Abstract
The intestinal barrier is a complex structure that not only regulates the influx of luminal contents into the systemic circulation but is also involved in immune, microbial, and metabolic homeostasis. Evidence implicating disruption in intestinal barrier functions in the development of many systemic diseases, ranging from non-alcoholic steatohepatitis to autism, or systemic complications of intestinal disorders has increased rapidly in recent years, raising the possibility of the intestinal barrier as a potential target for therapeutic intervention to alter the course and mitigate the complications associated with these diseases. In addition to the disease process being associated with a breach in the intestinal barrier functions, patients with hematologic and oncologic diseases are particularly at high risks for the development of increased intestinal permeability, due to the frequent use of broad-spectrum antibiotics and chemoradiation. They also face a distinct challenge of being intermittently severely neutropenic due to treatment of the underlying conditions. In this review, we will discuss how hematologic and oncologic diseases are associated with disruption in the intestinal barrier and highlight the complications associated with an increase in the intestinal permeability. We will explore methods to modulate the complication. To provide a background for our discussion, we will first examine the structure and appraise the methods of evaluation of the intestinal barrier.
Similar content being viewed by others
Background
The gastrointestinal (GI) mucosal epithelium is one of the largest tissue systems that maintain constant interaction with the external environment. It forms an important physical and functional barrier separating the host internal milieu from potentially harmful and toxic entities. In addition to selectively controlling the traverse of luminal contents into the systemic circulation, GI mucosal epithelium also regulates adaptive immune responses. The physical barrier arisen from the GI mucosa is selectively permeable. It allows the absorption of nutrients and water but prevents the translocation of luminal bacteria and bacterial products into the host. The barrier may be disrupted due to mucosal injury, changes in cellular molecules, or dysregulated immune responses from autoimmune diseases.
Disruption of the intestinal barrier has been implicated in various disease states. They include inflammatory bowel disease [1], celiac disease [2], non-alcoholic steatohepatitis [3], diabetes mellitus [4], and autism [5]. It has been postulated that the tissue injury in these diseases is mediated by immune and non-immune responses to an uncontrolled influx of antigens and luminal bacterial products that occurs when the intestinal barrier is breached [6]. Although the pathogenetic effects of increased intestinal permeability has been widely discussed in many diseases, their roles in hematologic and oncologic diseases are less examined. There is a paucity of literature that explores how the disruption of intestinal barrier functions resulting from these conditions and/or their treatment impacts the disease phenotypes and complications experienced by the patients.
The intestinal barrier may, therefore, be a target for therapeutic approaches to alter the course and mitigate the complications associated with a disruption in its functions. In this paper, we will discuss how hematologic and oncologic diseases are associated with disruption in the intestinal barrier and explore the consequences of an increase in the intestinal permeability in these patients. We will also propose approaches to modulate this intestinal pathology. To do so, we will first provide an overview of the structure and methods of evaluation of the intestinal barrier as the background on which discussions on hematologic and oncologic diseases will be based.
Main text
Anatomy of the intestinal barrier
Intestinal barrier components
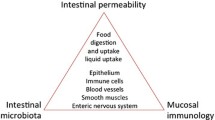
The intestinal barrier is broadly composed of three interactive layers (Fig. 1). The first layer is the luminal layer that consists of commensal microbes. These commensals inhibit the colonization of opportunistic and pathogenic microbial species. A balanced intestinal microbial community is essential for the maintenance of this layer of the barrier.
The three interactive layers of intestinal barrier. The luminal layer consists of the intestinal commensal organisms that spatially inhibit colonization of the intestine with pathogenic microbial species. The middle layer consists of mucus that prevents the contact of the mucosal epithelium with the intestinal micro-organisms. This mucus layer not only provides a physical barrier, it also contains antimicrobial proteins and IgA, both of which contribute further to protect the mucosal epithelium. The mucosal epithelium provides a selectively permeable barrier to the luminal contents
The second layer consists of unstirred water, glycocalyx and mucus. Secreted mucus mixes with antibacterial agents such as lysozyme, immunoglobulin A (IgA) and defensins produced by Paneth cells and enterocytes to confer a homeostatic environment. Enterocytes secrete transmembrane mucins that remains attached to the cell membrane and covers the apical surface for protection and sensing host-microbe interaction for innate immune response [7]. The more abundant and dynamic gel-forming mucin, mucin 2 (MUC 2), is produced by goblet cells [8]. The outer mucus layer is dynamic and has an abundance of microbes and microbial products, while the inner mucus layer remains attached to the epithelium and is more concentrated in secreted antimicrobial peptides that reduce antigen exposure to the underlying enterocytes. The mucus layer also protects the underlying epithelial layer from dehydration and mechanical stress, removes debris and microbes by flushing them away, and forms a diffusion barrier for the passage of ions, water, nutrients, and gases [9, 10]. Gut microbiota composition and mucus layer has a bidirectional interaction in which commensals promote mucus secretion and thickness, and pathogens degrade mucus.
The final component of the intestinal barrier is the epithelial layer. Enterocytes are connected by intercellular junctional complexes where tight junctions (TJs), adherens junctions and desmosomes regulate epithelial barrier function and transport. The Paneth cells in the epithelium produce defensins and other antimicrobial peptides. Underneath the epithelium, the lamina propria provides defense based on innate and acquired immunity cells such as dendritic cells, B-cells, T-cells and macrophages. Depletion of the mucus layer due to dysbiosis brings microbiota to close proximity of the epithelial cells. Pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) expressed on epithelial cells interact with microbiota-derived pathogen-associated-molecular patterns (PAMPs) such as lipopolysaccharide (LPS) to activate myeloid differentiation factor 88 (MYD88)-dependent signaling. In addition to PAMPs, damage-associated-molecular patterns (DAMPs) released from damaged intestinal epithelium interact with PRRs to facilitate macrophage- and dendritic cell-triggered inflammation. Dysbiosis can also lead to apical junction complex dysfunction. For example, excess growth of E. coli strain C25 increases gut permeability [11], spreading luminal content into the systemic circulation and triggering local and systemic immune response. Changes in intestinal microbiota in the form of increases in α-diversity and increase in the abundance of non-commensals or less dominant taxa correlate with an increased intestinal permeability [12].
Intestinal permeability
While epithelial cells are interconnected by the apical junction complex to create a barrier, the seal is not absolute. The intestinal barrier does permit the passage of selected luminal molecules via either the paracellular pathway or the transcellular pathway (Fig. 2).
Mechanisms of intestinal barrier functions. Traverse of intraluminal content occurs across tight junctions by two different routes termed pore and the leak pathways. The pore pathway is a high-capacity, charge-selective route that regulates the passage of small molecules less than 8 Å in diameter. The leak pathway is a low-capacity, non-charge selective route traversed by molecules up to 100 Å in diameter. When epithelial damage occurs, the tight junction-independent, size-nonselective, charge-nonselective unrestricted pathway becomes the dominant route of intestinal permeability
Paracellular pathway
The paracellular pathway provides the passage of luminal molecules between adjacent cells via TJs or intercellular spaces [13]. There are three distinct paracellular pathways: (1). The pore pathway, a high-conductance route, is charge- and size-selective (upper limit of 6 to 8 Å diameter) [13]; (2). The leak pathway, a lower conductance route, allows the movement of molecules with non-selective charge, upper size limit of ∼100 Å diameter [14]; and, (3). The unrestricted pathway, due to epithelial cell damage, is independent of TJs and allows for the pathologic flux of luminal content across the epithelium.
Pore pathway
Water, ions, and nutrients are transported via the pore pathway. TJ regulation of the pore pathway is dependent on various factors. Physiological Na+-glucose cotransport activation in intestinal epithelia enhances pore pathway permeability by activating the myosin light chain kinase (MLCK) [15]. Other modes of pore pathway regulation are governed by charge-selectivity and regulation of claudin 2 expression. Claudin 2 upregulation increases pore pathway permeability. Other members of the claudin family including 10a, 10b, 15, 16, and 17 also form either cation- or anion-selective channels [13]. Pore pathway permeability is sensitive to cytokine signaling. For example, interleukin 13 (IL-13) selectively induce claudin 2 expression to enhance pore pathway permeability [16].
Leak pathway
The specific site of leak pathway mediating macromolecular flux is considered to be the tricellular TJs [17]. Constitutively active MLCK expression increases leak pathway permeability [18]. Among the TJ proteins, occludin and ZO-1 are critical mediators of the leak pathway. MLCK-dependent occludin endocytosis via a caveolar process promotes leak pathway permeability [19]. Since ZO-1directly binds to F-actin [20] and the actin binding region of ZO-1 is required for barrier regulation by MLCK [21], ZO-1 downregulation or knockdown increases leak pathway permeability [22]. Among the cytokines, tumor necrosis factor (TNF) and IL-1β regulate leak pathway by promoting occludin endocytosis and MLCK activation [19, 23].
Unrestricted pathway
This pathway arises due to epithelial damage. This is the pathway for the translocation of luminal endotoxins, exotoxins, and intact enteric bacteria.
Transcellular pathway
Lipids and lipophilic substances cross the intestinal barrier via diffusion along the apical plasma membrane of enterocytes into the circulation by the transcellular pathway. In addition, large molecules, antigens and microbes can also pass through by endocytosis and transcytosis. Both endocytosis and transcytosis can be manipulated by microbes to establish their entry and translocation. M-cells in the epithelium can take up antigens and microbes by specific cell surface receptors. For example, GP2 receptor can identify specific antigens on the surface of microbes and initiate endocytosis, transcytosis, exocytosis, and engulfment by subepithelial dendritic cells [24, 25]. The goblet cell-associated antigen pathways can also aid in the internalization of endotoxins [26].
Intestinal permeability assessment in the clinics
Table 1 summarizes the methods available, primarily on a research basis, to study intestinal permeability in human and the obstacles associated with each of the methods. By far, the method most commonly used and widely available for assessing intestinal permeability in the clinic and outside the context of research is the lactulose: mannitol (L: M) test. This is a quantitative assay to measure the ability of these two non-metabolized sugar molecules to permeate the intestinal mucosa. Mannitol, a readily absorbed monomer, is absorbed and excreted in the urine while lactulose, a dimer, is only slightly-absorbed and serves as a marker for mucosal integrity [27]. An elevated L: M ratio is an indicator of intestinal barrier dysfunction. Despite being a non-invasive and quantitative method, studies have shown significant limitations in its use [28]. Other probes used include polyethylene glycol (PEG) and radioactive chromium complexed with ethylene diamine tetracetic acid (51Cr-EDTA).
Direct observation of intestinal barrier function may be achieved by confocal laser endomicroscopy (CLE). This is an endoscopic technique with excellent subcellular resolution and 400-fold magnification. The technique relies on injecting a fluorescein as a contrast agent to the patient and examining the cells and intracellular substance of the gastrointestinal tract mucosa during real-time endoscopy [29]. This has been applied successfully to study duodenal permeability in patients with acute pancreatitis [30], and in patients with inflammatory bowel disease [31]. However, its use is limited by the need for special training to perform the test. CLE is also not widely available currently.
Intestinal barrier function may also be examined by serum or plasma intestinal biomarkers. A number of serum markers can be used. Unfortunately, every marker denotes a different endpoint and significance. For example, intestinal fatty acid binding protein (iFABP), an enterocyte-derived protein, serves as a marker of mature enterocyte damage and ischemia [32]. On the other hand, serum measurement of zonulins, an integral part of the intercellular TJs, detects barrier disassembly and increased permeability [33]. Serum citrulline, an amino acid produced by small intestine enterocytes [34], reflects loss of small intestine mass. Finally, LPS measurement in serum or plasma, is elevated when the intestinal barrier is breached [35], but serum LPS is also increased during systemic inflammation and endotoxemia.
Different sizes of Fluorescein Isothiocyanate (FITC)-labeled dextran (dextran 4 k Da, dextran 70 k Da, or a combination of the two) have been used reproducibly for in vivo studies of intestinal permeability in the laboratory to differentiate between pore, leak and unrestricted pathways. This method has not been adapted for clinical evaluation.
Intestinal barrier disruption in hematologic diseases
Unlike diseases such as non-alcoholic steatohepatitis, inflammatory bowel disease, and autism that have been attributed to a primary breakdown in the intestinal barrier, the increased intestinal permeability associated with hematologic diseases is mostly secondary to the disease process. A compromised intestinal barrier increases the risk of complications in these patients. In this section, we will examine several hematologic diseases in which intestinal barrier functions are disrupted and discuss the clinical consequences of this pathology.
Sickle cell disease
In the last few years, the integrity of the intestinal barrier has been aggressively investigated in sickle cell disease (SCD), a genetic disorder of mutation, that results from a mutation of the β-globin gene, and renders the sickle hemoglobin (HbS) to polymerization upon deoxygenation, promoting sickling of erythrocytes carrying the HbS. The end-result of the event is the adherence of the sickle erythrocytes to activated leukocytes immobilized on the endothelium, causing microvascular occlusion, vaso-occlusive crisis (VOC), and tissue ischemia. VOC, when involving the splanchnic vasculature, damages the intestinal epithelium [36], as indicated by the elevated serum iFABP levels in SCD [37, 38], and increased intestinal permeability. The local hypoxemia may also be responsible for the altered intestinal microbial composition in SCD [39]. SCD patients exhibit increased abundance of Veillonella that correlated with the frequency of VOC [40], and reduced Alistipes and Pseudobutyrivibrio [41], that are producers of short-chain fatty acids (SCFAs) needed for intestinal health. Intestinal microbial density is also increased in SCD [38, 42]. Changes in bacterial composition and density exacerbate the intestinal injury induced by VOC.
As a result of a breach in the intestinal barrier, SCD patients may experience a vicious cycle of VOC [43]. The increased intestinal permeability allows for the traverse of bacterial products across the barrier to stimulate and activate cellular components that participate in VOC. Not only do SCD patients have higher leukocyte counts [44] and serum biomarkers of neutrophil activation, such as CD64 [45], CD11b/CD18 [46], and CD62L [37, 45, 46] compared to non-SCD individuals, their monocytes [47] and platelets [48] are also activated. Furthermore, circulating aged neutrophils (CANs), a subset of neutrophils with high surface expression of CXCR4 and low CD62L and participate in the VOC process, are also higher in SCD [37, 45, 49]. CANs are regulated by intestinal microbiota [49] through interaction with PAMPs via TLR 2/4 and MYD88 [50, 51]. The direct contact needed for this interaction support the pathogenetic role of increased intestinal permeability in contributing to VOC in SCD.
Thalassemias
Thalassemias are a group of inherited disorders of the α-globin gene cluster or the β-globin gene cluster involved in Hb synthesis. As a result, ineffective erythropoiesis with subsequent anemia occurs. The primary pathology inciting intestinal mucosal injury is iron overload due to an increased intestinal iron absorption signaled by ineffective erythropoiesis and/or from repeated blood transfusions. Undesired amount of epithelial cell shedding occurs during iron elimination, triggering mucosal permeability [52]. Metabolism of non-transferrin bound iron produces reactive oxygen species that contributes to the cellular dysfunction and apoptosis of enterocytes [53] and results in damage to the TJ complexes and leakage of LPS and (1 → 3)-β-d-glucan (BG), a major component of the fungal cell wall into the circulation [54]. This triggers a hyperinflammatory reaction with the activation of neutrophils and macrophages [55], which may inflict further damage to the intestinal mucosa. The clinical consequences are increased incidence of septicemia and other severe bacterial infections in these patients [56,57,58].
Human immunodeficiency virus (HIV) infection
Patients with HIV infections are at higher risks for the development of multiple comorbidities, including cardiovascular and liver diseases [59]. This is believed to be related to chronic immune activation caused by increased microbial translocation from a leaky intestine [60]. Intestinal pathology in HIV occurs at many different levels. The envelop glycoprotein of HIV-1 may directly affect mucosal epithelial cells by upregulating inflammatory cytokines, inducing mucosal injury [61]. Abnormal enterocyte differentiation and increased enterocyte apoptosis due to the failure of the cells to maintain ionic balance and by increased production of interferon-γ (IFNγ) and TNF results in a reduction in the height of the villus and an increase in crypt depth [62]. This has been supported by the demonstration of a decrease in serum citrulline in these patients [63]. Along with an increase in CD8+ T cell infiltration of the intestinal lamina propria, increased cytokine production causes damage to the TJs. With the loss of CD4+ T cells, especially TH17 cells, and B cell dysfunction, there is a decrease in immune modulators and luminal IgA. This facilitates increased microbial growth, TJ disruption, and translocation of luminal content [62]. During acute infection phase, levels of iFABP [64], BG [65], lipopolysaccharide binding protein (LBP), soluble CD14 (sCD14), and endotoxin core antibodies (EndoCAb) are high, indicative of a loss of intestinal barrier function and an increase in the translocation of microbial products. The level of LPS at this stage remains relatively normal suggesting rapidly neutralization of the ongoing LPS translocation [66]. However, during chronic infection, there is a progressive decline in EndoCAb and an increase in plasma LPS. A breakdown in the intestinal barrier functions, therefore, increases the susceptibility of the HIV patients to severe bacterial infections [67] and predispose the patients to the complications due to chronic inflammation and dysregulated immune responses.
Malaria
Patients with malaria are often complicated by a disruption in the intestinal barrier functions and are predisposed to concurrent septicemia, especially with non-typhoidal salmonella infections [39]. Parasitized erythrocytes are sequestrated in the splanchnic vasculature and cause local ischemia that induces intestinal dysbiosis, and increased intestinal permeability and translocation of bacterial products [68]. Parasite infected erythrocyte sequestration in the GI tract reduces the absorption of L-glutamine [69] needed for enterocyte development, proliferation and maintenance of TJ function [70]. Parasite infected erythrocytes in the lamina propria may also cause GI bleeding [71]. Dysregulated immune response as a consequence of Plasmodium infection recruits mast cells to the intestine [69]. Activation of mast cells releases histamine and mast cell proteases that may also damage intestinal barrier. Mast cell protease 1 cleaves occludin 11 in the TJs, and high levels of histamine reported in malaria patients reduces E-cadherin adhesion to promote intestinal permeability [69].
Intestinal barrier function disruption in oncologic diseases
In contrast to hematologic diseases in which the increased intestinal permeability is due primarily to the disease process, disruption in the intestinal barrier functions in oncologic patients are usually iatrogenic, related to treatment of the underlying conditions, although it may also contribute to the underlying disease. Not surprisingly, the iatrogenic-induced compromised intestinal barrier renders the patients to increased risks for the same range of complications as those observed in hematologic patients, in addition to some distinct end-results. In this section, we will examine several oncologic diseases in which intestinal barrier is breached and highlight the clinical consequences of disruption to the intestinal barrier functions in these patients.
Chemotherapy-induced disruption of the intestinal barrier
By far, the commonest cause of intestinal mucosal abnormalities in patients with oncologic diseases is chemotherapy-induced disruption of the intestinal barrier. Table 2 shows some of the chemotherapeutic agents well-recognized for inducing mucosal damage. The susceptibility of patients to chemotherapy-induced intestinal injury is also affected by age. Older patients are more likely to be affected than younger patients [72]. Higher chemotherapy dose and use of multiagent chemotherapy regimens also carries higher risks.
Figure 3 illustrates the cellular and molecular mechanisms associated with chemotherapy-induced intestinal injury. Chemotherapy affects the intestinal mucosa by its direct and indirect effects on DNA replication and cell growth. In addition, chemotherapy may also directly inhibit the formation of TJs. For example, oxaliplatin and irinotecan interfere with TJ formation [73, 74] to increase the intestinal permeability. Both chemotherapeutic agents are used commonly as part of the regimens for treating colon cancer. Major abdominal surgery for colectomy and staging process in these patients further worsens the damage. Methotrexate (MTX), another commonly used chemotherapy, impacts the integrity of TJs in the intestine. A significant decrease in the levels of occludin and claudin-1 proteins occurs 4 days after treatment with MTX [75]. This was not associated with changes in the levels of expression of the corresponding genes, suggesting that MTX affects the localization and cellular expression of TJ proteins, rather than their production [75]. MTX-induced increase in intestinal permeability is mediated by the mitogen-activated protein kinase (MAPK) and nuclear factor kappa B (NF-κB) pathways. The mechanistic effects of chemotherapy on the intestinal barrier functions are, therefore, diverse.
Chemotherapy-induced mucosal injury is also influenced by pro-inflammatory cytokines such as TNF∝, interferon-γ (IFN γ), interleukin 1 (IL-1), and IL-6 [76, 77]. TNF∝ directly affects the function of TJs [77]. It downregulates the expression and impairs the distribution of ZO-1, occludin, claudin-4 and claudin-5, leading to an increase in the barrier permeability over time [78]. IL-1 and IL-6 also induce changes in the TJs [79, 80]. Addition of IL-1 to cell cultures resulted in decreased expression of occludin [81, 82]. Similarly, treatment with IL-6 causes changes in the cytoskeleton, leading to increased permeability across cellular barriers through ZO-1 redistribution, actin structure remodeling, and increased actin contractility [83].
Chemotherapeutic agents may also affect the intestinal barrier functions through inducing alterations in the intestinal microbial community. Patients with chemotherapy-induced intestinal injury have increased abundance of enteropathogenic E. coli and Clostridium perfringens, both of which are known to disrupt TJ proteins and increase epithelial permeability [84, 85]. Epithelial cells infected with E. coli demonstrate increased permeability and destabilization of the TJ proteins ZO-1, occludin, and claudin-1 [84]. Not unlike E. coli, Clostridium perfringens interact with occludin to result in its redistribution and removal from the TJs [85]. Chemotherapy also decreases the microbial diversity of the intestinal microbiota [86, 87], including producers of SCFAs like butyrate. Butyrate, in particular, is not only needed for enterocyte health and TJ development but also has strong anti-inflammatory effects that reduce intestinal injury and maintain the mucus layer [88,89,90,91].
Infection-associated intestinal injury
Chemotherapy often induces neutropenia, rendering oncologic patients to increased risks for opportunistic infections. The frequent use of broad-spectrum antimicrobials, either for prophylaxis against systemic infections or for the empiric therapy of neutropenic fever, alters the intestinal microbial diversity. As a result, these patients are at increased risks for Clostridioides difficile (C. diff.) infections and Cytomegalovirus (CMV) colitis, especially in the setting of allogeneic hematopoietic stem cell transplantation. Antimicrobial agents also change intestinal microbiota that may alter the balance in the production of SCFAs vital for the physiologic development of intestinal mucosal functions.
C. diff. produces Cytotoxin B that damages the structures within enterocytes by attaching single sugar molecules to proteins that help form actin filaments [92]. As a result of the disarrayed F-actin at the luminal and basal ends of the cell, and the separation of occludin, ZO-1, and ZO-2 from the membrane of lateral TJs, C. diff. causes increased intestinal permeability. C. diff. infection occurs in 7–14% [93] and recurrent C. diff. infections in 11–31% [94, 95] of patients with hematologic malignancies, including acute leukemias, multiple myeloma, Hodgkin’s disease, and non-Hodgkin’s lymphoma.
Immunosuppressed patients are at increased risks for CMV colitis. CMV causes IL-6 mediated damage to the TJs in the intestinal epithelial cells, which leads to a decrease in the transepithelial electrical resistance and an increase in their permeability [96]. As a result, these patients are prone to secondary bacteremia that arises due to increased translocation of bacteria across the intestinal barrier.
Severe neutropenia induced by chemotherapy also predisposes patients to the development of typhilitis or neutropenic enterocolitis in which there is a progressive ascending inflammation of the cecum. Although the pathogenesis of typhilitis is yet to be fully dissected, it is associated with inflammation and mucosal injury, with an increase in intestinal permeability. Consequently, patients are at risk of overwhelming enteric-originated septicemia. Typhilitis is associated with a very high mortality rate [97].
Cytokine-induced intestinal injury
Since various pro-inflammatory cytokines affect the integrity of the intestinal mucosa, oncologic conditions associated high levels of these cytokines are expected to be associated with a breach in the intestinal barrier functions. Chimeric Antigen Receptor (CAR T)-cell therapy currently approved by the FDA for treating B-cell acute lymphoblastic leukemia [98], B-cell lymphomas [99], and multiple myeloma [100] and is increasingly being administered to patients is associated with cytokine release syndrome (CRS). Similarly, the increasing use of post-transplant high dose cyclophosphamide as a maneuver to reduce the risks for graft-versus-host disease (GVHD) [101] in patients undergoing allogeneic hematopoietic stem cell transplant, especially in peripheral blood stem cell and haploidentical transplants, is associated with high levels of cytokine release during the first 72 h following infusion of the hematopoietic stem cells. Although there have not been any studies investigating the intestinal barrier functions in these two clinical scenarios, it is expected that these patients will likely develop increased intestinal permeability and its associated complications.
Impaired intestinal barrier functions as driver for underlying oncologic diseases
Although not as extensively studied as in other conditions, a disruption to the intestinal barrier may be a driver for oncologic diseases. In this section, we will discuss how intestinal injury might affect the development of colorectal cancer, progression of myelodysplastic syndrome (MDS), and propagation of acute GVHD following allogeneic hematopoietic stem cell transplantation.
Intestinal permeability and colorectal cancer
Increase in intestinal permeability may predispose susceptible individuals to the development of colorectal cancer (CRC). This is mediated primarily via inflammatory responses induced by intestinal microbiota that promote tumor development. The intestinal microbiota exploits tumor surface barrier defects to invade and induce inflammation within the colonic tissue [102]. Fusobacterium nucleatum, a Gram-negative anaerobic bacterium that adheres to the intestinal mucosa, has been linked to progression of CRC [103]. Its adhesion molecule, FadA, binds to host E-cadherin to enter cells and triggers the WNT/β-catenin pathway, causing the release of cytokines such as IL-6, IL-8 and TNF-α and boosting NF-κB [103]. Interestingly, probiotics, such as Lactobacillus and Bifidobacterium, may prevent CRC growth by reducing inflammation and blood vessel growth, and by fortifying the intestinal barrier through the production of SCFAs [104]. The breakdown of the intestinal barrier also results in increased risks for the development of bacteremia/septicemia.
Further work supporting the role of intestinal barrier in the progression of sporadic CRC comes from experiments using susceptible mice. A lack of mucus and disruption in the production and localization of TJ proteins result in the entry of bacteria and their products into the tumor stroma to activate Toll-like receptor-mediated inflammatory responses [105]. This process occurs early in colonic tumorigenesis and contributes to the development of CRC through the production of inflammatory cytokines such as IL-23, IL-17A, IL-6, and IL-22 [105]. The role of defective gut barrier in CRC has also been confirmed in mucin 2-knockout (MUC2−/−) mice in which the lack of gastrointestinal mucin resulted in spontaneous CRC development [106]. Removal of matriptase, a membrane-anchored serine protease that helps form TJs in the intestinal epithelial barrier, specifically in the intestinal epithelium, also leads to the development of colon adenocarcinoma [107, 108].
Intestinal permeability in the progression of hematologic malignancies
Disruption of the intestinal barrier function may also be associated with the development of hematological malignancies. Bacterial translocation and elevated IL-6 levels caused by small intestine barrier dysfunction are crucial for the development of the pre-leukemic myeloproliferation (PMP) in mice lacking Tet2, a gene frequently mutated in hematologic malignancies. Disrupting the intestinal barrier integrity or exposing Tet2−/− mice to a systemic bacterial stimulus (e.g. TLR2 agonist) induces PMP in these mice [109].
In patients and mice with acute myeloid leukemia (AML), the normal intestinal microbiome is severely perturbed [110]. They exhibit an imbalance in the intestinal microbial community that results in a reduction of SCFAs needed for the development and health of enterocytes and the production of TJ proteins. Consequently, AML is associated with a decrease in the expression of TJ proteins (claudin-1 and ZO-1) with a resultant increase in the translocation of LPS into the systemic circulation to promote inflammatory responses that favor the progression of the disease [110].
Intestinal permeability and the propagation of acute graft-versus-host disease
GVHD is a systemic complication that occurs following allogeneic hematopoietic stem cell transplant. It starts with inflammation and tissue injury induced by the high-dose chemoradiation used as the transplant preparative regimens. The intestinal mucosal injury and associated changes in the intestinal microbiome provide the backdrop for the inflammatory processes. Numerous soluble inflammatory proteins result in diffuse, nonspecific damage to numerous organs and the vascular endothelium. Intestinal barrier breakdown allows the traverse of luminal bacteria and bacterial products into the systemic circulation to activate the TLR signaling pathways to worsen the condition. MLCK210 regulates the intestinal permeability. In GVHD, altered MLCK210 is pivotal for the propagation of GVHD-induced intestinal injury, despite lack of changes in the expression of ZO-1 [111]. Mice lacking MLCK210, although may develop GVHD in a Major-Histocompatibility Complex (MHC) mismatched transplant setting, are protected from prolonged intestinal barrier loss and severe GVHD, as shown by reduced tissue damage, decreased number of CD8 + T cells in the gut, and better overall survival [111].
Altered intestinal microbial diversity associated with allogeneic hematopoietic stem cell transplant and low concentrations of SCFAs and lactase, as well as a high level of lactose contribute to the increased intestinal permeability in these patients [112]. A multicenter study that examined the link between a healthy gut barrier and microbiome, and the occurrence of GVHD and its complications found that a diverse microbiome at the time of hematopoietic cell transplantation was linked to a lower death rate related to GVHD [113]. Patients with mild acute GVHD had better gut barrier function and less gut toxicity, as determined by the 51Cr-EDTA absorption test [114].
Strategies to improve intestinal barrier function
Several strategies are available for fortifying the intestinal barrier to modify the disease course or mitigate the potential complications associated with an increase in the intestinal permeability. These strategies may be applicable to all patients, although the choice of approach depends on the clinical scenario.
Short-chain fatty acids
Intestinal microbiota produces organic acids such as acetate, propionate, butyrate, and valerate through fermentation of dietary microbiota-accessible carbohydrates (MACs) that are non-digestible in the host colon but used by the microbes as an energy source. In the absence of dietary MACs, mucus-degrading bacterial population increases by feeding on mucin. Thus, disruption of the microbial composition will deplete mucus layer, and affect the production of the SCFAs needed for enterocyte health and metabolism, and TJ development. A deficiency of butyrate results in increased intestinal permeability in inflammatory bowel diseases (IBD) [115]. Butyrate also possesses anti-inflammatory properties that may modulate the inflammatory reactions induced by local invasive bacteria. Oral supplement of SCFAs is currently being investigated for hematologic and oncologic diseases (Table 3).
Pre- and probiotics
Pre- and probiotics supplements are potential approaches to increase intestinal barrier functions [116, 117]. They exert their activities through increasing the expression of TJ proteins, reducing intestinal inflammation, and modulating the local immune responses [118]. They modulate intestinal tissue dendritic cells to produce IL-10, decrease IFN-γ release by intestinal T-cells and decrease LPS-induced production of the proinflammatory IL-12 [119]. Despite a lack of US FDA regulation, the most well-studied products with regards to safety are Lactobacillus, Bifidobacterium, and Saccharomyces boulardii. A major shortfall in these products is that there exists extensive variability in the preparations available, including single or multi-strain products. The other concern on the use of probiotics in immunocompromised patients is the risks for fungemia and bacteremia. A retrospective literature review identified 59 cases of fungemia linked to the use of probiotics [120]. However, a study involving 31 pediatric and adolescent patients undergoing allogeneic hematopoietic stem cell transplant found that administration of Lactobacillus from Day -7 during the conditioning regimen through Day + 114 did not result in Lactobacillus bacteremia [121]. Dietary changes are being investigated in various hematologic and oncologic diseases (Table 3).
Fecal microbiota transplant
Fecal microbiota transplant (FMT) has been used successfully for the treatment of recurrent/refractory C. diff. infection [122]. It is also being investigated in various diseases associated with a breakdown in the intestinal barrier functions. In addition to restoring the balance of microbial community in the intestine, it provides a mean to replenish the microbial community with SCFA producers to fortify the intestinal barrier. FMT may be therapeutically beneficial to patients with various hematologic and oncologic diseases [123]. In addition to treating malignancy-associated recurrent/refractory C. diff. infections, FMT has been used to treat corticosteroid-refractory acute intestinal GVHD and reversal of resistance to immune checkpoint inhibitors in patients with metastatic melanoma. FMT is currently being investigated in various oncologic clinical studies. Table 4 shows a list of studies currently actively recruiting patients with hematologic and oncologic diseases for FMT.
However, just like probiotics, the risk of introducing infections remains the biggest concern, especially in this group of patients who are usually immunocompromised due to treatment of their underlying malignancies. Fatal extended-spectrum beta-lactamases (ESBL) E. coli septicemia was reported in a patient with MDS who received pre-emptive FMT [124].
Akkermansia muciniphila
Akkermansia muciniphila (A. muciniphila) is a Gram-negative obligative anaerobic bacteria that has been linked to various health benefits, including improved gut barrier function and reduced inflammation. Oral supplement of A. muciniphila has demonstrated efficacy in patients with metabolic syndrome [125]. However, an overgrowth or over-abundance of the organism may potentially be detrimental in oncologic patients with adenocarcinomas. A. muciniphila degrades mucin for its growth. Its abundance may, therefore, induce damage to the mucosal barrier, and promote intestinal permeability. Abundance of A. muciniphila may promote metastasis of adenocarcinoma, as has been demonstrated in a hormone receptor-positive breast cancer mouse model [126]. Excessive degradation of the intestinal mucin by the organism may also increase epithelial access by intestinal bacteria to trigger colitis, as has been shown in Citrobacter rodentium-induced colitis in gnotobiotic mice [127].
L-glutamine
L-glutamine is an amino acid considered a “conditionally essential” nutrient. It has been shown to play a role in regulating the intestinal barrier function. L-glutamine not only provides the source of energy for the intestinal epithelium, it also helps maintain the structural integrity of the gut epithelial cells and TJ development [70]. Supplementation with L-glutamine has been shown to improve gut barrier function in animal models and in some human studies, particularly in individuals with gut-related conditions such as IBD and short bowel syndrome [128]. L-glutamine is currently approved by the FDA for treating SCD. However, the biologic rationale for its use in SCD is not based on improving intestinal barrier function but rather to reduce erythrocyte redox imbalance, which triggers sickling of the erythrocytes. Despite this, SCD patients treated with L-glutamine have not shown significant improvement in the parameters for hemolysis [129]. The laboratory findings of breached intestinal barrier functions in patients with SCD [129] raise the possibility that the beneficial effects of L-glutamine in SCD occur via reduction in the intestinal permeability associated with the disease.
L-glutamine has been used in clinical trials to determine its role in reducing chemoradiation-induced mucositis [130, 131]. However, the results have been mixed and may reflect the different dosages and timing of administration of the L-glutamine.
Keratinocyte growth factors
Keratinocyte growth factors (KGFs) are a group of cytokines that promote the growth and differentiation of epithelial cells, including the intestinal epithelium. Studies have shown that KGFs play a role in regulating the intestinal barrier function by promoting the proliferation and differentiation of gut epithelial cells, and by maintaining the structural integrity of the TJs that form the gut barrier [132]. KGFs have been investigated as a potential therapeutic approach for a variety of diseases and conditions associated with epithelial cell dysfunction. In fact, KGFs have been shown to promote the healing of gut epithelium in individuals with IBD and improve gut barrier function [133]. KGFs have also been shown to improve the survival and proliferation of gut epithelial cells in short bowel syndrome by restoring the intestinal barrier functions [134, 135]. KGFs have been investigated as a potential therapeutic approach for the prevention and treatment of oral mucositis following high dose chemotherapy and autologous hematopoietic stem cell transplant [136]. Patients randomized to the recombinant KGF exhibited lower incidence of severe oral mucositis and reduced incidence of septicemia. KGF is currently licensed for use to prevent chemotherapy-induced mucositis. Unfortunately, its use has been limited by the high benefit: cost ratio.
Conclusions
There is now abundance of evidence to implicate the roles of increased intestinal permeability in various systemic disease states. In systemic diseases found to be associated with increased intestinal permeability, there remains many questions that needs to be answered before any preventive measures can be formulated. In particular, except for inflammatory bowel disease where there is a definite primary intestinal pathology, it is unclear if the disruption in the intestinal barrier function is primary and be responsible for the systemic diseases or secondary to other causes associated with the primary systemic diseases. If the primary pathology results from a disruption of the intestinal barrier functions, it also remains to be determined what the primary insults are. Various causes have been previously proposed, including nutritional factors, infections and toxins, “hygiene hypothesis”, “lifestyle hypothesis”, and endogenous factors [137]. The application of such factors to explain the pathogenesis of the disease next leads to the question of what then determines the phenotype of the disease that results. Why do some patients develop autism, others Parkinson’s disease, and yet others non-alcoholic steatohepatitis? Unlike the other diseases, the disruption in the intestinal barrier functions associated with many of the hematologic and oncologic diseases are primarily iatrogenic in origin. In these scenarios, the abnormalities may be transient, although may also be unavoidable. Understanding the anatomy and physiology of the intestinal barrier provides the opportunity for therapeutic targeting to either modify the disease course or mitigate the potential complications.
Unfortunately, efforts to accomplish the above aims are hampered by the lack of quality and widely available methods for evaluating and quantitating intestinal barrier functions. Furthermore, while strategies based on sound scientific rationale are available, their efficacy has so far not been translated into successes in the clinic, suggesting the need for further research to address the diagnostic and therapeutic gaps, especially in patients with hematologic and oncologic disease who pose the additional challenge of being immunocompromised.
Availability of data and materials
Not applicable.
Abbreviations
- 51Cr-EDTA:
-
Radioactive chromium complexed with ethylene diamine tetracetic acid
- AML:
-
Acute myeloid leukemia
- BG:
-
(1 → 3)-β-D-glucan
- CANs:
-
Circulating aged neutrophils
- CAR T:
-
Chimeric Antigen Receptor
- CLE:
-
Confocal laser endomicroscopy
- CMV:
-
Cytomegalovirus
- CRC:
-
Colorectal cancer
- CRS:
-
Cytokine release syndrome
- DAMPs:
-
Damage-associated-molecular patterns
- ESBL:
-
Extended-spectrum beta-lactamases
- EndoCAb:
-
Endotoxin core antibodies
- FITC:
-
Fluorescein isothiocyanate
- FMT:
-
Fecal microbiota transplant
- GI:
-
Gastrointestinal
- GVHD:
-
Graft-versus-host disease
- HIV:
-
Human immunodeficiency virus
- HbS:
-
Sickle hemoglobin
- IBD:
-
Inflammatory bowel diseases
- iFABP:
-
Intestinal fatty acid binding protein
- IFN:
-
Interferon
- IL:
-
Interleukin
- IgA:
-
Immunoglobulin A
- KGFs:
-
Keratinocyte growth factors
- L:M:
-
Lactulose:mannitol
- LBP:
-
Lipopolysaccharide binding protein
- LPS:
-
Lipopolysaccharide
- MACs:
-
Microbiota-accessible carbohydrates
- MAPK:
-
Mitogen-activated protein kinase
- MDS:
-
Myelodysplastic syndrome
- MHC:
-
Major-histocompatibility complex
- MLCK:
-
Myosin light chain kinase
- MTX:
-
Methotrexate
- MUC 2:
-
Mucin 2
- MYD88:
-
Myeloid differentiation factor 88
- NF-κB:
-
Nuclear factor kappa B
- PAMPs:
-
Pathogen-associated-molecular patterns
- PEG:
-
Polyethylene glycol
- PMP:
-
Pre-leukemic myeloproliferation
- PRRs:
-
Pattern recognition receptors
- SCD:
-
Sickle cell disease
- SCFAs:
-
Short-chain fatty acids
- TJs:
-
Tight junctions
- TLRs:
-
Toll-like receptors
- TNF:
-
Tumor necrosis factor
- VOC:
-
Vaso-occlusive crisis
References
Michielan A, D’Incà R. Intestinal permeability in inflammatory bowel disease: pathogenesis, clinical evaluation, and therapy of leaky gut. Mediators Inflamm. 2015;2015:628157.
Pizzuti D, Bortolami M, Mazzon E, Buda A, Guariso G, D’Odorico A, Chiarelli S, D’Incà R, De Lazzari F, Martines D. Transcriptional downregulation of tight junction protein ZO-1 in active coeliac disease is reversed after a gluten-free diet. Dig Liver Dis. 2004;36:337–41.
Plaza-Díaz J, Solís-Urra P, Rodríguez-Rodríguez F, Olivares-Arancibia J, Navarro-Oliveros M, Abadía-Molina F, Álvarez-Mercado AI. The gut barrier, intestinal microbiota, and liver disease: molecular mechanisms and strategies to manage. Int J Mol Sci. 2020;21:8351.
Yuan JH, Xie QS, Chen GC, Huang CL, Yu T, Chen QK, Li JY. Impaired intestinal barrier function in type 2 diabetic patients measured by serum LPS, Zonulin, and IFABP. J Diabetes Complicat. 2021;35:107766.
Fiorentino M, Sapone A, Senger S, Camhi SS, Kadzielski SM, Buie TM, Kelly DL, Cascella N, Fasano A. Blood-brain barrier and intestinal epithelial barrier alterations in autism spectrum disorders. Mol Autism. 2016;7:49.
Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017;11:821–34.
Johansson ME, Sjovall H, Hansson GC. The gastrointestinal mucus system in health and disease. Nat Rev Gastroenterol Hepatol. 2013;10:352–61.
Johansson ME, Hansson GC. Immunological aspects of intestinal mucus and mucins. Nat Rev Immunol. 2016;16:639–49.
Johansson ME, Ambort D, Pelaseyed T, Schütte A, Gustafsson JK, Ermund A, Subramani DB, Holmén-Larsson JM, Thomsson KA, Bergström JH, van der Post S, Rodriguez-Piñeiro AM, Sjövall H, Bäckström M, Hansson GC. Composition and functional role of the mucus layers in the intestine. Cell Mol Life Sci. 2011;68:3635–41.
Cornick S, Tawiah A, Chadee K. Roles and regulation of the mucus barrier in the gut. Tissue Barriers. 2015;3:e982426.
Zareie M, Riff J, Donato K, McKay DM, Perdue MH, Soderholm JD, Karmali M, Cohen MB, Hawkins J, Sherman PM. Novel effects of the prototype translocating Escherichia coli, strain C25 on intestinal epithelial structure and barrier function. Cell Microbiol. 2005;7:1782–97.
Karl JP, Margolis LM, Madslien EH, Murphy NE, Castellani JW, Gundersen Y, Hoke AV, Levangie MW, Kumar R, Chakraborty N, Gautam A, Hammamieh R, Martini S, Montain SJ, Pasiakos SM. Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. Am J Physiol Gastrointest Liver Physiol. 2017;312:G559–71.
Zuo L, Kuo WT, Turner JR. Tight junctions as targets and effectors of mucosal immune homeostasis. Cell Mol Gastroenterol Hepatol. 2020;10:327–40.
Buschmann MM, Shen L, Rajapakse H, Raleigh DR, Wang Y, Wang Y, Lingaraju A, Zha J, Abbott E, McAuley EM, Breskin LA, Wu L, Anderson K, Turner JR, Weber CR. Occludin OCEL-domain interactions are required for maintenance and regulation of the tight junction barrier to macromolecular flux. Mol Biol Cell. 2013;24:3056–68.
Turner JR, Rill BK, Carlson SL, Carnes D, Kerner R, Mrsny RJ, Madara JL. Physiological regulation of epithelial tight junctions is associated with myosin light-chain phosphorylation. Am J Physiol. 1997;273:C1378–85.
Weber CR, Raleigh DR, Su L, Shen L, Sullivan EA, Wang Y, Turner JR. Epithelial myosin light chain kinase activation induces mucosal interleukin-13 expression to alter tight junction ion selectivity. J Biol Chem. 2010;285:12037–46.
Krug SM, Amasheh S, Richter JF, Milatz S, Günzel D, Westphal JK, Huber O, Schulzke JD, Fromm M. Tricellulin forms a barrier to macromolecules in tricellular tight junctions without affecting ion permeability. Mol Biol Cell. 2009;20:3713–24.
Su L, Shen L, Clayburgh DR, Nalle SC, Sullivan EA, Meddings JB, Abraham C, Turner JR. Targeted epithelial tight junction dysfunction causes immune activation and contributes to development of experimental colitis. Gastroenterol. 2009;136:551–63.
Marchiando AM, Shen L, Graham WV, Weber CR, Schwarz BT, Austin JR 2nd, Raleigh DR, Guan Y, Watson AJ, Montrose MH, Turner JR. Caveolin-1-dependent occludin endocytosis is required for TNF-induced tight junction regulation in vivo. J Cell Biol. 2010;189:111–26.
Fanning AS, Ma TY, Anderson JM. Isolation and functional characterization of the actin binding region in the tight junction protein ZO-1. FASEB J. 2002;16:1835–7.
Yu D, Marchiando AM, Weber CR, Raleigh DR, Wang Y, Shen L, Turner JR. MLCK-dependent exchange and actin binding region-dependent anchoring of ZO-1 regulate tight junction barrier function. Proc Natl Acad Sci USA. 2010;107:8237–41.
Van Itallie CM, Fanning AS, Bridges A, Anderson JM. ZO-1 stabilizes the tight junction solute barrier through coupling to the perijunctional cytoskeleton. Mol Biol Cell. 2009;20:3930–40.
Al-Sadi R, Ye D, Dokladny K, Ma TY. Mechanism of IL-1beta-induced increase in intestinal epithelial tight junction permeability. J Immunol. 2008;180:5653–61.
Guerville M, Boudry G. Gastrointestinal and hepatic mechanisms limiting entry and dissemination of lipopolysaccharide into the systemic circulation. Am J Physiol Gastrointest Liver Physiol. 2016;311:G1–15.
Da Silva C, Wagner C, Bonnardel J, Gorvel JP, Lelouard H. The peyer’s patch mononuclear phagocyte system at steady state and during infection. Front Immunol. 2017;8:1254.
Knoop KA, Gustafsson JK, McDonald KG, Kulkarni DH, Kassel R, Newberry RD. Antibiotics promote the sampling of luminal antigens and bacteria via colonic goblet cell associated antigen passages. Gut Microbes. 2017;8:400–11.
Johnston SD, Smye M, Watson RG, McMillan SA, Trimble ER, Love AH. Lactulose-mannitol intestinal permeability test: a useful screening test for adult coeliac disease. Ann Clin Biochem. 2000;37(Pt 4):512–9.
Gan J, Nazarian S, Teare J, Darzi A, Ashrafian H, Thompson AJ. A case for improved assessment of gut permeability: a meta-analysis quantifying the lactulose:mannitol ratio in coeliac and Crohn’s disease. BMC Gastroenterol. 2022;22:16.
Neumann H, Kiesslich R, Wallace MB, Neurath MF. Confocal laser endomicroscopy: technical advances and clinical applications. Gastroenterol. 2010;139(388–392):392.e1-2.
Sun L, Yue M, Dai Y, Yu C, Chen C. Confocal laser endomicroscopy reveals alterations in duodenal permeability in patients with acute pancreatitis. J Int Med Res. 2019;47:1279–87.
Buchner AM. Confocal laser endomicroscopy in the evaluation of inflammatory bowel disease. Inflamm Bowel Dis. 2019;25:1302–12.
Kanda T, Nakatomi Y, Ishikawa H, Hitomi M, Matsubara Y, Ono T, Muto T. Intestinal fatty acid-binding protein as a sensitive marker of intestinal ischemia. Dig Dis Sci. 1992;37:1362–7.
Fasano A, Not T, Wang W, Uzzau S, Berti I, Tommasini A, Goldblum SE. Zonulin, a newly discovered modulator of intestinal permeability, and its expression in coeliac disease. Lancet. 2000;355:1518–9.
Crenn P, Messing B, Cynober L. Citrulline as a biomarker of intestinal failure due to enterocyte mass reduction. Clin Nutr. 2008;27:328–39.
Munford RS. Endotoxemia-menace, marker, or mistake? J Leukoc Biol. 2016;100:687–98.
Diebel LN, Liberati DM, Dulchavsky SA, Diglio CA, Brown WJ. Enterocyte apoptosis and barrier function are modulated by SIgA after exposure to bacteria and hypoxia/reoxygenation. Surgery. 2003;134:574–81.
Dutta D, Methe B, Amar S, Morris A, Lim SH. Intestinal injury and gut permeability in sickle cell disease. J Transl Med. 2019;17:183.
Poplawska M, Dutta D, Jayaram M, Salifu M, Chong NS, Lim SH. Intestinal pathophysiological abnormalities in steady state and after vaso-occlusive crisis in murine sickle cell disease. Br J Haematol. 2022;196:777–80.
Lim SH, Methé BA, Knoll BM, Morris A, Obaro SK. Invasive non-typhoidal Salmonella in sickle cell disease in Africa: is increased gut permeability the missing link? J Transl Med. 2018;16:239.
Brim H, Taylor J, Abbas M, Vilmenay K, Daremipouran M, Varma S, Lee E, Pace B, Song-Naba WL, Gupta K, Nekhai S, O’Neil P, Ashktorab H. The gut microbiome in sickle cell disease: characterization and potential implications. PLoS ONE. 2021;16:e0255956.
Lim SH, Morris A, Li K, Fitch AC, Fast L, Goldberg L, Quesenberry M, Sprinz P, Methé B. Intestinal microbiome analysis revealed dysbiosis in sickle cell disease. Am J Hematol. 2018;93:E91–3.
Tavakoli S, Xiao L. Depletion of intestinal microbiome partially rescues bone loss in sickle cell disease male mice. Sci Rep. 2019;9:8659.
Jang T, Poplawska M, Cimpeanu E, Mo G, Dutta D, Lim SH. Vaso-occlusive crisis in sickle cell disease: a vicious cycle of secondary events. J Transl Med. 2021;19:397.
Anyaegbu CC, Okpala IE, Akren’Ova YA, Salimonu LS. Peripheral blood neutrophil count and candidacidal activity correlate with the clinical severity of sickle cell anaemia (SCA). Eur J Haematol. 1998;60:267–8.
Lard LR, Mul FP, de Haas M, Roos D, Duits AJ. Neutrophil activation in sickle cell disease. J Leukoc Biol. 1999;66:411–5.
Lum AF, Wun T, Staunton D, Simon SI. Inflammatory potential of neutrophils detected in sickle cell disease. Am J Hematol. 2004;76:126–33.
Belcher JD, Marker PH, Weber JP, Hebbel RP, Vercellotti GM. Activated monocytes in sickle cell disease: potential role in the activation of vascular endothelium and vaso-occlusion. Blood. 2000;96:2451–9.
Sparkenbaugh E, Pawlinski R. Interplay between coagulation and vascular inflammation in sickle cell disease. Br J Haematol. 2013;162:3–14.
Zhang D, Chen G, Manwani D, Mortha A, Xu C, Faith JJ, Burk RD, Kunisaki Y, Jang JE, Scheiermann C, Merad M, Frenette PS. Neutrophil ageing is regulated by the microbiome. Nature. 2015;525:528–32.
Wiens M, Korzhev M, Krasko A, Thakur NL, Perović-Ottstadt S, Breter HJ, Ushijima H, Diehl-Seifert B, Müller IM, Müller WE. Innate immune defense of the sponge Suberites domuncula against bacteria involves a MyD88-dependent signaling pathway. induction of a perforin-like molecule. J Biol Chem. 2005;280:27949–59.
Tartey S, Takeuchi O. Pathogen recognition and toll-like receptor targeted therapeutics in innate immune cells. Int Rev Immunol. 2017;36:57–73.
Williams JM, Duckworth CA, Burkitt MD, Watson AJ, Campbell BJ, Pritchard DM. Epithelial cell shedding and barrier function: a matter of life and death at the small intestinal villus tip. Vet Pathol. 2015;52:445–55.
Taher AT, Saliba AN. Iron overload in thalassemia: different organs at different rates. Hematology Am Soc Hematol Educ Program. 2017;2017:265–71.
Sae-Khow K, Charoensappakit A, Visitchanakun P, Saisorn W, Svasti S, Fucharoen S, Leelahavanichkul A. Pathogen-associated molecules from gut translocation enhance severity of cecal ligation and puncture sepsis in iron-overload beta-Thalassemia mice. J Inflamm Res. 2020;13:719–35.
Visitchanakun P, Saisorn W, Wongphoom J, Chatthanathon P, Somboonna N, Svasti S, Fucharoen S, Leelahavanichkul A. Gut leakage enhances sepsis susceptibility in iron-overloaded beta-thalassemia mice through macrophage hyperinflammatory responses. Am J Physiol Gastrointest Liver Physiol. 2020;318:G966–79.
Vento S, Cainelli F, Cesario F. Infections and thalassaemia. Lancet Infect Dis. 2006;6:226–33.
Teawtrakul N, Jetsrisuparb A, Sirijerachai C, Chansung K, Wanitpongpun C. Severe bacterial infections in patients with non-transfusion-dependent thalassemia: prevalence and clinical risk factors. Int J Infect Dis. 2015;39:53–6.
Borgna-Pignatti C, Cappellini MD, De Stefano P, Del Vecchio GC, Forni GL, Gamberini MR, Ghilardi R, Origa R, Piga A, Romeo MA, Zhao H, Cnaan A. Survival and complications in thalassemia. Ann N Y Acad Sci. 2005;1054:40–7.
Lerner AM, Eisinger RW, Fauci AS. Comorbidities in persons with HIV: the lingering challenge. JAMA. 2020;323:19–20.
Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, Kazzaz Z, Bornstein E, Lambotte O, Altmann D, Blazar BR, Rodriguez B, Teixeira-Johnson L, Landay A, Martin JN, Hecht FM, Picker LJ, Lederman MM, Deeks SG, Douek DC. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–71.
Nazli A, Chan O, Dobson-Belaire WN, Ouellet M, Tremblay MJ, Gray-Owen SD, Arsenault AL, Kaushic C. Exposure to HIV-1 directly impairs mucosal epithelial barrier integrity allowing microbial translocation. PLoS Pathog. 2010;6:e1000852.
Sandler NG, Douek DC. Microbial translocation in HIV infection: causes, consequences and treatment opportunities. Nat Rev Microbiol. 2012;10:655–66.
Crenn P, De Truchis P, Neveux N, Galpérine T, Cynober L, Melchior JC. Plasma citrulline is a biomarker of enterocyte mass and an indicator of parenteral nutrition in HIV-infected patients. Am J Clin Nutr. 2009;90:587–94.
Mavigner M, Cazabat M, Dubois M, L’Faqihi FE, Requena M, Pasquier C, Klopp P, Amar J, Alric L, Barange K, Vinel JP, Marchou B, Massip P, Izopet J, Delobel P. Altered CD4+ T cell homing to the gut impairs mucosal immune reconstitution in treated HIV-infected individuals. J Clin Invest. 2012;122:62–9.
Mehraj V, Ramendra R, Isnard S, Dupuy FP, Ponte R, Chen J, Kema I, Jenabian MA, Costinuik CT, Lebouché B, Thomas R, Coté P, Leblanc R, Baril JG, Durand M, Chartrand-Lefebvre C, Tremblay C, Ancuta P, Bernard NF, Sheppard DC, Routy JP. Montreal primary HIV infection study and canadian HIV and aging cohort study groups. circulating (1–>3)-beta-D-glucan is associated with immune activation during human immunodeficiency virus infection. Clin Infect Dis. 2020;70:232–41.
Marchetti G, Tincati C, Silvestri G. Microbial translocation in the pathogenesis of HIV infection and AIDS. Clin Microbiol Rev. 2013;26:2–18.
Huson MA, Grobusch MP, van der Poll T. The effect of HIV infection on the host response to bacterial sepsis. Lancet Infect Dis. 2015;15:95–108.
Leopold SJ, Ghose A, Allman EL, Kingston HWF, Hossain A, Dutta AK, Plewes K, Chotivanich K, Day NPJ, Tarning J, Winterberg M, White NJ, Llinás M, Dondorp AM. Identifying the components of acidosis in patients with severe Plasmodium falciparum malaria using metabolomics. J Infect Dis. 2019;219:1766–76.
Donnelly E, de Water JV, Luckhart S. Malaria-induced bacteremia as a consequence of multiple parasite survival strategies. Curr Res Microb Sci. 2021;2:100036.
Wang B, Wu G, Zhou Z, Dai Z, Sun Y, Ji Y, Li W, Wang W, Liu C, Han F, Wu Z. Glutamine and intestinal barrier function. Amino Acids. 2015;47:2143–54.
Abkallo HM, Liu W, Hokama S, Ferreira PE, Nakazawa S, Maeno Y, Quang NT, Kobayashi N, Kaneko O, Huffman MA, Kawai S, Marchand RP, Carter R, Hahn BH, Culleton R. DNA from pre-erythrocytic stage malaria parasites is detectable by PCR in the faeces and blood of hosts. Int J Parasitol. 2014;44:467–73.
Lichtman SM. Physiological aspects of aging implications for the treatment of cancer. Drugs Aging. 1995;7:212–25.
Forsgård RA, Korpela R, Holma R, Lindén J, Frias R, Spillmann T, Österlund P. Intestinal permeability to iohexol as an in vivo marker of chemotherapy-induced gastrointestinal toxicity in sprague-dawley rats. Cancer Chemother Pharmacol. 2016;78:863–74.
Wardill HR, Bowen JM, Al-Dasooqi N, Sultani M, Bateman E, Stansborough R, Shirren J, Gibson RJ. Irinotecan disrupts tight junction proteins within the gut: implications for chemotherapy-induced gut toxicity. Cancer Biol Ther. 2014;15:236–44.
Beutheu Youmba S, Belmonte L, Galas L, Boukhettala N, Bôle-Feysot C, Déchelotte P, Coëffier M. Methotrexate modulates tight junctions through NF-κB, MEK, and JNK pathways. J Pediatr Gastroenterol Nutr. 2012;54:463–70.
Ma TY, Iwamoto GK, Hoa NT, Akotia V, Pedram A, Boivin MA, Said HM. TNF-α-induced increase in intestinal epithelial tight junction permeability requires NF-κB activation. Am J Physiol-Gastrointest Liver Physiol. 2004;286:G367–76.
Logan RM, Stringer AM, Bowen JM, Yeoh AS, Gibson RJ, Sonis ST, Keefe DM. The role of pro-inflammatory cytokines in cancer treatment-induced alimentary tract mucositis: Pathobiology, animal models and cytotoxic drugs. Cancer Treat Rev. 2007;33:448–60.
Logan RM, Stringer AM, Bowen JM, Gibson RJ, Sonis ST, Keefe DM. Serum levels of NFkappaB and pro-inflammatory cytokines following administration of mucotoxic drugs. Cancer Biol Ther. 2008;7:1139–45.
Williams DA. Inflammatory cytokines and mucosal injury. JNCI Monogr. 2001;2001:26–30.
Poritz LS, Garver KI, Tilberg AF, Koltun WA. Tumor necrosis factor alpha disrupts tight junction assembly. J Surg Res. 2004;116:14–8.
Ma TY, Boivin MA, Ye D, Pedram A, Said HM. Mechanism of TNF-α modulation of Caco-2 intestinal epithelial tight junction barrier: role of myosin light-chain kinase protein expression. Am J Physiol-Gastrointest Liver Physiol. 2005;288:G422-430.
Sonis ST. The biologic role for nuclear factor-kappa B in disease and its potential involvement in mucosal injury associated with anti-neoplastic therapy. Crit Rev Oral Biol Med. 2002;13:380–9.
Marcus BC, Wyble CW, Hynes KL, Gewertz BL. Cytokine-induced increases in endothelial permeability occur after adhesion molecule expression. Surgery. 1996;120:411–7.
Singh AP, Aijaz S. Enteropathogenic E. coli: breaking the intestinal tight junction barrier. Res. 2015;4:231.
Vecchio AJ, Rathnayake SS, Stroud RM. Structural basis for Clostridium perfringens enterotoxin targeting of claudins at tight junctions in mammalian gut. Proc Natl Acad Sci USA. 2021;118:e2024651118.
Wei L, Wen XS, Xian CJ. Chemotherapy-induced intestinal microbiota dysbiosis impairs mucosal homeostasis by modulating toll-like receptor signaling pathways. Int J Mol Sci. 2021;22:9474.
Montassier E, Gastinne T, Vangay P, Al-Ghalith GA, des Bruley Varannes S, Massart S, Moreau P, Potel G, de La Cochetière MF, Batard E, Knights D. Chemotherapy-driven dysbiosis in the intestinal microbiome. Aliment Pharmacol Ther. 2015;42:515–28.
Louis P, Flint HJ. Formation of propionate and butyrate by the human colonic microbiota. Environ Microbiol. 2017;19:29–41.
Sun Q, Ji YC, Wang ZL, She X, He Y, Ai Q, Li LQ. Sodium butyrate alleviates intestinal inflammation in mice with necrotizing enterocolitis. Mediators Inflamm. 2021;2021:6259381.
Yan H, Ajuwon KM. Butyrate modifies intestinal barrier function in IPEC-J2 cells through a selective upregulation of tight junction proteins and activation of the Akt signaling pathway. PLoS ONE. 2017;12:e0179586.
Silva JPB, Navegantes-Lima KC, Oliveira ALB, Rodrigues DVS, Gaspar SLF, Monteiro VVS, Moura DP, Monteiro MC. Protective mechanisms of butyrate on inflammatory bowel disease. Curr Pharm Des. 2018;24:4154–66.
Voth DE, Ballard JD. Clostridium difficile toxins: mechanism of action and role in disease. Clin Microbiol Rev. 2005;18:247–63.
McGlone SM, Bailey RR, Zimmer SM, Popovich MJ, Tian Y, Ufberg P, Muder RR, Lee BY. The economic burden of clostridium difficile. Clin Microbiol Infect. 2012;18:282–9.
Willems L, Porcher R, Lafaurie M, Casin I, Robin M, Xhaard A, Andreoli AL, Rodriguez-Otero P, Dhedin N, Socié G, Ribaud P, de Peffault Latour R. Clostridium difficile infection after allogeneic hematopoietic stem cell transplantation: incidence, risk factors, and outcome. Biol Blood Marrow Transplant. 2012;18:1295–301.
Kamboj M, Xiao K, Kaltsas A, Huang YT, Sun J, Chung D, Wu S, Sheahan A, Sepkowitz K, Jakubowski AA, Papanicolaou G. Clostridium difficile infection after allogeneic hematopoietic stem cell transplant: strain diversity and outcomes associated with NAP1/027. Biol Blood Marrow Transplant. 2014;20:1626–33.
Maidji E, Somsouk M, Rivera JM, Hunt PW, Stoddart CA. Replication of CMV in the gut of HIV-infected individuals and epithelial barrier dysfunction. PLoS Pathog. 2017;13:e1006202.
Altınel E, Yarali N, Isık P, Bay A, Kara A, Tunc B. Typhlitis in acute childhood leukemia. Med Princ Pract. 2012;21:36–9.
Sheykhhasan M, Manoochehri H, Dama P. Use of CAR T-cell for acute lymphoblastic leukemia (ALL) treatment: a review study. Cancer Gene Ther. 2022;29:1080–96.
Chavez JC, Locke FL. CAR T cell therapy for B-cell lymphomas. Best Pract Res Clin Haematol. 2018;31:135–46.
Rendo MJ, Joseph JJ, Phan LM, DeStefano CB. CAR T-cell therapy for patients with multiple myeloma: current evidence and challenges. Blood Lymphat Cancer. 2022;12:119–36.
Luznik L, Jones RJ, Fuchs EJ. High-dose cyclophosphamide for graft-versus-host disease prevention. Curr Opin Hematol. 2010;17:493–9.
Gao R, Gao Z, Huang L, Qin H. Gut microbiota and colorectal cancer. Eur J Clin Microbiol Infect Dis. 2017;36:757–69.
Shang FM, Liu HL. Fusobacterium nucleatum and colorectal cancer: a review. World J Gastrointest Oncol. 2018;10:71–81.
Lin C, Cai X, Zhang J, Wang W, Sheng Q, Hua H, Zhou X. Role of gut microbiota in the development and treatment of colorectal cancer. Digestion. 2019;100:72–8.
Grivennikov SI, Wang K, Mucida D, Stewart CA, Schnabl B, Jauch D, Taniguchi K, Yu GY, Osterreicher CH, Hung KE, Datz C, Feng Y, Fearon ER, Oukka M, Tessarollo L, Coppola V, Yarovinsky F, Cheroutre H, Eckmann L, Trinchieri G, Karin M. Adenoma-linked barrier defects and microbial products drive IL-23/IL-17-mediated tumour growth. Nature. 2012;491:254–8.
Velcich A, Yang W, Heyer J, Fragale A, Nicholas C, Viani S, Kucherlapati R, Lipkin M, Yang K, Augenlicht L. Colorectal cancer in mice genetically deficient in the mucin Muc2. Science. 2002;295:1726–9.
Kosa P, Szabo R, Molinolo AA, Bugge TH. Suppression of Tumorigenicity-14, encoding matriptase, is a critical suppressor of colitis and colitis-associated colon carcinogenesis. Oncogene. 2012;31:3679–95.
Buzza MS, Netzel-Arnett S, Shea-Donohue T, Zhao A, Lin CY, List K, Szabo R, Fasano A, Bugge TH, Antalis TM. Membrane-anchored serine protease matriptase regulates epithelial barrier formation and permeability in the intestine. Proc Natl Acad Sci USA. 2010;107:4200–5.
Meisel M, Hinterleitner R, Pacis A, Chen L, Earley ZM, Mayassi T, Pierre JF, Ernest JD, Galipeau HJ, Thuille N, Bouziat R, Buscarlet M, Ringus DL, Wang Y, Li Y, Dinh V, Kim SM, McDonald BD, Zurenski MA, Musch MW, Furtado GC, Lira SA, Baier G, Chang EB, Eren AM, Weber CR, Busque L, Godley LA, Verdú EF, Barreiro LB, Jabri B. Microbial signals drive pre-leukaemic myeloproliferation in a Tet2-deficient host. Nature. 2018;557:580–4.
Wang R, Yang X, Liu J, Zhong F, Zhang C, Chen Y, Sun T, Ji C, Ma D. Gut microbiota regulates acute myeloid leukaemia via alteration of intestinal barrier function mediated by butyrate. Nat Commun. 2022;13:2522.
Nalle SC, Zuo L, Ong MLDM, Singh G, Worthylake AM, Choi W, Manresa MC, Southworth AP, Edelblum KL, Baker GJ, Joseph NE, Savage PA, Turner JR. Graft-versus-host disease propagation depends on increased intestinal epithelial tight junction permeability. J Clin Invest. 2019;129:902–14.
Tyszka M, Biliński J, Basak GW. Advances in intestinal barrier preservation and restoration in the allogeneic hematopoietic cell transplantation setting. J Clin Med. 2021;10:2508.
Peled JU, Gomes ALC, Devlin SM, Littmann ER, Taur Y, Sung AD, Weber D, Hashimoto D, Slingerland AE, Slingerland JB, Maloy M, Clurman AG, Stein-Thoeringer CK, Markey KA, Docampo MD, da Burgos Silva M, Khan N, Gessner A, Messina JA, Romero K, Lew MV, Bush A, Bohannon L, Brereton DG, Fontana E, Amoretti LA, Wright RJ, Armijo GK, Shono Y, Sanchez-Escamilla M, Castillo Flores N, Alarcon Tomas A, Lin RJ, Yáñez San Segundo L, Shah GL, Cho C, Scordo M, Politikos I, Hayasaka K, Hasegawa Y, Gyurkocza B, Ponce DM, Barker JN, Perales MA, Giralt SA, Jenq RR, Teshima T, Chao NJ, Holler E, Xavier JB, Pamer EG, van den Brink MRM. Microbiota as predictor of mortality in allogeneic hematopoietic-cell transplantation. N Engl J Med. 2020;382:822–34.
Johansson JE, Ekman T. Gut toxicity during hemopoietic stem cell transplantation may predict acute graft-versus-host disease severity in patients. Dig Dis Sci. 2007;52:2340–5.
Li G, Lin J, Zhang C, Gao H, Lu H, Gao X, Zhu R, Li Z, Li M, Liu Z. Microbiota metabolite butyrate constrains neutrophil functions and ameliorates mucosal inflammation in inflammatory bowel disease. Gut Microbes. 2021;13:1968257.
Rosenfeldt V, Benfeldt E, Valerius NH, Paerregaard A, Michaelsen KF. Effect of probiotics on gastrointestinal symptoms and small intestinal permeability in children with atopic dermatitis. J Pediatr. 2004;145:612–6.
Madsen K, Cornish A, Soper P, McKaigney C, Jijon H, Yachimec C, Doyle J, Jewell L, De Simone C. Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterol. 2001;121:580–91.
Butel MJ. Probiotics, gut microbiota and health. Med Mal Infect. 2014;44:1–8.
de de Moreno Leblanc A, Del Carmen S, Zurita-Turk M, Santos Rocha C, de Guchte M, Azevedo V, Miyoshi A, Leblanc JG. Importance of IL-10 modulation by probiotic microorganisms in gastrointestinal inflammatory diseases. ISRN Gastroenterol. 2011;2011:892971.
Rannikko J, Holmberg V, Karppelin M, Arvola P, Huttunen R, Mattila E, Kerttula N, Puhto T, Tamm Ü, Koivula I, Vuento R, Syrjänen J, Hohenthal U. Fungemia and other fungal infections associated with use of Saccharomyces boulardii probiotic supplements. Emerg Infect Dis. 2021;27:2090–6.
Ladas EJ, Bhatia M, Chen L. The safety and feasibility of probiotics in children and adolescents undergoing hematopoietic cell transplantation. Bone Marrow Transplant. 2016;51:262–6.
Rohlke F, Stollman N. Fecal microbiota transplantation in relapsing clostridium difficile infection. Therap Adv Gastroenterol. 2012;5:403–20.
Bou Zerdan M, Niforatos S, Nasr S, Nasr D, Ombada M, John S, Dutta D, Lim SH. Fecal microbiota transplant for hematologic and oncologic diseases: principle and practice. Cancers. 2022;14:691.
DeFilipp Z, Bloom PP, Torres Soto M, Mansour MK, Sater MRA, Huntley MH, Turbett S, Chung RT, Chen YB, Hohmann EL. Drug-resistant E. coli bacteremia transmitted by fecal microbiota transplant. N Engl J Med. 2019;381:2043–50.
Depommier C, Everard A, Druart C, Plovier H, Van Hul M, Vieira-Silva S, Falony G, Raes J, Maiter D, Delzenne NM, de Barsy M, Loumaye A, Hermans MP, Thissen JP, de Vos WM, Cani PD. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nat Med. 2019;25:1096–103.
Rosean CB, Bostic RR, Ferey JC, Feng T, Azar FN, Tung KS, Dozmorov MG, Smirnova E, Bos PD, Rutkowski MR. Preexisting commensal dysbiosis is a host-intrinsic regulator of tissue inflammation and tumor cell dissemination in hormone receptor–positive breast cancer. Cancer Res. 2019;79:3662–75.
Desai MS, Seekatz AM, Koropatkin NM, Kamada N, Hickey CA, Wolter M, Pudlo NA, Kitamoto S, Terrapon N, Muller A. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell. 2016;167:1339-1353.e21.
Kim MH, Kim H. The Roles of glutamine in the intestine and its implication in intestinal diseases. Int J Mol Sci. 2017;18:1051.
Niihara Y, Miller ST, Kanter J, Lanzkron S, Smith WR, Hsu LL, Gordeuk VR, Viswanathan K, Sarnaik S, Osunkwo I, Guillaume E, Sadanandan S, Sieger L, Lasky JL, Panosyan EH, Blake OA, New TN, Bellevue R, Tran LT, Razon RL, Stark CW, Neumayr LD, Vichinsky EP. Investigators of the phase 3 trial of L-glutamine in sickle cell disease. a phase 3 trial of L-glutamine in sickle cell disease. N Engl J Med. 2018;379:226–35.
Thomsen M, Vitetta L. Adjunctive treatments for the prevention of chemotherapy- and radiotherapy-induced mucositis. Integr Cancer Ther. 2018;17:1027–47.
Sayles C, Hickerson SC, Bhat RR, Hall J, Garey KW, Trivedi MV. Oral glutamine in preventing treatment-related mucositis in adult patients with cancer: a systematic review. Nutr Clin Pract. 2016;31:171–9.
Athar U, Gentile TC. Keratinocyte growth factor. Expert Opin Biol Ther. 2009;9:779–87.
Ido A, Numata M, Kodama M, Tsubouchi H. Mucosal repair and growth factors: recombinant human hepatocyte growth factor as an innovative therapy for inflammatory bowel disease. J Gastroenterol. 2005;40:925–31.
Johnson WF, DiPalma CR, Ziegler TR, Scully S, Farrell CL. Keratinocyte growth factor enhances early gut adaptation in a rat model of short bowel syndrome. Vet Surg. 2000;29:17–27.
Yang H, Wildhaber BE, Teitelbaum DH. Keratinocyte growth factor improves epithelial function after massive small bowel resection. JPEN J Parenter Enteral Nutr. 2003;27:198–206.
Tsirigotis P, Triantafyllou K, Girkas K, Giannopoulou V, Ioannidou E, Chondropoulos S, Kalli T, Papaxoinis G, Pappa V, Papageorgiou E, Economopoulos T, Ladas SD, Dervenoulas J. Keratinocyte growth factor is effective in the prevention of intestinal mucositis in patients with hematological malignancies treated with high-dose chemotherapy and autologous hematopoietic SCT: a video-capsule endoscopy study. Bone Marrow Transplant. 2008;42:337–43.
Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke JD, Serino M, Tilg H, Watson A, Wells JM. Intestinal permeability–a new target for disease prevention and therapy. BMC Gastroenterol. 2014;14:189.
Acknowledgements
Figures created with BioRender.com.
Funding
None.
Author information
Authors and Affiliations
Contributions
EH, PAK, LS, JK, and KG carried out the literature search and wrote the initial drafts of the manuscript. DD coordinated, supervised and guided writing of the draft and design of the figures. SHL conceived the idea and was responsible for the overall writing and final draft of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Haroun, E., Kumar, P.A., Saba, L. et al. Intestinal barrier functions in hematologic and oncologic diseases. J Transl Med 21, 233 (2023). https://doi.org/10.1186/s12967-023-04091-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-023-04091-w