Abstract
Background
The selection of treatment for a patient with breast cancer largely relies on the cancer subtype. However, this process is complicated by changes in tumor biology at relapse. Smoking has been identified as a risk factor for breast cancer. The direct effect of a tobacco component delivered via blood circulation on the mammary gland tissue and subsequent DNA damage have been proposed to explain the association between cigarette smoking and breast cancer carcinogenesis. This postulation is supported by both tissue culture and animal studies demonstrating that the associated DNA damage further alters breast cancer cells, as indicated by an increased proliferative capacity and malignant transformation. In this study, we aimed to explore the relationship between changes in Estrogen receptor (ER), progesterone receptor (PgR), and human epidermal growth factor receptor 2 (HER2) each receptor at recurrence, and smoking and the prognosis after recurrence.
Methods
This retrospective study included 989 patients with primary breast cancer who developed relapse after surgery and 50 patients who underwent regenerative biopsy or surgery from December 2007 to March 2018. ER, PgR, and HER2 expression in the primary and recurrent lesions was evaluated using immunohistochemistry, and the correlations of these expression patterns with smoking history (pack-years) were examined.
Results
When ER was evaluated in recurrent tumors, negative and positive conversions were recognized in 3 (6.0%) and 1 patient (2.0%), respectively. When PgR was evaluated, negative conversion was recognized in 15 patients (30.0%). When HER2 was evaluated, positive conversion was recognized in 6 patients (12.0%). Consequently, we observed a change in the intrinsic subtype in in 5 patients with recurrent tumors (10.0%). Although most clinical factors were not correlated with smoking, a positive conversion of HER2 in recurrence was significantly more frequent among smokers than among non-smokers (p = 0.024).
Conclusions
Biological changes during breast cancer recurrence should be given careful clinical consideration because they affect treatment after recurrence. Our results suggest that smoking may induce increased HER2 expression in recurrent breast tumors.
Similar content being viewed by others
Background
Smoking is a risk factor for the development of breast cancer [1]. One proposed explanation for this link between cigarettes and breast cancer carcinogenesis suggests that a tobacco component is delivered directly to the mammary gland tissue via blood circulation, leading to DNA damage in the mammary gland cells [2, 3]. This potential mechanism is supported by tissue culture and animal experiments in which this damage causes changes in breast cells, such as an increased proliferative capacity and malignant transformation [4,5,6].
When determining the course of breast cancer treatment, it is important to evaluate the status of estrogen receptor (ER), progesterone receptor (PgR), and human epidermal growth factor receptor 2 (HER2) expression. However, changes in the receptor expression patterns over the course of treatment can present clinical challenges. Specifically, these patterns often differ between primary and recurrent tumors, leading to a poor prognosis after recurrence [7, 8]. Therefore, it is necessary to re-evaluate the receptor expression status when a recurrent tumor arises. Given the potential effects of tobacco components on breast cancer cell traits, we hypothesized that smoking may contribute to these changes in receptor expression in recurrent disease. In this study, we aimed to analyze the relationships between changes in each receptor at recurrence, smoking and the subsequent prognosis.
Methods
Patient background
This retrospective study included 989 patients with resectable primary breast cancer who underwent curative resection as the first-line treatment between December 2007 and March 2018 at the Osaka City University Hospital (Osaka, Japan). Patients who received preoperative treatment and those with synchronous or metachronous bilateral breast cancer cases were excluded. At this institution, the patient’s smoking history (cigarettes smoked per day and years of smoking) is routinely recorded at the first visit, which yields the data necessary to calculate the pack-years as the number of cigarettes smoked per day divided by 20, then multiplied by the number of smoking years.
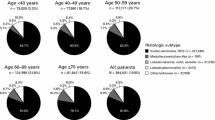
Each breast cancer received a definitive pathological diagnosis and was subjected to immunohistochemistry to determine the expression of ER, PgR, HER2, and Ki-67 (proliferation index). Based on the results, we classified the tumors in accordance with our previous work as hormone receptor-positive breast cancer (HRBC; ER- and/or PgR-positive), HER2-enriched breast cancer (HER2BC; ER−, PgR−, and HER2+), or triple-negative breast cancer (TNBC; ER−, PgR−, and HER2−) [9, 10]. We also applied a Ki-67 cutoff of 14% with reference to a previous report [11]. Tumor stage and resectability were evaluated using ultrasonography (US), computed tomography (CT), and bone scintigraphy.
Patients underwent primary tumor resection via mastectomy or breast-conserving surgery. Sentinel node biopsy or axillary dissection was performed in cases involving axillary nodal surgery; in the former cases, the detection of a sentinel node macrometastasis indicated the need for subsequent axillary dissection. After surgery, the patient was administered postoperative radiotherapy, delivered to the remnant breast, and standard postoperative adjuvant therapy according to the pathological diagnosis of the resected specimen. However, some patients did not receive postoperative treatment because of refusal or a poor general condition. All patients were followed-up via physical examinations, US, CT and bone scintigraphy according to the degree of recurrence risk.
Recurrence occurred in 77 of 989 patients who underwent curative resection. However, 19 of these patients did not undergo biopsy because the recurrent disease involved distant metastasis. This study also included some cases of distant metastasis wherein a biopsy was performed because it was difficult to differentiate the primary cancer of another organ from a distant metastasis of breast cancer. Of the remaining patients with recurrent disease, smoking history were not available for 3 patients. Therefore, we studied the remaining 50 cases (Fig. 1), all of whom underwent biopsy or resection immediately after relapse. No biopsies or resections were performed after the administration of antitumor drug treatment for recurrent disease.
Consort diagram. Recurrence occurred in 77 of 989 patients who underwent curative resection. However, nineteen of them did not undergo biopsy because of distant metastatic recurrence. In this study, such cases are also included. Of the remaining, 3 patients did not know the smoking history, so we studied in the remaining 50 cases
Regarding survival outcomes, progression-free survival (PFS) was defined as the time interval from recurrence to deterioration by treatment started after recurrence or death. Post-recurrence survival (PRS) was defined as the time interval from recurrence to death. The 50 patients with recurrent disease were followed for a median of 2128 days (range, 416-–3789 days) postoperatively.
Statistical analysis
Comparisons between the two groups were performed using the Chi square test. The odds ratio (OR) and 95% confidence intervals (CI) were calculated by the logistic analysis. PFS and PRS were estimated using the Kaplan–Meier method and compared between groups using the log-rank test. The hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using the Cox proportional hazards model. A multivariable analysis was performed using the Cox regression model. All statistical analyses were performed using the JMP software package (SAS, Tokyo, Japan), and statistical significance was defined as a p value of < 0.05.
Ethics statement
This study was conducted at the Osaka City University Graduate School of Medicine, according to the Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK) guidelines. The study protocol involved a retrospectively written plan of research, pathological evaluation, and statistical analysis [12]. The study complied with the provisions of the Declaration of Helsinki, and all patients provided written informed consent for their treatment and data collection. The retrospective protocol was approved by the ethics committee of Osaka City University (approval number #926).
Results
Clinicopathological features
Fifty patients underwent radical surgery without preoperative treatment and a biopsy or resection of a recurrent tumor (Table 1). The median age of these patients was 60 (range, 37–79) years, and the median tumor size at the time of surgery was 21.8 (8.0–45.0). Fourteen patients (28.0%) had a history of smoking before surgery, with a median duration of 30 (1.4–150) pack-years. An evaluation of surgical specimens revealed that seven patients (14.0%) had lymph node metastases, as well as the following distribution of intrinsic subtypes: HRBC, 38 cases (76.0%); HER2BC, 2 (4.0%) cases; and TNBC, 10 (20.0%) cases. All patients with HRBC had a HER2-negative status. Thirteen patients (26.0%) with a pathological diagnosis that suggested a high risk of recurrence received postoperative adjuvant chemotherapy. Eleven patients (22.0%) received postoperative radiotherapy delivered to the remnant breast, and 1 patient (2.0%) received trastuzumab therapy. Moreover, 72% of all patients received endocrine therapy, and this high rate was attributed to the administration of this type of therapy to most patients with HRBC. In contrast, 6 patients (12.0%) did not receive any postoperative treatment.
The median DFS duration was 792 (99–3300) days, and the median age at recurrence was 62 (range 41–86) years. Most biopsied recurrent tumors involved the local or regional lymph nodes, although biopsies were obtained from distant metastases in 5 cases (10.0%), including the lung in 3 cases (6.0%), brain in 1 case (2.0%), and liver in 1 case (2.0%). In 7 patients (14.0%), recurrences were observed in organs that were not biopsied simultaneously (Additional file 1: Table S1), including 3 patients who underwent biopsy of a local recurrence and also presented with lymph node metastasis, lung metastasis, or bone metastasis and 4 patients who underwent biopsy of a regional lymph node recurrence who presented with lung metastasis. No cases involved simultaneous recurrent lesions in 3 or more organs.
We further explored receptor expression in the recurrent tumors via histopathology. Regarding ER, negative conversion was recognized in 3 patients (6.0%) and positive conversion was recognized in 1 patient (2.0%). Regarding PgR, negative conversion was recognized in 15 patients (30.0%). Regarding HER2, positive conversion was recognized in 6 patients (12.0%). Consequently, 5 patients (10.0%) exhibited a change of intrinsic subtype upon recurrence.
Correlation between changes in receptor expression and clinical factors
The potential correlations of these receptor expression changes with clinical features were explored (Table 2). Patients who exhibited a negative PgR conversion were significantly more likely to have received postoperative endocrine therapy (p = 0.003). Patients who experienced a change in ER expression were less likely to have received postoperative radiation therapy, although this correlation was not significant (p = 0.052). No significant correlations were observed between a change in HER2 expression and any clinical factors. We then examined the potential correlations between smoking and clinical factors (Table 3). However, a significant correlation was only observed between a positive conversion of HER2 in recurrence and a history of smoking (p = 0.024). In addition, a univariate analysis with HER2 changes by pack-years showed that the odds ratio increased as pack-years increased (Table 4).
Prognostic analysis based on a change in receptor expression and smoking history
The analysis revealed no significant difference in PFS between smokers and non-smokers (p = 0.102, log-rank; Fig. 2a). A univariate analysis identified significant correlations of chemotherapy after surgery and a change in intrinsic subtype in the recurrent tumor with a poor PFS (p = 0.015, HR = 3.734, 95% CI 1.316–10.115 and p = 0.039, HR = 3.889, 95% CI 1.083–11.236, respectively) (Table 5). However, no factors independently associated with PFS were identified in a multivariate analysis.
Similarly, no significant difference in PRS was identified between smokers and non-smokers (p = 0.140, log-rank; Fig. 2b). Although a univariate analysis identified a biopsied distant metastasis as associated significantly with a poor PRS (p = 0.041, HR = 8.527, 95% CI 1.114–52.010), no significant independent factors were identified in a multivariate analysis (Table 6). In summary, our results do not suggest an association between smoking and the prognosis after relapse.
Discussion
Decisions regarding the selection of breast cancer therapies require an accurate determination of the ER, PgR, and HER2 expression status of the tumor, which are usually determined via biopsy to achieve a definitive diagnosis. However, a biopsy specimen represents only part of lesion and often differs from the surgical specimen. Previous reports describe ER expression concordance rates between biopsy specimens and surgical specimens as high as 92–98% and similarly high PgR concordance rates of 85–97% [13, 14]. However, the reported HER2 concordance rates are slightly lower, at 80–90% [13, 15, 16]. Moreover, anticancer therapy affects the expression of these receptors. In a meta-analysis of patients who underwent neoadjuvant chemotherapy for breast cancer, ER and PgR discordance rates of 2.5–17% and 5.9–51.7%, respectively, were reported [17]. There are reports that it turns out to be often positive, while others report that it often turns negative. Regarding HER2, studies reported discordance rates between biopsy specimens and surgical specimens of 1.3–20% in patients who received neo-adjuvant chemotherapy (NAC) without trastuzumab and of 12–43% in whose who received NAC with trastuzumab. These data suggest that trastuzumab therapy induces a negative HER2 conversion. In our study, therefore, we targeted cases that were preoperative treatment-naïve to address the potential differences between biopsy and surgical specimens and changes due to NAC.
Some reports have described differences in the patterns of receptor expression between surgical specimens and recurrent tumor specimens [7, 8, 18,19,20]. A change in the ER status is observed in approximately 15% of cases, and the numbers of cases with increasing and decreasing expression are roughly equivalent. In contrast, a change in the PgR status is observed in approximately 25–40% of cases, and usually involves decreased expression. Changes in HER2 are observed in approximately 10% of cases, and more frequently tend to involve decreased expression. Consequently, some reports describe a change in breast cancer subtype to TNBC in recurrence, and these cases tend to have a worse prognosis than those with primary TNBC [7, 8]. In our study, we also compared the receptor expression patterns between surgical specimen and corresponding biopsies of recurrent tumors, which involved the local or regional lymph nodes in 90% of cases. The primary tumor type was HRBC in 76.0% of cases, and the frequencies of change in the ER, PgR, and HER2 statuses between the surgical and recurrent specimens were similar to those in previous reports.
In vitro experiments have demonstrated the ability of tobacco components to increase the proliferative capacity and induce malignant transformation in breast cancer cells [4,5,6], and various reports have described an association between ER expression and smoking in clinical practice [21,22,23,24,25,26]. However, few reports have explored the potential relationship between HER2 expression and smoking in breast cancer. Notably, we observed a significant correlation between smoking and a positive conversion of HER2 in our study. Although smoking is a known etiologic factor in lung cancer, an interesting potential correlation between HER2 mutation and lung cancer in never-smokers has attracted clinical attention [27, 28]. However, in vitro experiments have demonstrated the ability of tobacco components to induce HER2 [29] and amplify the expression of EGFR and HER3 [29, 30]. Crosstalk has been identified within the HER family, and potentially the amplification of another HER family member may enhance the expression of HER2 [31, 32]. In the future, it is necessary to examine the biological changes caused by tobacco components in breast cancer cells using immunohistochemical staining, genetic analysis, and protein quantification in vitro.
The choice of treatment after recurrence varied among the cases in our study, as some patients underwent excision of the recurrent lesions and others began anticancer therapy. Consequently, an evaluation of prognosis was challenging. However, we found that a negative hormone receptor conversion, positive HER2 conversion, and change of the intrinsic breast cancer subtype appears to reduce the DFS. However, smokers in our study appeared to have a better DFS and OS, possibly because the switch from ER+/HER2− to ER+/HER2+ breast cancer in most smokers enabled the administration of more effective drug treatment.
This study had a few limitations of note. Particularly, we only obtained data about the smoking history up to surgery, and the use of an interview to collect these data may have introduced bias. Although we agree that the postoperative smoking status is important, some reports suggest that the total smoking history is more important than the current smoking status with respect to carcinogenesis and recurrence [33, 34]. Moreover, we were not able to reach clear conclusions about receptor expression patterns on distant metastases, as most recurrences occurred in local or regional lymph nodes. However, the identification of a correlation between smoking and the positive conversion of HER2 at recurrence suggests that appropriate treatment may not have been administered to patients with distant metastases. We must therefore consider the possible link between smoking and HER2 amplification when evaluating cases in which a biopsy of a distant metastasis cannot be performed.
Conclusions
In conclusion, our results emphasize that biological changes during breast cancer recurrence should receive careful clinical consideration because of the potential effects on treatment after recurrence. However, smoking only appeared to have an effect on HER2 expression patterns after recurrence, but not on survival prognosis.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Abbreviations
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- ER:
-
Estrogen receptor
- HRBC:
-
Hormone receptor-positive breast cancer
- HER2:
-
Human epidermal growth factor receptor 2
- HER2BC:
-
HER2-enriched breast cancer
- HR:
-
Hazard ratio
- NAC:
-
Neo-adjuvant chemotherapy
- PFS:
-
Progression-free survival
- PgR:
-
Progesterone receptor
- PRS:
-
Post-recurrence survival
- REMARK:
-
Reporting Recommendations for Tumor Marker Prognostic Studies
- TNBC:
-
Triple-negative breast cancer
- US:
-
Ultrasonography
References
Dossus L, Boutron-Ruault MC, Kaaks R, Gram IT, Vilier A, Fervers B, Manjer J, Tjonneland A, Olsen A, Overvad K, et al. Active and passive cigarette smoking and breast cancer risk: results from the EPIC cohort. Int J Cancer. 2014;134(8):1871–88.
Ambrosone CB, Kropp S, Yang J, Yao S, Shields PG, Chang-Claude J. Cigarette smoking, N-acetyltransferase 2 genotypes, and breast cancer risk: pooled analysis and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008;17(1):15–26.
Hecht SS. Tobacco smoke carcinogens and breast cancer. Environ Mol Mutagen. 2002;39(2–3):119–26.
Forteza RM, Casalino-Matsuda SM, Falcon NS, Valencia Gattas M, Monzon ME. Hyaluronan and layilin mediate loss of airway epithelial barrier function induced by cigarette smoke by decreasing E-cadherin. J Biol Chem. 2012;287(50):42288–98.
Melendez-Colon VJ, Luch A, Seidel A, Baird WM. Cancer initiation by polycyclic aromatic hydrocarbons results from formation of stable DNA adducts rather than apurinic sites. Carcinogenesis. 1999;20(10):1885–91.
Nishioka T, Kim HS, Luo LY, Huang Y, Guo J, Chen CY. Sensitization of epithelial growth factor receptors by nicotine exposure to promote breast cancer cell growth. Breast Cancer Res. 2011;13(6):R113.
Dieci MV, Barbieri E, Piacentini F, Ficarra G, Bettelli S, Dominici M, Conte PF, Guarneri V. Discordance in receptor status between primary and recurrent breast cancer has a prognostic impact: a single-institution analysis. Ann Oncol. 2013;24(1):101–8.
Liedtke C, Broglio K, Moulder S, Hsu L, Kau SW, Symmans WF, Albarracin C, Meric-Bernstam F, Woodward W, Theriault RL, et al. Prognostic impact of discordance between triple-receptor measurements in primary and recurrent breast cancer. Ann Oncol. 2009;20(12):1953–8.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ, Panel M. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22(8):1736–47.
Takada K, Kashiwagi S, Goto W, Asano Y, Takahashi K, Morisaki T, Takashima T, Tomita S, Hirakawa K, Ohira M. Novel evaluation scale for QOL (QOL-ACD-BP) in preoperative chemotherapy for breast cancer. J Cancer Res Clin Oncol. 2018;144(8):1547–59.
Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard PS, Parker JS, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101(10):736–50.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. Statistics Subcommittee of the NCIEWGoCD: reporting recommendations for tumor marker prognostic studies (REMARK). J Natl Cancer Inst. 2005;97(16):1180–4.
Chen X, Yuan Y, Gu Z, Shen K. Accuracy of estrogen receptor, progesterone receptor, and HER2 status between core needle and open excision biopsy in breast cancer: a meta-analysis. Breast Cancer Res Treat. 2012;134(3):957–67.
Li S, Yang X, Zhang Y, Fan L, Zhang F, Chen L, Zhou Y, Chen X, Jiang J. Assessment accuracy of core needle biopsy for hormone receptors in breast cancer: a meta-analysis. Breast Cancer Res Treat. 2012;135(2):325–34.
Lebeau A, Turzynski A, Braun S, Behrhof W, Fleige B, Schmitt WD, Grob TJ, Burkhardt L, Holzel D, Jackisch C, et al. Reliability of human epidermal growth factor receptor 2 immunohistochemistry in breast core needle biopsies. J Clin Oncol. 2010;28(20):3264–70.
Lee AH, Key HP, Bell JA, Hodi Z, Ellis IO. Concordance of HER2 status assessed on needle core biopsy and surgical specimens of invasive carcinoma of the breast. Histopathology. 2012;60(6):880–4.
van de Ven S, Smit VT, Dekker TJ, Nortier JW, Kroep JR. Discordances in ER, PR and HER2 receptors after neoadjuvant chemotherapy in breast cancer. Cancer Treat Rev. 2011;37(6):422–30.
Thompson AM, Jordan LB, Quinlan P, Anderson E, Skene A, Dewar JA, Purdie CA, Breast Recurrence in Tissues Study G. Prospective comparison of switches in biomarker status between primary and recurrent breast cancer: the Breast Recurrence In Tissues Study (BRITS). Breast Cancer Res. 2010;12(6):R92.
Amir E, Miller N, Geddie W, Freedman O, Kassam F, Simmons C, Oldfield M, Dranitsaris G, Tomlinson G, Laupacis A, et al. Prospective study evaluating the impact of tissue confirmation of metastatic disease in patients with breast cancer. J Clin Oncol. 2012;30(6):587–92.
Nishimura R, Osako T, Okumura Y, Tashima R, Toyozumi Y, Arima N. Changes in the ER, PgR, HER2, p53 and Ki-67 biological markers between primary and recurrent breast cancer: discordance rates and prognosis. World J Surg Oncol. 2011;9:131.
Kawai M, Malone KE, Tang MT, Li CI. Active smoking and the risk of estrogen receptor-positive and triple-negative breast cancer among women ages 20 to 44 years. Cancer. 2014;120(7):1026–34.
Park SY, Palmer JR, Rosenberg L, Haiman CA, Bandera EV, Bethea TN, Troester MA, Viscidi E, Kolonel LN, Olshan AF, et al. A case-control analysis of smoking and breast cancer in African American women: findings from the AMBER Consortium. Carcinogenesis. 2016;37(6):607–15.
Morabia A, Bernstein M, Ruiz J, Heritier S, Diebold Berger S, Borisch B. Relation of smoking to breast cancer by estrogen receptor status. Int J Cancer. 1998;75(3):339–42.
Manjer J, Malina J, Berglund G, Bondeson L, Garne JP, Janzon L. Smoking associated with hormone receptor negative breast cancer. Int J Cancer. 2001;91(4):580–4.
Nishino Y, Minami Y, Kawai M, Fukamachi K, Sato I, Ohuchi N, Kakugawa Y. Cigarette smoking and breast cancer risk in relation to joint estrogen and progesterone receptor status: a case-control study in Japan. Springerplus. 2014;3:65.
Cooper JA, Rohan TE, Cant EL, Horsfall DJ, Tilley WD. Risk factors for breast cancer by oestrogen receptor status: a population-based case-control study. Br J Cancer. 1989;59(1):119–25.
Bu S, Wang R, Pan Y, Yu S, Shen X, Li Y, Sun Y, Chen H. Clinicopathologic Characteristics of Patients with HER2 Insertions in Non-small Cell Lung Cancer. Ann Surg Oncol. 2017;24(1):291–7.
Shan L, Qiu T, Ling Y, Guo L, Zheng B, Wang B, Li W, Li L, Ying J. Prevalence and Clinicopathological Characteristics of HER2 and BRAF Mutation in Chinese Patients with Lung Adenocarcinoma. PLoS ONE. 2015;10(6):e0130447.
Mishra R, Foster D, Vasu VT, Thaikoottathil JV, Kosmider B, Chu HW, Bowler RP, Finigan JH. Cigarette smoke induces human epidermal receptor 2-dependent changes in epithelial permeability. Am J Respir Cell Mol Biol. 2016;54(6):853–64.
O’Donnell RA, Richter A, Ward J, Angco G, Mehta A, Rousseau K, Swallow DM, Holgate ST, Djukanovic R, Davies DE, et al. Expression of ErbB receptors and mucins in the airways of long term current smokers. Thorax. 2004;59(12):1032–40.
Nahta R, Yu D, Hung MC, Hortobagyi GN, Esteva FJ. Mechanisms of disease: understanding resistance to HER2-targeted therapy in human breast cancer. Nat Clin Pract Oncol. 2006;3(5):269–80.
Takada K, Kashiwagi S, Goto W, Asano Y, Morisaki T, Fujita H, Takashima T, Ohsawa M, Hirakawa K, Ohira M. Analysis of HER Family (HER1-4) expression as a biomarker in combination therapy with pertuzumab, trastuzumab and docetaxel for advanced HER2-positive breast cancer. Anticancer Res. 2018;38(4):2285–94.
Pierce JP, Patterson RE, Senger CM, Flatt SW, Caan BJ, Natarajan L, Nechuta SJ, Poole EM, Shu XO, Chen WY. Lifetime cigarette smoking and breast cancer prognosis in the After Breast Cancer Pooling Project. J Natl Cancer Inst. 2014;106(1):359.
Saquib N, Stefanick ML, Natarajan L, Pierce JP. Mortality risk in former smokers with breast cancer: pack-years vs. smoking status. Int J Cancer. 2013;133(10):2493–7.
Acknowledgements
We thank Yayoi Matsukiyo and Tomomi Okawa (Department of Breast and Endocrine Surgery, Osaka City University Graduate School of Medicine) for helpful advice regarding data management.
Funding
This study was supported in part by Grants-in Aid for Scientific Research (Japan Society for the Promotion of Science, KAKENHI, Nos. 19K18067, 26461957, and 17K10559) from the Ministry of Education, Science, Sports, Culture and Technology of Japan.
Author information
Authors and Affiliations
Contributions
All authors were involved in the preparation of this manuscript. KT collected the data and wrote the manuscript. SK, YA, WG, RK, AY, TM, MS, and TT performed the operation and designed the study. KT and SK summarized the data and revised the manuscript. HF, KH, and MO provided a substantial contribution to the study design, performed the operation, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all subjects. This research conformed to the provisions of the Declaration of Helsinki in 2013. All patients were informed of the investigational nature of this study and provided their written, informed consent. The study protocol was approved by the Ethics Committee of Osaka City University (#926).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
The recurrence cases of organs that was not biopsied at the simultaneously.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Takada, K., Kashiwagi, S., Asano, Y. et al. The effect of smoking on biological change of recurrent breast cancer. J Transl Med 18, 153 (2020). https://doi.org/10.1186/s12967-020-02307-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-020-02307-x