Abstract
Background
Hearing loss has been shown to be a risk factor for psychiatric disorders. In addition, long-term hearing loss is associated with increased hospitalization and mortality rates; however, the increased risk and duration of effect of hearing loss in combination with other chronic diseases on each psychiatric disorder are still not clearly defined. The purpose of this article is to clarify the risk of hearing loss for each disorder over time.
Methods
This was a retrospective cohort study, and a national health insurance research database in Taiwan was utilized. All (n = 1,949,101) Taiwanese residents who had a medical visit between 2000 and 2015 were included. Patients with hearing loss and a comparative retrospective cohort were analyzed. Every subject was tracked individually from their index date to identify the subjects who later received a diagnosis of a psychiatric disorder. The Kaplan‒Meier method was used to analyze the cumulative incidence of psychiatric disorders. Cox regression analysis was performed to identify the risk of psychiatric disorders.
Results
A total of 13,341 (15.42%) and 31,250 (9.03%) patients with and without hearing loss, respectively, were diagnosed with psychiatric disorders (P < 0.001). Multivariate analysis indicated that hearing loss significantly elevated the risk of psychiatric disorders (adjusted HR = 2.587, 95% CI 1.723–3.346, p < 0.001).
Conclusion
Our findings indicate that patients with hearing loss are more likely to develop psychiatric disorders. Furthermore, the various psychiatric disorders are more likely to occur at different times. Our findings have important clinical implications, including a need for clinicians to implement early intervention for hearing loss and to pay close attention to patients’ psychological status.
Trial registration TSGHIRB No. E202216036.
Similar content being viewed by others
Background
Hearing loss is a serious medical problem, and some types of hearing loss are irreversible [1]. According to the WHO, there are 538 million people with hearing loss worldwide [2], which is an average of one out of every 16 people. These patients face additional challenges in their daily lives, such as communication difficulties at work and at home, thus necessitating lifestyle changes. At the same time, people with hearing loss are at an increased risk of accidents (e.g., work-related, leisure-related) in their daily lives [3]. In clinical practice, most physicians assess patients in a relatively quiet environment, which is not comparable to patients' typical everyday surroundings; therefore, physicians cannot accurately assess the severity of hearing impairment in patients [4].
Psychiatric disorders have a tremendous impact on society. In addition to affecting the ability to work [5], they also have a negative impact on health [6]. However, if promptly managed, potential irreversible damage can be avoided [7,8,9]. Cognitive decline is also an issue in today's aging society. As cognitive decline progresses, some patients may develop dementia, and the subsequent medical care will become a great burden on the family, society, and medical institutions.
Long-term hearing loss not only increases the risk of depression, bipolar disorder, and cognitive decline but also increases hospitalization and mortality rates [10]. However, these articles only examine the relationship between a single disease and hearing loss. Furthermore, no research articles examine the relationship between hearing loss and multiple psychiatric disorders. Given the need for extensive population-based studies published on the risk of psychiatric disorders after hearing loss with a long-term follow-up, there is a clear gap in knowledge in this respect. Therefore, the purpose of this study is to analyze the risk of hearing loss for each psychiatric disorder by using large-scale study data from the National Health Insurance Research Database (NHIRD) in Taiwan.
Methods
Data source
In Taiwan, the National Health Insurance Program (NHIP) was launched on March 1, 1995, and currently provides over 99% coverage. The National Health Insurance Research Database (NHIRD) includes Taiwan's outpatient, emergency, and inpatient data. Under the policy, patients pay only a small portion of their medical costs, and hospitals rely on the data to request the remaining costs from insurance companies. If researchers want to use data from that database, they must pass a comprehensive review by a peer review committee. Research projects are approved by the Institutional Review Board at the TSGH. (TSGHIRB No. E202216036).
Sample definition
In our study, we enrolled all patients with hearing impairment (ICD-9-CM: 389). Events with more than three visits, a diagnosed psychiatric disorder (ICD-9-CM: 290-319), and chronic disease were followed up. To minimize bias, we excluded patients with hearing impairment before 2000, events that occurred before follow-up, and patients of unknown sex. All study participants were followed up from the index date until the diagnosis of psychiatric disorders. Poor prognosis in this article was used as a collective term for psychiatric disorders, suicide or all-cause mortality, the details of which are listed in Additional file 1: Table S1.
To clarify the risk of psychiatric disorders for each age group, we divided the population into four groups: under 19 years old, 20 to 44 years old, 45 to 64 years old, and 65 years old and above. For the income classification (since premiums are correlated with income), we divided the same sample into three groups: those with premiums below 18,000 (NTD), those with premiums between 18,000 and 34,999, and those above 35,000 (NTD).
In addition, multisystem disease comorbidity may cause greater mental stress, so we listed the risks associated with systemic disease comorbidity. Based on the industrial structure and population density of each region, the degree of urbanization was classified into four levels; the regions were grouped into northern, central, southern, eastern, and outlying islands; and the hospitals were classified into regional hospitals, county hospitals and medical centers. Finally, to compare seasonal differences, we also categorized patients by the season when they were diagnosed with the disease.
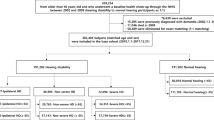
Figure 1 illustrates the design of our study, including the criteria for inclusion and exclusion. There were outpatient and inpatient data for 1,949,101 patients from January 1, 2000, to December 31, 2015, of whom 95,336 were diagnosed with hearing loss. Patients excluded were those with hearing loss prior to 2000 and those of unknown sex or age. In addition, those who had a psychiatric disorder before the diagnosis of hearing loss were also excluded. The final case group totaled 86,522 individuals. The same exclusion criteria were used for the control group as was used for the case group, and no hearing loss occurred during the study period. The control group, which included 346,088 individuals, was composed of four individuals per case-patient who were matched by index year, index month, sex, and age. These subjects were tracked through December 31, 2015 (Fig. 1).
Statistical analysis
For categorical variables, frequencies and percentages were used, while for continuous variables, mean and standard deviation were used. To further compare the variations between the hearing loss and non-hearing loss groups at baseline and at the tracking endpoint, the X2 test and Mann‒Whitney U test (Wilcoxon rank-sum test) were utilized. The Kaplan–Meier method was used to estimate the difference in the risk of hearing loss between the study and observation groups, and a log-rank test was used to evaluate the difference between the groups in terms of the occurrence of cumulative hearing loss. The risk of psychiatric disorders was determined using multivariate Cox proportional hazards regression analysis, and the results were expressed as crude and adjusted hazard ratios (HRs) and 95% confidence intervals (CIs). The formula for the Cox regression analysis is as follows: for “crude HR”, Y (dependent variable) is poor prognosis, and X (independent variable) is each individual variable in the table (one Y corresponds to one X); for “adjusted HR”, Y (dependent variable) is poor prognosis, and X (independent variable) is all the variables in the table (one Y corresponds to multiple X). SAS 9.1 (SAS, Cary, NC) was used for the Schoenfeld residuals test. SPSS 22.0 (IBM, Armonk, NY) was used for all other statistical calculations, and a double-tailed p value of 0.05 was taken as the significant level.
Results
The hearing loss group and the control group included 86,522 and 346,088 cases, respectively. Table 1 shows the demographic variables, psychiatric disorders, and other comorbidities for the hearing loss and control groups. There were no statistically significant differences in sex distribution between the hearing loss and control groups (p value: 0.999). In terms of psychiatric disorders, there was a significant difference in hearing loss compared to the control group (hearing loss group: 15.42%; control group: 9.03%; p value < 0.001). Regarding the demographic variables, in the age distribution, the majority of patients with hearing loss were younger than 19 years and older than 65 years (≦ 19: 33.63%; ≧ 65: 29.72%). The distribution of income was mostly concentrated in the group with a monthly income of less than NT$18,000 (< 18,000NT: 81%), but the distribution was relatively equal in terms of region and urbanization. The distribution of the population in terms of medical institutions increases from regional hospitals to medical centers. For other comorbidities, the hearing loss group had the highest rate in the injury group (injury: 21.84), followed by chronic diseases such as diabetes, hypertension, and kidney disease.
Table 2 shows the results of the Cox regression analysis for the risk of psychiatric disorders in the hearing loss group compared to the nonhearing-loss control group. The adjusted HR was 2.587 (95% CI 1.723–3.346, p < 0.001). The results showed that patients with hearing loss had a 2.587-fold higher risk of developing psychiatric disorders than those without hearing loss. Hearing loss had the highest adjusted HR relative to other items. We conducted a Schoenfeld residuals test based on the literature [11]. The global test for an adjusted HR showed a p value of 0.7941. The p value was not significant, indicating that the assumptions of Cox regression were satisfied [11]. We also performed an omnibus test of the Cox model for the adjusted HR, and the p value was significant, indicating that the model was reliable.
Table 3 compares “hearing loss or not” with the other variables in the reference table. Regarding the demographic variables, the risk of psychiatric disorders increased with age in the hearing loss group compared to the control group, and a similar pattern was observed for the urbanization and level of medical facility categories. In the winter subgroup of the hearing loss group, the risk of psychiatric disorders was 2.62-fold higher than that of the nonhearing-loss group. In the comorbidity subgroup, having other comorbidities slightly increased the risk of psychiatric disorders in the hearing loss group. For example, in the group without diabetes, the hearing loss group had a 2.57-fold risk of psychiatric disorders in the nonhearing-loss group, and their risk increased to 2.66-fold if they had diabetes.
Additional file 2: Table S3 classifies patients with hearing loss. There are two groups, the first being diagnoses made by otolaryngologists and the second being diagnoses made by other specialists. Other specialists included those in the fields of family medicine, emergency medicine and pediatrics. The two groups with hearing loss both have a similar chance of having psychiatric disorders.
Table 4 presents the subgroups of psychiatric disorders, and we list the common diagnoses, such as depression, bipolar disorder, or PTSD.
Three models are presented: the first model is without restrictions, and the remaining two models excluded patients with hearing loss who are diagnosed with a psychiatric disorder within the first year of follow-up and within the first five years of follow-up. This was used to differentiate the impact of each period, as shown in Additional file 3: Table S4.
The risk of PTSD/ASD was highest in the first two groups (HR ratio: 3.371 and 3.253) but was not statistically significant in the third group (p value: 0.101), which meant that it had a medium-term impact. The second highest risk was for depression and anxiety, which was statistically significant in all groups.
Discussion
This is the first pilot study to define explicit risk associations between hearing loss and psychiatric disorders utilizing a large national population. Based on subgroup analysis, we also identified the most common psychiatric disorders caused by hearing loss, with the highest to lowest rates ranked as post-traumatic stress syndrome (PTSD), depression, and anxiety disorders. In this study, we provide more detailed information on the risk of psychiatric disorders in patients with hearing loss. For health care professionals, better health care plans can be developed, and for public health workers, more comprehensive social welfare programs can be established to reduce overall health care costs.
In Table 2, we list the risk factors for psychiatric disorders and calculate the hazard ratio. Compared to other comorbidities and demographic variables, hearing loss had the highest risk of developing psychiatric disorders. In Table 3, we compare the effects of different conditions on the hearing loss group. The risk of psychiatric disorders in the hearing loss group was found to increase with age. The elderly group’s hazard ratio was greater than that of the younger group (2.610 and 2.555). This could be related to other comorbidities. Systemic diseases are already a stressor for psychiatric disorders [12], and hearing loss is also considered a stressor [4], so a higher risk can be expected when both disorders are present, and this hypothesis is confirmed by our statistical data. In addition, the effect of seasonal changes on patients with hearing loss can be explained by seasonal affective disorder. Psychiatric disorders are more likely to develop in the winter [13], and this is no exception in the hearing loss community. In Additional file 2: Table S3, an additional test was conducted due to concerns about possible discrepancies in the diagnosis of hearing loss between doctors in different specialties, but the results did not appear to be significantly different.
In compiling the data, we found a phenomenon: the more urbanized the patient was, the higher the risk of developing psychiatric disorders. Another study supports our findings [14]. We believe this is because urban living requires more effective communication. This means that patients with hearing loss need to be fully attentive to every message they receive, which inevitably stresses patients with hearing loss. In Taiwan, most medical centers are in highly urbanized areas, where they receive more patients with hearing loss and more complex diseases. As a result, patients at medical centers have a higher risk of developing psychiatric disorders after follow-up visits (adjusted HR = 2.630). Patients in medical centers usually have more complicated medical problems.
Scholars have confirmed that hearing loss is a risk factor for psychiatric disorders [4] and that it also contributes to cognitive decline [15]. We make inferences about this observation, which can be divided into two main categories: psychological and physical. Psychologically, hearing loss is stressful for patients who need to compensate for their hearing deficits by reading lips. Furthermore, since the COVID-19 outbreak, the public has been wearing masks, which makes it more difficult for patients with hearing loss to understand the verbal communication of others [16]. Despite the fact that hearing aids have been shown to be effective in lowering the incidence of psychiatric disorders, there is still a gap when compared to the general population, most likely due to the noticeable appearance of hearing aids and poor sound recognition [17]. Additionally, when patients with hearing loss suffer from psychiatric disorders, they are unable to communicate effectively with physicians in psychiatric outpatient clinics because most physicians are not proficient in sign language. Therefore, a third person who understands sign language is usually needed to relay the message, but this may distort the message and make it difficult for the physician to have a more accurate handle on the condition. Physiologically, studies have shown that when a patient suffers from hearing loss, there are changes in the volume of relevant areas of the brain, causing the surrounding brain tissue to be affected and eventually causing cognitive impairment [18, 19]. This progression is very slow, and by the time psychiatric symptoms appear, a significant amount of brain tissue has already atrophied.
The Kaplan‒Meier method for long-term follow-up of cumulative risk of psychiatric disorders had a statistically significant log-rank (p < 0.001) (Fig. 2). In our study, patients with hearing loss may have developed symptoms slowly over time, in addition to psychiatric symptoms in the short term.
In our event subgroup analysis, we found that patients had the highest risk of ASD and PTSD within the first five years of diagnosis (adjusted HR = 3.371). We also found other articles that supported our data and hypothesis [20] that acquired hearing loss may result in ASD or PTSD symptoms, as well as underlying stressful pre-existing relationship breakdowns, job failures, or an inability to adapt. In the long term, the risk of anxiety and depression is more than three times greater in these patients. Charlene J. Crump et al. showed that patients with hearing loss were often unable to communicate effectively with their psychiatrists during long-term local follow-up visits, which then affected their judgment and treatment, leading to a worsening of their disease [21]. Age, chronic disease, sensory stimulation loss, e.g., hearing loss, and other variables can all contribute to cognitive decline. The use of cochlear implants [22] or hearing aids [23] can significantly decrease cognitive decline, improving the elderly's capacity for self-care [24] and lowering the cost of long-term care services.
In addition to evaluating the use of hearing aids or cochlear implants, we recommend that clinicians working with patients who are diagnosed with hearing loss briefly assess the patient’s cognitive and mental status at the outpatient follow-up visit. If psychiatric disorders are suspected, early consultation with a neurologist or psychiatrist for evaluation and treatment is indicated. Some hearing losses, such as age-related hearing loss, progress over time [25]. This means that the sooner a psychiatrist is involved, the better the patient's chances of communicating effectively with him or her.
More importantly, in the public health context, this study provides a more accurate risk ratio than other studies, which can be used to predict the number of patients with psychiatric disorders in the future, as well as to assess the budget for subsidies, such as reducing the cost of hearing aids, cochlear implants, auditory brainstem implants, or sign language education. The strength of this study is mainly in the large sample size obtained from our national database to statistically determine the relative risk, as no previous large-scale study has statistically determined the risk ratio of hearing loss for each psychiatric disorder. In addition, the long-term follow-up made it possible to analyze short-, medium-, and long-term effects at the same time.
However, there are still limitations to this study. First, there is no detailed information on the severity of hearing loss. There is no way to specify the progress of each patient with psychiatric disorders. In other words, we cannot know whether hearing loss is a key incident in the development of psychiatric disorders. It may be that a patient has symptoms of a psychiatric disorder prior to hearing loss but has not been diagnosed. However, this can be minimized by extending the follow-up years to exclude the first year or the first 5 years. Statistically significant differences were seen for most of the subgroups (p value < 0.001). Second, these tables do not include medications other than those used for hearing loss. For example, proton pump inhibitors can lead to depression in some patients with specific physical conditions [26], but we believe that this has very little impact on the results of the study because the percentage of people is small and the condition can be cured by changing the medication. Third, we were unable to perform an accurate sensitivity test to diagnose hearing loss. However, we conducted an additional test, shown in Additional file 2: Table S3, to compare patients with hearing loss diagnosed by otolaryngologists and other specialists who had a poor prognosis when followed up over time. The results were similar. Fourth, patients with each type of psychiatric disorder may have different backgrounds. Therefore, the impact of hearing loss on the development of each psychiatric disorder may be different. The potential mechanisms underlying individual responses remain to be further examined on a large scale.
Conclusions
This study with long-term follow-up demonstrated that hearing loss significantly increases the risk of developing psychiatric disorders and that the risk increases with age. Patients with hearing loss who also have other comorbidities are at a higher risk for psychiatric disorders. For this reason, we recommend that clinicians not overlook the clinical importance of these relationships. During outpatient hearing examinations, it is recommended to additionally assess the patient's cognitive and mental status and refer patients with low status to neurologists or psychiatrists.
Availability of data and materials
All the data underlying the present study are from the National Health Insurance Research Database (NHIRD). Researchers can obtain the data through formal application to the Ministry of Health and Welfare, Taiwan.
Abbreviations
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- PTSD:
-
Posttraumatic stress disorder
- CLD:
-
Chronic liver disease
- ASD:
-
Acute stress disorder
- SRD:
-
Substance-related disorder
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- PYs:
-
Person-years
References
Metidieri MM, Rodrigues HFS, de Oliveira FJMB, Ferraz DP, de Almeida Neto AF, Torres S. Noise-induced hearing loss (NIHL): literature review with a focus on occupational medicine. Int Arch Otorhinolaryngol. 2013;17:208–12.
Stevens G, Flaxman S, Brunskill E, Mascarenhas M, Mathers CD, Finucane M, et al. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Public Health. 2013;23:146–52.
Lin HW, Mahboubi H, Bhattacharyya N. Self-reported hearing difficulty and risk of accidental injury in US adults, 2007 to 2015. JAMA Otolaryngol Head Neck Surg. 2018;144:413–7.
Blazer DG, Tucci DL. Hearing loss and psychiatric disorders: a review. Psychol Med. 2019;49:891–7.
Lidwall U, Bill S, Palmer E, Olsson BC. Mental disorder sick leave in Sweden: a population study. Work. 2018;59:259–72.
Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859–77.
Vieta E, Salagre E, Grande I, Carvalho AF, Fernandes BS, Berk M, et al. Early intervention in bipolar disorder. Am J Psychiatry. 2018;175:411–26.
Cheng SC, Schepp KG. Early intervention in schizophrenia: a literature review. Arch Psychiatr Nurs. 2016;30:774–81.
McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. 2008;7:148–56.
Cunningham LL, Tucci DL. Hearing loss in adults. N Engl J Med. 2017;377:2465–73.
Abeysekera W, Sooriyarachchi M. Use of Schoenfeld’s global test to test the proportional hazards assumption in the Cox proportional hazards model: an application to a clinical study. J Natl Sci Found Sri Lanka. 2009. https://doi.org/10.4038/jnsfsr.v37i1.456.
Chen CM, Lee IC, Su YY, Mullan J, Chiu HC. The longitudinal relationship between mental health disorders and chronic disease for older adults: a population-based study. Int J Geriatr Psychiatry. 2017;32:1017–26.
Fonte A, Coutinho B. Seasonal sensitivity and psychiatric morbidity: study about seasonal affective disorder. BMC Psychiatry. 2021;21:1–7.
van der Werf M, van Winkel R, van Boxtel M, van Os J. Evidence that the impact of hearing impairment on psychosis risk is moderated by the level of complexity of the social environment. Schizophr Res. 2010;122:193–8.
Lin FR, Yaffe K, Xia J, Xue QL, Harris TB, Purchase-Helzner E, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173:293–9.
Atcherson SR, Mendel LL, Baltimore WJ, Patro C, Lee S, Pousson M, et al. The effect of conventional and transparent surgical masks on speech understanding in individuals with and without hearing loss. J Am Acad Audiolo. 2017;28:058–67.
McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol. 2013;52:360–8.
Rutherford BR, Brewster K, Golub JS, Kim AH, Roose SP. Sensation and psychiatry: linking age-related hearing loss to late-life depression and cognitive decline. Am J Psychiatry. 2018;175:215–24.
Lin FR, Ferrucci L, An Y, Goh JO, Doshi J, Metter EJ, et al. Association of hearing impairment with brain volume changes in older adults. Neuroimage. 2014;90:84–92.
Hallam R, Ashton P, Sherbourne K, Gailey L. Acquired profound hearing loss: mental health and other characteristics of a large sample. Int J Audiol. 2006;45:715–23.
Crump CJ, Hamerdinger SH. Understanding etiology of hearing loss as a contributor to language dysfluency and its impact on assessment and treatment of people who are deaf in mental health settings. Community Ment Health J. 2017;53:922–8.
Mosnier I, Bebear JP, Marx M, Fraysse B, Truy E, Lina-Granade G, et al. Improvement of cognitive function after cochlear implantation in elderly patients. JAMA Otolaryngol Head Neck Surg. 2015;141:442–50.
Sarant J, Harris D, Busby P, Maruff P, Schembri A, Lemke U, et al. The effect of hearing aid use on cognition in older adults: can we delay decline or even improve cognitive function? J Clin Med. 2020;9:254.
Lim Y-H, Baek Y, Kang SJ, Kang K, Lee H-W. Clinical application of the experimental ADL test for patients with cognitive impairment: pilot study. Sci Rep. 2021;11:1–8.
Gates GA, Mills JH. Presbycusis Lancet. 2005;366:1111–20.
Laudisio A, Antonelli Incalzi R, Gemma A, Giovannini S, Lo Monaco MR, Vetrano DL, et al. Use of proton-pump inhibitors is associated with depression: a population-based study. Int Psychogeriatr. 2018;30:153–9.
Acknowledgements
Not applicable.
Funding
Hung-Che Lin was supported, in part, by the Tri-Service General Hospital (TSGH-C108-198, TSGH-E-110266, TSGH-E-113222) and National Defense Medical Research grants, Taiwan, ROC (MND-MAB-D-113176). Wu-Chien Chien was supported by the Tri-Service General Hospital (TSGH-B-113025).
Author information
Authors and Affiliations
Contributions
Conceptualization, QYN, WCC and HCL; methodology, QYN, WCC and CHC; software, WCC and CHC; formal analysis, QYN, WCC and HCL; resources, WCC and HCL; writing—original draft preparation, QYN and HCL; writing—review and editing, QYN, WCC and HCL; supervision: CAC, CPS, CYK, HCC, YYL, JCL, CHW and LHC; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Institutional Review Board of the Tri-Service General Hospital (TSGHIRB No. E202216036).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Abbreviations, ICD-9-CM codes, and definitions.
Additional file 2: Table S3.
Factors of poor prognosis among different diagnosed department of hearing loss by using Cox regression and Bonferroni correction for multiple comparisons.
Additional file 3: Table S4.
Analysis of whether events had a short-, medium-, or long-term impact.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nian, QY., Cheng, CA., Cheng, LH. et al. Increased risk of psychiatric disorder in patients with hearing loss: a nationwide population-based cohort study. J Transl Med 22, 345 (2024). https://doi.org/10.1186/s12967-024-04992-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-024-04992-4