Abstract
Background
Individuals with arterial hypertension often have an autonomic nervous system (ANS) imbalance with predominance of sympathetic ANS. This predominance can lead to injury of several organs affecting its functioning. There is evidence that performing high intensity resistance training (RT) with heavier loads and a lower number of repetitions results in lower cardiovascular stress when compared with lighter loads and a higher number of repetitions. However, the effects of different protocols of RT in autonomic modulation are not known. Therefore, the aim of the study was to analyze and compare the effects of different protocols of high intensity of effort RT on autonomic cardiac modulation of hypertensive women.
Methods
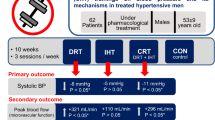
A randomized crossover design clinical trial was conducted with 15 postmenopausal hypertensive women who underwent a control session and two high intensity RT protocols involving 6 and 15 repetition maximum (RM). Heart rate variability (HRV), systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR) and double product (DP) were collected pre, immediately post, 1 h post, and 24 h post each protocol. Repeated-measures ANOVA were used.
Results
SBP was higher for 6RM than control immediately after session (p < 0.05). There were no differences for DBP among protocols (p ≥ 0.05). HR was higher for 15RM than 6RM and control immediately after and 1 h after session (p ≤ 0.05). DP values for 15RM were significantly higher than 6RM and control immediately after the session and remained higher than control 1 h after session (p ≤ 0.05). The indices that compose HRV (rMSSD) were lower after 15RM than 6RM and control (p ≥ 0.05). The parameters of parasympathetic activity (HF) were decreased and sympathetic (LF) activity was increased for 15RM when compared to the 6RM and control session immediately after the exercise session (p ≤ 0.05).
Conclusion
Performing high intensity RT with lower loads and a higher number of repetitions seems to promote acute increases in sympathetic ANS activity, which may be related to cardiovascular stress. On the other hand, heavier load and lower repetition RT did not significantly impact upon autonomic modulation when compared to a control session.
Similar content being viewed by others
Background
Arterial hypertension (AH) is a multifactorial clinical condition characterized by elevated and sustained blood pressure (BP) levels reaching approximately 46% of the US population over 20 years [1]. AH is one of the most important public health problems and is considered one of the main risk factors for cardiovascular diseases [2, 3].
The autonomic nervous system (ANS) has an important role in regulating physiological processes both in normal and pathological conditions [4, 5]. Individuals with AH typically have an ANS imbalance with greater performance and predominance of sympathetic ANS [6,7,8]. In women, this sympathetic predominance is more pronounced with age, possibly as a result of the decrease in estrogen production, especially in the postmenopausal period, which favors the occurrence of AH [9, 10].
Among the techniques used to evaluate ANS activity, heart rate variability (HRV) is a simple and noninvasive measure of autonomic impulses, representing one of the most promising quantitative markers of autonomic modulation. In general, HRV describes the oscillations of the intervals between beats (R–R intervals) that are related to the influence of the ANS on the sinus node [4, 11, 12]. Recent studies showed that resistance training (RT) may promote positive adaptations in the ANS with a consequent increase in HRV as well as a chronic increase in muscle strength and a decrease in BP [13,14,15,16].
Whilst RT is considered effective in positively modulating the ANS, there is a shortage of studies evaluating the impact of different RT protocols on ANS. Understanding these responses would provide guidance for the most efficacious RT prescription for improvement in cardiovascular adaptation while decreasing other cardiovascular risk factors, particularly in populations such as those with AH who it may be advisable to avoid high levels of acute cardiovascular stress. Therefore, the aim of the study was to analyze and compare the effects of different protocols of high intensity of effort RT on hemodynamic parameters and autonomic cardiac modulation of postmenopausal hypertensive women.
Methods
Experimental approach to the problem
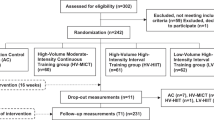
A randomized crossover study was conducted to compare cardiac autonomic modulation and other hemodynamic parameters in hypertensive women, aged 45–69 years. Tests were performed before, immediately after, 1 and 24 h after different protocols of resistance training with high intensity of effort. The study involved the comparison of three conditions: control, resistance training with lighter loads and higher number of repetitions (15 repetitions maximum, 15RM) and resistance training with heavier loads and a lower number of repetitions (six repetitions maximum, 6RM). The selection of participants was performed through the analysis of medical records at the University Hospital where preliminary data were obtained from the candidates for study participation. During the first contact via telephone, it was verified if the participants filled the participation criteria and the participants were invited to an initial visit for presentation, clarifications regarding the methodological procedures and any other doubts that could exist about the progress of the research. The study was approved by the Institutional Research Ethics Committee (Protocol 1,641,089).
Participants
The sample consisted of 15 hypertensive and postmenopausal women, who were regularly enrolled in University Hospital care and who accepted to participate in the study. Exclusion criteria involved: current smoker or user of tobacco products; chronic alcoholism; body mass index (BMI) exceeding 35 kg/m2; hormone replacement therapy; beta-blocker use; use of anti-depressive and/or anxiolytic drugs; recent cardiovascular event such as acute myocardial infarction, stroke or heart failure (≤ 3 months); diabetes; heart failure and/or renal failure; musculoskeletal, untreated joint disease, or other incapacitating disease that could prevent the performance of the protocols. The drugs used to control AH were: diuretics (14 participants), angiotensin-converting enzyme inhibitors (7 participants) and angiotensin II receptor blockers (9 participants). Patients using any class of beta-blockers was excluded because it’s the only drug for AH control that interference on ANS responses in the different protocols [17, 18].
Anthropometric measures
All anthropometric measures were performed using the World Health Organization standardization [19]. Body mass was measured using a portable electronic scale with a capacity of up to 200 kg and with a variation of 0.1 kg (OMRON HBF-214; OMRON Heath Care, Inc, Illinois, USA, 2013). The measurement was performed with the patient positioned in the center of the platform, without support and without making movements, in orthostatic posture, with arms hanging vertical alongside the body. Height was measured using a portable stadiometer with a variation of 0.1 cm (Seca Stadiometer; Seca GmBH & Co, Hamburg, Germany). The participants were instructed to stand barefoot, in an upright position, with their legs extended, feet parallel and heels together aligned with the door. BMI was calculated as the ratio between mass and the square of the participant’s height (kg/m2).
Strength testing
Initial familiarization sessions were performed in order to adapt the participants to the practice and execution of the RT exercises. The exercises used were bench press, lat pull down and 45̊ leg press. The participants were individually supervised by at least two researchers on the correct execution of each exercise. During the familiarization session, each participant performed three sets of 12–15 repetitions with the minimum possible load in each exercise as warm-up. After 3-day intervals, the participants returned to University Hospital to perform the repetition maximum tests. The 15RM test started with a warm-up of 12 repetitions at a self-selected comfortable load. After warm-up, the participants performed up to five attempts with progressive load increases until the participant could not complete the 16th repetition for each of the proposed exercises. The participants were allowed to rest 5 min between each attempt. Following a period of at least 3 days each participant returned to the University Hospital for the 6RM test. The test started with a warm-up of 12 repetitions at a comfortable load. After the warm-up period, up to five attempts with progressive load increase were performed until the participant could not complete the 7th repetition for each of the proposed exercises. Five minutes of rest were allowed between each attempt.
Experimental protocol
After determination of the loads of 6RM and 15RM, the participants performed three different experimental protocols: a control session, a RT session with 6RM, and a RT session with 15RM. The order of execution of the sessions was performed randomly by lot. A period of 3 days was given between each session. The protocols were performed at the same time of day (8–10 am) and in a room with controlled temperature (22 °C), in order to avoid the influence of the circadian cycle and external conditions. The participants were instructed to fast for 8 h, to avoid consumption of alcohol and stimulants (coffee, teas, soft drinks, etc.) 24 h before each test session, to not perform strenuous physical activities 48 h previous to the tests and to follow similar routines for all sessions. A food record was given to each participant to record the time, quantities and preparation of each food consumed the day before the first test. Then they were oriented to follow the same pattern in the days before the other sessions.
Upon arrival at the University Hospital the participants were referred to the clinical research laboratory and were advised to remain in the supine position for 10 min. After this period, systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured using an oscillometric device (OMRON, model HEM-705CP; OMRON Heath Care, Inc, Illinois, USA). Heart Rate (HR) and HRV were collected using a heart rate monitor (Polar® V800, Electro Oi, Finland) using consecutive heart rate intervals (RR interval) for 10 min. During this period, the participants were oriented to remain in the supine position, avoid any movement, remain silent, do not sleep and maintain spontaneous breathing. After resting measures, participants were given 30 g of maltodextrin diluted in 300 mL of potable water.
The participants assigned to the sessions of 6RM or 15RM performed the three exercises already mentioned (lat pulldown, barbell bench press and 45° leg press) in three sets of 6RM or 15RM depending on the protocol chosen for the day. The exercises were selected following a minimal dose approach, based on multi-joint exercises [20, 21]. Before each session, 10 repetitions were performed at 30% of the 6RM load in each exercise as warm up. The participants were oriented to training to momentary concentric failure, as previously defined to control effort between conditions [22]. During training, the loads were adjusted between each set to allow momentary concentric failure to occur in the required repetition range (6 or 15RM). The participants were advised to perform the exercises with a controlled repetition duration, taking 2–3 s for each phase of movement and no pauses between muscle actions. The rest intervals between sets and exercises lasted for 2 min. Immediately after the training sessions, HRV, SBP, DBP and double product (DP) were collected. Two other measures were performed: 1 and 24 h after the session, always following the methodology adopted in the initial resting data collection. During the control session the participants followed the same procedures, but substituted the RT session for 20 min of rest in the laboratory. The time was stipulated according to the average duration of the RT sessions.
Heart rate variability analysis
After completion of three test sessions, data obtained from each participant was transferred from the heart rate monitor through a transmission cable supplied by the device. Data processing and analysis were performed using Kubios HRV 3.0.2 software (© Kubios Oy, Finland). Artifacts such as peaks or discrepant intervals were manually extracted to correct possible errors in the values analyzed. The parts of greater stability of the signal were selected for the analyzes, which included at least 256 consecutive beats [4]. The analyzes were made from linear time domain models: rMSSD (the square root of the mean squared differences of successive R–R intervals), and in the frequency domain, through the spectral analysis: low frequency components (LF) being representative of the sympathetic component of the system, high frequency (HF) being representative of the parasympathetic component of the system and the ratio LF/HF representing the sympatho-vagal balance. The HRV was also analyzed by nonlinear models from the Approximate Entropy (ApEn) analysis, which enabled the quantification of the sympathetic and parasympathetic components of the autonomic modulation of the heart rate.
Data analysis
Data are presented as mean ± standard deviation. The values for the HRV, SBP, DBP and DP before and after the three experimental sessions were compared by repeated measures ANOVA with a 3 × 4 (protocol × time). If necessary, multiple comparisons with confidence adjustment by the Bonferroni procedure were used as post hoc analyses. The analyses were performed with IBM SPSS Statistics 21 software (SPSS Inc., Chicago, Illinois, USA). The main factors were the protocol (control, 6RM and 15RM) and the time (rest, after the session, 1 h after and 24 h after). The alpha value of p ≤ 0.05 was considered significant.
Results
All participants completed the three protocols. The characteristics of the participants are presented in Table 1. According to the results of the randomization by lot, three women performed the control session first, nine of the 6RM session, and three the15RM session. The volume of work performed (sets × repetitions × load) in the different protocols are present in Table 2.
Blood pressure
The SBP and DBP data before and after the different RT protocols (control, 6RM and 15RM) are described in Table 3. Rest values were similar for all protocols (p ≥ 0.05). Compared with the resting values, there was an increase in SBP for the 6RM protocol immediately after RT (128 ± 17 vs. 140 ± 17 mmHg; p ≤ 0.05). There was no significant difference in DBP values immediately after RT between groups (78 ± 10 vs. 78 ± 11 mmHg, p ≥ 0.05). There were no differences in blood pressure between protocols at any other time point.
Heart rate
The HR data before and after the control, 6RM and 15RM protocols are described in Table 3. The results show a significantly higher HR after 6RM in comparison to control immediately after the exercise session: (76.24 ± 9.35 bpm vs 65.98 ± 7.26 bpm; p < 0.05). Heart rate was significantly higher, immediately (85.32 ± 13.21 bpm), and 1 h after (73.82 ± 11.23 bpm) in the 15RM protocol when compared to control (65.98 ± 7.26 and 6404 ± 8.26 bpm); and 6RM (76.24 ± 9.35 and 68.59 ± 8.66).
Double product
The DP data before and after the different protocols (control, 6RM and 15RM) are described in Table 3. The results of the DP show significant differences in both 6RM: (10,718.28 ± 2090.03) and 15RM (11,769.10 ± 2783.33) immediately after the session in comparison to the control (8650.36 ± 1477.97); p < 0.05. The values for 15RM were significantly higher than both 6RM and control immediately after the session and 1 h after the session (p < 0.05). Within groups comparison revealed that there was a significant difference for groups 6RM and 15RM between baseline and immediately after exercise (p < 0.05).
Heart rate variability
The HRV indices are described in Table 4 and in Figs. 1, 2 and 3. Rest values were similar for all protocols in all variables (p ≥ 0.05). The 15RM protocol resulted in significantly lower values of rMSSD index immediately after the exercise session when compared to the 6RM and control protocols (p < 0.05). For the LF index there were no significant differences between the protocols of 6RM and control, however the 15RM protocol resulted in significantly higher values compared to control 1 h after session and to 6RM immediately after session (p < 0.05). In the HF index there was a contrary response; 15RM protocol resulted in significantly lower values when compared to the group control and 6RM (p < 0.05). The measurements of the LF/HF ratio showed a significant increase in the values for the 15RM protocol in relation to the others immediately after the session (p < 0.05). Within groups comparison revealed that there was a significant difference in the LF and HF for 15RM protocol immediately after exercise when compared to baseline (p < 0.05).
Changes observed in the low frequency values after the control sessions (triangles), 6RM (lozenges), 15RM (squares), where the time 1 rest, time 2 after the intervention, time 3 one hour after the intervention and time 4 twenty hours after the intervention. *Significantly different from pre-intervention (p ≤ 0.05). †Significantly different from the control session (p ≤ 0.05). ‡ Significantly different from the 6RM session (p ≤ 0.05)
Changes observed in the high frequency values after the control sessions (triangles), 6RM (lozenges), 15RM (squares), where the time 1 rest, time 2 after the intervention, time 3 one hour after the intervention and time 4 twenty hours after the intervention. *Significantly different from pre-intervention (p ≤ 0.05). †Significantly different from the control session (p ≤ 0.05). ‡ Significantly different from the 6RM session (p ≤ 0.05)
Changes observed in the ratio low frequency/high frequency values after the control sessions (triangles), 6RM (lozenges), 15RM (squares), where the time 1 rest, time 2 after the intervention, time 3 one hour after the intervention and time 4 twenty hours after the intervention. †Significantly different from the control session (p ≤ 0.05). ‡Significantly different from the 6RM session (p ≤ 0.05)
Discussion
The results of the present study suggest that the performance of a session of high intensity of effort RT using lighter loads and a higher number of repetitions (15RM) promoted greater changes in cardiovascular parameters such as DP and HR, indicating greater cardiovascular stress, when compared to 6RM and control. On the other hand, the performance of a high intensity of effort RT session using heavier loads and fewer repetitions (6RM) did not change the analyzed cardiovascular parameters when compared to a control condition. Therefore, despite the two protocols involving high intensity of effort, the heavier load and the fewer repetition protocol (6RM) induced lower cardiovascular stress and therefore might be considered a safer alternative, particularly for those with AH.
The use of HRV parameters as an indication of cardiovascular risk is already well established [4]. However, its relationship with the practice of RT in people with hypertension is not well understood. Some authors, such as Lima et al. [23] and Rezk et al. [24], suggest that RT with heavier loads leads to an increase in sympathetic activation due to the greater mechanical overload in the vascular system [25], with consequent decrease in HRV. However, our results showed that HRV components that indicate sympathetic activation were greater after RT performed at lighter loads and a higher repetition range (15RM). According to our results, immediately after the 15RM protocol, there was an increase in the sympathetic predominance, as demonstrated by the variables LF and LF/HF, and a decrease in the parasympathetic predominance as demonstrated by the rMSSD and HF variables. Regarding HR and DP, the values for 15RM were greater than the control and 6RM protocols. On the other hand, the 6RM protocol did not result in significant changes in HRV when compared to the control condition. This suggests that load might not influence sympathovagal balance. Other variables such as total work volume and time under tension might be related to the sympathetic activation system and consequent increase in cardiovascular risk, as previously suggested [23, 24].
Despite the recent evidence presenting RT as an alternative for the treatment of several comorbidities, including cardiovascular diseases [26, 27], its prescription is often neglected for patients with AH in many guidelines [28, 29]. When RT is recommended, the guidance is to perform it using lighter loads and a higher number of repetitions, arguing that heavier load RT would not be safe [30,31,32]. Our results challenge this suggestion, since after RT using heavier loads, the responses of variables such as BP and HRV were similar to those at rest. On the other hand, the practice of RT with lighter loads resulted in an increase in DP response and a decrease in HRV immediately after its execution, with these changes persisting even 1 h after the session end. Chronic studies are warranted to analyze the long-term effect of different RT protocol on cardiovascular function in order to test if this acute effects translate into chronic results.
RT might have several benefits for patients with hypertension, such as decreasing resting BP [26, 27, 33] and increasing muscle strength. As for the last, it has been previously reported that higher levels of muscle strength are associated with lower mortality rates both in the general population [34,35,36], and in people with AH [37]. Therefore, increasing muscle strength might be an important aim of RT protocols. Considering that previous studies showed that training with a higher or lower number of repetitions results in similar strength gains, when performed to failure [38,39,40,41], and further, even microvascular adaptations appear to be similar whether using heavier or lighter loads [42] the choice of protocol might be based on other aspects, such as safety and discomfort. In this regard, previous studies reported that the practice of RT with lighter loads and greater number of repetitions generates greater discomfort when compared to RT with heavier loads and fewer repetitions [39, 43]. Moreover, previous studies have shown that performing RT with heavier loads and a lower number of repetitions resulted in smaller increases in blood pressure and pulse rate during training when compared with training at lighter loads and higher number of repetitions [44,45,46]. When combined with these previous findings, our results suggest that the protocols with a heavier load and lower repetitions might be recommended to promote increases in muscle strength and improve health parameters in hypertensive patients while resulting in a reduced cardiovascular overload.
Conclusion
In conclusion, performing RT with lower loads and a higher number of repetitions seems to promote acute increases in sympathetic ANS activity, which may be related to cardiovascular stress. On the other hand, heavier load and lower repetition RT did not significantly impact upon autonomic modulation when compared to a control session. The study is not without limitations, such as, the absence of BP and HRV measurement during the protocols. However, there are reasonable amounts of evidence comparing different protocols on BP during exercise, as previously cited. As for HRV, it is not possible to reliably measure it during exercise by currently available methods; however, it is reasonable to suggest that, if it is altered after the interruption of the exercises, similar dynamics might be seen during exercise. Future studies should confirm if the present findings are reproduced in different populations and also evaluate the long term effects of different protocols in order to allow a better insight into the risk–benefit ratio of such approaches with respect to health outcomes and adverse events.
Abbreviations
- AH:
-
arterial hypertension
- BP:
-
blood pressure
- ANS:
-
autonomic nervous system
- HRV:
-
heart rate variability
- R–R intervals:
-
intervals between beats
- RT:
-
resistance training
- RM:
-
repetitions maximum
- BMI:
-
body mass index
- SPB:
-
systolic blood pressure
- DPB:
-
diastolic blood pressure
- HR:
-
heart rate
- DP:
-
double product
- rMSSD:
-
square root of the mean squared differences of successive R–R intervals
- LF:
-
low frequency
- HF:
-
high frequency
- LF/HF:
-
ratio low frequency high frequency
- ApEn:
-
approximate entropy
References
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–248.
Malachias M. 7th Brazilian guideline of arterial hypertension: presentation. Arquivos brasileiros de cardiologia 2016; 107:XV-XIX.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Task Force of the European Society of Cardiology the North American Society of Pacing Electrophysiology. Heart rate variability standards of measurement, physiological interpretation, and clinical use. Eur Heart J. 1996;17(3):354–81.
Lakusic N, Mahovic D, Kruzliak P. Changes in heart rate variability after coronary artery bypass grafting and clinical importance of these findings. BioMed Res Int. 2015;2015:680515.
Terathongkum S, Pickler RH. Relationships among heart rate variability, hypertension, and relaxation techniques. J Vasc Nurs. 2004;22(3):78–82.
Konrady AO, Rudomanov OG, Yacovleva OI, Shlyakhto EV. Power spectral components of heart rate variability in different types of cardiac remodelling in hypertensive patients. Med Sci Monit. 2001;7(1):58–63.
Caetano J, Delgado Alves J. Heart rate and cardiovascular protection. Eur J Intern Med. 2015;26(4):217–22.
Kim JM, Kim TH, Lee HH, Lee SH, Wang T. Postmenopausal hypertension and sodium sensitivity. J Menopausal Med. 2014;20(1):1–6.
Xue B, Johnson AK, Hay M. Sex differences in angiotensin II- and aldosterone-induced hypertension: the central protective effects of estrogen. Am J Physiol Regul Integr Comp Physiol. 2013;305(5):R459–63.
Aubert AE, Seps B, Beckers F. Heart rate variability in athletes. Sports Med. 2003;33(12):889–919.
Pumprla J, Howorka K, Groves D, Chester M, Nolan J. Functional assessment of heart rate variability: physiological basis and practical applications. Int J Cardiol. 2002;84(1):1–14.
Forte R, De Vito G, Figura F. Effects of dynamic resistance training on heart rate variability in healthy older women. Eur J Appl Physiol. 2003;89(1):85–9.
Figueroa A, Kingsley JD, McMillan V, Panton LB. Resistance exercise training improves heart rate variability in women with fibromyalgia. Clin Physiol Funct Imaging. 2008;28(1):49–54.
Gerage AM, Forjaz CL, Nascimento MA, Januario RS, Polito MD, Cyrino ES. Cardiovascular adaptations to resistance training in elderly postmenopausal women. Int J Sports Med. 2013;34(9):806–13.
Nicolino J, Ramos D, Leite MR, Rodrigues FM, de Alencar Silva BS, Tacao GY, et al. Analysis of autonomic modulation after an acute session of resistance exercise at different intensities in chronic obstructive pulmonary disease patients. Int J Chronic Obstr Pulm Dis. 2015;10:223–9.
Sandrone G, Mortara A, Torzillo D, La Rovere MT, Malliani A, Lombardi F. Effects of beta blockers (atenolol or metoprolol) on heart rate variability after acute myocardial infarction. Am J Cardiol. 1994;74(4):340–5.
Cowan MJ, Pike K, Burr RL, Cain KC, Narayanan SB. Description of time- and frequency- domain-based measures of heart rate variability in individuals taking antiarrhythmics, beta blockers, calcium channel blockers, and/or antihypertensive drugs after sudden cardiac arrest. J Electrocardiol. 1993;26(Suppl):1–13.
WHO (World Health Organization). Physical status: the use and interpretation of anthropometry Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995; 854:1–452.
Gentil P, Fisher J, Steele J. A review of the acute effects and long-term adaptations of single- and multi-joint exercises during resistance training. Sports Med. 2016;47(5):843–55.
Fisher JP, Steele J, Gentil P, Giessing J, Westcott WL. A minimal dose approach to resistance training for the older adult; the prophylactic for aging. Exp Gerontol. 2017;99:80–6.
Steele J, Fisher J, Giessing J, Gentil P. Clarity in reporting terminology and definitions of set endpoints in resistance training. Muscle Nerve. 2017;56(3):368–74.
Lima AHR, Forjaz CL, Silva GQ, Menêses AL, Silva AJ, Ritti-Dias RM. Efeito agudo da intensidade do exercício de força na modulação autonômica cardíaca pós-exercício. Arquivos brasileiros de cardiologia. 2011;96:498–503.
Rezk CC, Marrache RC, Tinucci T, Mion D Jr, Forjaz CL. Post-resistance exercise hypotension, hemodynamics, and heart rate variability: influence of exercise intensity. Eur J Appl Physiol. 2006;98(1):105–12.
Mitchell JHJB. Wolffe memorial lecture. Neural control of the circulation during exercise. Med Sci Sports Exer. 1990;22(2):141–54.
Kelley GA, Kelley KS. Progressive resistance exercise and resting blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2000;35(3):838–43.
Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58(5):950–8.
Gabb GM, Mangoni AA, Anderson CS, Cowley D, Dowden JS, Golledge J, et al. Guideline for the diagnosis and management of hypertension in adults—2016. Med J Aust. 2016;205(2):85–9.
Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. ACC/AHA guideline on the assessment of cardiovascular risk. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013.
Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA. American college of sports medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36(3):533–53.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC practice guidelines for the management of arterial hypertension. Blood Press. 2014;23(1):3–16.
Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L, et al. The 2015 Canadian hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2015;31(5):549–68.
Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(1):e004473.
Ruiz JR, Sui X, Lobelo F, Morrow JR Jr, Jackson AW, Sjostrom M, et al. Association between muscular strength and mortality in men: prospective cohort study. BMJ. 2008;337:a439.
Garcia-Hermoso A, Cavero-Redondo I, Ramirez-Velez R, Ruiz JR, Ortega FB, Lee DC, et al. Muscular strength as a predictor of all-cause mortality in an apparently healthy population: a systematic review and meta-analysis of data from approximately 2 million men and women. Arch Phys Med Rehabil. 2018. https://doi.org/10.1016/j.apmr.2018.01.008
Dankel SJ, Loenneke JP, Loprinzi PD. Determining the importance of meeting muscle-strengthening activity guidelines: is the behavior or the outcome of the behavior (strength) a more important determinant of all-cause mortality? Mayo Clin Proc. 2016;91(2):166–74.
Artero EG, Lee DC, Ruiz JR, Sui X, Ortega FB, Church TS, et al. A prospective study of muscular strength and all-cause mortality in men with hypertension. J Am Coll Cardiol. 2011;57(18):1831–7.
Assuncao AR, Bottaro M, Ferreira-Junior JB, Izquierdo M, Cadore EL, Gentil P. The chronic effects of low- and high-intensity resistance training on muscular fitness in adolescents. PLoS ONE. 2016;11(8):e0160650.
Fisher JP, Steele J. Heavier and lighter load resistance training to momentary failure produce similar increases in strength with differing degrees of discomfort. Muscle Nerve. 2017;56(4):797–803.
Fisher J, Steele J, Smith D. High- and low-load resistance training: interpretation and practical application of current research findings. Sports Med. 2017;47(3):393–400.
Mitchell CJ, Churchward-Venne TA, West DW, Burd NA, Breen L, Baker SK, et al. Resistance exercise load does not determine training-mediated hypertrophic gains in young men. J Appl Physiol. 2012;113(1):71–7.
Holloway TM, Morton RW, Oikawa SY, McKellar S, Baker SK, Phillips SM. Microvascular adaptations to resistance training are independent of load in resistance trained young men. Am J Physiol Regul Integr Comp Physiol. 2018;315(2):R267–73. https://doi.org/10.1152/ajpregu.00118.2018.
Stuart C, Steele J, Gentil P, Giessing J, Fisher JP. Fatigue and perceptual responses of heavier- and lighter-load isolated lumbar extension resistance exercise in males and females. Peer J. 2018;6:e4523.
Gjovaag T, Hjelmeland AK, Oygard JB, Vikne H, Mirtaheri P. Acute hemodynamic and cardiovascular responses following resistance exercise to voluntary exhaustion. Effects of different loadings and exercise durations. J Sports Med Phys Fitness. 2016;56(5):616–23.
Gjovaag TF, Mirtaheri P, Simon K, Berdal G, Tuchel I, Westlie T, et al. Hemodynamic responses to resistance exercise in patients with coronary artery disease. Med Sci Sports Exer. 2016;48(4):581–8.
Fleck SJ, Dean LS. Resistance-training experience and the pressor response during resistance exercise. J Appl Physiol. 1987;63(1):116–20.
Authors’ contributions
PG and JAC designed the study. AFV and JAC performed the experiment. AFV, JAC and PG analysed the data and wrote the manuscript. TVJ, PCVJ, JPF and JS participated in the design of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The data of the current study are available at request for scientists wishing to use them with kind full permission.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All participants read and signed an informed consent document with the description of the testing procedures. The study was approved by the Institutional Research Ethics Committee (Protocol 1,641,089), and conformed to standards for the use of human subjects.
Funding
This research was conducted with authors’ institutional founds.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vale, A.F., Carneiro, J.A., Jardim, P.C.V. et al. Acute effects of different resistance training loads on cardiac autonomic modulation in hypertensive postmenopausal women. J Transl Med 16, 240 (2018). https://doi.org/10.1186/s12967-018-1615-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-018-1615-3