dyke TE, et al. Haim-Munk syndrome and Papillon–Lefèvre syndrome are allelic mutations in cathepsin C. J Med Genet. 2000;37(2):88–94. https://doi.org/10.1136/jmg.37.2.88.
Rai R, Thiagarajan S, Mohandas S, Natarajan K, Shanmuga Sekar C, Ramalingam S. Haim Munk syndrome and Papillon Lefevre syndrome—allelic mutations in cathepsin C with variation in phenotype. Int J Dermatol. 2010;49(5):541–3. https://doi.org/10.1111/j.1365-4632.2010.04300.x.
Science Therapy Committee of the American Academy of Periodontology. Position paper: periodontal diseases of children and adolescents. J Periodontol. 2003;74(11):1696–704. https://doi.org/10.1902/jop.2003.74.11.1696.
Noack B, Görgens H, Hempel U, Fanghänel J, Hoffmann T, Ziegler A, Schackert HK. Cathepsin C gene variants in aggressive periodontitis. J Dent Res. 2008;87(10):958–63. https://doi.org/10.1177/154405910808701017.
Hodge P, Michalowicz B. Genetic predisposition to periodontitis in children and young adults. Periodontol. 2000;2001(26):113–34. https://doi.org/10.1034/j.1600-0757.2001.2260106.x.
Kinane DF, Hart TC. Genes and gene polymorphisms associated with periodontal disease. Crit Rev Oral Biol Med. 2003;14(6):430–49. https://doi.org/10.1177/154411130301400605.
Loos BG, John RP, Laine ML. Identification of genetic risk factors for periodontitis and possible mechanisms of action. J Clin Periodontol. 2005;32(Suppl 6):159–79. https://doi.org/10.1111/j.1600-051X.2005.00806.x.
Perera NC, Wiesmüller KH, Larsen MT, Schacher B, Eickholz P, Borregaard N, Jenne DE. NSP4 is stored in azurophil granules and released by activated neutrophils as active endoprotease with restricted specificity. J Immunol. 2013;191(5):2700–7. https://doi.org/10.4049/jimmunol.1301293.
Williams R. Killing controversy. J Exp Med. 2006;203(11):2404. https://doi.org/10.1084/jem.20311fta.
Stabholz A, Taichman NS, Soskolne WA. Occurrence of Actinobacillus actinomycetemcomitans and anti-leukotoxin antibodies in some members of an extended family affected by Papillon–Lefèvre syndrome. J Periodontol. 1995;66(7):653–7. https://doi.org/10.1902/jop.1995.66.7.653.
Leavell KJ, Peterson MW, Gross TJ. Human neutrophil elastase abolishes interleukin-8 chemotactic activity. J Leukoc Biol. 1997;61(3):361–6. https://doi.org/10.1002/jlb.61.3.361.
Ryu OH, Choi SJ, Firatli E, Choi SW, Hart PS, Shen RF, et al. Proteolysis of macrophage inflammatory protein-1alpha isoforms LD78beta and LD78alpha by neutrophil-derived serine proteases. J Biol Chem. 2005;280(17):17415–21. https://doi.org/10.1074/jbc.M500340200.
Choi SJ, Cruz JC, Craig F, Chung H, Devlin RD, Roodman GD, Alsina M. Macrophage inflammatory protein 1-alpha is a potential osteoclast stimulatory factor in multiple myeloma. Blood. 2000;96(2):671–5.
Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Clin Periodontol. 2018;45(S20):S149–61. https://doi.org/10.1111/jcpe.12945.
Romero-Quintana JG, Frías-Castro LO, Arámbula-Meraz E, Aguilar-Medina M, Dueñas-Arias JE, Melchor-Soto JD, et al. Identification of novel mutation in cathepsin C gene causing Papillon–Lefèvre syndrome in Mexican patients. BMC Med Genet. 2013;14(1):7. https://doi.org/10.1186/1471-2350-14-7.
Allende LM, García-Pérez MA, Moreno A, Corell A, Carasol M, Martínez-Canut P, et al. Cathepsin C gene: first compound heterozygous patient with Papillon–Lefèvre syndrome and a novel symptomless mutation. Hum Mutat. 2001;17(2):152–3. https://doi.org/10.1002/1098-1004(200102)17:2.
Ochiai T, Nakano H, Rokunohe D, Akasaka E, Toyomaki Y, Mitsuhashi Y, et al. Novel p.M1T and recurrent p.G301S mutations in cathepsin C in a Japanese patient with Papillon-Lefèvre syndrome: implications for understanding the genotype/phenotype relationship. J Dermatol Sci. 2009;53(1):73–5. https://doi.org/10.1016/j.jdermsci.2008.07.006.
Nakano A, Nakano H, LaForgia S, Pulkkinen L, Uitto J, Nomura K, et al. Papillon–Lefèvre Syndrome: mutations and polymorphisms in the cathepsin C gene. J Invest Dermatol. 2001;116(2):339–43. https://doi.org/10.1046/j.1523-1747.2001.01244.x.
Tekin B, Yucelten D, Beleggia F, Sarig O, Sprecher E. Papillon–Lefèvre syndrome: report of six patients and identification of a novel mutation. Int J Dermatol. 2016;55(8):898–902. https://doi.org/10.1111/ijd.13297.
Molitor A, Prud’homme T, Miao Z, Conrad S, Bloch-Zupan A, Pichot A, et al. Exome sequencing identifies a novel missense variant in CTSC causing nonsyndromic aggressive periodontitis. J Hum Genet. 2019;64(7):689–94. https://doi.org/10.1038/s10038-019-0615-3.
Hewitt C, McCormick D, Linden G, Turk D, Stern I, Wallace I, et al. The role of cathepsin C in Papillon–Lefèvre syndrome, prepubertal periodontitis, and aggressive periodontitis. Hum Mutat. 2004;23(3):222–8. https://doi.org/10.1002/humu.10314.
Zhang Y, Hart PS, Moretti AJ, Bouwsma OJ, Fisher EM, Dudlicek L, et al. Biochemical and mutational analyses of the cathepsin c gene (CTSC) in three North American families with Papillon Lefèvre syndrome. Hum Mutat. 2002;20(1):75. https://doi.org/10.1002/humu.9040.
Sørensen OE, Clemmensen SN, Dahl SL, Østergaard O, Heegaard NH, Glenthøj A, et al. Papillon–Lefèvre syndrome patient reveals species-dependent requirements for neutrophil defenses. J Clin Invest. 2014;124(10):4539–48. https://doi.org/10.1172/jci76009.
Cury VF, Costa JE, Gomez RS, Boson WL, Loures CG, De ML. A novel mutation of the cathepsin C gene in Papillon–Lefèvre syndrome. J Periodontol. 2002;73(3):307–12. https://doi.org/10.1902/jop.2002.73.3.307.
Wu Y, Zhao L, Xu C, Wu Y. CTSC compound heterozygous mutations in two Chinese patients with Papillon–Lefèvre syndrome. Oral Dis. 2019;25(5):1394–402. https://doi.org/10.1111/odi.13095.
Toomes C, James J, Wood AJ, Wu CL, McCormick D, Lench N, et al. Loss-of-function mutations in the cathepsin C gene result in periodontal disease and palmoplantar keratosis. Nat Genet. 1999;23(4):421–4. https://doi.org/10.1038/70525.
Meenu S, Pradeep B, Ramalingam S, Sairam T, Rai R, Sankaran R. Papillon–Lefèvre syndrome (PLS) with novel compound heterozygous mutation in the exclusion and peptidase C1A domains of Cathepsin C gene. Mol Biol Rep. 2020;47(7):5681–7. https://doi.org/10.1007/s11033-020-05622-0.
Hu T-T, Zou X-Y, Ye F. Gene mutational analyses of cathepsin C gene in a family with Papillon–Lefèvre syndrome. Hua Xi Kou Qiang Yi Xue Za Zhi. 2019;37(1):31–6. https://doi.org/10.7518/hxkq.2019.01.006.
Hattab FN, Amin WM. Papillon–Lefèvre syndrome with albinism: a review of the literature and report of 2 brothers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(6):709–16. https://doi.org/10.1016/j.tripleo.2004.08.030.
Allende LM, Moreno A, de Unamuno P. A genetic study of cathepsin C gene in two families with Papillon–Lefèvre syndrome. Mol Genet Metab. 2003;79(2):146–8. https://doi.org/10.1016/s1096-7192(03)00070-2.
Erzurumluoglu AM, Alsaadi MM, Rodriguez S, Alotaibi TS, Guthrie PA, Lewis S, et al. Proxy molecular diagnosis from whole-exome sequencing reveals Papillon–Lefevre syndrome caused by a missense mutation in CTSC. PLoS ONE. 2015;10(3): e0121351. https://doi.org/10.1371/journal.pone.0121351.
Castori M, Madonna S, Giannetti L, Floriddia G, Milioto M, Amato S, et al. Novel CTSC mutations in a patient with Papillon–Lefèvre syndrome with recurrent pyoderma and minimal oral and palmoplantar involvement. Br J Dermatol. 2009;160(4):881–3. https://doi.org/10.1111/j.1365-2133.2008.08878.x.
Noack B, Görgens H, Hoffmann T, Fanghänel J, Kocher T, Eickholz P, et al. Novel mutations in the cathepsin C gene in patients with pre-pubertal aggressive periodontitis and Papillon–Lefèvre syndrome. J Dent Res. 2004;83(5):368–70. https://doi.org/10.1177/154405910408300503.
Machado RA, Cuadra-Zelaya FJM, Martelli-Júnior H, Miranda RT, Casarin RCV, Corrêa MG, et al. Clinical and molecular analysis in Papillon–Lefèvre syndrome. Am J Med Genet A. 2019;179(10):2124–31. https://doi.org/10.1002/ajmg.a.61285.
Jouary T, Goizet C, Coupry I, Redonnet-Vernhet I, Levade T, Burgelin I, et al. Detection of an intragenic deletion expands the spectrum of CTSC mutations in Papillon–Lefèvre syndrome. J Investig Dermatol. 2008;128(2):322–5. https://doi.org/10.1038/sj.jid.5700987.
de Haar SF, Jansen DC, Schoenmaker T, De Vree H, Everts V, Beertsen W. Loss-of-function mutations in cathepsin C in two families with Papillon–Lefèvre syndrome are associated with deficiency of serine proteinases in PMNs. Hum Mutat. 2004;23(5):524. https://doi.org/10.1002/humu.9243.
Yin W, Dong M, Ye D, Liu Q, Liu S, Shi C, et al. Cathepsin C promotes the progression of periapical periodontitis. Sci Bull (Beijing). 2020;65(11):951–7. https://doi.org/10.1016/j.scib.2019.12.006.
Nitta H, Wara-Aswapati N, Lertsirivorakul J, Nakamura T, Yamamoto M, Izumi Y, et al. A novel mutation of the cathepsin C gene in a thai family with Papillon-Lefevre syndrome. J Periodontol. 2005;76(3):492–6. https://doi.org/10.1902/jop.2005.76.3.492.
Bullón P, Morillo JM, Thakker N, Veeramachaneni R, Quiles JL, Ramírez-Tortosa MC, et al. Confirmation of oxidative stress and fatty acid disturbances in two further Papillon–Lefèvre syndrome families with identification of a new mutation. J Eur Acad Dermatol Venereol. 2014;28(8):1049–56. https://doi.org/10.1111/jdv.12265.
Hart TC, Hart PS, Bowden DW, Michalec MD, Callison SA, Walker SJ, et al. Mutations of the cathepsin C gene are responsible for Papillon–Lefèvre syndrome. J Med Genet. 1999;36(12):881–7.
Martinho S, Levade T, Fergelot P, Stephan JL. Papillon–Lefèvre syndrome: a new case. Arch Pediatr. 2017;24(4):360–2. https://doi.org/10.1016/j.arcped.2017.01.013.
Kurban M, Cheng T, Wajid M, Kiuru M, Shimomura Y, Christiano AM. A novel mutation in the cathepsin C gene in a Pakistani family with Papillon-Lefevre syndrome. J Eur Acad Dermatol Venereol. 2010;24(8):967–9. https://doi.org/10.1111/j.1468-3083.2010.03575.x.
Moghaddasian M, Arab H, Dadkhah E, Boostani H, Babak AR, Abbaszadegan MR. Protein modeling of cathepsin C mutations found in Papillon–Lefèvre syndrome. Gene. 2014;538(1):182–7. https://doi.org/10.1016/j.gene.2013.11.079.
Yang Y, Bai X, Liu H, Li L, Cao C, Ge L. Novel mutations of cathepsin C gene in two Chinese patients with Papillon–Lefèvre syndrome. J Dent Res. 2007;86(8):735–8. https://doi.org/10.1177/154405910708600809.
Pallos D, Acevedo AC, Mestrinho HD, Cordeiro I, Hart TC. Novel cathepsin C mutation in a Brazilian family with Papillon–Lefèvre syndrome: case report and mutation update. J Dent Child (Chic). 2010;77(1):36–41.
Lefèvre C, Blanchet-Bardon C, Jobard F, Bouadjar B, Stalder JF, Cure S, et al. Novel point mutations, deletions, and polymorphisms in the cathepsin C gene in nine families from Europe and North Africa with Papillon–Lefèvre syndrome. J Invest Dermatol. 2001;117(6):1657–61. https://doi.org/10.1046/j.0022-202x.2001.01595.x.
Wani AA, Devkar N, Patole MS, Shouche YS. Description of two new cathepsin C gene mutations in patients with Papillon–Lefèvre syndrome. J Periodontol. 2006;77(2):233–7. https://doi.org/10.1902/jop.2006.050124.
Kobayashi T, Sugiura K, Takeichi T, Akiyama M. The novel CTSC homozygous nonsense mutation p.Lys106X in a patient with Papillon–Lefèvre syndrome with all permanent teeth remaining at over 40 years of age. Br J Dermatol. 2013;169(4):948–50. https://doi.org/10.1111/bjd.12429.
Kosem R, Debeljak M, Repič Lampret B, Kansky A, Battelino T, Trebušak PK. Cathepsin C gene 5’-untranslated region mutation in Papillon–Lefèvre syndrome. Dermatology. 2012;225(3):193–203. https://doi.org/10.1159/000342509.
Selvaraju V, Markandaya M, Prasad PV, Sathyan P, Sethuraman G, Srivastava SC, et al. Mutation analysis of the cathepsin C gene in Indian families with Papillon–Lefèvre syndrome. BMC Med Genet. 2003;4:5. https://doi.org/10.1186/1471-2350-4-5.
Wu W, Chen B, Chen X, Chen L, Yi L, Wang Y, et al. A novel large deletion combined with a nonsense mutation in a Chinese child with Papillon–Lefèvre syndrome. J Periodontal Res. 2016;51(3):376–80. https://doi.org/10.1111/jre.12317.
Wang X, Liu Y, Liu Y, Dong G, Kenney EB, Liu Q, et al. Long-term change of disease behavior in Papillon–Lefèvre syndrome: Seven years follow-up. Eur J Med Genet. 2015;58(3):184–7. https://doi.org/10.1016/j.ejmg.2014.12.003.
Wang Y, Zhang H, Feng S. Novel compound heterozygous mutations in CTSC Gene in a Chinese family with Papillon–Lefevre syndrome. Ann Dermatol. 2021;33(4):369–72. https://doi.org/10.5021/ad.2021.33.4.369.
Wen X, Wang X, Duan X. High immunoglobulin E in a Chinese Papillon–Lefèvre syndrome patient with novel compound mutations of cathepsin C. J Dermatol. 2012;39(7):664–5. https://doi.org/10.1111/j.1346-8138.2011.01474.x.
Li X, Zhang X, Zhang J, Chen Y. Mutational analysis of the cathepsin C gene in a family of Han nationality with Papillon-Lefevre syndrome. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2008;25(5):502–5.
Li Z, Liu J, Fang S, Zhu H, Zhang X, Cai J, et al. Novel compound heterozygous mutations in CTSC gene cause Papillon–Lefèvre syndrome with high serum immunoglobulin E. J Dermatol Sci. 2014;76(3):258–60. https://doi.org/10.1016/j.jdermsci.2014.09.009.
Hayashi M, Nakano H, Sawamura D, Suzuki T. Japanese case of Papillon–Lefèvre syndrome with novel compound heterozygous mutations. J Dermatol. 2020;47(8):e293–5. https://doi.org/10.1111/1346-8138.15412.
Yuanjiao C, Chen-Jun L. Gene mutational analyses of the cathepsin C gene in families with Papillon–Lefèvre syndrome. Hua Xi Kou Qiang Yi Xue Za Zhi. 2016;34(4):346–9. https://doi.org/10.7518/hxkq.2016.04.005.
Hart PS, Pallos D, Zhang Y, Sanchez J, Kavamura I, Brunoni D, et al. Identification of a novel cathepsin C mutation (p.W185X) in a Brazilian kindred with Papillon–Lefèvre syndrome. Mol Genet Metab. 2002;76(2):145–7. https://doi.org/10.1016/S1096-7192(02)00031-8.
Moura AL, Regateiro FS, Peres Resende E, Coimbra Silva H, Gonçalo M, Todo Bom A, et al. A new terminal nonsense mutation of the cathepsin C gene in a patient with atypical Papillon-Lefèvre syndrome. J Investig Allergol Clin Immunol. 2020;30(2):151–3.
Ghanei M, Abbaszadegan MR, Forghanifard MM, Aarabi A, Arab H. A novel mutation in the cathepsin C (CTSC) gene in Iranian family with Papillon-Lefevre syndrome. Clin Exp Dent Res. 2021;7(4):568–73. https://doi.org/10.1002/cre2.387.
Farkas K, Paschali E, Papp F, Vályi P, Széll M, Kemény L, et al. A novel seven-base deletion of the CTSC gene identified in a Hungarian family with Papillon–Lefèvre syndrome. Arch Dermatol Res. 2013;305(5):453–5. https://doi.org/10.1007/s00403-013-1323-z.
Schackert HK, Agha-Hosseini F, Görgens H, Jatzwauk M, von Kannen S, Noack B, et al. Complete homozygous deletion of CTSC in an Iranian family with Papillon–Lefèvre syndrome. Int J Dermatol. 2014;53(7):885–7. https://doi.org/10.1111/j.1365-4632.2012.05769.x.
Hart TC, Hart PS, Michalec MD, Zhang Y, Marazita ML, Cooper M, et al. Localisation of a gene for prepubertal periodontitis to chromosome 11q14 and identification of a cathepsin C gene mutation. J Med Genet. 2000;37(2):95–101. https://doi.org/10.1136/jmg.37.2.95.
Fardal Ø, Drangsholt E, Olsen I. Palmar plantar keratosis and unusual periodontal findings. J Clin Periodontol. 1998;25(2):181–4. https://doi.org/10.1111/j.1600-051X.1998.tb02425.x.
Brown RS, Hays GL, Flaitz CM, O’Neill PA, Abramovitch K, White RR. A possible late onset variation of Papillon–Lefèvre syndrome: report of 3 cases. J Periodontol. 1993;64(5):379–86. https://doi.org/10.1902/jop.1993.64.5.379.
Dai J, Liu J, Zhang Q, An Y, Xia B, Wan C, et al. Cathepsin C is involved in macrophage M1 polarization via p38/MAPK pathway in sudden cardiac death. Cardiovasc Ther. 2021;2021:6139732. https://doi.org/10.1155/2021/6139732.
Roberts H, White P, Dias I, McKaig S, Veeramachaneni R, Thakker N, et al. Characterization of neutrophil function in Papillon–Lefèvre syndrome. J Leukoc Biol. 2016;100(2):433–44. https://doi.org/10.1189/jlb.5A1015-489R.
Bullón P, Castejón-Vega B, Román-Malo L, Jimenez-Guerrero MP, Cotán D, Forbes-Hernandez TY, et al. Autophagic dysfunction in patients with Papillon–Lefèvre syndrome is restored by recombinant cathepsin C treatment. J Allergy Clin Immunol. 2018;142(4):1131-43.e7. https://doi.org/10.1016/j.jaci.2018.01.018.
Klionsky DJ, Abdelmohsen K, Abe A, Abedin MJ, Abeliovich H, Acevedo Arozena A, et al. Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy. 2016;12(1):1–222. https://doi.org/10.1080/15548627.2015.1100356.
Boya P, Kroemer G. Lysosomal membrane permeabilization in cell death. Oncogene. 2008;27(50):6434–51. https://doi.org/10.1038/onc.2008.310.
Sadik CD, Noack B, Schacher B, Pfeilschifter J, Mühl H, Eickholz P. Cytokine production by leukocytes of Papillon–Lefèvre syndrome patients in whole blood cultures. Clin Oral Investig. 2012;16(2):591–7. https://doi.org/10.1007/s00784-011-0532-0.
McCarthy C, Reeves EP, McElvaney NG. The role of neutrophils in alpha-1 antitrypsin deficiency. Ann Am Thorac Soc. 2016;13(Suppl 4):S297-304. https://doi.org/10.1513/AnnalsATS.201509-634KV.
Korkmaz B, Lesner A, Marchand-Adam S, Moss C, Jenne DE. Lung protection by cathepsin c inhibition: a new hope for COVID-19 and ARDS? J Med Chem. 2020;63(22):13258–65. https://doi.org/10.1021/acs.jmedchem.0c00776.
Fassan M, Collesei A, Angerilli V, Sbaraglia M, Fortarezza F, Pezzuto F, et al. Multi-design differential expression profiling of COVID-19 lung autopsy specimens reveals significantly deregulated inflammatory pathways and SFTPC impaired transcription. Cells. 2022;11(6):1011. https://doi.org/10.3390/cells11061011.
Khaket TP, Singh MP, Khan I, Bhardwaj M, Kang SC. Targeting of cathepsin C induces autophagic dysregulation that directs ER stress mediated cellular cytotoxicity in colorectal cancer cells. Cell Signal. 2018;46:92–102. https://doi.org/10.1016/j.cellsig.2018.02.017.
Zhang GP, Yue X, Li SQ. Cathepsin C interacts with TNF-α/p38 MAPK signaling pathway to promote proliferation and metastasis in hepatocellular carcinoma. Cancer Res Treat. 2020;52(1):10–23. https://doi.org/10.4143/crt.2019.145.
Ikenoue T, Hong S, Inoki K. Monitoring mammalian target of rapamycin (mTOR) activity. Methods Enzymol. 2009;452:165–80. https://doi.org/10.1016/s0076-6879(08)03611-2.
Xiao Y, Cong M, Li J, He D, Wu Q, Tian P, et al. Cathepsin C promotes breast cancer lung metastasis by modulating neutrophil infiltration and neutrophil extracellular trap formation. Cancer Cell. 2021;39(3):423-37.e7. https://doi.org/10.1016/j.ccell.2020.12.012.
Joyce JA, Hanahan D. Multiple roles for cysteine cathepsins in cancer. Cell Cycle. 2004;3(12):1516–619. https://doi.org/10.4161/cc.3.12.1289.
Gocheva V, Zeng W, Ke D, Klimstra D, Reinheckel T, Peters C, et al. Distinct roles for cysteine cathepsin genes in multistage tumorigenesis. Genes Dev. 2006;20(5):543–56. https://doi.org/10.1101/gad.1407406.
Gocheva V, Joyce JA. Cysteine cathepsins and the cutting edge of cancer invasion. Cell Cycle. 2007;6(1):60–4. https://doi.org/10.4161/cc.6.1.3669.
Folkerts H, Hilgendorf S, Vellenga E, Bremer E, Wiersma VR. The multifaceted role of autophagy in cancer and the microenvironment. Med Res Rev. 2019;39(2):517–60. https://doi.org/10.1002/med.21531.
Ruffell B, Affara NI, Cottone L, Junankar S, Johansson M, DeNardo DG, et al. Cathepsin C is a tissue-specific regulator of squamous carcinogenesis. Genes Dev. 2013;27(19):2086–98. https://doi.org/10.1101/gad.224899.113.
Khaket TP, Singh MP, Khan I, Kang SC. In vitro and in vivo studies on potentiation of curcumin-induced lysosomal-dependent apoptosis upon silencing of cathepsin C in colorectal cancer cells. Pharma Res. 2020;161: 105156. https://doi.org/10.1016/j.phrs.2020.105156.
Kim S, Lee SI, Kim N, Joo M, Lee KH, Lee MW, et al. Decursin inhibits cell growth and autophagic flux in gastric cancer via suppression of cathepsin C. Am J Cancer Res. 2021;11(4):1304–20.
Jerke U, Eulenberg-Gustavus C, Rousselle A, Nicklin P, Kreideweiss S, Grundl MA, et al. Targeting cathepsin C in PR3-ANCA vasculitis. J Am Soc Nephrol. 2022;33(5):936–47. https://doi.org/10.1681/asn.2021081112.
Jerke U, Eulenberg-Gustavus C, Rousselle A, Kreideweiss S, Grundl M, Eickholz P, et al. Characterization of cathepsin C as a treatment targent in anca-associated vasculitis. Rheumatology. 2019;58(Suppl_2):kez061.11. https://doi.org/10.1093/rheumatology/kez061.011.
Kain R, Nackenhorst MC. A view on cathepsin C as a target for therapy in AAV. J Am Soc Nephrol. 2022;33(5):875–8. https://doi.org/10.1681/asn.2022030309.
Beertsen W, Willenborg M, Everts V, Zirogianni A, Podschun R, Schröder B, et al. Impaired phagosomal maturation in neutrophils leads to periodontitis in lysosomal-associated membrane protein-2 knockout mice. J Immunol. 2008;180(1):475–82. https://doi.org/10.4049/jimmunol.180.1.475.
Kumar A, Avishay DM, Jones CR, Shaikh JD, Kaur R, Aljadah M, et al. Sudden cardiac death: epidemiology, pathogenesis and management. Rev Cardiovasc Med. 2021;22(1):147–58. https://doi.org/10.31083/j.rcm.2021.01.207.
Osman J, Tan SC, Lee PY, Low TY, Jamal R. Sudden Cardiac Death (SCD)—risk stratification and prediction with molecular biomarkers. J Biomed Sci. 2019;26(1):39. https://doi.org/10.1186/s12929-019-0535-8.
Myerburg RJ, Junttila MJ. Sudden cardiac death caused by coronary heart disease. Circulation. 2012;125(8):1043–52. https://doi.org/10.1161/circulationaha.111.023846.
Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116(12):1887–906. https://doi.org/10.1161/circresaha.116.304521.
Herías V, Biessen EA, Beckers C, Delsing D, Liao M, Daemen MJ, et al. Leukocyte cathepsin C deficiency attenuates atherosclerotic lesion progression by selective tuning of innate and adaptive immune responses. Arterioscler Thromb Vasc Biol. 2015;35(1):79–86. https://doi.org/10.1161/atvbaha.114.304292.
Koike M, Shibata M, Ezaki J, Peters C, Saftig P, Kominami E, et al. Differences in expression patterns of cathepsin C/dipeptidyl peptidase I in normal, pathological and aged mouse central nervous system. Eur J Neurosci. 2013;37(5):816–30. https://doi.org/10.1111/ejn.12096.
Liang J, Li N, Zhang Y, Hou C, Yang X, Shimizu T, et al. Disinhibition of cathepsin C caused by cystatin F deficiency Aggravates the demyelination in a cuprizone model. Front Mol Neurosci. 2016;9:152. https://doi.org/10.3389/fnmol.2016.00152.
Zhao X, Liu S, Yang X, Liu Y, Liu G, Fan K, et al. Cathepsin C aggravates neuroinflammation via promoting production of CCL2 and CXCL2 in glial cells and neurons in a cryogenic brain lesion. Neurochem Int. 2021;148: 105107. https://doi.org/10.1016/j.neuint.2021.105107.
Miller BE, Mayer RJ, Goyal N, Bal J, Dallow N, Boyce M, et al. Epithelial desquamation observed in a phase I study of an oral cathepsin C inhibitor (GSK2793660). Br J Clin Pharmacol. 2017;83(12):2813–20. https://doi.org/10.1111/bcp.13398.
Stojkovska Docevska M, Novinec M. Cathepsin C: structure, function, and pharmacological targeting. Rare Dis Orphan Drugs J. 2023. https://doi.org/10.20517/rdodj.2023.09.
Korkmaz B, Lamort A-S, Domain R, Beauvillain C, Gieldon A, Yildirim AÖ, et al. Cathepsin C inhibition as a potential treatment strategy in cancer. Biochem Pharmacol. 2021;194: 114803. https://doi.org/10.1016/j.bcp.2021.114803.
Wei H, Wee LWY, Born B, Seang S, Koh MJA, Yee R, Lin G, Rafi'ee K, Mey S, Tan EC. Palmoplantar keratoderma, oral involvement, and homozygous CTSC mutation in two brothers from Cambodia. Am J Med Genet A. 2020;182(2):296–302. https://doi.org/10.1002/ajmg.a.61447.
Acknowledgements
LS was supported by Chulalongkorn University, second century high potential professoriate fund at the Faculty of Dentistry.
Funding
This study was funded by the Ratchadapisek Sompoch Endowment Fund (2023), Chulalongkorn University (Meta_66_005_3200_002), Thailand Science Research and Innovation Fund Chulalongkorn University, Health Systems Research Institute (66–101), National Research Council of Thailand (N42A650229), and Faculty of Dentistry, Chulalongkorn University (DRF67_012). The funding body had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
CC, NS: investigation, data interpretation, drafting the manuscript. KS, TT, FBPJ: data collection and analyses. LS: Writing—critical review, writing and editing. TP; conception, design, data analysis, drafting the manuscript. All authors critically revised the manuscript, gave their final approval, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chitsamankhun, C., Siritongtaworn, N., Fournier, B.P.J. et al. Cathepsin C in health and disease: from structural insights to therapeutic prospects. J Transl Med 22, 777 (2024). https://doi.org/10.1186/s12967-024-05589-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-024-05589-7