Abstract
Background
Previous studies have shown that multicomponent interventions may improve meal frequency and eating habits in children, but evidence among young people is limited. This study evaluated the effect of the Healthy High School (HHS) intervention on daily intake of breakfast, lunch, water, fruit, and vegetables at 9-month follow-up.
Methods
The study included first-year students (≈16 years) attending high school in Denmark. Participating schools were randomized into the HHS intervention (N = 15) or control group (operating as usual) (N = 15). The intervention was designed to promote well-being (primary outcome) by focusing on healthy habits including meals, stress prevention, and strong peer relations. It included a curriculum, structural and organisational initiatives, a workshop, and a smartphone application. Students completed self-administered online questionnaires at the beginning of the school year and nine months later. To account for clustering of data, we used multilevel logistic regression analyses to estimate odds ratios (OR). We applied an intention-to-treat approach with multiple imputations of missing data.
Results
At baseline 4577 of 5201 students answered the questionnaire and 4512 at follow-up. In both groups the proportion of students eating breakfast decreased from approximately 50% to 40% from baseline to follow-up, and lunch frequency decreased from approximately 50% to 47%. Daily water intake, intake of fresh fruit and intake of vegetables remained unchanged from baseline to follow-up. There were no significant between group differences on any of the outcomes at first follow-up: breakfast: OR = 0.85 (95% CI: 0.65;1.10), lunch: OR = 0.96 (95% CI: 0.75;1.22), water intake: OR = 1.14 (95% CI: 0.92;1.40), intake of fresh fruit: (OR = 1.07, 95% CI: 0.84;1.37), vegetables: (OR = 1.01, 95% CI: 0.77;1.33).
Conclusion
No evidence of an effect of the HHS intervention was found for any of the outcomes. Future studies are warranted to explore how health promoting interventions can be integrated in further education to support educational goals. Moreover, how to fit interventions to the lives and wishes of young people, by also including systems outside of the school setting.
Trial registration
ISRCTN, ISRCTN43284296. Registered 28 April 2017 - retrospectively registered.
Similar content being viewed by others
Introduction
Eating patterns among Danish high school students (≈15–20 years old) are, as among most young people in western countries, characterized by more frequent meal skipping than in younger children [1, 2] and a low intake of water [3, 4], fruit, and vegetables [1,2,3, 5]. Danish Authorities recommend a daily intake of at least 600 g of fruit and vegetables and approximately 1–1.5 l water per day [6]. Up to half of Danish 15–18 year-olds skips breakfast at least once a week, and two-thirds skip lunch [2, 3, 7]. Two-fifths of high school students eat fruit daily, and more than 90% eat vegetables at least 2–4 times a week [2, 7]. In Denmark, water represents on average only 44% of 13–18-year-olds’ daily fluid intake corresponding to about 700 ml/day [8]. Furthermore, girls tend to eat more fruit and vegetables than boys [1, 3, 7, 9] but also to skip breakfast more often [1, 7, 10, 11]. Children and young people of low socioeconomic position report a lower intake of fruit and vegetables [1, 9] and to skip breakfast [1, 12, 13] and lunch [12, 13] more often than children and young people of high socioeconomic position.
The eating patterns among young people are worrying as they may negatively affect diet quality [10, 14], health, and well-being [15,16,17,18] but also track into adulthood with an increased risk of non-communicable diseases [19,20,21,22,23,24]. Healthy meal and eating habits may contribute to the prevention of overweight and obesity in young people [15] as well as maintenance of a healthy body weight and optimal cardiometabolic health [25]. Moreover, regular meals positively affect cognitive function, academic performance, learning abilities and school attendance [17, 26, 27]. The replacement of juice, milk, and diet or sugar-sweetened beverages (SSB), with water may reduce the total energy intake [28] and be beneficial in weight management [29].
Internationally, evidence regarding effective school-based multicomponent interventions targeting meal frequency and eating habits among young people (> 16 years) is limited [30,31,32]. Similarly, no previous dietary intervention studies have targeted this older age group in Denmark, while some multicomponent intervention studies have succeeded in improving dietary outcomes among children and adolescents in primary schools [8] through free provision of school meals [33, 34] and fruit and vegetables [35].
Among children (< 16 years) international reviews suggest that school-based multicomponent interventions including educational, policy, and environmental components, as well as parent involvement, are more effective in promoting healthy meal habits than single-component interventions [30, 32, 36]. Moreover, healthy and unhealthy behaviours tend to cluster [17, 37, 38] and multi-behavioural interventions aimed at improving nutrition and physical activity simultaneously have shown a better effect on weight-related outcomes than dietary or physical interventions alone [30]. This calls for a broad approach to health promotion among young people, that consider multiple factors at the same time [38]. A needs assessment among Danish high school students and staff found that students experienced that their transition to high school had resulted in unhealthy eating habits and more frequent meal skipping which made them feel tired and unable to concentrate. Most student brought their lunch from home as shown in another study [39]. Other options were to buy food in the school canteen or nearby supermarkets and restaurants. Student expressed that the options in the canteen made them eat unhealthier and they would like to have healthier options. We also found that the canteen management most often has full autonomy of their selection primarily because they are run by private actors. Making it an interesting arena for an intervention. Interviewed principals, teachers, and student counsellors highlighted that compared to primary school high schools were characterized by more self-dependent students and less school-home collaboration with parents, which questions whether a parental component is suitable in the high school setting (Bonnesen et al. unpublished).
This paper aims to examine the effect of the multi-behavioural multicomponent Healthy High School (HHS) intervention on meal frequencies and eating habits among first-year high school students (≈16 years old) at the end of the school year, in which the intervention was implemented. The paper reports the findings for daily intake of breakfast, lunch, and amount of daily water intake (secondary outcomes of the HHS study), and intake of fruit and vegetables (explorative outcomes of the HHS study). Furthermore, we will examine if the intervention effect differs by gender and socioeconomic position.
Methods
The HHS intervention
The overall aim of the HHS intervention was to promote well-being (primary outcome) among first-year high school students in Denmark. The intervention was tested in a cluster-randomized controlled trial (RCT). The trial is registered in ISRCTN, ISRCTN43284296 (28 April 2017 - retrospectively registered) and the trial design been described in detail elsewhere [40].
The Intervention Mapping approach was used to develop the programme theory and intervention components and to plan the evaluation systematically based on a comprehensive needs assessment compiling evidence, theory, and knowledge about the context and target group [40, 41]. As part of the needs assessment we conducted 1) 16 focus group interviews with students (n = 74), two focus group interviews (n = 7) and five single interviews with principals, teachers, and student counsellors at high schools and telephone interviews with two canteen managers; 2) a brainstorm session with students and school staff to explore the feasibility of early intervention ideas and schools’ capacity to implement; 3) an epidemiological assessment using existing questionnaire data from more than 70.000 Danish high school students; 4) literature reviews of determinants of the five secondary outcomes and previous school-based multicomponent or multiple health behaviour change interventions (Bonnesen et al. unpublished).
The needs assessment identified stress prevention and promotion of regular meals, physical activity, and sleep as well as students’ sense of community at school as five important pathways to achieve a higher level of well-being (Bonnesen et al. unpublished). The intervention consisted of four intervention components (Table 1) which combined educational and environmental initiatives and were designed to change important and modifiable determinants of these five secondary outcomes: a curriculum; a catalogue specifying organisational and environmental changes for a supportive school environment; ‘Young & Active’ - a peer-led innovation workshop to initiate school-based movement activities; and a smartphone application (app) [40] (Bonnesen et al. unpublished). The intervention was implemented among first-year high school students in the school year 2016/2017. This paper focuses on the dietary outcomes of the intervention. The primary outcome (well-being) as well as the outcomes of the four other pathways to well-being will be reported elsewhere.
Setting
Education in Denmark is financed by taxes and therefore free of charge. All children in Denmark are obligated to primary schooling from age 6–7 to 15–16 years (9th grade). Afterwards they may choose to attend further education (e.g., upper secondary school – admission can require certain grades or assessments from teachers or counsellors) or to enter the labour market without prior training. The upper secondary school leaving examination is one of five general upper secondary education and training programmes in Denmark that qualifies for access to higher education. In this paper we apply the term ‘high school’ (in Danish: gymnasium) to refer to this three-year program [43]. Approximately 70% of young people in Denmark get enrolled in high school, after they finish 9th or 10th grade. Thus the high school setting provides an opportunity to reach a large proportion of young people [44].
Study design and participants
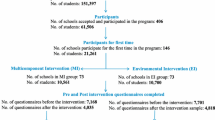
We invited schools that had previously participated in the Danish National Youth Study 2014 (the sampling strategy has been described in detail elsewhere [40]). Thirty-one of 92 invited schools agreed to participate (33.7%). The participating schools were randomized into the intervention (n = 16) and the control group (n = 15) by computer-based random number generation. One intervention school withdrew from the study after randomization, leaving a total of 30 schools (Fig. 1) [40]. Sample size calculations showed that a minimum of 26 schools of 224 students in each group were required to detect a between group difference for the primary outcome well-being [40] which make the final school and student sample illustrated in Fig. 1 sufficient. Control schools received no intervention and were asked to continue operating as usual. A refined version of the intervention material was not offered to the control schools before the summer 2020 to avoid that collection of process and effect evaluation data was influenced by spill over effects to control schools.
Data collection
At the beginning of the school year (August 2016), before intervention start, and at the end of the school year (May 2017) each school was responsible for allocating a 45-min-lesson for students to completed a self-administered online questionnaire (220 items at baseline, 253 items at follow-up) in class after a standardized instruction given by their teacher [40].
Similarly, the principals were to answer an online questionnaire at the two time points, regarding school characteristics, organisational issues, and facilities, as well as the nearby environment (e.g. access to supermarkets and restaurants) [40]. The online format enabled the principals to complete the questionnaire when it was convenient for them.
Outcome measures
Meal frequency was evaluated by the questions: “How often do you eat the following meals during the week (Monday to Friday)?” 1) “Breakfast (more than a glass of juice or milk)” and 2) “Lunch” with the response options “no days”, “one day”, “two days”, “three”, “four days” and “five days”; And the question “How often do you eat the following meals on weekends?” 1) “Breakfast (more than a glass of juice or milk)” 2) “Lunch” with the response options “no days”, “1 day” and “2 days”. For each meal (breakfast and lunch), the student responses were combined and dichotomized into daily vs 6 days or less a week.
Amount of daily water intake was measured by the question: “How many glasses of water do you drink on average a day (just water/sparkling water, not squash, coffee, tea or other fluids that contains water)?” with the response options “0 glasses” adding one glass until the final option “8 glasses or more” (one glass was estimated to 250 ml). Student responses were dichotomized into ≥4 glasses (1 l or more) a day vs < 4 glasses a day (less than 1 l). The cut-off point of 1 l per day was based on the Nordic Nutrition Recommendation 2012 (NNR 2012) of drinking 1–1.5 l of water per day, depending on activity level, season, and body composition [45].
Intake of fruit and intake of vegetables was measured by the question “On a normal week: How often do you eat …? ” 1) “… fresh fruit”; 2) “… vegetables, raw or cooked (not potatoes)”, with the response options “never”, “less than 1 day a week”, “1 day a week”, “2-4 days a week”, “5-6 days a week”, “every day once a day” and “every day twice or several times a day”. To realistically reflect adherence to dietary recommendations, without knowing the amount eaten, the responses for the intake of fruit and vegetables respectively were dichotomized: twice or several times daily (at least twice a day) vs once a day or less.
Covariates
Covariates strongly correlated with the outcomes of interest were included to increase the precision of the effect estimates [46]. Gender was measured by the question “What is your gender” with the categories “Boy” and” Girl”. Parental occupational social class (OSC) was measured by the questions “Does your father/mother have a job?”, “If no, why does he/she have no job?”, “If yes, please say in what place he/she works (for example hospital, bank, restaurant) and please write down exactly what job he/she does there (for example teacher, bus driver)”. Based on standardised guidelines the answers were coded into OSC from I (high) to V (low) by the research group [47]. We added an extra category for economically inactive parents who receive unemployment benefits, disability pension or other kinds of transfer income. Based on the highest-ranking parent each student was categorized into four levels of OSC: High (I-II e.g., professionals and managerial positions), middle (III-IV, e.g. technical and administrative staff, skilled workers), low (V, unskilled workers and economically inactive) and unclassifiable.
Statistical analyses
At baseline 4577 answered the questionnaire (response rate = 88.0%), and at follow-up 3426 answered the questionnaire (response rate = 75.9%). .
Baseline data from students and principals were used to characterize the study population and to compare students and schools from the intervention and control group. The main effect analysis applied an intention-to-treat (ITT) approach with multiple imputations of missing data. The imputation was based on variables from the baseline questionnaire which were expected to be associated with the pre-planned outcome measures or loss to follow-up e.g. gender, socio-economic position, and other health behaviours [48].
To allow for correlation between students from the same class and high school, we used multilevel logistic regression analyses to estimate the association between the intervention and the outcomes, with students (level 1) nested within classes (level 2), and classes nested within high schools (level 3). The crude model included the intervention group only. The main model included the intervention group and covariates; baseline level of the specific outcome, gender, and OCS at student-level. School and school class were included as random effects. Intervention group and covariates were included as fixed effects. The intervention was designed as a universal intervention to affect all students. However, as both gender and socioeconomic differences in the outcomes of interest have been demonstrated, we investigated differential effects of the intervention by gender and OSC in explorative subgroup analyses, using the imputed data set.
The statistical analyses were carried out using SAS, version 9.4 (SAS Institute, Inc., Cary, NC) and a significance level of 0.05 was chosen a priori. All analyses were pre-specified in a statistical analysis plan which was approved by all co-authors before the analyses were performed.
Sensitivity analyses
Sensitivity analyses were carried out on complete case data sets for all outcomes. We also analysed alternative cut-off points for meal frequencies (‘daily Monday-Friday’ vs ‘four days or less’), the amount of daily water intake (‘≥6 glasses a day (1.5 litres)’) and frequency of fruit and vegetable intake (‘at least five days a week’), to investigate whether the intervention only affected students’ intake during school days and higher consumption of water. We also analysed the intervention effect on the combined intake of both fruit and vegetables as they are treated as one food group in dietary recommendations [6].
Attrition analyses
We performed attrition analyses for all covariates and outcomes of interest on each complete case data set. We performed chi-square test and logistic regression analyses to test for any significant differences between the intervention and control group among students who were either lost to follow-up or had missing data on items included in the complete data sets.
Results
Baseline characteristics
At baseline, students at intervention and control schools shared similar characteristics (Table 2). Just above 60% of the students were girls, the mean age was 16 years, and almost half of the students were categorized as high OSC. Half of the students reported to eat breakfast and lunch daily. Larger proportions of students had breakfast daily during weekends compared to school days (Monday-Friday), while smaller proportions had lunch daily during the weekend. Around 70% of students reported drinking at least 1 l of water per day. Less than one-sixth ate fresh fruit and vegetables at least twice a day.
Principal questionnaire data showed that more intervention schools had access to fast food (n = 12) and healthy lunch (n = 12) from nearby restaurants than control schools (fast food n = 9, healthy lunch n = 6). All schools except one control school had a canteen. Most schools had access to free, cold, clean water from a hygienic source for students, but more intervention schools had water fountains available compared to control schools (data not shown).
Attrition analyses
Of the 5201 students invited at baseline (Fig. 1), 689 students were lost to followup as they dropped out of school/moved to another school. There were around 30% students with missing data on items included in the complete data sets; breakfast frequency (n = 1334, out of total 4512), lunch frequency (n = 1352, out of total 4512), amount of daily water intake (n = 1327, out of total 4512), frequency of fresh fruit intake (n = 1335, out of total 4512), frequency of vegetables intake (n = 1356, out of total 4512).
There were no noticeable differences in baseline characteristics between the complete case and imputed data set, except for a higher proportion (almost 10%-points) of students who reported having breakfast in the complete case data set, and a slight tendency of more favourable proportions for the other outcomes compared to the imputed cases data set (Table S1).
We found no significant differences in the attrition between the intervention and the control group according to gender, OSC, baseline breakfast or lunch frequency, amount of daily water intake, and frequency of vegetable intake. However, more students at intervention schools who reported to eat fruit at least twice a day at baseline were lost to follow-up, compared to students at control schools (16.2% versus 12.4%) (data not shown).
Effect of the HHS intervention on meal frequency and eating habits
In both groups, the proportion of students who reported to have breakfast daily decreased from approximately 50% at baseline to around 40% at follow-up. Around half of students in both groups had lunch daily at baseline, while this proportion was 46.3% for students at intervention schools and 48.6% for students at control schools at follow-up. In both groups, the proportion of students who had four or more glasses (≥1 l) of water a day were approximately 70% at both time points. In both groups 14–15% of the students ate fresh fruit at least twice a day at both baseline and follow-up. Around 15.5% of the intervention students and 14.3% of the control students reported eating vegetables at least twice a day at baseline and this proportion increased to 16% at follow-up in both groups.. Data showed tendencies of gender and socioeconomic differences in all outcomes. A larger proportion of boys reported to eat breakfast and lunch and to drink at least 1 litre of water daily than girls, whereas a larger proportion of girls reported to eat fresh fruit or vegetables, than boys (Table S3 and S4). There was a social gradient in all outcomes. Students of high OSC more frequently reported to have regular meals, drink water and eat fruit and vegetables at least twice a day (Table S3 and S4).
We found no significant between group difference on frequency of breakfast (OR = 0.85, 95%CI: 0.65;1.10), and lunch intake (OR = 0.96, 95%CI: 0.75;1.22), daily amount of water intake (OR = 1.14, 95% CI: 0.92;1.40), intake of fresh fruit (OR = 1.07, 95% CI: 0.84;1.37) or vegetables (OR = 1.01, 95% CI: 0.77;1.33) in the adjusted ITT analyses (Table 3). Similarly, the sensitivity analyses of complete cases (Table 3) and alternative cut-points (Table S2) did not either show any evidence of an intervention effect. For the daily amount of water intake (< 1,5 l per day), the complete case analysis became borderline significant (OR = 1.26 (95% CI: 1.01;1.57) (Table S2). We found no significant between group difference on any of the outcomes in the explorative subgroup analyses (Fig. 2 and Table S4).
Effect of the Healthy High School intervention at 9-month follow-up on meal frequency and water consumption stratified by gender and parental occupational social class (OSC). Analyses on imputed data sets. Analyses on gender effects were adjusted for baseline level of outcome and OSC. Analyses on OSC effects were adjusted for baseline level of outcome and gender
Discussion
The HHS study is one of the first studies aimed at promoting meal frequency and healthy eating habits among young people in high school. We found no evidence of an effect of the HHS intervention on meal frequency, daily amount of water intake, or intake of fruit and vegetables in the total study sample nor in specific subgroups The intervention may be ineffective due to low implementation levels (implementation failure), misspecification of the working mechanisms (theory failure), and/or measurement error.
Implementation failure
The HHS intervention was designed to promote regular meals and healthy eating habits by influencing individual, social, and environmental determinants. The canteen initiative addressed environmental determinants i.e., availability, whereas individual determinants such as knowledge and skills were primarily targeted by the HHS app and the HHS curriculum, which both were subject to low implementation. The delivery of the app to the students was delayed significantly due to re-organisations in the app development company and the intended synergy from launching all intervention components at the same time on awareness of the app was compromised (Table 1). This challenged students’ uptake of the app, together with the need for using a code to install the app (Table 1). Raw data from the HHS app showed that 1080 intervention students (45.5% of those invited) downloaded the app, however only 246 (15.7%) students answering the follow-up questionnaire reported to have used the HHS app. Among those who had not used the HHS app the main reason was that they had never heard about the app (27.2%) (unpublished data).
A new educational reform and spending cuts challenged teachers’ implementation of the HHS curriculum. Among 108 teachers responding a process evaluation questionnaire at follow-up, only 39.7% delivered the HHS curriculum, ranging from 0% at some schools to 66.7% at other schools [49]. Between one-fourth and half of intervention students reported to have received each of the five lessons aimed at healthy eating (unpublished data). Thus, important individual determinants were not addressed as planned whereas all except one of the intervention schools implemented the canteen initiative and thereby addressed school-environmental determinants. The process evaluation studies showed that most canteens had followed the consultants’ advice and had changed one or a few products to a healthier alternative e.g. by reducing the content of salt or substituting white bread and pasta with wholegrain products [50]. An intervention at vocational schools used a similar strategy on gradually making a healthier assortment in canteens [51]. Canteens increased their share of healthier food products from 60 to 80% of the assortment over 10 months and increased their sale of healthy products [51]. This effect was found to be even higher when the changes were gradually implemented (60% to 70% to 80%) instead of abruptly (60% to 80%) [51]. Similarly, the interviewed canteen staff in our study underlined the importance of slow and small changes to lure the students in and not ‘scare’ them off [50].
Implementation of structural initiatives [52,53,54] and complex interventions [55] takes time and 9-month follow-up may be too early to detect the effect of the canteen initiative. However, our process evaluation showed that the canteen staff’s motivation to implement dropped during the intervention year [50] which speaks against this hypothesis.
Looking strictly at breakfast frequency, previous studies have shown that free breakfast at school [56] and low-cost grab and go breakfast at the school [57] is positively associated with breakfast consumption. The HHS intervention did focus on making especially breakfast more available at school, by encouraging canteen staff to provide affordable and healthy breakfast options, or for the school to implement common breakfast for all first-year students. However, the common breakfast was not a mandatory initiative and no schools implemented it. Furthermore, some canteen owners were reluctant to expand their selection of breakfast options, as they did not experience a demand for it.
The program theory revisited
The program theory assumed that the canteen initiative would prompt the students to buy food in the canteen. However, approximately half of the intervention students never or less than once a week bought food in the canteen for lunch. This proportion remained rather stable towards follow-up. At both baseline and follow-up, more than 60% of students ate packed lunch on most school days (at least 3 days a week). These trends were similar at control schools (unpublished data). Similarly, a Danish study found that 43% of 15–19 year-olds eat food that is prepared at home for lunch e.g. packed lunch [39]. The project group took this into account by sharing recipes for healthy packed lunch, for student to prepare at home, in the app. However, as mentioned previously, few students used the app. Of those who had downloaded the app just 7% had read one or more articles about diet (which included the recipes), 6% used the tracking of water intake, and 5% completed a test on eating and meal habits. In both groups, one-fifth of students at baseline and one-fourth at follow-up bought lunch outside of school (e.g., kiosk, supermarket, fast food restaurants) 1–2 days a week (unpublished data) and many opportunities were available for buying foods and snacks around the schools participating in the HHS study. A previous study found that only 1% of revenues in the canteens at four vocational schools in the Netherlands came from sales of fruit and vegetables [51], which may explain the lack of effect of the HHS intervention on the intake of fruit and vegetables.
The HHS intervention might have benefitted from including a parental component addressing the home environment and parental behaviour as parental involvement is crucial for the promotion of healthy eating habits among 10–18 years-olds [32, 58]. However, based on the needs assessment and recommendations from school staff and students, a parental component was not considered feasible within the high school setting nor beneficial for the students’ uptake of the intervention as they strive for independence. Future qualitative studies should explore parental perspectives on, if, and how they would to be involved in high school-based interventions. Even with a parental component, scholars argue, that school-based interventions often fail, as student behaviour is affected by many other settings than school and families. This calls for more upstream initiatives and a whole system approach to improve health and health-related behaviour in children and young people [59,60,61].
Mismatch between intervention focus and outcome measures
Based on previous effective interventions [56, 57, 62, 63], the canteen initiative was developed to increase access to cheap and healthy breakfast, lunch and snacks at the school. Meanwhile, the initiative ended up focusing more on the nutritional values of the food than intended as the recruited intervention provider - the canteen consultant - used the scoring system “Kantinetjekket|Buffet” (in English “Canteencheck|Buffet”) (Table 1) . Changes in nutritional values e.g., salt content were not captured by our broad outcomes of meal frequency and eating habits. We had to keep the number of items measuring food intake to a minimum due to the many outcomes of interests of the overall HHS study. As we only measured meal frequency and overall eating habits, we do not know whether the intervention resulted in e.g., a healthier breakfast among students eating breakfast. However, as many of the canteen changes were quite invisible e.g., adding more wholegrain flour in the bread, the students would probably not have noticed and been able to report that they ate more wholegrain when they bought lunch in the school canteen. A recent review found that school-based interventions aimed at improving food behaviours through nudging are positively associated with food selection, but often fail to detect an effect on actual consumption as it is not measured, or measures on food waste is not taken into consideration [64].
Strengths and limitations
The previous sections have elaborated on study limitations related to implementation levels, programme theory, and outcome measures. Strengths of the HHS study include; 1) the RCT design, 2) the high response rate of students, 3) the use of multilevel modelling taking the clustering of the data into account, 4) the long duration of the intervention, 5) the systematic, transparent planning process guided by the Intervention Mapping Protocol [41] (Bonnesen et al. unpublished), based on a thorough mixed-methods needs assessment analysis (Bonnesen et al. unpublished), use of behavioural and environmental change theory [65] and the best available evidence in the field [30, 32]. Moreover, the HHS intervention design acknowledges the complex drivers of young peoples’ health behaviour including the clustering of behaviour and uses several initiatives to target determinants on both an environmental, interpersonal, and individual level.
Public health implications
Scholars have called for environmental initiatives [55, 66,67,68,69], and the HHS canteen initiative could inspire future interventions. The process evaluation showed promising results for the initiative in changing the canteen selection. Canteen staff expressed appreciation for the consultant‘s tailored advice and the “health-check” of the canteen [50]. However, their motivation lowered during the intervention period. Future studies may consider multiple consulting meetings to uphold the motivation and sustain positive changes in the school canteen. Environmental initiatives such as provision of free school meals which has shown positive health effects in younger children in Sweden [70] could be interesting to test in this age group.
We found a relative low use of the app, which has been argued could be due to implementation failure. Moreover, some students reported that reasons for not using the app were that the app was not interesting that they had other apps already with similar features. This study thereby highlights the possible pitfalls and barriers to the use of an app. However, we still find it relevant to explore how technology as apps can be used to target important individual determinants in interventions.
The HHS intervention aimed to support students in replacing unhealthy choices with more healthy choices. Future studies should investigate the effect of the intervention on intake of unhealthy snacks and SSB and the effect of the initiative on all outcomes of interests at 20-month follow-up to explore the sustainability of the intervention and the hypothesis that implementation takes time [40]. Furthermore the interplay between snack behaviour and meal frequencies is an interesting area of research as some might skip meals for snacks or report meals as snacks. Moreover, it is warranted to develop valid outcome measures to detect the possible small changes in student’s eating habits that might have occurred from the changes we observed in the canteens.
Despite showing no evidence of an effect of the HHS intervention, the descriptive findings underline the continued need for effective initiatives targeting meal frequency and eating habits among high school students in Denmark, to ensure health and well-being in both youth and adult life. Future studies could benefit from looking beyond the school setting and include several systems [59,60,61].
Conclusion
This study evaluated the effect of the multicomponent school-based HHS intervention in 16-year-old students on meal frequencies, amount of daily water intake, intake of fresh fruit and intake of vegetables at 9-month follow-up. We found no evidence of an effect of the intervention on any of the outcomes in the total study population nor specific subgroups.
The descriptive data shows that at least 40% of Danish high school students skip breakfast and/or lunch, and approximately 70% do not drink enough water. Also, only one out of seven eats fresh fruit or vegetables at least twice a day, respectively. This highlights the continued need for effective interventions targeting meal frequencies and eating habits among young people in Denmark. Based on some of the newest literature it is warranted that future interventions should include the whole system of young people’s lives and focus more on interventions at several structural levels, and not just the school setting. Moreover, is it needed to explore further how to successfully engage high schools in health promoting activities.
Availability of data and materials
The data sets generated and/or analysed during the current study are not publicly available due to the sensitivity of data but are available from the corresponding author on reasonable request.
Abbreviations
- SSB:
-
Sugar-sweetened beverage;
- HHS:
-
Healthy High School study
- app:
-
Smartphone application
- OSC:
-
Parental occupational social class
- ITT:
-
Intention-to-treat
- RCT:
-
Randomized controlled study
References
Inchley J, Currie D, Budisavljevic S, Torsheim T, Jåstad A, Cosma A. Spotlight on adolescents health and well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) survey in Europe and Canada. Copenhagen: WHO Regional Office for Europe; 2020. (Key findings). Report No.: Volume 1.
Pisinger V, Thorsted A, Jezek AH, Jørgensen A, Christensen AI, Thygesen LC. UNG19 - Sundhed og trivsel på gymnasiale uddannelser 2019 [Internet]. Copenhagen: The National Institute of Public Health; 2019. Available from: www.sdu.dk/sif
Pedersen AN, Christensen T, Matthiessen J, Knudsen VK, Rosenlund-Sørensen M, Biltoft-Jensen A, et al. Danskernes kostvaner 2011–2013: hovedresultater. DTU Fødevareinstituttet, Afdeling for Ernæring: Søborg; 2015.
Popkin BM, D’Anci KE, Rosenberg IH. Water, hydration and health. Nutr Rev. 2010;68(8):439–58.
Beal T, Morris SS, Tumilowicz A. Global Patterns of Adolescent Fruit, Vegetable, Carbonated Soft Drink, and Fast-Food Consumption: A Meta-Analysis of Global School-Based Student Health Surveys: Food and Nutrition Bulletin [Internet]. 2019 16 [cited 2020 Jul 16]; Available from: https://journals.sagepub.com/doi/10.1177/0379572119848287?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0www.ncbi.nlm.nih.gov
Fødevarestyrelsen, Ministeriet for Fødevarer, Landbrug og Fiskeri. De officielle kostråd - godt for sundhed og klima [Internet]. Fødevarestyrelsen; 2020. Available from: https://altomkost.dk/fileadmin/user_upload/altomkost.dk/Billeder/Alt_om_kost/De_Officielle_Kostraad_november_2020/ONLINE_Kostraad_pjece_2021.pdf
Bendtsen P, Schou Mikkelsen S, Tolstrup JS, Statens Institut for Folkesundhed. Ungdomsprofilen 2014: sundhedsadfærd, helbred og trivsel blandt elever på ungdomsuddannelser. Statens Institut for Folkesundhed; 2015.
Tetens I, Biltoft-Jensen A, Hermansen K, Mølgaard C, Nyvad B, Rasmussen M, et al. Fremme af sunde mad- og måltidsvaner blandt børn og unge. Kbh: Vidensråd for Forebyggelse. 2018.
Rasmussen M, Krølner R, Klepp K-I, Lytle L, Brug J, Bere E, et al. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part I: quantitative studies. Int J Behav Nutr Phys Act. 2006;3(1):22.
Sjöberg A, Hallberg L, Höglund D, Hulthén L. Meal pattern, food choice, nutrient intake and lifestyle factors in the Göteborg adolescence study. Eur J Clin Nutr. 2003;57(12):1569–78.
Pedersen T, Meilstrup C, Holstein BE, Rasmussen M. Fruit and vegetable intake is associated with frequency of breakfast, lunch and evening meal: cross-sectional study of 11-, 13-, and 15-year-olds. Int J Behav Nutr Phys Act. 2012;9(1):9.
Utter J, Denny S, Crengle S, Ameratunga S, Clark T, Maddison R, et al. Socio-economic differences in eating-related attitudes, behaviours and environments of adolescents. Public Health Nutr. 2011;14(4):629–34.
El-Gilany A-H, Elkhawaga G. Socioeconomic determinants of eating pattern of adolescent students in Mansoura, Egypt. Pan Afr Med J [Internet]. 2012 1 [cited 2020 Jul 17];13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527023/
Rodrigues PRM, Luiz RR, Monteiro LS, Ferreira MG, Gonçalves-Silva RMV, Pereira RA. Adolescents’ unhealthy eating habits are associated with meal skipping. Nutrition. 2017 Oct 1;42:114–120.e1.
Mesas AE, Muñoz-Pareja M, López-García E, Rodríguez-Artalejo F. Selected eating behaviours and excess body weight: a systematic review. Obes Rev. 2012;13(2):106–35.
Szajewska H, Ruszczyński M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit Rev Food Sci Nutr. 2010;50(2):113–9.
Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc. 2005;105(5):743–60.
Niemeier HM, Raynor HA, Lloyd-Richardson EE, Rogers ML, Wing RR. Fast food consumption and breakfast skipping: predictors of weight gain from adolescence to adulthood in a nationally representative sample. J Adolesc Health. 2006;39(6):842–9.
Pedersen TP, Holstein BE, Flachs EM, Rasmussen M. Meal frequencies in early adolescence predict meal frequencies in late adolescence and early adulthood. BMC Public Health. 2013;13(1):445.
Mikkilä V, Räsänen L, Raitakari OT, Pietinen P, Viikari J. Longitudinal changes in diet from childhood into adulthood with respect to risk of cardiovascular diseases: the cardiovascular risk in young Finns study. Eur J Clin Nutr. 2004;58(7):1038–45.
Lien N, Lytle LA, Klepp K-I. Stability in consumption of fruit, vegetables, and sugary foods in a cohort from age 14 to age 21. Prev Med. 2001;33(3):217–26.
Kelder SH, Perry CL, Klepp KI, Lytle LL. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am J Public Health. 1994l;84(7):1121–6.
Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017 01;46(3):1029–56.
Yip CSC, Chan W, Fielding R. The associations of fruit and vegetable intakes with burden of diseases: a systematic review of Meta-analyses. J Acad Nutr Diet. 2019 Mar 1;119(3):464–81.
St-Onge M-P, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation [Internet]. 2017 Feb 28 [cited 2020 Jul 1];135(9). Available from: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000476
Stovgaard M, Thorborg MM, Bjerge HH, Andersen BV, Wistoft K. Rammer for mad og måltider i skolen: en systematisk forskningskortlægning. DCA - Nationalt Center for Fødevarer og Jordbrug: Tjele; 2017.
Stovgaard M, Thorborg MM. Rammer for mad og måltider i skolen. DCA - Nationalt Center for Fødevarer og Jordbrug: Tjele; 2017.
Daniels MC, Popkin BM. The impact of water intake on energy intake and weight status: a systematic review. Nutr Rev. 2010 Sep;68(9):505–21.
Zheng M, Allman-Farinelli M, Heitmann BL, Rangan A. Substitution of sugar-sweetened beverages with other beverage alternatives: a review of long-term health outcomes. J Acad Nutr Diet. 2015;115(5):767–79.
De Bourdeaudhuij I, Van Cauwenberghe E, Spittaels H, Oppert J-M, Rostami C, Brug J, et al. School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project: school-based nutrition and PA interventions. Obes Rev. 2011;12(3):205–16.
Van Cauwenberghe E, Maes L, Spittaels H, van Lenthe FJ, Brug J, Oppert J-M, et al. Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: systematic review of published and ‘grey’ literature. Br J Nutr. 2010;103(6):781–97.
Meiklejohn S, Ryan L, Palermo C. A Systematic Review of the Impact of Multi-Strategy Nutrition Education Programs on Health and Nutrition of Adolescents. Journal of Nutrition Education and Behavior. 2016 Oct;48(9):631–646.e1.
Sabinsky M. Healthy eating at schools: how does a school food programme affect the quality of dietary intake at lunch among children aged 7–13 years? [internet]. National Food Institute: Technical University of Denmark; 2013 [cited 2021 Jul 22]. Available from: https://orbit.dtu.dk/en/publications/healthy-eating-at-schools-how-does-a-school-food-programme-affect
Andersen R, Biltoft-Jensen A, Christensen T, Andersen EW, Ege M, Thorsen AV, et al. Dietary effects of introducing school meals based on the new Nordic diet – a randomised controlled trial in Danish children. The OPUS school meal study. Br J Nutr. 2014;111(11):1967–76.
Krølner R, Suldrup Jørgensen T, Aarestrup AK, Hjøllund Christiansen A, Christensen AM, Due P. The boost study: design of a school- and community-based randomised trial to promote fruit and vegetable consumption among teenagers. BMC Public Health. 2012;12(1):191.
Kothe EJ, Mullan B. Increasing the frequency of breakfast consumption. British Food Journal [Internet]. 2013 [cited 2020 Mar 18]; Available from: https://www.emerald.com/insight/content/doi/10.1108/00070701111140115/full/html
Sleddens EF, Kroeze W, Kohl LF, Bolten LM, Velema E, Kaspers PJ, et al. Determinants of dietary behavior among youth: an umbrella review. International Journal of Behavioral Nutrition and Physical Activity [Internet]. 2015 Dec [cited 2019 May 13];12(1). Available from: https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-015-0164-x
Nutbeam D, Aarø L, Wold B. The lifestyle concept and health education with young people: results from a WHO international survey. World Health Stat Q. 1991 Feb 1;44:55–61.
Møller Christensen L, Kørup K, Trolle E, Matthiessen J, Fagt S. Børn og unges måltidsvaner 2005–2008. Afdelingen for Ernæring: DTU Fødevareinstituttet; 2012.
Bonnesen CT, Toftager M, Madsen KR, Wehner SK, Jensen MP, Rosing JA, et al. Study protocol of the healthy high school study: a school-based intervention to improve well-being among high school students in Denmark. BMC Public Health. 2020;20(1):95.
Bartholomew LK, editor. Planning health promotion programs: an intervention mapping approach. 3rd ed. San Francisco, CA: Jossey-Bass; 2011. 745 p.
DTU Fødevaresinstituttet. Tjek på buffetens sundhed - DTU Fødevareinstituttet [Internet]. https://www.food.dtu.dk. 2012 [cited 2020 Feb 5]. Available from: https://www.food.dtu.dk/nyheder/Nyhed?id={2D0DE6EF-FDAD-40EA-A2B9-96DA0F2EEB8E}.
Børne- og Undervisningsministeriet. Gymnasiale uddannelser [Internet]. 2020 [cited 2020 Dec 14]. Available from: https://www.uvm.dk/gymnasiale-uddannelser
Børne- og Undervisningsministeriet. Fortsat stor søgning mod gymnasiet [Internet]. 2017 [cited 2020 Dec 14]. Available from: https://www.uvm.dk/global/news/uvm/udd/gym/2017/marts/170320-fortsat-stor-soegning-mod-gymnasiet
Nordic nutrition recommendations 2012. Place of publication not identified: Nordic Council Of Ministe; 2014.
de Boer MR, Waterlander WE, Kuijper LDJ, Steenhuis IHM, Twisk JWR. Testing for baseline differences in randomized controlled trials: an unhealthy research behavior that is hard to eradicate. Int J Behav Nutr Phys Act. 2015 Jan 24;12:4.
Christensen U, Krølner R, Nilsson CJ, Lyngbye PW, Hougaard CØ, Nygaard E, et al. Addressing social inequality in aging by the Danish occupational social class measurement. J Aging Health. 2014;26(1):106–27.
Graham JW, Cumsille PE, Shevock AE. Methods for Handling Missing Data. In: Handbook of Psychology, Second Edition [Internet]. American Cancer Society; 2012 [cited 2021 Jan 11]. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/9781118133880.hop202004
Bonnesen CT, Jensen MP, Madsen KR, Toftager M, Rosing JA, Krølner RF. Implementation of initiatives to prevent student stress: process evaluation findings from the healthy high school study. Health Educ Res. 2020;35(3):195–215.
Duus KS, Madsen KR, Krølner RF. Sundere kantiner på gymnasier [Internet]. Denmark: Statens Institut for Folkesundhed, Syddansk Universitet; 2019. Available from: https://www.sdu.dk/sif/-/media/images/sif/cfi/publikationer_filer/kantinerapport_sundere_kantiner_paa_gymnasier.pdf
van Kleef E, Kremer F, van Trijp HCM. The impact of a gradual healthier assortment among vocational schools participating in a school canteen Programme: evidence from sales and student survey data. Int J Environ Res Public Health. 2020;17:17(12).
Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation research: A Synthesis of the Literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network (FMHI Publication #231); 2005.
Bast LS, Due P, Bendtsen P, Ringgard L, Wohllebe L, Damsgaard MT, et al. High impact of implementation on school-based smoking prevention: the X:IT study-a cluster-randomized smoking prevention trial. Implement Sci. 2016 17;11(1):125.
Aarestrup AK, Krølner R, Jørgensen TS, Evans A, Due P, Tjørnhøj-Thomsen T. Implementing a free school-based fruit and vegetable programme: barriers and facilitators experienced by pupils, teachers and produce suppliers in the boost study. BMC Public Health. 2014;14(1):146.
Moore GF, Evans RE, Hawkins J, Littlecott H, Melendez-Torres GJ, Bonell C, et al. From complex social interventions to interventions in complex social systems: future directions and unresolved questions for intervention development and evaluation. Evaluation. 2019;25(1):23–45.
Christensen CB, Mikkelsen BE, Toft U. The effect of introducing a free breakfast club on eating habits among students at vocational schools. BMC Public Health [Internet]. 2019 3 [cited 2020 Aug 21];19. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6446271/
Larson N, Wang Q, Grannon K, Wei S, Nanney MS, Caspi C. A Low-Cost, Grab-and-Go Breakfast Intervention for Rural High School Students: Changes in School Breakfast Program Participation Among At-Risk Students in Minnesota. Journal of Nutrition Education and Behavior. 2018 Feb 1;50(2):125–132.e1.
Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr. 2009 Feb;12(2):267–83.
Roberto CA, Swinburn B, Hawkes C, Huang TT-K, Costa SA, Ashe M, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385(9985):2400–9.
Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ [Internet]. 2014 27 [cited 2021 Jan 28];348. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4035503/
Lloyd J, Creanor S, Logan S, Green C, Dean SG, Hillsdon M, et al. Effectiveness of the healthy lifestyles Programme (HeLP) to prevent obesity in UK primary-school children: a cluster randomised controlled trial. Lancet Child Adolesc Health. 2018 Jan;2(1):35–45.
Hanks AS, Just DR, Smith LE, Wansink B. Healthy convenience: nudging students toward healthier choices in the lunchroom. J Public Health (Oxf). 2012 Aug;34(3):370–6.
Ensaff H, Homer M, Sahota P, Braybrook D, Coan S, McLeod H. Food choice architecture: an intervention in a secondary school and its impact on students’ plant-based food choices. Nutrients. 2015 Jun 2;7(6):4426–37.
Metcalfe JJ, Ellison B, Hamdi N, Richardson R, Prescott MP. A systematic review of school meal nudge interventions to improve youth food behaviors. Int J Behav Nutr Phys Act. 2020 Dec;17(1):77.
Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. First ed. London: Silverback Publishing; 2014. 329 p.
Lloyd JJ, Logan S, Greaves CJ, Wyatt KM. Evidence, theory and context - using intervention mapping to develop a school-based intervention to prevent obesity in children. Int J Behav Nutr Phys Act. 2011 Jul 13;8(1):73.
Axford N, Berry V, Lloyd J, Hobbs T, Wyatt K. Promoting learning from null or negative results in prevention science trials. Prev Sci. 2020 Aug;4:1–13.
McHugh C, Hurst A, Bethel A, Lloyd J, Logan S, Wyatt K. The impact of the World Health Organization health promoting schools framework approach on diet and physical activity behaviours of adolescents in secondary schools: a systematic review. Public Health. 2020 May 1;182:116–24.
Flodgren GM, Helleve A, Lobstein T, Rutter H, Klepp K. Primary prevention of overweight and obesity in adolescents: An overview of systematic reviews. Obesity Reviews [Internet]. 2020 Nov [cited 2021 Jan 29];21(11). Available from: https://onlinelibrary.wiley.com/doi/10.1111/obr.13102
Lundborg P, Rooth D-O, Alex-Petersen J. Long-Term eEffects of Childhood Nutrition: Evidence from a School Lunch Reform. The Review of Economic Studies [Internet]. 2021 May 11 [cited 2021 Jul 22];(rdab028). Available from: https://doi.org/10.1093/restud/rdab028.
Acknowledgements
We would like to thank all the schools that participated in the HHS study and took the time to implement the initiatives, especially the canteen staff who played a significant part for this specific study. Furthermore, we would like to thank all the students who took the time to answer the questionnaires and the rest of the HHS project group as well as other colleagues and students who have been involved in the HHS study since its beginning in 2014. We acknowledge Mette Rasmussen’s comments to an earlier draft of this manuscript.
Funding
This study was funded by TrygFonden (grant: 30035); Nordea-fonden (02–2015-1364).
The funding bodies have not been involved in the study design, data analysis, nor interpretation of data.
Author information
Authors and Affiliations
Contributions
RFK and CTB secured funding and contributed to the study design. RFK was the principal investigator of the HHS study. RFK, CTB, MT, TPP, and KRM contributed to intervention design. KSD, RFK, CTB, MT, KRM, and JAR contributed to intervention delivery and data collection. JAR and CTB performed data cleaning and imputation. KSD performed all data analyses. LCT supervised data imputation and all analyses and contributed to data visualization. KSD, CTB, JAR, RFK and LCT contributed to data interpretation. KSD drafted the manuscript. All authors contributed to the revision of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study adheres to all Danish ethical standards and has been approved by the Danish Data Protection Agency (ref: 10.703). The Regional Scientific Ethical Committee, the Capital Region of Denmark, reviewed the study and concluded that formal ethical approval was not required (J. No. 16018722). Written information was sent to principals, teachers and student councils at all invited high schools explaining the implications of participating in the study. For all data collection methods, respondents were informed about the aim of the study, that participation was voluntary, that their information would be used for research purpose only and treated with confidence. By participating they gave consent that their data could be used for research.
Consent for publication
N/A
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Duus, K.S., Bonnesen, C.T., Rosing, J.A. et al. Effect of the multicomponent healthy high school intervention on meal frequency and eating habits among high school students in Denmark: a cluster randomized controlled trial. Int J Behav Nutr Phys Act 19, 12 (2022). https://doi.org/10.1186/s12966-021-01228-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-021-01228-2