Abstract
Background
Unhealthy lifestyle behaviours are becoming increasingly common and might contribute to the growing burden of mental disorders in adolescence. We examined the associations between a comprehensive set of lifestyle behaviours and depression and anxiety in middle adolescents.
Methods
School-based survey responses were collected from 24,274 Canadian high school students at baseline and 1-year follow-up (average age 14.8 and 15.8 years, respectively). Using linear mixed-effects models, we examined prospective associations of adherence to recommendations for vegetables and fruit, grains, milk and alternatives, meat and alternatives, sugar-sweetened beverages [SSB], physical activity, screen time, sleep, and no use of tobacco, e-cigarettes, cannabis, and binge drinking at baseline with the depressive and anxiety symptoms (measured by CESD-R-10 and GAD-7 scales, respectively) at follow-up.
Results
Adherence to recommendations was low overall, particularly for vegetables and fruit (3.9%), grains (4.5%), and screen time (4.9%). Students adhering to individual recommendations, particularly for meat and alternatives, SSB, screen time, sleep, and no cannabis use, at baseline had lower CESD-R-10 and GAD-7 scores at follow-up. Adhering to every additional recommendation was associated with lower CESD-R-10 (β=-0.15, 95% CI -0.18, -0.11) and GAD-7 scores (β=-0.10, 95% CI -0.14, -0.07) at follow-up. Assuming cumulative impact, this might translate into 7.2- and 4.8-point lower CESD-R-10 and GAD-7 scores, respectively, among students adhering to 12 vs. 0 recommendations over four years of high school.
Conclusions
The results highlight the preventive potential of population-based approaches promoting healthy lifestyle behaviours, particularly those with the lowest prevalence, as a strategy to improve mental health in adolescence.
Similar content being viewed by others
Introduction
Mental health problems are becoming increasingly common among adolescents in Canada, as reflected in the increasing rates of related healthcare visits even before the COVID-19 pandemic. For example, compared to stable rates of healthcare visits due to physical health conditions, there were 53% more emergency department and 74% more inpatient visits due to mental health problems (most commonly anxiety, mood, and substance use disorders) in 15-17-year-olds between 2006/07 and 2013/14 [1]. Pandemic-related disruptions have further exacerbated the mental health burden in adolescents, with noted increases in the proportion of mental health-related hospitalizations and the use of mood and anxiety medications. [2] This underscores the urgent need for population-based health promotion and primary prevention [3] that, in the absence of effective treatment options, are a crucial strategy to curb the mental health burden.
The evidence on the detrimental impact that substance use (i.e., tobacco smoking, binge drinking, [4] vaping, [5] cannabis use [6]), lack of physical activity, excess screen time, [7] or poor sleep [8] each individually have on the development of mental health problems is strong, and the importance of healthy diet is emerging too. [9, 10] Studies generally focus on the impact of individual lifestyle behaviours, but this does not augment our understanding of the intricate relationships among lifestyle behaviours which tend to cluster among adolescents, [11,12,13] and how these intertwined behaviours may be linked to mental health. Several studies quantified associations between belonging to different clusters of lifestyle behaviours and mental health outcomes in adolescents. [14, 15] While interesting, such studies often examine different combinations of a limited number of lifestyle behaviours and/or assess them using different scales, thus making results across studies difficult to compare. Operationalizing lifestyle behaviours in terms of adherence to existing evidence-based recommendations (which remain mostly unchanged over the years and comparable across countries) can help circumvent these challenges. Additionally, results of studies examining adherence to lifestyle recommendations in relation to mental health outcomes can be easier to understand by public health professionals and thus conducive to being implemented in practice.
To our knowledge, there is only one prospective study [16] that has estimated the effect of overall adherence to nine lifestyle recommendations (i.e., vegetables and fruit, grains, milk and alternatives, meat and alternatives, added sugar, saturated fat, sleep, screen time, physical activity) on the risk of developing internalizing and externalizing mental disorders in early adolescence (i.e., ages 10–14). However, as adolescents mature, they gain more independence, their social relationships become more complex and influential, [17] and as a result they often adopt new unhealthy behaviours, particularly substance use behaviours, often initiated around the age of 15. [18, 19] In fact, 30% of middle adolescents (i.e., 14–17 years) reported binge drinking, e-cigarette smoking (vaping), and drug use in 2018/19 [20]. Given this high prevalence of substance use behaviours, it is imperative to evaluate a wide range of lifestyle behaviours in relation to mental health outcomes in middle adolescence. To date, no Canadian study has examined the extent to which the co-occurrence of a full range of lifestyle behaviours (including substance use) may relate to mental illness in this age group. Therefore, the goal of this study is two-fold: (1) to examine individual and overall adherence to 12 lifestyle recommendations (i.e., five recommendations for diet and one each for physical activity, screen time, sleep, and no tobacco smoking, vaping, cannabis use, and binge drinking), and (2) to assess the relationship between adherence to these recommendations and the severity of depressive and anxiety symptoms among Canadian middle adolescents. We hypothesized that both individually and in combination, healthier lifestyle behaviours are prospectively associated with better mental health in middle adolescence.
Methods
The Cannabis, Obesity, Mental health, Physical activity, Alcohol, Smoking, and Sedentary behaviour (COMPASS) is a large longitudinal study that annually collects survey data on an extensive range of lifestyle behaviours from more than 65,000 grade 9–12 students (age 13–18 years) recruited through a convenience sample of 122 secondary schools in Alberta, British Columbia, Ontario, and Québec, Canada. [21] Using an active-information passive-consent parental permission protocol, students complete an anonymous COMPASS questionnaire at school during class time. COMPASS procedures are available elsewhere. [21] For this study, we linked [22] participants’ responses from 2017/18 (average age of participants 14.8 [SD = 1.2] years old) to the same participants’ responses from 2018/19 (average age 15.8 [SD = 1.2] years old). Records of grade 12 participants and those who changed schools between 2017/18 and 2018/19 were not linked: out of 66,434 participants from 122 schools in 2017/18, the linked sample comprised records of 29,022 participants from 116 schools. Analyses were based on a subsample of 24,274 participants, with data available for all variables listed below. Response rates in 2017/18 and 2018/19 were 81.8% and 84.2%, respectively, with non-response being mainly due to absenteeism or scheduled spare time during data collection. [23].
Measures
The Center for Epidemiologic Studies Depression Scale Revised-10 (CESD-R-10) [24] is a 10-item self-report scale that queries participants about the frequency of symptoms of unipolar depression in the last seven days (none or < 1 day; 1–2 days; 3–4 days; and 5–7 days). The Generalized Anxiety Disorder-7 (GAD-7) scale [25] is a 7-item self-report scale that asks participants about the frequency of generalized anxiety disorder symptoms in the last two weeks (not at all; several days; over half the days; and nearly every day). Both scales demonstrated strong psychometric properties in adolescents. [26, 27] On both scales, items are scored from 0 to 3. Scores are then summed, with the final scores ranging from 0 to 30 for CESD-R-10 and 0 to 21 for GAD-7 scales. Higher scores on both scales indicate greater severity of symptoms. For both scales, missing values on up to two items were imputed for 5168 participants. [28,29,30].
Adherence to established recommendations [31,32,33,34,35] was conceptualized as both individual and overall adherence to recommendations for: vegetables and fruit, grains, milk and alternatives, meat and alternatives, sugar-sweetened beverages (SSB), physical activity, screen time, sleep, and no use of tobacco, e-cigarettes, cannabis, and binge drinking. Participants reported the number of servings (up to nine or more) of vegetables and fruit, grain products, milk and alternatives, and meat and alternatives they consumed the previous day. [36] Participants reported the number of days in a usual school week when they consumed sugar-sweetened beverages, high-energy drinks, and coffee or tea with sugar, which were combined into a sugar-sweetened beverages composite variable (SSB). Participants reported the number of minutes of moderate-to-vigorous physical activity (MVPA) on each day in the past week; the number of hours and minutes per day they usually spend watching/streaming TV shows or movies, playing video/computer games, talking on the phone, surfing the Internet, and texting, messaging, emailing, which were summed to obtain total daily screen time [37]; and the number of hours and minutes per day they usually sleep. Participants reported the past-30-days frequency of smoking one or more cigarettes and e-cigarettes (vaping) (none, 1, 2–3, 4–5, 6–10, 11–20, 21–29, 30 days) and the past-12-months frequency of cannabis use (never, used but not in the past 12 months, less than once/month, once/month, 2–3 times/month, once/week, 2–3 times/week, 4–6 times/week, and every day) and of having five or more drinks of alcohol on one occasion (i.e., binge drinking) (never, not in the past 12 months, less than once/month, once/month, 2–3 times/month, once/week, 2–5 times/week, daily or almost daily). Participants that never tried cigarettes, cannabis use, and binge drinking were considered as those meeting recommendations. Participants’ responses to questions pertaining to each lifestyle behaviour were assigned 0 points if a recommendation was not met and 1 point if it was met (Table 1).
Points for all lifestyle behaviours were then summed to create a composite score ranging from 0 to 12, with higher scores indicating higher overall adherence to lifestyle recommendations and thus a healthier lifestyle. Additionally, based on the composite score, participants were categorized into those having very unfavourable (meeting ≤ 3 recommendations), unfavourable (4–6), intermediate (7–9), or favourable (10–12) lifestyles.
Covariates
A-priori-defined confounders were age (years), sex (female, male), ethnicity (White, Black, Hispanic, Asian, Other/Mixed), school area urban class (rural area and small [population of 1,000–29,999], medium [30,000–99,999], and large urban [≥ 100,000] population centers, defined by the 2016 Canadian Census [39]), school-area median household income ($20,000-$40,000, $40,001-$60,000, $60,001-$80,000, and more than $80,000, derived from the first three letters of each school’s postal code), weight status (derived from self-reported height and weight and categorized into underweight, normal weight, overweight, obese, and missing according to age- and sex-specific cut-off points [40]), weight perception (very or slightly underweight, about the right weight, slightly or very overweight), and weight loss attempts (positive responses to the statement “[I am] trying to lose weight”). The latter three covariates were included to account for the potentially confounding effect of these variables on associations between lifestyle behaviours, particularly diet and physical activity, and mental health outcomes.
Data analyses
We used Student’s t-test and analysis of variance (ANOVA) tests to assess differences in mean CESD-R-10 and GAD-7 scores. We estimated 1-year prospective associations between individual and overall adherence to lifestyle recommendations at baseline and the severity of depressive and anxiety symptoms at 1-year follow-up. Univariate and multivariable linear mixed-effects models (LMMs) were used to account for the nested data structure (i.e., students in schools). Multivariable models were first adjusted for age, ethnicity, school area urban class, school-area median household income, weight status, weight perception, weight loss attempts, and mental health at baseline (CESD-R-10 and GAD-7 scores, as appropriate) (Model 1). Next, these models were repeated while being mutually adjusted for other lifestyle behaviours (Model 2) to quantify the individual effect of separate lifestyle behaviours on the severity of depressive and anxiety symptoms in those meeting vs. not meeting recommendations. In this study, we consider lifestyle behaviours as competing exposures and their relationships with mental health outcomes to be similarly confounded. To compare the combined effect of all 12 lifestyle behaviours on the severity of depressive and anxiety symptoms in those with unfavourable, intermediate, and favourable lifestyles (i.e., meeting 4–6, 7–9, and 10–12 recommendations, respectively) vs. very unfavourable lifestyle (i.e., meeting ≤ 3 recommendations), we ran models adjusting for the same covariates as Model 1 described above. Finally, we ran the same models with the number of recommendations met as the independent variable to quantify the effect of adhering to each additional recommendation on the severity of depressive and anxiety symptoms. The final models were sex-stratified since lifestyle behaviours [41, 42] and mental health [43] are sex-patterned. Missing baseline values for age, sex, and ethnicity were imputed based on the available information (e.g., age reported in 2018/19 minus one, and sex and ethnicity – same as in 2018/19). All models were adjusted for confounders (and confounding is a causal concept [44]), therefore we use causal language throughout the manuscript for transparency and clarity. [45] Cross-sectional associations at baseline are reported in Supplementary materials (Tables S1 and S2) but are not discussed in this paper. Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Results
Participant characteristics are provided in Table 2: 54.4% were female, 71.6% identified as white, 55.9% resided in large population centres, and 42.2% attended schools located in areas of higher median household income. More than half of the participants were classified as normal weight. Compared to males, females more often perceived themselves as normal weight (58.4% vs. 52.4%) and reported weight loss attempts (41.1% vs. 21.8%).
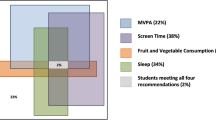
Only 3.9% of participants met recommendations for vegetables and fruit, 4.5% for grains, and 4.9% for screen time. Close to one-third (28.9%) met recommendations for SSB, 36.4% for milk and alternatives, and 38.5% for MVPA (Table 2). Recommendations for sleep and meat and alternatives were met by 48.3% and 55.4%, respectively. Three-quarters of participants reported no binge drinking, 83.5% no vaping, 86.4% no cannabis use, and 93.2% no tobacco smoking. On average, participants in this study met 5.6 recommendations, while almost none of the participants met all 12 recommendations. Overall, 70.0% of participants were classified as having very unfavourable or unfavourable lifestyles, while 29.3% had intermediate and 0.7% favourable lifestyles. No notable sex differences were observed in individual or overall adherence to 12 lifestyle recommendations.
At baseline and follow-up, CESD-R-10 scores were 8.03 (SD = 5.70) and 8.92 (SD = 5.99) and GAD-7 scores 5.85 (SD = 5.30) and 6.47 (SD = 5.50), respectively (Table 2). At baseline, CESD-R-10 and GAD-7 scores were lower among participants who followed recommendations for individual lifestyle behaviours, except for vegetables and fruit, and grains (Table 3). Those who were meeting recommendations for vegetables and fruit, and grains had similar CESD-R-10 scores and higher GAD-7 scores than those not meeting these recommendations. Participants with a very unfavourable lifestyle (i.e., meeting ≤ 3 recommendations) had generally higher CESD-R-10 and GAD-7 scores (10.60 [SD = 6.42] and 7.89 [SD = 5.89], respectively) compared to those with favourable lifestyle (5.49 [SD = 4.76] and 3.87 [SD = 4.90], respectively). This pattern was particularly pronounced in females.
When considered individually, adherence to lifestyle recommendations, particularly for meat and alternatives, SSB, screen time, sleep, and no cannabis use at baseline was associated with lower CESD-R-10 and GAD-7 scores at follow-up (Table 4). Sex-based subgroup analyses revealed some differences. Females adhering to recommendations for meat and alternatives, SSB, screen time, and sleep had lower severity of depressive and anxiety symptoms, while the opposite was observed for MVPA: contrary to expectations, adherence to the individual recommendation for MVPA was associated with higher severity of depressive symptoms. Males adhering to recommendations for SSB, MVPA, screen time, sleep, and cannabis use had lower severity of depressive and particularly anxiety symptoms.
As for the combined effect, for every additional lifestyle recommendation met, females (β=-0.13, 95% CI -0.18, -0.08) and males (β=-0.17, 95% CI -0.22, -0.12) had lower CESD-R-10 scores at follow-up. Compared to those with the very unfavourable lifestyle (i.e., meeting ≤ 3 recommendations), females and males with the favourable lifestyle (i.e., meeting 10–12 recommendations) had lower CESD-R-10 scores (Table 5: β=-1.15, 95% CI -2.28, -0.02 and β=-1.35, 95% CI -2.28, -0.41, respectively) and males with unfavourable and intermediate (i.e., meeting 7–9 recommendations) lifestyles had lower GAD-7 scores (β=-0.29, 95% CI -0.54, -0.03 and β=-0.65, -0.93, -0.38, respectively) at follow-up. Given that students spend four years in high school and assuming the homogeneity and additivity of the effect of lifestyle behaviours on mental health outcomes throughout high school, these estimates may add up to 4.6- and 5.4-point lower CESD-R-10 scores in females and males with the favourable lifestyle and up to 1.16- and 2.6-point lower GAD-7 scores in males with the unfavourable and intermediate lifestyles, compared to those with the very unfavourable lifestyle. Cross-sectional estimates (Table S1 and S2) were more pronounced than those in prospective analyses.
Discussion
In this study, we found adherence to 12 lifestyle behaviours in middle adolescence to be very low, particularly for vegetables and fruit, grains, and screen time with less than 5% of participants adhering to each of these recommendations. Participants reported adhering, on average, to 5.6 lifestyle recommendations and almost none adhering to all 12 recommendations. Adherence to recommendations for lifestyle behaviours, particularly for meat and alternatives, SSB, screen time, sleep, and no cannabis use, was prospectively associated with less severe depressive and anxiety symptoms in middle adolescents. When considered in combination, adolescents meeting 10–12 and 7–9 recommendations had lower CESD-R-10 scores and those meeting 7–9 recommendations had lower GAD-7 scores at follow-up, compared to those with the very unfavourable lifestyle (i.e., meeting ≤ 3 recommendations). Moreover, adherence to each additional recommendation was associated with lower CESD-R-10 and GAD-7 scores at follow-up.
As mentioned before, there is only one prospective study that considered individual and combined effects of adherence to a range of lifestyle behaviours in relation to mental health outcomes, but it is limited to early adolescence. This study by Loewen et al. linked population-based survey data from 3,436 early adolescents (10–11 year old) to administrative records up to the age of 15. Early adolescents meeting 4–6 and 7–9 lifestyle recommendations had, respectively, 39% and 56% fewer healthcare visits for mental health problems in the following four years compared to those meeting 1–3 lifestyle recommendations. [16] Available studies on the combined effect (i.e., the impact of overall adherence to recommendations on mental health) in older adolescents are cross-sectional in design. For example, a study of 10,183 adolescents in grades 7–12 showed that meeting recommendations for sleep, screen time, and physical activity was linked to lower odds of suicidal ideation (odds ratio [OR] = 0.24, 95% CI 0.09, 0.69) and suicide attempts (OR = 0.08, 95% CI 0.02, 0.41) in male students. [46] Another cross-sectional study of 244,250 Norwegian adolescents aged 13–19 showed that those with higher overall adherence to recommendations for physical activity, screen time, tobacco smoking, and alcohol consumption had up to 60% lower odds of depressive symptoms. [47] Although results reported in these studies are encouraging, prospective effect estimates are more reliable since they consider baseline levels of mental health.
Prospective estimates reported in the current study should be considered through a population health lens. As Geoffrey Rose noted, [48] ‘a large number of people at a small risk may give rise to more cases of disease than the small number who are at a high risk’. Although evidence shows that targeted prevention of mental disorders appear more effective and cost-effective than population-level prevention, [49] the latter covers not only those at increased risk of mental disorders, but serves as a protective shield for all children and adolescents. [50] Moreover, population-level prevention strategies for physical health conditions mostly target the same lifestyle behaviours (e.g., diet, physical activity, sedentary behaviour, screen time, substance use) as those aiming to prevent mental disorders, and therefore these strategies can be united under the shared framework for prevention of common mental and noncommunicable diseases. [51] If implemented throughout childhood and early adolescence, these interventions may be effective at curbing the increasing burden of both physical and mental health problems in the longer term.
The finding that females adhering to the physical activity recommendation tended to have higher depressive and anxiety symptoms is surprising. The same finding, albeit only in relation to anxiety symptoms at 1-year follow-up, was previously reported in another COMPASS study. [52] One may speculate the influence of social desirability bias: female adolescents, aware of existing recommendations to engage in physical activity, might over-report their MVPA, particularly those who are overweight. [53] If the severity of mental health symptoms is also over-reported by female adolescents, it could contribute to this spurious association. Nonetheless, it remains unclear what could explain this counterintuitive relationship, given that physical activity is one of the most effective lifestyle interventions to promote mental health in adolescents. [54] Still, it emphasizes the importance of conducting sex-based subgroup analyses to understand sex differences better.
Limitations
Several limitations are worth considering when interpreting study findings. First, data come from a convenience sample predominantly from schools located in large population centres and areas with higher school-area median income. Thus, the study findings may not be representative of adolescents in Canada. Second, all measures were self-reported, yet social desirability and recall bias might have been at least partially negated by the anonymous nature of the COMPASS questionnaire. Third, although many measures are based on previously validated national surveillance tools and guidelines, measurement error is possible, leading to misclassification. [21] Considering the trajectories of adherence to recommendations in relation to mental health outcomes could partly overcome the measurement error associated with the self-reported adherence to lifestyle recommendations, but given this study’s short timeframe (i.e., one year), we assumed that trajectories of most lifestyle behaviours stayed fairly stable. Finally, analyses could be overpowered given the large sample size, and hence we focus on effect estimates rather than p-values in our interpretation of the results, as per current recommendations. [55, 56]
Conclusion
In prospective analyses, we found that overall adherence to recommendations for a comprehensive set of lifestyle behaviours common in middle adolescents was associated with lower severity of depressive symptoms in females and males and anxiety symptoms in males one year later. These results support the public health message that making even modest positive changes to lifestyle behaviours that increase overall adherence to lifestyle recommendations can improve mental health in adolescents. Given the multifactorial etiology of mental health problems, population-based approaches promoting healthy lifestyle behaviours, particularly those with the lowest prevalence (e.g., healthy eating, limited screen time), may yield the biggest improvement in mental health in adolescents, along with many other health, social, and developmental outcomes.
Data Availability
Data are available on reasonable request. COMPASS data are available for researchers upon successful completion and approval of the COMPASS data usage application (https://uwaterloo.ca/compass-system/information-researchers).
Abbreviations
- ANOVA:
-
analysis of variance
- CESD-R-10:
-
Center for Epidemiologic Studies Depression Scale Revised-10
- COVID-19:
-
Coronavirus disease 2019
- COMPASS:
-
Cannabis, Obesity, Mental health, Physical activity, Alcohol, Smoking, and Sedentary behaviour
- GAD-7:
-
General Anxiety Disorder-7
- LMM:
-
linear mixed-effects model
- MVPA:
-
moderate-to-vigorous physical activity
- OR:
-
odds ratio
- SD:
-
standard deviation
- SSB:
-
sugar-sweetened beverages
References
Canadian Institute for Health Information. Care for children and youth with mental disorders. 2015. https://secure.cihi.ca/estore/productFamily.htm?locale=en&pf=PFC2866. Accessed 18 Oct 2022.
Canadian Institute for Health Information. Children and youth mental health in Canada. 2022. https://www.cihi.ca/en/children-and-youth-mental-health-in-canada. Accessed 10 Aug 2022.
Canadian Public Health Association. A public health approach to population mental wellness. 2021. https://www.cpha.ca/public-health-approach-population-mental-wellness. Accessed 11 Mar 2021.
Cairns KE, Yap MBH, Pilkington PD, Jorm AF. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2014;169:61–75.
Becker TD, Arnold MK, Ro V, Martin L, Rice TR. Systematic review of electronic cigarette use (vaping) and mental health comorbidity among adolescents and young adults. N&TR. 2021;23(3):415–25.
Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood. A systematic review and meta-analysis. JAMA Psychiatry. 2019;76(4):426–34.
Asare M. Sedentary behaviour and mental health in children and adolescents: a meta-analysis.J Child Adolesc Behav. 2015;03(06).
Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. 2014;18(6):521–9.
Khalid S, Williams CM, Reynolds SA. Is there an association between diet and depression in children and adolescents? A systematic review. Br J Nutr. 2016;116(12):2097–108.
Orlando L, Savel KA, Madigan S, Colasanto M, Korczak DJ. Dietary patterns and internalizing symptoms in children and adolescents: a meta-analysis.Aust N Z J Psychiatry. 2021;00048674211031486.
Alamian A, Paradis G. Clustering of chronic disease behavioral risk factors in Canadian children and adolescents. Prev Med. 2009;48(5):493–9.
deRuiter WK, Cairney J, Leatherdale S, Faulkner G. The period prevalence of risk behavior co-occurrence among Canadians. Prev Med. 2016;85:11–6.
Laxer RE, Brownson RC, Dubin JA, Cooke M, Chaurasia A, Leatherdale ST. Clustering of risk-related modifiable behaviours and their association with overweight and obesity among a large sample of youth in the COMPASS study. BMC Public Health. 2017;17:102.
Gardner LA, Champion KE, Grummitt L, Chapman C, Sunderland M, Thornton L, et al. Clustering of six key risk behaviors for chronic disease among adolescent females. IJERPH. 2020;17(19):1–12.
Champion KE, Mather M, Spring B, Kay-Lambkin F, Teesson M, Newton NC. Clustering of multiple risk behaviors among a sample of 18-year-old Australians and associations with mental health outcomes: a latent class analysis. Front Public Health. 2018;6(101616579):135.
Loewen OK, Maximova K, Ekwaru JP, Faught EL, Asbridge M, Ohinmaa A, et al. Lifestyle behavior and mental health in early adolescence. Pediatrics. 2019;143(5):e20183307.
Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across life course. Annu Rev Sociol. 2010;36:139–57.
Statistics Canada. Correlates of vaping among adolescents in Canada. 2022. https://www150.statcan.gc.ca/n1/pub/82-003-x/2022007/article/00003-eng.htm. Accessed 26 Jul 2022.
Canadian Public Health Association. Tobacco and vaping use in Canada: moving forward. 2021. https://www.cpha.ca/tobacco-and-vaping-use-canada-moving-forward. Accessed 26 Jul 2022.
Health Canada. Summary of results for the Canadian Student Tobacco, Alcohol and Drugs Survey 2018-19. 2022. Available from: https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey/2018-2019-summary.html. Accessed 13 Sep 2022.
Leatherdale ST, Brown KS, Carson V, Childs RA, Dubin JA, Elliott SJ et al. The COMPASS study: a longitudinal hierarchical research platform for evaluating natural experiments related to changes in school-level programs, policies and built environment resources.BMC Public Health. 2014 Apr8;14:331.
Battista K, Qian W, Bredin C, Leatherdale ST. Student data linkage over multiple years. Technical Report Series. 2019;6(3): Waterloo, Ontario: University of Waterloo. https://uwaterloo.ca/compass-system/student-data-linkage-over-multiple-years. Accessed 18 Oct 2022.
Burns KE, Vermeer J, Battista K, Leatherdale ST. A School-Level examination of the association between programs and policies and physical activity outcomes among females from the COMPASS study. Int J Environ Res Public Health. 2021;18(6):3314.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (center for epidemiologic Studies Depression Scale). Am J Prev Med. 1994 Apr;10(2):77–84.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Haroz EE, Ybarra M, Eaton WW. Psychometric evaluation of a self-report scale to measure adolescent depression: the CESDR-10 in two national adolescent samples in the United States. J Affect Disord. 2014;158:154–60.
Tiirikainen K, Haravuori H, Ranta K, Kaltiala-Heino R, Marttunen M. Psychometric properties of the 7-item generalized anxiety disorder scale (GAD-7) in a large representative sample of finnish adolescents. Psychiatry Res. 2019;272:30–5.
Downey RG, King C. Missing data in Likert ratings: a comparison of replacement methods. J Gen Psychol. 1998 Apr;125(2):175–91.
Bono C, Ried LD, Kimberlin C, Vogel B. Missing data on the Center for epidemiologic Studies Depression Scale: a comparison of 4 imputation techniques. Res Social Adm Pharm. 2007 Mar;3(1):1–27.
Romano I, Ferro MA, Patte KA, Leatherdale ST. Measurement invariance of the GAD-7 and CESD-R-10 among adolescents in Canada. J Pediatr Psychol. 2022;47(5):585–94.
Health Canada. Eating Well with Canada’s Food Guide. 2011. Available from: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/hpfb-dgpsa/pdf/food-guide-aliment/print_eatwell_bienmang-eng.pdf. Accessed 22 Sep 2019.
Tremblay MS, Carson V, Chaput JP, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(6):S311–27.
Health Canada. Smoking, vaping and tobacco. 2015. https://www.canada.ca/en/health-canada/services/smoking-tobacco.html. Accessed 18 Oct 2022.
Drug Free Kids Canada. Youth and alcohol. https://www.drugfreekidscanada.org/wp-content/uploads/2019/10/DFK_Info_YouthAlcohol_FINAL.pdf. Accessed 18 Oct 2022.
Drug Free Kids Canada. Vaping. https://www.drugfreekidscanada.org/prevention/issues/vaping/. Accessed 22 Jun 2022.
Leatherdale ST, Laxer RE. Reliability and validity of the weight status and dietary intake measures in the COMPASS questionnaire: are the self-reported measures of body mass index (BMI) and Canada’s food guide servings robust? Int J Behav Nutr Phys Act. 2013;10:42.
Leatherdale S, Laxer RE, Faulkner G. Reliability and validity of the physical activity and sedentary behaviour measures in the COMPASS study. COMPASS Technical Report Series. 2014;2(1). Waterloo, Ontario: University of Waterloo. https://uwaterloo.ca/compass-system/publications/reliability-and-validity-physical-activity-and-sedentary. Accessed 18 Oct 2022.
Health Canada. Canada’s Food Guide. 2021. Available from: https://www.canada.ca/en/health-canada/services/canada-food-guides.html. Accessed 13 January 2023.
Statistics Canada, Profile C. 2016 Census. 2017. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E. Accessed 18 Oct 2022.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–3.
Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115(2):291–313.
Angold A, Costello EJ. Puberty and depression. Child Adolesc Psychiatr Clin N Am. 2006;15(4):919–37.
Breslau J, Gilman SE, Stein BD, Ruder T, Gmelin T, Miller E. Sex differences in recent first-onset depression in an epidemiological sample of adolescents. Transl Psychiatry. 2017;7(5):e1139.
Hernán MA. The C-word: scientific euphemisms do not improve causal inference from observational data. Am J Public Health. 2018;108(5):616–9.
Haber NA, Wieten SE, Rohrer JM, Arah OA, Tennant PWG, Stuart EA, et al. Causal and associational language in observational health research: a systematic evaluation. Am J Epidemiol. 2022;191(12):2084–97.
Sampasa-Kanyinga H, Chaput JP, Goldfield GS, Janssen I, Wang J, Hamilton HA, et al. 24-hour movement guidelines and suicidality among adolescents. J Affect Disord. 2020;274:372–80.
Kleppang AL, Haugland SH, Bakken A, Stea TH. Lifestyle habits and depressive symptoms in norwegian adolescents: a national cross-sectional study. BMC Public Health. 2021;21(1):816.
Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427–32.
Le LKD, Esturas AC, Mihalopoulos C, Chiotelis O, Bucholc J, Chatterton ML, et al. Cost-effectiveness evidence of mental health prevention and promotion interventions: a systematic review of economic evaluations. PLoS Med. 2021;18(5):e1003606.
Fenwick-Smith A, Dahlberg EE, Thompson SC. Systematic review of resilience-enhancing, universal, primary school-based mental health promotion programs. BMC Psychol. 2018;6(1):30.
O’Neil A, Jacka FN, Quirk SE, Cocker F, Taylor CB, Oldenburg B, et al. A shared framework for the common mental disorders and non-communicable disease: key considerations for disease prevention and control. BMC Psychiatry. 2015;15:15.
Buchan MC, Romano I, Butler A, Laxer RE, Patte KA, Leatherdale ST. Bi-directional relationships between physical activity and mental health among a large sample of Canadian youth: a sex-stratified analysis of students in the COMPASS study. IJBNPA. 2021;18(1):132.
McMurray RG, Ward DS, Elder JP, Lytle LA, Strikmiller PK, Baggett CD, et al. Do overweight girls overreport physical activity? Am J Health Behav. 2008;32(5):538–46.
Hu MX, Turner D, Generaal E, Bos D, Ikram MK, Ikram MA, et al. Exercise interventions for the prevention of depression: a systematic review of meta-analyses. BMC Public Health. 2020;20(1):1255.
Cummins KM, Marks C. Farewell to bright-line: a guide to reporting quantitative results without the S-word. Front Psychol. 2020. https://doi.org/10.3389/fpsyg.2020.00815.
Wasserstein RL, Schirm AL, Lazar NA. Moving to a world beyond “p < 0.05. Am Stat. 2019;73(sup1):1–19.
Acknowledgements
We would like to acknowledge all students who participated in the COMPASS study and their contribution by completing the surveys.
Funding
This research has been funded by the Stollery Children’s Hospital Foundation and the Alberta Women’s Health Foundation through the Women and Children’s Health Research Institute (Innovation Grant) awarded to PJV. KM holds the Murphy Family Foundation Chair in Early Life Interventions. The COMPASS study has been supported by a bridge grant from the CIHR Institute of Nutrition, Metabolism and Diabetes (INMD) through the “Obesity – Interventions to Prevent or Treat” priority funding awards (OOP-110788; awarded to STL), an operating grant from the CIHR Institute of Population and Public Health (IPPH) (MOP-114875; awarded to STL), a CIHR project grant (PJT-148562; awarded to STL), a CIHR bridge grant (PJT-149092; awarded to KAP/STL), a CIHR project grant (PJT-159693; awarded to KAP), and by a research funding arrangement with Health Canada (#1617-HQ-000012; contract awarded to STL), a CIHR-Canadian Centre on Substance Abuse (CCSA) team grant (OF7 B1-PCPEGT 410-10-9633; awarded to STL), a project grant from the CIHR Institute of Population and Public Health (IPPH) (PJT-180262; awarded to STL and KAP). A SickKids Foundation New Investigator Grant, in partnership with CIHR Institute of Human Development, Child and Youth Health (IHDCYH) (Grant No. NI21-1193; awarded to KAP) funds a mixed methods study examining the impact of the COVID-19 pandemic on youth mental health, leveraging COMPASS study data. The COMPASS-Quebec project additionally benefits from funding from the Ministère de la Santé et des Services sociaux of the province of Québec, and the Direction régionale de santé publique du CIUSSS de la Capitale-Nationale.“
Role of funding body.
The funding source had no role in the design of this study, neither during its execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Contributions
STL conceptualized the COMPASS host study, and KAP conceptualized the COMPASS Mental Health Module. STL and KAP secured funding for the COMPASS host study. PJV, KM, JD, and STL conceptualized the current study and methodology. PJV and KM secured funding and resources for this specific project. PJV, KM, and JD developed a statistical analysis plan, and AA analyzed the data. JD interpreted the results and drafted the manuscript. PJV, KM, STL, AA, and KAP reviewed the original draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The University of Waterloo Office of Research Ethics (ORE: 30118) and appropriate School Board committees approved all procedures, including passive consent. Analyses presented in this study were approved by the Research Ethics Board at the University of Alberta (Pro00103881).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12966_2023_1436_MOESM1_ESM.docx
Supplementary Material 1 Table S1. Associations of individual adherence to 12 lifestyle recommendations with the CESD-R-10 and GAD-7 scores at baseline
12966_2023_1436_MOESM2_ESM.docx
Supplementary Material 2 Table S2. Associations of overall adherence to 12 lifestyle recommendations with CESD-R-10 and GAD-7 scores at baseline
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dabravolskaj, J., Veugelers, P.J., Amores, A. et al. The impact of 12 modifiable lifestyle behaviours on depressive and anxiety symptoms in middle adolescence: prospective analyses of the Canadian longitudinal COMPASS study. Int J Behav Nutr Phys Act 20, 45 (2023). https://doi.org/10.1186/s12966-023-01436-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-023-01436-y