Abstract
Background
Physical activity referral schemes (PARS) are complex multicomponent interventions that represent a promising healthcare-based concept for physical activity (PA) promotion. This systematic review and narrative synthesis aimed to identify the constitutive components of PARS and provide an overview of their effectiveness.
Methods
Following a published protocol, we conducted a systematic search of PubMed, Scopus, Web of Science, CINAHL, ScienceDirect, SpringerLink, HTA, Wiley Online Library, SAGE Journals, Taylor & Francis, Google Scholar, OpenGrey, and CORE from 1990 to January 2023. We included experimental, quasi-experimental, and observational studies that targeted adults participating in PARS and reported PA outcomes, scheme uptake, or adherence rates. We performed an intervention components analysis using the PARS taxonomy to identify scheme components and extracted data related to uptake, adherence, and PA behavior change. We combined these to provide a narrative summary of PARS effectiveness.
Results
We included 57 studies reporting on 36 PARS models from twelve countries. We identified 19 PARS components: a patient-centered approach, individualized content, behavior change theory and techniques, screening, brief advice, written materials, a written prescription, referral, baseline and exit consultation, counselling support session(s), PA sessions, education session(s), action for non-attendance, structured follow-up, a PA network, feedback for the referrer, and exit strategies/routes. The PARS models contained a mean of 7 ± 2.9 components (range = 2–13). Forty-five studies reported PA outcome data, 28 reported uptake, and 34 reported adherence rates. Of these, approximately two-thirds of studies reported a positive effect on participant PA levels, with a wide range of uptake (5.7–100.0%) and adherence rates (8.5–95.0%).
Conclusions
Physical activity referral scheme components are an important source of complexity. Despite the heterogeneous nature of scheme designs, our synthesis was able to identify 19 components. Further research is required to determine the influence of these components on PARS uptake, adherence, and PA behavior change. To facilitate this, researchers and scheme providers must report PARS designs in more detail. Process evaluations are also needed to examine implementation and increase our understanding of what components lead to which outcomes. This will facilitate future comparisons between PARS and enable the development of models to maximize impact.
Similar content being viewed by others
Background
Chronic non-communicable diseases (NCDs) present a challenge to public health and modern healthcare systems [1]. Physical activity (PA) interventions offer a window of opportunity for NCD prevention and management, [2] particularly in primary care [3, 4]. This is because healthcare professionals are considered to be a credible source of information about the well-established health-enhancing benefits of PA [5]. In 2016, 39 billion outpatient healthcare visits were made globally [6], which, if utilized concurrently for PA promotion, might have reached an estimated 1.4 billion insufficiently inactive adults [7]. Physical activity healthcare interventions, such as brief advice and physical activity referral schemes (PARS), are considered viable approaches that enable healthcare professionals to encourage patients to be more active [4, 8, 9]. At the system level, PARS offer a practical way for healthcare professionals to harness the role of PA in reducing the burden of NCDs and help overcome fragmented efforts in PA promotion. At the individual level, referral schemes are suggested to improve not only PA of participants, but also their depression levels [10, 11], insulin sensitivity [12], body composition, and cardiometabolic risk factors [13]. Additionally, participants have reported a sense of belonging and social inclusion [14].
Physical activity referral schemes are widespread, complex interventions that involve the coordinated efforts of healthcare and exercise professionals in an individual’s journey to achieve PA behavior change. They are comparable to other healthcare referrals, which are defined as “the direction of an individual to the appropriate facility or specialist in a health system or network of service providers to address the relevant health needs” [4]. In PARS, individuals who have or are at risk of NCDs and have a health need in terms of insufficient PA are directed to appropriate PA specialists, facilities, or activities. These types of interventions offer an opportunity to break the ice between PA offers and inactive patients. As such, the World Health Organization advocates offering brief PA interventions, including referral pathways, in primary care to support PA behavior change [7]. Despite this endorsement, PARS have only demonstrated a modest impact on PA levels [15]. Current understanding of effectiveness is limited by the dominance of UK-based studies, which are characterized by high heterogeneity [16]. This has resulted in a lack of understanding about what works [17]. There is a need to better define different PARS models, so that reviews of evidence can distinguish between distinct designs (e.g., UK versus Swedish models). However, even with small individual-level effects, great benefits can be seen at the population level when interventions are disseminated at scale [18]. Thus, attention has been directed to embedding PARS into healthcare systems; for example, the European Physical Activity on Prescription model (EUPAP) project aims to establish the Swedish model in Belgium, Denmark, Germany, Italy, Lithuania, Malta, Portugal, Romania, and Spain [19].
Physical activity referral schemes incorporate various components to elicit behavior change [8, 20]. The Swedish model includes five components: a patient-centered approach, evidence-based PA recommendations, a written prescription, follow-up, and a community-based network [20, 21]. Schemes that incorporate these components are known to be effective, but it is unclear whether some components produce more favorable results than others [11]. Previous systematic reviews have called attention to PARS components [15], especially the component-effectiveness relationship [11] that is recognized as a researchable link in the complex intervention field [22, 23]. Complex intervention understanding and research can be approached by treating an intervention as a uniform package, “downplaying complexity,” or as an intervention composed of components, “recognizing complexity” [22]. At the systematic review level, PARS effectiveness has been examined as a complete package [10, 11, 15, 24], pooling only effect sizes and discounting intervention components. Other systematic reviews have explored PARS effectiveness in terms of scheme characteristics (referral reason and follow-up) [25, 26], but this is different from examining components. Components are single, active parts that comprise the entire PARS [22, 27] or guiding operational principles at scheme level [28], such as counseling using a patient-centered approach [20]. In contrast, PARS characteristics include setting, scheme length, and provider profession. While we acknowledge that complexity is multifaceted [29] and PARS characteristics may impact effectiveness [25], in this review, we have focused only on components as a source of complexity. The identification of components can enable the future investigation of their relative impact on effectiveness, creating useful knowledge for program developers and decision-makers [22, 29].
Review question
As per our previously published protocol [28], we planned to examine PARS by reviewing the design of interventions to identify their constitutive components (Review Question 1) and further analyze their impact on effectiveness in terms of PA, uptake, and adherence (Review Question 2). In this paper, we focus on the first question by providing an overview of components that make up PARS models and information on their characteristics. Additionally, we present a narrative summary of the evidence of effectiveness.
Methods
This systematic review was conducted by following the Cochrane Handbook for Systematic Reviews of Interventions [30] and reported by adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [31] and Synthesis without meta-analysis (SwiM) [32] guidelines. The methods were pre-registered in the protocol [28] and are briefly described here.
Eligibility criteria
Eligible studies were those that investigated PARS initiated in a primary or secondary healthcare setting; targeted a population aged ≥ 16 years; and reported PA, uptake, or adherence outcomes. We considered all interventions labeled as PARS, exercise referral schemes, or exercise on prescription or any similar intervention, such as PA counselling that included at least some form of documentation, such as a prescription or referral form. Advice only, exercise/PA only, or combined lifestyle intervention studies that included other health behaviors in addition to PA were excluded. We included experimental, quasi-experimental, and observational studies that were published in English or German and reported the outcomes of interest, irrespective of the type of outcome measurement, methodological quality, comparison group, and follow-up duration.
Search and study selection
We conducted systematic searches in Scopus, PubMed, Web of Science, CINAHL, ScienceDirect, SpringerLink, HTA, Wiley Online Library, SAGE Journals, Taylor & Francis, Google Scholar, OpenGrey, and CORE for articles published since 1990 (Additional file 1), combined with search methods such as citation and hand searching. The initial search was conducted by one author (EM) in June 2020 and updated on January 31, 2023 (Additional file 1). Duplicates were removed, and the remaining articles were downloaded into Citavi V.6 (Swiss Academic Software). Titles and abstracts were screened independently by one reviewer (EM) and a pair of reviewers (IN, AW). One reviewer (EM) screened all full texts. An independent second full-text screening was distributed among the team (AW, IN, JS). The extent of agreement was measured using Cohen’s kappa, and divergences were resolved via discussion.
Data extraction and items
Reports on the same study were grouped together, and data on study characteristics, PARS content (characteristics and components), and effectiveness outcomes (PA, uptake, and adherence) were extracted. A single reviewer (EM) extracted the data into a customized Microsoft Excel spreadsheet (Microsoft Corporation, Washington, USA), with a second reviewer (JS) extracting 15% of included studies to check for accuracy.
Scheme content
Data were extracted at the scheme level using the PARS taxonomy, a classification system to document, audit, monitor, and report such programs [16]. We contacted twelve primary investigators to clarify questions or ask for support in the form of additional information, and half of them replied.
Effectiveness outcomes
We extracted total PA and also moderate to vigorous PA, leisure time PA, and walking when available. Additionally, we extracted scheme uptake and adherence rates. When the primary investigators did not explicitly define uptake or adherence, we extracted data that fit our predefined uptake definition, that is, attendance at the first PARS activity after receiving a referral or prescription or the extent to which the prescribed activities or enrolled programs were completed [28].
Risk of bias in individual studies
This systematic review was solely focused on content analysis to identify PARS components (first review question [28]) and did not include a meta-analysis of the effects of components. A risk-of-bias assessment is not included in this review but is being prepared for a subsequent analysis related to the second review question, that is, which of the identified components has the potential to maximize scheme effectiveness in terms of PA level, uptake, and adherence rates [28].
Synthesis methods
Data were synthesized following the principles of the first stage of intervention component analysis (ICA), which is intended to compare interventions in terms of their similarities and differences [33]. The first stage of ICA involves two parallel processes: (a) content analysis and (b) narrative effectiveness synthesis.
-
(a)
We combined the inductive ICA approach to content analysis with a deductive approach using levels one and two of the PARS taxonomy, scheme classification, and characteristics [16]. The use of this taxonomy reduced the chances of the arbitrary identification of the components given that at least 43 experts from research, PARS provision, healthcare, and policy-making backgrounds were involved in its creation.
Two authors (CLH and SM) conducted the content analysis, using NVIVO20 (QSR International, Melbourne, Australia) to organize the data. The analysis was checked by a third reviewer (EM). Given that PARS do not follow a standard design, we mapped the referral routes using cross-functional flowcharts in Lucidchart software [30] to aid in the comparison and identify patterns and structural components as per our protocol [23].
-
(b)
Along with the identified components, effectiveness data were synthesized and presented in a tabular format. Physical activity outcomes were displayed by employing vote counting; that is, for each included study, we indicated the direction of the effect regardless of statistical significance [34]. Scheme uptake and adherence are given as percentages, as reported in the individual studies.
Results
Studies included
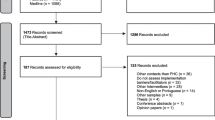
The systematic search of the databases yielded 6,211 unique records, and an additional seven were found through snowball searching (Fig. 1). We examined 243 full texts, and 74 met with this study’s eligibility criteria. Using the study as the unit of analysis [30], we conflated multiple reports of a single study, leading to 57 unique studies as the sample size for this systematic review. Reports of the same study presenting different outcomes (e.g., one reporting PA data and another reported adherence data) were included as separate study units ([35,36,37,38]). The extent of the agreement between reviewers for the inclusion of studies was strong (Cohen’s kappa = 0.804, 95% CI = 0.797–0.809).
Study characteristics
The majority of studies (n = 28, 49.0%) used an experimental design (randomized controlled trial [RCT], pragmatic or cluster RCT) [39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67]. Sample sizes ranged from 14 [68] to 6,610 [69]. Studies were spread across four continents, and the most common location was Europe (n = 42, 73.7%) [35,36,37,38,39,40,41,42,43,44,45,46, 50, 51, 57, 58, 60, 61, 63, 64, 67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88]. Table 1 summarizes the study characteristics, and Additional file 2 describes them in more detail.
Scheme characteristics
Table 2 summarizes the characteristics of the PARS models investigated in the included studies. More detailed information about each scheme (e.g., the content of the PA sessions) can be found in Additional file 4. The studies collectively investigated 36 PARS models, and seven schemes were researched by multiple studies. The Swedish Physical Activity on Prescription (PAP) model was investigated the most [35,36,37,38, 40,41,42,43,44, 58, 70,71,72, 89,90,91], with some studies examining schemes with the standard core components of this model [35,36,37,38, 41, 58, 72] and others focusing on enhanced variations [40, 42, 43, 70, 71]. The second most investigated model was the Green Prescription (GRx), originating from New Zealand, including the standard scheme [48, 62, 92] and variations [47, 53, 54]. This scheme was also replicated in the US [59]. Eighteen different schemes were included from the UK [45, 46, 50, 51, 63, 64, 68, 69, 73,74,75,76,77,78,79,80,81,82,83, 88]. These ranged from a simple referral to a PA program [81] to more complex referral systems [46].
PARS components
The component analysis revealed 19 components that make up PARS (Table 3). While there was some inconsistency in the use of terms to designate intervention components, the definitions that were established during the analysis can be found in Additional file 3.
The identified components appertain to the following:
-
a)
the theoretical basis (person-centered approach, individualized content, and behavior change theory and techniques);
-
b)
scheme entry and transitioning and exit (screening, brief advice, written prescription, referral, exit routes/strategies, and feedback to the referrer);
-
c)
behavioral support (baseline consultation, final consultation, counseling support session(s), structured follow-up, action for non-attendance, education session(s), and written materials);
-
d)
and PA opportunities (PA sessions and a PA network).
For some of the components, we were able to identify specific elements that are listed in Table 3, together with frequencies.
There was substantial variation in the number of components included within the design of various PARS. The PARS models contained a mean of 7 ± 2.9 components (range = 2–13).
Narrative effectiveness synthesis
Table 4 summarizes the distribution of the 19 components across the 57 studies. For each study, the components are indicated as present or not and mapped against the effect direction on PA level (regardless of significance level), uptake rate, and adherence rate. These data are solely descriptive and are not intended to indicate the effectiveness of specific components.
The majority of studies reported positive effects on the part of PARS on PA levels [39, 41, 46,47,48, 52, 57, 67, 99, 100] as compared with usual care, while four RCTs reported no group difference [58, 61] or mixed results [56, 63]. In contrast, only one randomized trial reported any additional benefit on the part of PARS on PA level [62] when compared with PA advice alone, while three trials did not detect any additional benefit [40, 49, 59], and one reported mixed results [51]. The offer of a PARS program was shown to be more beneficial in terms of increasing PA than prescription only [50, 100], with inconsistent results being found in one study [60]. Approximately one-fifth of the included studies compared different versions of PARS regarding intensity and the activities offered. Most studies did not report added benefits for an enhanced intervention over standard provisions [42,43,44,45, 73, 85]. However, two trials [64, 65] and one observational study [70] reported that more intensive PARS offer added benefits for participants, and one study reported inconsistent results [55]. Observational and pre-post studies consistently reported an increase in PA levels for PARS participants [35, 37, 68, 71, 72, 75, 76, 78,79,80, 84, 86], with the exception of one study [77].
Among the 28 studies that reported uptake, rates ranged from 5.7% [87] to 100.0% [44, 54]. Although not always explicitly stated, the uptake definition was consistent among studies, i.e., the number of participants who entered the scheme after being referred to. In other words, those who participated in at least one scheme activity after the referral. The adherence or attendance rate was reported in 34 studies, with variations in terms of definitions. For example, adherence was defined as adherence to the prescribed PA, adherence to the allocated PARS intervention, scheme completion, or the average attended PA sessions. Adherence rates varied from 8.5% [92] to 95.0% in terms of completing the entire PARS [47].
Discussion
This is the first review to examine the components that are included in PARS. We identified 19 components: using a person-centered approach, individualized content, being based on behavior change theory, the use of BCTs, screening, brief advice, the provision of written materials, written prescriptions, referral to a PARS program/professional, a baseline consultation, an exit consultation, counseling support session(s), PA sessions, education session(s), action for non-attendance, structured follow-up, PA networks, feedback to the referrer, and having exit routes/strategies. The PARS models we examined contained a mean of 7 ± 2.9 components (range = 2–13). The level of detail provided in studies of PARS content varied, making it difficult to ensure that all components were identified. In our narrative effectiveness synthesis, approximately two-thirds of studies reported a positive effect on participant PA levels, with wide ranges of uptake (5.7–100.0%) and adherence rates (8.5–95.0%). The large cross-country and within-country (for example, UK) differences in the number and arrangement of components included in the PARS models in this review highlights the complexity of understanding which components affect which outcomes. This is not only because these differences might impact effect sizes (changes in PA) and participant engagement with the scheme (uptake and adherence). The inclusion of different components in a scheme creates differing implementation demands, which must be adequately resourced. Implementation fidelity will be reflected in scheme outcomes, adding another layer of complexity.
The complexity of the role of components within PARS has played a limited role in evidence synthesis to date. Existing PARS meta-analyses have synthesized the effects of PARS interventions as an uniform package [10, 15], without any consideration of differences in design and delivery. Thus, the true heterogeneity of PARS models, as a function of their components, has not been incorporated in the effectiveness equation. Previous reviews have considered the potential influence of demographics (e.g., age, sex, and socio-economic status) [109, 110], personal factors (e.g., referral reasons, medical conditions, and psychological factors) [14, 109, 110], healthcare system/team-related factors (e.g., adequacy of health services and participant-provider relationship) [110], and scheme characteristics (e.g., scheme length, number of exercise sessions, and scheme setting) [25, 109] on uptake and adherence rates, as well as PA behavior change. Our findings advance the prior understanding of PARS complexity by highlighting specific scheme components (e.g., brief advice and PA sessions), in addition to other relevant demographic or personal factors.
The reviewed evidence demonstrates that single PARS components are a subject of growing interest, but they have not been included in meta-analyses. Many of the included studies have the potential added effect of certain components, such as behavior change theory [45, 65], a written prescription [59, 62], written materials [99], counseling support [42, 55, 64, 70], and PA sessions [49], on PA and health outcomes. Additionally, components such as individualization [40, 42, 44], exit routes and strategies [74, 75], measures to keep scheme participation high [77], baseline consultation [77], and structured follow-up [51, 75, 99] have been suggested to be important to scheme success. This growing attention to the role of components in individual studies, in combination with heterogeneous scheme designs, risks producing research that is difficult to combine for synthesis. Our review highlights the fact that there is not yet a standard terminology that can be used to understand these differences between PARS designs. Our analysis adds value because it has distinguished between PARS components and provides a basis for a future standardized terminology. This will aid in scheme comparison and allow for evidence harmonization and synthesis. To enable better differentiation between PARS and an examination of which components add value, researchers and providers must improve the reporting of scheme content.
A lack of detailed information on intervention content and other study-relevant items is a known problem, despite the widespread recommendations of reporting guidelines [111], and this is reflected in the findings of this review. The incomplete reporting of behavioral interventions has a direct impact on identifying and understanding how intervention characteristics actually impact behavior [112]. Therefore, we suggest using the PARS checklist [16] to provide sufficient data quantity and clear information in a standardized way. Given the review findings, it may be beneficial to extend the checklist to include a section about counseling support session(s) and how these are offered. The PARS checklist [16] can be employed directly at the protocol stage, as utilized in one of our projects [113], or as a compass when designing interventions. Differentiating between scheme components strengthens comparability at the scheme level and can facilitate future research endeavors.
Studies show that individual components may have potential to maximize PARS effectiveness [62, 65, 70, 99]. This is important given the ambiguity in the existing evidence regarding the effect of PARS on PA and other health outcomes [8, 18]; thus, we strongly recommend the further investigation of the role of components in order to improve the case for investment in PARS. While we have identified potential components, their role in the effectiveness equation depends on their successful implementation. Only if the component under study is delivered as intended can its relevance to scheme success be determined. Thus, process evaluations of PARS [97, 104] are essential to understanding components.
Strengths and weaknesses
The strength of this systematic review lies in the prior publication of the protocol [28], which reduced the chance of bias. We used a comprehensive search strategy, involving independent reviewers in the selection of studies for inclusion and using a standardized synthesis process in the identification of components. Additionally, the use of ICA [33] in combination with the PARS taxonomy [16] allowed for a systematic assessment of the intervention content of 36 models.
The results of the component analysis are, however, bound by two unique limitations. Both are closely related to the identification of the components and the rating of schemes as having or not having these components. Firstly, because the identification of PARS components was partially subjective, confirmation bias cannot be ruled out. Thus, the components list is by no means exhausting, and we may have overlooked other potentially relevant components. Secondly, poor reporting may have compromised our ability to detect certain components within a PARS when they were, in fact, present. The reporting level of the included studies varied substantially, from very detailed (e.g., [60, 73]) to a scant description of PARS content (e.g., [79]).
The terminology used to label components was inconsistent. Thus, during the ICA, the rating of a component as present or absent was based on its content, rather than the original label provided by the primary investigators. The identified components might also overlap with one another. For instance, individualization can be an inherent part of a person-centered approach, but one can individualize the content of PA sessions in an arbitrary way, without actively involving the participant in the process. Thus, we separated the concepts of person-centeredness and individualization, although they were often conflated in individual studies. One can also argue that a specific BCT, such as goal setting, could be a separate [114] of PA interventions. However, we focused on scheme-level components, that is, whether BCTs were incorporated. We applied the same reasoning for behavior change theory. While a particular type of theory can impact the intervention effects, the question of whether a PARS being theory-based impacts the PARS outcomes is more relevant to this review.
Conclusions
Physical activity referral scheme components are an important source of complexity, and this review identified 19 components included in 36 PARS models that were delivered in twelve countries. Further research is required to determine the influence of these components on PARS uptake, adherence, and PA behavior change. To facilitate this, we recommend that researchers and scheme providers report PARS designs in more detail. We also suggest the need for process evaluations to examine the implementation of PARS designs and the role of components. This will increase our understanding of what works, leading to increased scheme optimization.
Availability of data and materials
All data relevant to the results of this systematic review are available in the main tables and additional files. The data collected, including data extraction forms, can be made available upon reasonable request.
Abbreviations
- BCTs:
-
Behavior change techniques
- ICA:
-
Intervention component analysis
- NCDs:
-
Non-communicable diseases
- PA:
-
Physical activity
- PAP:
-
Physical activity on prescription
- PARS:
-
Physical activity referral scheme(s)
- PRISMA:
-
Preferred reporting items for systematic review and meta-analysis
- RCT:
-
Randomized controlled trial
- SwiM:
-
Synthesis without meta-analysis
References
Holman HR. The relation of the chronic disease epidemic to the health care crisis. ACR Open Rheumatol. 2020;2:167–73. https://doi.org/10.1002/acr2.11114.
World Health Organization. Global action plan on physical activity 2018–2030: more active people for a healtier world. Geneva: World Health Organization; 2018.
World Health Organization. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Geneva: World Health Organization; 2020.
World Health Organization. Promoting physical activity through primary health care: a toolkit. Geneva: World Health Organization; 2021.
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32:541–56. https://doi.org/10.1097/HCO.0000000000000437.
Moses MW, Pedroza P, Baral R, Bloom S, Brown J, Chapin A, et al. Funding and services needed to achieve universal health coverage: applications of global, regional, and national estimates of utilisation of outpatient visits and inpatient admissions from 1990 to 2016, and unit costs from 1995 to 2016. Lancet Public Health. 2019;4:e49–73. https://doi.org/10.1016/S2468-2667(18)30213-5.
World Health Organization. Global status report on physical activity 2022. Geneva: World Health Organization; 2022.
National Institute for Health and Care Excellence. Physical activity: exercise referral schemes (PH54). London: NICE; 2014.
WHO Regional Office for Europe. Integrated brief interventions for noncommunicable disease risk factors in primary care: the manual. Copenhagen: BRIEF project; 2022.
Pavey TG, Taylor AH, Fox KR, Hillsdon M, Anokye N, Campbell JL, et al. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. BMJ. 2011;343: d6462. https://doi.org/10.1136/bmj.d6462.
Onerup A, Arvidsson D, Blomqvist Å, Daxberg E-L, Jivegård L, Jonsdottir IH, et al. Physical activity on prescription in accordance with the Swedish model increases physical activity: a systematic review. Br J Sports Med. 2019;53:383–8. https://doi.org/10.1136/bjsports-2018-099598.
Hellgren MI, Jansson P-A, Wedel H, Lindblad U. A lifestyle intervention in primary care prevents deterioration of insulin resistance in patients with impaired glucose tolerance: a randomised controlled trial. Scand J Public Health. 2016;44:718–25. https://doi.org/10.1177/1403494816663539.
Kallings LV, Sierra Johnson J, Fisher RM, Faire Ud, Ståhle A, Hemmingsson E, Hellénius M-L. Beneficial effects of individualized physical activity on prescription on body composition and cardiometabolic risk factors: results from a randomized controlled trial. Eur J Cardiovasc Prev Rehabil. 2009;16:80–4. https://doi.org/10.1097/HJR.0b013e32831e953a.
Eynon M, Foad J, Downey J, Bowmer Y, Mills H. Assessing the psychosocial factors associated with adherence to exercise referral schemes: a systematic review. Scand J Med Sci Sports. 2019;29:638–50. https://doi.org/10.1111/sms.13403.
Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, et al. A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technol Assess. 2015;19:1–110. https://doi.org/10.3310/hta19600.
Hanson CL, Oliver EJ, Dodd-Reynolds CJ, Pearsons A, Kelly P. A modified Delphi study to gain consensus for a taxonomy to report and classify physical activity referral schemes (PARS). Int J Behav Nutr Phys Act. 2020;17:158. https://doi.org/10.1186/s12966-020-01050-2.
Oliver EJ, Hanson CL, Lindsey IA, Dodd-Reynolds CJ. Exercise on referral: evidence and complexity at the nexus of public health and sport policy. Int J Sport Policy Politics. 2016;8:731–6. https://doi.org/10.1080/19406940.2016.1182048.
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7. https://doi.org/10.2105/ajph.89.9.1322.
European Physical Activity on Prescription model (EUPAP). https://www.eupap.org/. Accessed 1 December 2022.
Kallings L. The Swedish approach on physical activity on prescription. Clin Health Promot. 2016;6:31–3.
Kallings L. Physical activity on prescription in the Nordic region: experiences and recommendations. 2010.
Clark AM. What are the components of complex interventions in healthcare? Theorizing approaches to parts, powers and the whole intervention. Soc Sci Med. 2013;93:185–93. https://doi.org/10.1016/j.socscimed.2012.03.035.
Petticrew M, Anderson L, Elder R, Grimshaw J, Hopkins D, Hahn R, et al. Complex interventions and their implications for systematic reviews: a pragmatic approach. J Clin Epidemiol. 2013;66:1209–14. https://doi.org/10.1016/j.jclinepi.2013.06.004.
Laake J-P, Fleming J. Effectiveness of physical activity promotion and exercise referral in primary care: protocol for a systematic review and meta-analysis of randomised controlled trials. Syst Rev. 2019;8:303. https://doi.org/10.1186/s13643-019-1198-y.
Arsenijevic J, Groot W. Physical activity on prescription schemes (PARS): do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses. BMJ Open. 2017;7: e012156. https://doi.org/10.1136/bmjopen-2016-012156.
Rowley N, Mann S, Steele J, Horton E, Jimenez A. The effects of exercise referral schemes in the United Kingdom in those with cardiovascular, mental health, and musculoskeletal disorders: a preliminary systematic review. BMC Public Health. 2018;18:949. https://doi.org/10.1186/s12889-018-5868-9.
Lewin S, Hendry M, Chandler J, Oxman AD, Michie S, Shepperd S, et al. Assessing the complexity of interventions within systematic reviews: development, content and use of a new tool (iCAT_SR). BMC Med Res Methodol. 2017;17:76. https://doi.org/10.1186/s12874-017-0349-x.
Mino E, Geidl W, Naber I, Weissenfels A, Klamroth S, Gelius P, et al. Physical activity referral scheme components: a study protocol for systematic review and meta-regression. BMJ Open. 2021;11: e049549. https://doi.org/10.1136/bmjopen-2021-049549.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374: n2061.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated August 2022): Cochrane; 2022. https://training.cochrane.org/handbook.
Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Campbell M, Mckenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368: l6890. https://doi.org/10.1136/bmj.l6890.
Sutcliffe K, Thomas J, Stokes G, Hinds K, Bangpan M. Intervention Component Analysis (ICA): a pragmatic approach for identifying the critical features of complex interventions. Syst Rev. 2015;4:140. https://doi.org/10.1186/s13643-015-0126-z.
Mckenzie JE, Brennan S. E. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated August 2022): Cochrane; 2022. https://training.cochrane.org/handbook/current/chapter-12.
Kallings LV, Leijon M, Hellenius ML, Stahle A. Physical activity on prescription in primary health care: a follow-up of physical activity level and quality of life. Scand J Med Sci Sports. 2008;18:154–61. https://doi.org/10.1111/j.1600-0838.2007.00678.x.
Kallings LV, Leijon ME, Kowalski J, Hellénius M-L, Ståhle A. Self-reported adherence: a method for evaluating prescribed physical activity in primary health care patients. J Phys Act Health. 2009;6:483–92. https://doi.org/10.1123/jpah.6.4.483.
Leijon ME, Bendtsen P, Nilsen P, Festin K, Ståhle A. Does a physical activity referral scheme improve the physical activity among routine primary health care patients? Scand J Med Sci Sports. 2009;19:627–36. https://doi.org/10.1111/j.1600-0838.2008.00820.x.
Leijon ME, Bendtsen P, Ståhle A, Ekberg K, Festin K, Nilsen P. Factors associated with patients self-reported adherence to prescribed physical activity in routine primary health care. BMC Fam Pract. 2010;11:38. https://doi.org/10.1186/1471-2296-11-38.
Aittasalo M, Miilunpalo S, Kukkonen-Harjula K, Pasanen M. A randomized intervention of physical activity promotion and patient self-monitoring in primary health care. Prev Med. 2006;42:40–6. https://doi.org/10.1016/j.ypmed.2005.10.003.
Bendrik R, Kallings LV, Bröms K, Kunanusornchai W, Emtner M. Physical activity on prescription in patients with hip or knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2021;35:1465–77. https://doi.org/10.1177/02692155211008807.
Kallings LV, Johnson JS, Fisher RM, Faire Ud, Ståhle A, Hemmingsson E, Hellénius M-L. Beneficial effects of individualized physical activity on prescription on body composition and cardiometabolic risk factors: results from a randomized controlled trial. Eur J Cardiovasc Prev Rehabil. 2009b;16:80–4. https://doi.org/10.1097/HJR.0b013e32831e953a.
Lundqvist S, Börjesson M, Cider Å, Hagberg L, Ottehall CB, Sjöström J, Larsson MEH. Long-term physical activity on prescription intervention for patients with insufficient physical activity level—a randomized controlled trial. Trials. 2020;21:793. https://doi.org/10.1186/s13063-020-04727-y.
Romé A, Persson U, Ekdahl C, Gard G. Physical activity on prescription (PAP): costs and consequences of a randomized, controlled trial in primary healthcare. Scand J Prim Health Care. 2009;27:216–22. https://doi.org/10.3109/02813430903438734.
Sørensen JB, Kragstrup J, Skovgaard T, Puggaard L. Exercise on prescription: a randomized study on the effect of counseling vs counseling and supervised exercise. Scand J Med Sci Sports. 2008;18:288–97. https://doi.org/10.1111/j.1600-0838.2008.00811.x.
Duda JL, Williams GC, Ntoumanis N, Daley A, Eves FF, Mutrie N, et al. Effects of a standard provision versus an autonomy supportive exercise referral programme on physical activity, quality of life and well-being indicators: a cluster randomised controlled trial. Int J Behav Nutr Phys Act. 2014;11:10. https://doi.org/10.1186/1479-5868-11-10.
Murphy SM, Edwards RT, Williams N, Raisanen L, Moore G, Linck P, et al. An evaluation of the effectiveness and cost effectiveness of the National Exercise Referral Scheme in Wales, UK: a randomised controlled trial of a public health policy initiative. J Epidemiol Community Health. 2012;66:745–53. https://doi.org/10.1136/jech-2011-200689.
Lawton BA, Rose SB, Elley CR, Dowell AC, Fenton A, Moyes SA. Exercise on prescription for women aged 40–74 recruited through primary care: two year randomised controlled trial. BMJ. 2008;337: a2509. https://doi.org/10.1136/bmj.a2509.
Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ. 2003;326:793. https://doi.org/10.1136/bmj.326.7393.793.
Gallegos-Carrillo K, García-Peña C, Salmerón J, Salgado-de-Snyder N, Lobelo F. Brief counseling and exercise referral scheme: a pragmatic trial in Mexico. Am J Prev Med. 2017;52:249–59. https://doi.org/10.1016/j.amepre.2016.10.021.
Harrison RA, Roberts C, Elton PJ. Does primary care referral to an exercise programme increase physical activity one year later? A randomized controlled trial. J Public Health (Oxf). 2005a;27:25–32. https://doi.org/10.1093/pubmed/fdh197.
Isaacs AJ, Critchley JA, Tai SS, Buckingham K, Westley D, Harridge SDR, et al. Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only. Health Technol Assess. 2007;11(1–165):iii–iv. https://doi.org/10.3310/hta11100.
James EL, Ewald BD, Johnson NA, Stacey FG, Brown WJ, Holliday EG, et al. Referral for expert physical activity counseling: a pragmatic RCT. Am J Prev Med. 2017;53:490–9. https://doi.org/10.1016/j.amepre.2017.06.016.
Kolt GS, Schofield GM, Kerse N, Garrett N, Ashton T, Patel A. Healthy Steps trial: pedometer-based advice and physical activity for low-active older adults. Ann Fam Med. 2012;10:206–12. https://doi.org/10.1370/afm.1345.
Williams MH, Cairns SP, Simmons D, Rush EC. Face-to-face versus telephone delivery of the Green Prescription for Maori and New Zealand Europeans with type-2 diabetes mellitus: influence on participation and health outcomes. N Z Med J. 2017;130:71–9.
Fortier MS, Hogg W, O’Sullivan TL, Blanchard C, Sigal RJ, Reid RD, et al. Impact of integrating a physical activity counsellor into the primary health care team: physical activity and health outcomes of the Physical Activity Counselling randomized controlled trial. Appl Physiol Nutr Metab. 2011;36:503–14. https://doi.org/10.1139/h11-040.
Livingston PM, Craike MJ, Salmon J, Courneya KS, Gaskin CJ, Fraser SF, et al. Effects of a clinician referral and exercise program for men who have completed active treatment for prostate cancer: a multicenter cluster randomized controlled trial (ENGAGE). Cancer. 2015;121:2646–54. https://doi.org/10.1002/cncr.29385.
Martín-Borràs C, Giné-Garriga M, Puig-Ribera A, Martín C, Solà M, Cuesta-Vargas AI. A new model of exercise referral scheme in primary care: is the effect on adherence to physical activity sustainable in the long term? A 15-month randomised controlled trial. BMJ Open. 2018;8: e017211. https://doi.org/10.1136/bmjopen-2017-017211.
Morén C, Welmer A-K, Hagströmer M, Karlsson E, Sommerfeld DK. The effects of “physical activity on prescription” in persons with transient ischemic attack: a randomized controlled study. J Neurol Phys Ther. 2016;40:176–83. https://doi.org/10.1097/NPT.0000000000000134.
Pfeiffer BA, Clay SW, Conatser JRRR. A green prescription study: does written exercise prescribed by a physician result in increased physical activity among older adults? J Aging Health. 2001;13:527–38. https://doi.org/10.1177/089826430101300405.
Riera-Sampol A, Bennasar-Veny M, Tauler P, Aguilo A. Effectiveness of physical activity prescription by primary care nurses using health assets: a randomized controlled trial. J Adv Nurs. 2020. https://doi.org/10.1111/jan.14649.
Samdal GB, Meland E, Eide GE, Berntsen S, Abildsnes E, Stea TH, Mildestvedt T. The Norwegian Healthy Life Centre Study: a pragmatic RCT of physical activity in primary care. Scand J Public Health. 2019;47:18–27. https://doi.org/10.1177/1403494818785260.
Swinburn BA, Walter LG, Arroll B, Tilyard MW, Russell DG. The green prescription study: a randomized controlled trial of written exercise advice provided by general practitioners. Am J Public Health. 1998;88:288–91. https://doi.org/10.2105/ajph.88.2.288.
Taylor AH, Doust J, Webborn N. Randomised controlled trial to examine the effects of a GP exercise referral programme in Hailsham, East Sussex, on modifiable coronary heart disease risk factors. J Epidemiol Community Health. 1998;52:595–601. https://doi.org/10.1136/jech.52.9.595.
Taylor AH, Taylor RS, Ingram WM, Anokye N, Dean S, Jolly K, et al. Adding web-based behavioural support to exercise referral schemes for inactive adults with chronic health conditions: the e-coachER RCT. Health Technol Assess. 2020;24:1–106. https://doi.org/10.3310/hta24630.
Petrella RJ, Lattanzio CN, Shapiro S, Overend T. Improving aerobic fitness in older adults: effects of a physician-based exercise counseling and prescription program. Can Fam Physician. 2010;56:e191–200.
Shepich J, Slowiak JM, Keniston A. Do subsidization and monitoring enhance adherence to prescribed exercise? Am J Health Promot. 2007;22:2–5. https://doi.org/10.4278/0890-1171-22.1.2.
Gademan MGJ, Deutekom M, Hosper K, Stronks K. The effect of exercise on prescription on physical activity and wellbeing in a multi-ethnic female population: a controlled trial. BMC Public Health. 2012;12:758. https://doi.org/10.1186/1471-2458-12-758.
Webb R, Thompson JES, Ruffino J-S, Davies NA, Watkeys L, Hooper S, et al. Evaluation of cardiovascular risk-lowering health benefits accruing from laboratory-based, community-based and exercise-referral exercise programmes. BMJ Open Sport Exerc Med. 2016;2: e000089. https://doi.org/10.1136/bmjsem-2015-000089.
Harrison RA, McNair F, Dugdill L. Access to exercise referral schemes – a population based analysis. J Public Health (Oxf). 2005b;27:326–30. https://doi.org/10.1093/pubmed/fdi048.
Andersen P, Holmberg S, Årestedt K, Lendahls L, Nilsen P. Physical activity on prescription in routine health care: 1-year follow-up of patients with and without counsellor support. Int J Environ Res Public Health. 2020;17:5679. https://doi.org/10.3390/ijerph17165679.
Sjöling M, Lundberg K, Englund E, Westman A, Jong MC. Effectiveness of motivational interviewing and physical activity on prescription on leisure exercise time in subjects suffering from mild to moderate hypertension. BMC Res Notes. 2011;4:1–7. https://doi.org/10.1186/1756-0500-4-352.
Rödjer L, H. Jonsdottir I, Börjesson M. Physical activity on prescription (PAP): self-reported physical activity and quality of life in a Swedish primary care population, 2-year follow-up. Scand J Prim Health Care. 2016;34:443–52. doi:https://doi.org/10.1080/02813432.2016.1253820.
Buckley B, Thijssen DH, Murphy RC, Graves LE, Cochrane M, Gillison F, et al. Pragmatic evaluation of a coproduced physical activity referral scheme: a UK quasi-experimental study. BMJ Open. 2020;10: e034580. https://doi.org/10.1136/bmjopen-2019-034580.
Edmunds J, Ntoumanis N, Duda JL. Adherence and well-being in overweight and obese patients referred to an exercise on prescription scheme: a self-determination theory perspective. Psychol Sport Exerc. 2007;8:722–40. https://doi.org/10.1016/j.psychsport.2006.07.006.
Dodd-Reynolds CJ, Vallis D, Kasim A, Akhter N, Hanson CL. The Northumberland Exercise Referral Scheme as a universal community weight management programme: a mixed methods exploration of outcomes, expectations and experiences across a social gradient. Int J Environ Res Public Health. 2020;17:5297. https://doi.org/10.3390/ijerph17155297.
Hanson CL, Allin LJ, Ellis JG, Dodd-Reynolds CJ. An evaluation of the efficacy of the exercise on referral scheme in Northumberland, UK: association with physical activity and predictors of engagement. A naturalistic observation study BMJ Open. 2013;3: e002849. https://doi.org/10.1136/bmjopen-2013-002849.
Hanson CL, Neubeck L, Kyle RG, Brown N, Gallagher R, Clark RA, et al. Gender differences in uptake, adherence and experiences: a longitudinal, mixed-methods study of a physical activity referral scheme in Scotland, UK. Int J Environ Res Public Health. 2021;18:1700. https://doi.org/10.3390/ijerph18041700.
Prior F, Coffey M, Robins A, Cook P. Long-term health outcomes associated with an exercise referral scheme: an observational longitudinal follow-up study. J Phys Act Health. 2019;16:288–93. https://doi.org/10.1123/jpah.2018-0442.
Stewart L, Dolan E, Carver P, Swinton PA. Per-protocol investigation of a best practice exercise referral scheme. Public Health. 2017;150:26–33. https://doi.org/10.1016/j.puhe.2017.04.023.
Ward M, Phillips CJ, Farr A, Harries D. Heartlinks—A real world approach to effective exercise referral. Int J Health Promot Educ. 2010;48:20–7. https://doi.org/10.1080/14635240.2010.10708176.
Crone D, Johnston LH, Gidlow C, Henley C, James DVB. Uptake and participation in physical activity referral schemes in the UK: an investigation of patients referred with mental health problems. Issues Ment Health Nurs. 2008;29:1088–97. https://doi.org/10.1080/01612840802319837.
Lord JC, Green F. Exercise on prescription: does it work? Health Educ J. 1995;54:453–64. https://doi.org/10.1177/001789699505400408.
Dinan S, Lenihan P, Tenn T, Iliffe S. Is the promotion of physical activity in vulnerable older people feasible and effective in general practice? Br J Gen Pract. 2006;56:791–3.
Sørensen J, Sørensen JB, Skovgaard T, Bredahl T, Puggaard L. Exercise on prescription: changes in physical activity and health-related quality of life in five Danish programmes. Eur J Public Health. 2011;21:56–62. https://doi.org/10.1093/eurpub/ckq003.
Bredahl T, Singhammer J, Roessler K. “ Is Intensity Decisive?” Changes in Levels of Self-efficacy, Stages of Change and Physical Activity for Two Different Forms of Prescribed Exercise. Sport Science Review. 2011;20:85. https://doi.org/10.2478/v10237-011-0056-1.
Pardo A, Violán M, Cabezas C, García J, Miñarro C, Rubinat M, et al. Effectiveness of a supervised physical activity programme on physical activity adherence in patients with cardiovascular risk factors. Apunts Medicina de l’Esport. 2014;49:37–44. https://doi.org/10.1016/j.apunts.2014.02.001.
van de Vijver PL, Schalkwijk FH, Numans ME, Slaets JPJ, van Bodegom D. Linking a peer coach physical activity intervention for older adults to a primary care referral scheme. BMC Prim Care. 2022;23:118. https://doi.org/10.1186/s12875-022-01729-4.
Hesketh K, Jones H, Kinnafick F, Shepherd SO, Wagenmakers AJM, Strauss JA, Cocks M. Home-Based HIIT and traditional MICT prescriptions improve cardiorespiratory fitness to a similar extent within an exercise referral scheme for at-risk individuals. Front Physiol. 2021;12: 750283. https://doi.org/10.3389/fphys.2021.750283.
Leijon ME, Faskunger J, Bendtsen P, Festin K, Nilsen P. Who is not adhering to physical activity referrals, and why? Scand J Prim Health Care. 2011;29:234–40. https://doi.org/10.3109/02813432.2011.628238.
Lundqvist S, Börjesson M, Larsson MEH, Hagberg L, Cider Å. Physical Activity on Prescription (PAP), in patients with metabolic risk factors. A 6-month follow-up study in primary health care. PLoS ONE. 2017;12:e0175190. https://doi.org/10.1371/journal.pone.0175190.
Romé Å, Persson U, Ekdahl C, Gard G. Costs and outcomes of an exercise referral programme – A 1-year follow-up study. Eur J Physiother. 2014;16:82–92. https://doi.org/10.3109/21679169.2014.886291.
Foley L, Maddison R, Jones Z, Brown P, Davys A. Comparison of two modes of delivery of an exercise prescription scheme. N Z Med J. 2011;124:44–54.
Elley CR, Garrett S, Rose SB, Des O'Dea, Lawton BA, Moyes SA, Dowell AC. Cost-effectiveness of exercise on prescription with telephone support among women in general practice over 2 years. Br J Sports Med. 2011;45:1223–9.
Elley R, Kerse N, Arroll B, Swinburn B, Ashton T, Robinson E. Cost-effectiveness of physical activity counselling in general practice. N Z Med J. 2004;117:U1216.
Kerse N, Elley CR, Robinson E, Arroll B. Is physical activity counseling effective for older people? A cluster randomized, controlled trial in primary care. J Am Geriatr Soc. 2005;53:1951–6. https://doi.org/10.1111/j.1532-5415.2005.00466.x.
Edwards RT, Linck P, Hounsome N, Raisanen L, Williams N, Moore L, Murphy S. Cost-effectiveness of a national exercise referralprogramme for primary care patients in Wales: results of a randomised controlled trial. BMC Public Health. 2013;13:1021. https://doi.org/10.1186/1471-2458-13-1021.
Moore GF, Raisanen L, Moore L, Din NU, Murphy S. Mixed-method process evaluation of the Welsh National Exercise Referral Scheme. Health Edu. 2013;113:476–501. https://doi.org/10.1108/HE-08-2012-0046.
Johnson NA, Ewald B, Plotnikoff RC, Stacey FG, Brown WJ, Jones M, et al. Predictors of adherence to a physical activity counseling intervention delivered by exercise physiologists: secondary analysis of the NewCOACH trial data. Patient Prefer Adherence. 2018;12:2537–43. https://doi.org/10.2147/PPA.S183938.
Smith BJ, Bauman AE, Bull FC, Booth ML, Harris MF. Promoting physical activity in general practice: a controlled trial of written advice and information materials. Br J Sports Med. 2000;34:262–7. https://doi.org/10.1136/bjsm.34.4.262.
Galaviz K, Lévesque L, Kotecha J. Evaluating the effectiveness of a physical activity referral scheme among women. J Prim Care Community Health. 2013;4:167–71. https://doi.org/10.1177/2150131912463243.
Gallegos-Carrillo K, Reyes-Morales H, Pelcastre-Villafuerte B, García-Peña C, Lobelo F, Salmeron J, Salgado-de-Snyder N. Understanding adherence of hypertensive patients in Mexico to an exercise-referral scheme for increasing physical activity. Health Promot Int. 2020. https://doi.org/10.1093/heapro/daaa110.
Gallegos-Carrillo K, Garcia-Peña C, Salgado-de-Snyder N, Salmerón J, Lobelo F. Levels of adherence of an exercise referral scheme in primary health care: effects on clinical and anthropometric variables and depressive symptoms of hypertensive patients. Front Physiol. 2021;12.
Lundqvist S, Cider Å, Larsson MEH, Hagberg L, Björk MP, Börjesson M. The effects of a 5-year physical activity on prescription (PAP) intervention in patients with metabolic risk factors. PLoS ONE. 2022;17:e0276868. https://doi.org/10.1371/journal.pone.0276868.
Lambert J, Taylor A, Streeter A, Greaves C, Ingram WM, Dean S, et al. A process evaluation, with mediation analysis, of a web-based intervention to augment primary care exercise referral schemes: the e-coachER randomised controlled trial. Int J Behav Nutr Phys Act. 2022;19:128. https://doi.org/10.1186/s12966-022-01360-7.
Taylor A, Taylor RS, Ingram W, Dean SG, Jolly K, Mutrie N, et al. Randomised controlled trial of an augmented exercise referral scheme using web-based behavioural support for inactive adults with chronic health conditions: the e-coachER trial. Br J Sports Med. 2021;55:444. https://doi.org/10.1136/bjsports-2020-103121.
Bredahl T, Singhammer J. The influence of self-rated health on the development of change in the level of physical activity for participants in prescribed exercise. Sport Sci Rev. 2011;20:73–94. https://doi.org/10.2478/v10237-011-0065-0
Patel A, Keogh JWL, Kolt GS, Schofield GM. The long-term effects of a primary care physical activity intervention on mental health in low-active, community-dwelling older adults. Aging Ment Health. 2013;17:766–72. https://doi.org/10.1080/13607863.2013.781118.
Gidlow C, Johnston LH, Crone D, Morris C, Smith A, Foster C, James DVB. Socio-demographic patterning of referral, uptake and attendance in physical activity referral schemes. J Public Health (Oxf). 2007;29:107–13.
Pavey T, Taylor A, Hillsdon M, Fox K, Campbell J, Foster C, et al. Levels and predictors of exercise referral scheme uptake and adherence: a systematic review. J Epidemiol Community Health. 2012;66:737–44. https://doi.org/10.1136/jech-2011-200354.
Calonge Pascual S, Casajús Mallén JA, González-Gross M. Adherence factors related to exercise prescriptions in healthcare settings: a review of the scientific literature. Res Q Exerc Sport. 2020:1–10. https://doi.org/10.1080/02701367.2020.1788699.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348: g1687. https://doi.org/10.1136/bmj.g1687.
Michie S, Abraham C. Advancing the science of behaviour change: a plea for scientific reporting. Addiction. 2008;103:1409–10. https://doi.org/10.1111/j.1360-0443.2008.02291.x.
Weissenfels A, Klamroth S, Carl J, Naber I, Mino E, Geidl W, et al. Effectiveness and implementation success of a co-produced physical activity referral scheme in Germany: study protocol of a pragmatic cluster randomised trial. BMC Public Health. 2022;22:1545. https://doi.org/10.1186/s12889-022-13833-2.
McEwan D, Harden SM, Zumbo BD, Sylvester BD, Kaulius M, Ruissen GR, et al. The effectiveness of multi-component goal setting interventions for changing physical activity behaviour: a systematic review and meta-analysis. Health Psychol Rev. 2016;10:67–88. https://doi.org/10.1080/17437199.2015.1104258.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. Open Access funding enabled and organized by Projekt DEAL. This systematic review was conducted within the BewegtVersorgt project, which is supported by the Federal Ministry of Health based on a resolution of the German Bundestag by the Federal Government (ZMV I 1—2519FSB109). No direct funding was sought for this paper. The Federal Ministry of Health had no input into any of the review stages, including review design, data extraction, analysis, results, and writing.
Author information
Authors and Affiliations
Contributions
WG and KP supervised EM, who coordinated the systematic review process and conducted the literature search, collection and screening, data extraction, synthesis, and table and manuscript preparation. AW, IN, and JS participated in the literature screening. JS helped in the data extraction. CLH and SM conducted the content analysis. EM drafted the manuscript, tables and supplementary materials. CLH edited the manuscript. All authors (WG, KP, CLH, AW, IN, SK, SM, JS, SW, KW, GG, KA, and PG) critically reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no interests to declare.
Disclaimer
SW, KW and GG are staff members of the WHO. The authors alone are responsible for the views expressed in this publication, and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy results. This file contains the systematic search strategy and results for all the literature databases. Additional file 2. Overview of included studies sorted by comparison group. This file contains the characteristics of all the studies included in the systematic review, including the main results. Additional file 3. Description of PARS components. This file contains the description of the nineteen components identified through the content analysis. Additional file 4. Overview of PARS characteristics sorted by country. This file contains the characteristics of PARS models included in the systematic review. Additional file 5. PARS identified worldwide. This file provides an overview of all the PARS models identified during the screening for eligible articles, including those that we were not able to include in this review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mino, E., Hanson, C.L., Naber, I. et al. A systematic review and narrative synthesis of physical activity referral schemes’ components. Int J Behav Nutr Phys Act 20, 140 (2023). https://doi.org/10.1186/s12966-023-01518-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-023-01518-x