Abstract
O-linked N-acetylglucosamine protein modification (O-GlcNAcylation) is a dynamic post-translational modification (PTM) involving the covalent binding of serine and/or threonine residues, which regulates bone cell homeostasis. Reactive oxygen species (ROS) are increased due to oxidative stress in various pathological contexts related to bone remodeling, such as osteoporosis, arthritis, and bone fracture. Autophagy serves as a scavenger for ROS within bone marrow-derived mesenchymal stem cells, osteoclasts, and osteoblasts. However, oxidative stress-induced autophagy is affected by the metabolic status, leading to unfavorable clinical outcomes. O-GlcNAcylation can regulate the autophagy process both directly and indirectly through oxidative stress-related signaling pathways, ultimately improving bone remodeling. The present interventions for the bone remodeling process often focus on promoting osteogenesis or inhibiting osteoclast absorption, ignoring the effect of PTM on the overall process of bone remodeling. This review explores how O-GlcNAcylation synergizes with autophagy to exert multiple regulatory effects on bone remodeling under oxidative stress stimulation, indicating the application of O-GlcNAcylation as a new molecular target in the field of bone remodeling.
Graphical Abstract

Similar content being viewed by others
Background
Oxidative stress results from an imbalance in cellular physiology between reactive oxygen species (ROS) and antioxidant signaling, wherein ROS production surpasses the capacity of the ROS defense system [1]. The mitochondrial respiratory chain is the primary endogenous source of ROS, and intracellular ROS is maintained at a consistently low level under normal physiological conditions [2]. This balance is not only involved in intracellular signaling regulation but also sustains bone metabolism [3].
Bones exhibit dynamic characteristics throughout life, including the resorption of aging or compromised bone tissue and the subsequent deposition of new bone material. These ongoing alterations are termed bone remodeling and are vital for maintaining the structural integrity of the skeletal system [4]. However, besides physiological ROS generation, pathophysiological factors such as hyperglycemia [5], medication-related osteonecrosis of the jaw (MRONJ) [6], and osteoporosis [7] can elevate ROS levels in bone tissues and disrupt the remodeling process.
The degradation and maintenance of intracellular proteins and organelles depend on the intricate autophagy process [8]. Cells sequester misfolded proteins or damaged organelles into lysosomes for degradation, thereby sustaining cell homeostasis during starvation, hypoxia, infection, and other stress [9, 10]. Autophagy dysfunction is correlated with various diseases, and its association with bone diseases has been extensively studied, especially in the metabolism of bone marrow-derived mesenchymal stem cells (BMSCs), osteoblasts, and osteoclasts [11].
O-linked N-acetylglucosamine protein modification (O-GlcNAcylation) is a monosaccharide post-translational modification (PTM), which is implicated in several physiological functions, such as metabolism, signaling, transcription, and translation [12]. As a crucial sensor of oxidative stress, many proteins involved in the autophagic process have been identified as targets for O-GlcNAcylation [13]. Only two conserved enzymes, O-GlcNAc transferase (OGT) and O-GlcNAcase (OGA), are involved in O-GlcNAcylation. OGT facilitates the attachment of O-GlcNAc to the hydroxy group of serine and threonine residues, whereas OGA hydrolytically cleaves O-GlcNAc from modified proteins [12].
The depletion of OGT in BMSCs was shown to compromise bone formation in mice, and osteoclast-specific OGT knockout increased bone mineral density, which established the essential role of O-GlcNAcylation in bone remodeling [14, 15]. Presently, most research on O-GlcNAcylation-mediated bone remodeling has concentrated on metabolic pathways encompassing glucose and glutamine uptake and utilization, with the precise phase and principal cellular localization of O-GlcNAcylation governing bone remodeling yet to be elucidated. Recent investigations introduced a novel perspective, indicating that OGT inhibition disrupts mitochondrial function, culminating in oxidative stress and autophagy [16]. Thus, as a crucial nexus linking signal transduction and metabolism, O-GlcNAcylation orchestrates oxidative stress and autophagy [17].
The objective of this review was to explore the potential mechanism by which O-GlcNAcylation mitigates oxidative stress in bone remodeling and the associated bone pathologies through autophagy. Additionally, novel strategies for improving bone remodeling in various diseases via O-GlcNAcylation are also provided.
Interplay between O-GlcNAcylation and oxidative stress
Several pathological factors, including hyperglycemia and alterations in hormone levels, can induce oxidative stress, which is an autonomous risk factor for bone diseases. However, O-GlcNAcylation intricately connects cellular metabolic status with oxidative stress via the hexosamine biosynthetic pathway (HBP), thereby regulating bone remodeling.
O-GlcNAcylation: a sensor of metabolic status
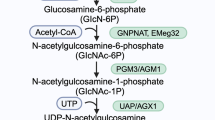
Unlike traditional glycosylation, O-GlcNAcylation adds an O-GlcNAc moiety to nucleocytoplasmic and mitochondrial compartments, maintaining it as a monosaccharide rather than further developing into a polysaccharide [18]. About 2–5% of total cellular glucose is funneled through the HBP, which is a glycolysis shunt that is activated by enhanced glucose absorption [19]. The HBP produces uridine-5′-diphosphate-N-acetylglucosamine (UDP-GlcNAc), the donor substrate for OGT [20] (Fig. 1). O-GlcNAcylation also interacts with other PTMs like phosphorylation and ubiquitination to affect signal transduction in stressful environments, which further influences disease outcomes and prognoses [21,22,23]. Therefore, O-GlcNAcylation serves as a nutrition sensor, tying the metabolic state to the control of several signaling cascades [24]. The absence of either OGT or OGA in mice resulted in embryonic and perinatal lethality, underscoring their crucial roles in survival and development [25].
The hexosamine biosynthetic pathway and O-GlcNAcylation. Approximately 2% to 5% of glucose is directed toward the HBP during glycolysis. The pivotal stage in the HBP, governed by the enzyme GFAT, involves the conversion of fructose-6-phosphate to glucosamine-6-phosphate through glutamine and the involvement of enzymes, subsequently yielding UDP-GlcNAc. As a substrate for OGT, UDP-GlcNAc actively engages in the O-GlcNAcylation of cytoplasmic or nuclear proteins. O-GlcNAcylation equilibrium is maintained by OGT and OGA. Abbreviations: HK, hexokinase; GPI, glucose phosphate isomerase; Gluc-6P, glucosamine-6-phosphate; Fruc-6P, fructose-6-phosphate; GlcN-6P: glucosamine-6-phosphate; GlcNAc-6P: N-acetylglucosamine-6-phosphate; GlcNAc-1P, N-acetylglucosamine-1-phosphate; GAFT, glutamine-fructose-6-phosphatase aminotransferase; EMeg32, glucosamine-6-phosphate acetyl-transferase; AGM1, phosphoacetylglucosamine mutase
Oxidative stress and bone remodeling
The equilibrium of the bone remodeling processes is crucially influenced by oxidative stress [26]. Aged mice exhibited up-regulated oxidative stress genes and down-regulated osteoblast-related genes compared to young mice, potentially contributing to age-related osteoporosis [27]. Additionally, excessive ROS produced by oxidative stress promotes osteoclast differentiation. Antioxidant drugs have demonstrated their efficacy in treating osteoporosis by enhancing osteoblast and bone development while inhibiting osteoclast and bone resorption [28]. In contrast, reducing nuclear factor erythroid 2‐related factor 2 (Nrf2)-responsive antioxidants were shown to increase receptor activator of NF-κB ligand (RANKL)-induced intracellular ROS levels, contributing to osteoclast differentiation [29].
O-GlcNAcylation and oxidative stress
The interplay of O-GlcNAcylation and protein oxidation is essential in regulating cellular damage [30, 31]. O-GlcNAcylation levels can respond to oxidative damage through signal transduction and metabolism [32]. For instance, oxidative stress increases the O-GlcNAcylation of nucleoplasmic proteins, whereas suppressing O-GlcNAcylation increases cellular vulnerability to stress, resulting in reduced cell viability and bone formation [33, 34]. Previous studies showed that this may be related to the increased activity of signal transducer and activator of transcription(STAT3) and forkhead box transcription factor O1 (FoxO1) mediated by OGT [35].
O-GlcNAcylation can also change intracellular ROS levels and influence bone remodeling. Glucose-6-phosphate dehydrogenase (G6PDH) was reported to be activated by hyper O-GlcNAcylation, thereby up-regulating NADPH/NADP+ and GSH/GSSG couples to relieve oxidative stress [36]. A high GSH/GSSG ratio also significantly increased the mRNA expression levels of markers associated with osteogenic differentiation and mineralization [37]. Similarly, the nuclear factor of activated T cells (NFAT) family and NF-κB activities were suppressed by elevated O-GlcNAcylation, which inhibited RANKL-induced osteoclast differentiation [38, 39].
Although some oxidative stress-related O-GlcNAcylation substrates have been identified, more work is needed to determine the complete O-GlcNAcylated site that transduces these signals in mitochondrial network homeostasis [40]. A thorough comprehension of how O-GlcNAcylation contributes to signal transduction under oxidative stress conditions could reveal novel avenues for therapeutic interventions in bone remodeling.
O-GlcNAcylation: a sweet regulator of autophagy
Autophagy functions as a cellular self-defense mechanism that shields cells from metabolic stress and oxidative damage. Recent studies showed that O-GlcNAcylation exerted varied effects on proteins engaged in distinct phases of autophagy, which affected the overall process of bone remodeling by regulating autophagy in BMSCs, osteoclasts, and osteoblasts [13, 41].
Autophagy and bone remodeling
A previous study proposed a dual association between autophagy and BMSCs, whereby the regulation of autophagy affects the function of BMSCs, and BMSCs may also modulate the autophagy of immune cells, ultimately influencing the therapeutic properties of BMSCs [42]. For example, macrophages with low-inflammatory characteristics can induce autophagy in BMSCs, thereby enhancing osteogenesis [43]. Anti-inflammatory macrophages frequently exhibit increased levels of O-GlcNAcylation and OGT. Further investigations are needed to ascertain its potential correlation with autophagy [44]. Additionally, increased mitochondrial respiration with ATP production is vital for BMSCs or pre-osteoblast differentiation and leads to further increases in endogenous ROS [45]. However, as a critical form of selective autophagy, OGT-regulated mitophagy selectively removes dysfunctional or redundant mitochondria to ensure mitochondrial quality, which is essential for preventing BMSCs senescence [46,47,48].
Compared to cytoprotection in osteoblasts, autophagy actively promotes osteoclast differentiation. A recent study demonstrated that metformin mitigated bone loss by inhibiting osteoclast differentiation, a consequence of dysregulated autophagy in osteoclast precursors [49]. This phenomenon may be attributed to the capacity of metformin to reduce the O-GlcNAcylation of AMP-activated protein kinase (AMPK), thus enhancing cell cycle arrest [50]. Additionally, the ablation of autophagy in osteoblasts promoted bone resorption by triggering the release of RANKL [51]. These studies underscore the role of autophagy as a target of O-GlcNAcylation during bone remodeling.
Autophagy mechanisms
The development of the isolation membrane, formerly known as the phagophore, marks the initiation of autophagy. The extension of this membrane is further facilitated by autophagy-related (ATG) genes and proteins, culminating in the formation of autophagosomes. Subsequently, the autophagosome merges with the endosomal lysosomal apparatus, which converts it to an autolysosome to degrade isolated cytoplasmic materials [52]. The entire autophagy process primarily encompasses the formation of autophagosomes (initiation, nucleation, and phagophore expansion) and autolysosomes [53] (Fig. 2). The molecular regulation of autophagy is as follows:
-
i)
Initiation: FAK family kinase-interacting protein of 200 kDa (FIP200), ATG13, ATG101, and ULK1/2 make up the UNC51-like kinase (ULK) complex [54]. ULK1 and ULK2 phosphorylate FIP200 and ATG13 to initiate the phagophore production process [55].
-
ii)
Nucleation: A class III PI3K complex made up of Beclin1, ATG14, vacuolar protein-sorting 15 (VPS15), and VPS34 is the target of the activated ULK complex. Phosphatidylinositol 3-phosphate (PI3P), which VPS34 generates on phagophore membranes, facilitates the recruitment of additional autophagic machinery protein complexes [56]. Recent findings indicated that ATG14 also enhanced autophagosome fusion with the endolysosomal compartment [57].
-
iii)
Expansion: The lipidation of microtubule-associated protein 1 light chain 3 (MAP1LC3; also known as LC3) with phosphatidylethanolamine is the result of the recruitment of ATG5-ATG12-ATG16 complex to the autophagosome membrane [8]. LC3 is required for expansion, and ATG4B is essential for LC3 lipidation and processing [58].
-
iv)
Formation of autolysosomes: RAB GTPases, tethering proteins, and soluble N-ethylmaleimide-sensitive factor attachment protein receptors (SNAREs) work in concert to facilitate the merging of autophagosomes with late endosomes/lysosomes. Several SNARE proteins primarily mediate this process: STX17 and SNAP29 on autophagosomes and VAMP8 on late endosomes/lysosomes or YKT6 and SNAP29 on autophagosomes and STX7 on late endosomes/lysosomes. Recent studies also identified multiple tethered proteins facilitating the fusion process, including the HOPS complex, EPG5, and PLEKHM1 [59].
Brief representation of the autophagy process. The process of autophagy comprises initiation, nucleation, phagophore expansion and autolysosome fusion. Each process is regulated by many autophagy-related proteins and genes, such as the ULK1 complex, PI3K complex, LC3, and the SNARE complex, which are targets of O-GlcNAcylation
Besides the essential ATG proteins, specific adaptors for autophagy, such as SQSTM1 (p62), NBR1, and NDP52, play crucial roles in selectively recruiting aberrant proteins to autophagosomes and promoting their subsequent fusion with lysosomes for degradation [60].
Regulation of O-GlcNAcylation on autophagy
O-GlcNAcylation can promote the formation of autophagosomes while inhibiting autolysosome formation. Thus, identifying effective targets for alleviating oxidative stress by promoting autophagy is predicted to facilitate bone remodeling. The consequences of O-GlcNAcylation on bone remodeling through autophagy under different O-GlcNAcylation-related stimuli and the possible mechanisms are summarized in Table 1.
Regulation of O-GlcNAcylation in autophagosome formation
The necessity of O-GlcNAcylation for autophagy has been demonstrated using an OGT knockout mouse model, which found that the absence of OGT reduced autophagy levels [72]. Further investigation revealed that ULK1 underwent O-GlcNAcylation at the threonine 754 site under glucose shortage conditions, which was essential for activating lipid kinase VPS34 and producing of PI3P [61]. The AMPK-ULK1-autophagy axis has been shown to promote osteoblast differentiation and bone regeneration, suggesting the potential therapeutic effect of O-GlcNAcylation on bone remodeling [62]. Beclin-1, an essential contributor to both autophagy and osteoclast formation, is O-GlcNAcylated, thereby inhibiting autophagy. This process leads to defects in chondrocyte differentiation and osteoclast dysfunction [66, 67]. Additionally, the O-GlcNAcylation of ATG4B was shown to up-regulate its proteolytic activity to promote autophagy, whereas the O-GlcNAcylation ATG5 suppressed autophagy [65, 70]. Whether O-GlcNAcylation can amplify the maturation of osteoclasts caused by the activation of ATG4-LC3 deserves further study [64].
Regulation of O-GlcNAcylation in autolysosome formation
O-GlcNAcylation appears to have an inhibitory effect in the fusion stage of autophagosomes and lysosomes, contrary to its role in the initial stage [73]. A decrease in the OGT-induced O-GlcNAcylation of SNAP-29 caused the SNARE complex to assemble more readily, which enhanced cisplatin-induced autophagy [68]. In contrast, augmenting SNAP29 O-GlcNAcylation inhibited the formation of the SNARE fusion complex, leading to increased ROS generation and subsequent apoptosis [69]. The increase in ROS not only promoted the differentiation of osteoclasts but also hampered the assembly of the SNARE complex due to SNAP O-GlcNAcylation, which, in turn, inhibited the production of bone matrix mediated by osteoblasts [74].
O-GlcNAcylation: at the crossroads of oxidative stress and autophagy
Although oxidative stress and autophagy have been well-investigated, the impact of O-GlcNAcylation on both processes varies in different bone remodeling conditions, possibly due to the collective influence of O-GlcNAcylation across diverse signal transduction pathways. Consequently, we have consolidated the insight into autophagy-related oxidative stress signaling pathways, such as ROS/AMPK/mTOR, ROS/Keap1/Nrf2, ROS/FoxOs, and ROS/NF-κB, hoping to elucidate the effects of O-GlcNAcylation on bone remodeling under oxidative stress.
AMPK/mTOR
AMPK/mTOR signaling in oxidative stress
AMPK consists of regulatory β- and γ-subunits and catalytic α-subunits, and is activated by intracellular ATP synthesis and elevated ROS levels [75, 76]. The mammalian target of rapamycin (mTOR) serves as the catalytic subunit within two separate entities identified as mTORC1 and mTORC2 [77]. mTORC1 acts as a major regulator of protein synthesis by regulating eukaryotic initiation factor binding protein 1 (4E-BP1) and p70 ribosomal protein S6 kinase 1(S6K1). Additionally, mTORC1 can suppress autophagy by regulating the ULK1 complex. mTORC2 also functions as a crucial upstream regulator that initiates the PI3K-AKT pathway [78] (Fig. 3).
ROS/AMPK/mTOR signaling pathways and O-GlcNAcylation. ROS influences AMPK activity through direct interactions or indirectly by modifying adenine nucleotide ratios. AMPK, in turn, can either activate ULK1 or inhibit mTORC1, promoting autophagy as a response to mitigate oxidative stress. The O-GlcNAcylation of Raptor activates the mTORC1 complex, thereby impacting downstream targets such as S6K1 and 4EBP1, both of which are subject to O-GlcNAcylation-mediated regulation
Early studies found that exogenous H2O2 could activate AMPK directly or by reducing the ATP/ADP ratio [79, 80]. Conversely, elevated glucose levels promote ROS generation, which causes the ubiquitination of AMPKα and subsequent degradation [81]. These contrasting impacts imply that the multiple regulatory effects of ROS on AMPK/mTOR signaling are closely related to glucose metabolism. Recent studies found that AMPK activation could inhibit ROS-induced osteoclastogenesis. Thus, the role of O-GlcNAcylation in this process deserves further investigation [82].
ROS/AMPK/mTOR/autophagy signaling
The association between oxidative stress and AMPK/mTOR is frequently mediated by autophagy. ULK1 activation can be achieved through the direct phosphorylation of AMPK or indirectly by inhibiting mTORC1, thus alleviating its suppressive influence on ULK1 [83, 84]. BMSC-derived exosomes were reported to inhibit ROS/NLRP3 inflammasomes through AMPK/mTOR/autophagy signaling [85], and AMPK/mTOR/ULK-1 signaling has been shown to ameliorate rheumatoid arthritis [86]. Thus, the ROS/AMPK/mTOR/autophagy signaling pathway has emerged as a promising therapeutic target in bone remodeling [87].
O-GlcNAcylation of ROS/AMPK/mTOR/autophagy signaling
As the key regulator of the mTORC1 complex, AMPK can also be O-GlcNAcylated [88, 89]. Nutrient-sensitive pathways regulate both O-GlcNAcylation and AMPK, linking metabolic homeostasis to the control of various intracellular processes [90]. The activity of AMPK is blocked after O-GlcNAcylation, which then suppresses autophagy and ULK1 activity [91]. Notably, ULK1 can be activated after O-GlcNAcylation and promote bone remodeling. Whether the O-GlcNAcylation of AMPK counteracts this process has not been reported [61, 62]. In the absence of O-GlcNAcylation, AMPK activation can facilitate skeletal muscle to utilize glucose more efficiently [92]. However, the natural antioxidant α-lipoic acid was shown to decrease interactions between AMPK and OGT in diabetic mice, further contributing to cell survival, partly through AMPK activation or OGT inhibition [93]. In summary, increased O-GlcNAcylation significantly decreased autophagy through AMPK/mTOR signaling, indicating the inhibitory impact of AMPK O-GlcNAcylation on bone remodeling.
In addition to the AMPK pathway, direct cross-regulations between mTOR signaling and O-GlcNAcylation have also been reported [94]. mTOR O-GlcNAcylation inhibition increased autophagosome numbers and the levels of the autophagic markers SQSTM1/p62 and LC3-II [95]. The treatment of HepG2 cells with mTOR inhibitors to induce autophagic flux resulted in an unanticipated reduction in overall O-GlcNAcylation due to decreased OGT and increased OGA [96]. Conversely, increased levels of O-GlcNAcylation were observed after increasing mTOR activation [97]. Recent studies suggested that the regulation of mTORC1 activation by glucose is tightly controlled by the O-GlcNAcylation of Raptor, a crucial constituent of mTORC1. Specifically, O-GlcNAcylation occurs at threonine 700 of Raptor, facilitating its binding with Rag GTPases. This binding facilitates the relocation of mTOR to lysosomal surfaces, initiating mTORC1 activation. Raptor O-GlcNAcylation was suppressed by the AMPK phosphorylation of Raptor, which prevented Raptor from interacting with Rags GTPases [98]. The RhoA protein of GTPases contributes to the differentiation of osteoclasts and ultimately causes osteoporosis, indicating that O-GlcNAcylation can not only inhibit autophagy by activating mTOR in bone remodeling but also promote osteoclast absorption [99].
The downstream mTOR pathway also responds to O-GlcNAcylation [100]. OGT was reported to inhibit the proinflammatory activation of macrophages by catalyzing S6K1 O-GlcNAcylation and, hence, inhibit mTORC1 signaling [100], suggesting that a comparable mechanism may weaken bone absorption caused by osteoclasts in oxidative stress.
In general, AMPK negatively regulates the mTOR pathway to promote autophagy and alleviate oxidative stress, while the O-GlcNAcylation of AMPK reduces its activity. O-GlcNAcylation not only directly regulates mTORC1 but also influences the downstream mTOR pathway. The regulation of O-GlcNAcylation in the ROS/AMPK/mTOR/autophagy pathway integrates nutritional signals to respond to oxidative stress, which further promotes bone remodeling.
Keap1/Nrf2
Keap1/Nrf2 signaling in oxidative stress
Nrf2 is an antioxidative transcription factor, safeguarding cells from oxidative stress by controlling antioxidant response elements (ARE) [101] (Fig. 4). Kelch‐like ECH‐associated protein 1 (Keap1) develops a ubiquitin E3 ligase complex with CULLIN3 (CUL3) under quiescent conditions, which results in the ubiquitination and degradation of Nrf2 [102]. However, ubiquitin E3 ligase activity is decreased when Keap1 is subjected to oxidative stress, which ultimately facilitates the subsequent translocation of Nrf2 to the nucleus, initiating the antioxidant response [103]. Recent findings indicated that osteocyte Nrf2 activity promoted the expression of the osteocytic gene and was necessary for bone homeostasis [104]. An Nrf2 activator was shown to inhibit osteoclast formation and bone resorption in vivo by interfering with NF-κB signaling transduction [105]. Conversely, osteoclast differentiation was enhanced after attenuating the Nrf2-mediated antioxidant response [29].
p62-Keap1-Nrf2 feedback loop and O-GlcNAcylation. O-GlcNAcylation is necessary for Nrf2 degradation by Keap1-CUL3 ubiquitin E3 ligase. Keap1-CUL3 ubiquitin E3 ligase functionality decreases when exposed to oxidative stress, resulting in the translocation of Nrf2 into the nucleus and initiating a cascade of antioxidant gene activation. At the same time, activated p62 can promote the generation of Nrf2 through autophagy to form a positive cycle
ROS/Keap1/Nrf2/autophagy signaling
P62 is a selective autophagy receptor protein that bridges between autophagy and the Keap1-Nrf2 system [106,107,108]. The pivotal function of p62 involves delivering diverse ubiquitination cargo to the autophagosome, culminating in its degradation by lysosomes, which is further stimulated by oxidative stress [108, 109]. p62 can form a complex with Keap1 (p62-Keap1 complex) that undergoes elimination via the ubiquitin–proteasome system or induces the degradation of Keap1 via selective autophagy [107, 110]. Additionally, Nrf2 induces the expression of p62 and Sestrin2 in a reciprocating manner, which establishes a positive feedback loop between p62 and Keap1-Nrf2 that amplifies protective effects on cells [110, 111]. Simultaneously, Sestrin2 activates autophagy by inhibiting mTORC1 expression [112]. Recent studies showed that phosphorylating p62 at Ser349 and Thr269/Ser272 protected bones from destruction, ameliorating arthritis by activating the p62-Keap1-Nrf2 feedback loop [113]. Thus, preserving bone homeostasis depends on the balance of a positive feedback loop that includes p62, Keap1, and Nrf2.
O-GlcNAcylation of ROS/Keap1/Nrf2/autophagy signaling
O‐GlcNAcylation is necessary for the efficient ubiquitination of Nrf2 since O‐GlcNAcylation of Keap1 at serine 104 was shown to enhance its productive interaction with CUL3 [114]. Increasing Keap1 O-GlcNAcylation led to the ubiquitination and degradation of Nrf2 while simultaneously inhibiting autophagy [115]. In contrast, ovarian cancer cells with low‐OGT activity tended to have strong Nrf2 activation signatures [116]. A previous study showed that Nrf2 activation could inhibit oxidative stress in ovariectomized rats, preventing osteoporosis and promoting osteogenesis [117]. O-GlcNAcylation inhibits bone remodeling in Keap1-Nrf2 signal transduction, which involves inhibiting the antioxidant effect of Nrf2 and further blocking the amplification of autophagy by the p62-Keap1-Nrf2 feedback loop [118]. Conversely, as a member of the same Nrf2 family, OGT improves the stability of the Nrf1a protein [119]. In addition, CUL3 can down-regulate OGT expression, which depends on binding to the OGT promoter region [120].
As recently as 30 years ago, studies found that p62 activity was sensitive to glucose metabolism and was modified by O-GlcNAc after translation [121, 122]. Although the p62 site of O-GlcNAcylation has been identified, its downstream effects remain unknown [123]. The protective role of the p62/Keap1/Nrf2 feedback loop in bone destruction has been proven, suggesting that the O-GlcNAcylation of p62 is a potential therapeutic target in bone remodeling [113].
The p62-Keap1-Nrf2 positive feedback loop connects Nrf2 to autophagy, alleviating ROS exposure and promoting bone remodeling. O-GlcNAcylation acts as a terminator and destroys the positive effects on bone remodeling. Consequently, it is essential to manage interactions between the Keap1-Nrf2 pathway, autophagy, and O-GlcNAcylation for effective bone remodeling.
FoxOs
FoxOs in oxidative stress
FoxO transcription factors, namely FoxO1, FoxO3, FoxO4, and FoxO6, regulate antioxidant responses in glucose metabolism [124, 125]. Runx2 and PPARγ are the main transcription factors for osteogenesis and adipogenesis, respectively, and are controlled by Wnt/β-catenin through binding to T cell factor (TCF). Wnt/β-catenin significantly contributes to the osteogenic differentiation of BMSCs under normal circumstances [126]. However, as modulators of the cellular stress response, FoxOs are stimulated by ROS to interact with β-catenin, thereby jointly activating the transcription of target genes related to the antioxidant response [127]. In contrast, FoxO activity is influenced by ROS and is associated with post-translational changes, such as phosphorylation and O-GlcNAcylation [128,129,130] (Fig. 5).
O-GlcNAcylation response to FoxO and autophagy in oxidative stress. Upon exposure to ROS, β-catenin engages with FoxO, triggering the activation of antioxidant genes and the induction of autophagy to mitigate oxidative stress. Prolonged ROS exposure disrupts the interaction between TCF and β-catenin, promoting apoptosis and decreasing osteogenic differentiation. O-GlcNAcylation emerges as a mechanism capable of enhancing β-catenin expression, counteracting the detrimental consequences of persistent ROS stimulation. However, both OGT and FoxO genes are implicated in the onset of diabetes and cancer
Considering the bidirectional regulation between FoxOs and ROS, FoxOs assume a dual role in bone remodeling under oxidative stress. The impaired functionality of FoxOs in bone cells contributes to osteoarthritis, osteoporosis, and other bone diseases, with FoxO1 and FoxO3 being extensively expressed and studied [131]. The overexpression of FoxO3 in osteoclasts augments bone mass by stimulating catalase to inhibit ROS and bone resorption [132, 133]. FoxO1 promotes the differentiation of BMSCs into osteoblasts by suppressing the transcription and expression of PPARG/PPARγ, which adversely regulates adipogenesis [134]. However, prolonged ROS exposure was shown to facilitate the redirection of β-catenin from TCF to FoxO transcription, consequently hindering the Wnt/β-catenin signaling pathway and diminishing osteogenic functionality [133]. Recent studies found that the down-regulation of FoxO1 expression could prevent BMSC apoptosis in acute inflammation [135], and the absence of FoxO1 was reported to indirectly enhance bone remodeling and mitigate age-related bone resorption by improving the binding of β-catenin and TCF [136]. Notably, the sustained activation of FoxOs increased PPARγ levels, forming complexes with β‐catenin and inducing β‐catenin degradation. Thus, the repressive action of prolong ROS can cause age-related decreases in bone mineral density during bone remodeling [131].
ROS/FoxOs/autophagy signaling
FoxO transcription factors, especially FoxO3 and FoxO1, can also mediate autophagy activity to regulate bone remodeling under oxidative stress [41]. An increase in ROS was reported to activate FoxO3 phosphorylation at Ser294 and contribute to its nuclear translocation, ultimately mitigating ROS levels by up-regulating autophagy [137]. Similar protective effects were observed in osteoarthritis-induced meniscus injury alleviation [138]. However, the FoxO3-mediated transcriptional activation of autophagy-related genes, such as LC3, BNIP3, Beclin-1, ATG4, and ATG12, was inhibited after Akt down-regulated FoxO3 expression in starvation [139]. Additionally, early-onset osteoarthritis was observed in FoxO1 or FoxO3-deficient mice, whereas FoxO1 shielded chondrocytes from oxidative stress and promoted the overexpression of genes related to autophagy and proteoglycan 4, a crucial joint lubricant [140].
O-GlcNAcylation of ROS/FoxOs/autophagy signaling
Given the crucial involvement of FoxOs in glucose metabolism, it is reasonable to contemplate their interaction with O-GlcNAcylation [141, 142]. Since 1991, studies have hinted that elevated O-GlcNAcylation levels might stimulate insulin resistance [143, 144]. The increased O-GlcNAcylation of FoxO1 was observed in diabetes, resulting in the activation of FoxO1 and regulating antioxidative stress in response to glucose metabolism [145]. Recent findings that identified OGT-FoxO1/3 gene fusion in multiple tumors suggest that the O-GlcNAc/FoxOs axis may be the basis for these observations [146, 147]. Another study observed the nuclear translocation of FoxO1 and increased autophagy flux in a hyperglycemic environment [148]. However, FoxO1, FoxO3, and FoxO4 knockout reduced the number of osteoclasts and improved bone remodeling in diabetes-induced osteoporosis [149].
Although these findings suggest that O-GlcNAcylation plays a positive role in antioxidation and autophagy in bone remodeling through FoxOs, their comprehensive mechanisms have not been fully explained. With the emergence of new research methods, the complex role of O-GlcNAcylation and β-catenin has been further revealed in recent years. By employing dual-specificity aptamers targeting OGT/β-catenin, O-GlcNAcylation was found to stabilize β-catenin [150]. O-GlcNAc elevation not only amplified β-catenin protein levels but also augmented its nuclear accumulation, which, in turn, increased O-GlcNAc expression levels [151]. However, the depletion of OGT decreased Wnt/β-catenin signaling activity during embryonic neurogenesis [152]. This phenomenon may be attributed to the direct competition between O-GlcNAcylation and phosphorylation at threonine 41 of β-catenin [153]. In addition, the Wnt/β-catenin signaling pathway can regulate glycolysis to promote the osteogenic differentiation of BMSCs and improve alveolar bone repair [154]. In summary, the current research indicates that O-GlcNAcylation plays a coordinating role in the FoxO signaling pathway. Under short-term ROS stimulation, O-GlcNAcylation promotes bone remodeling through FoxO-mediated antioxidation and autophagy, while under long-term ROS stimulation, it may counteract the adverse effects on bone remodeling by stabilizing β-catenin.
NF-κB
NF-κB in oxidative stress
RelA (also called p65), c-Rel, RelB, NF-κB1 (which consists of p50 and its predecessor p105), and NF-κB2 (which consists of p52 and its precursor p100) are members of the NF-κB transcription factor family [155]. In many studies, NF-κB is commonly referred to as the p65/p50 heterodimer in the canonical NF-κB pathway, while RelB/p52 heterodimers are known to activate noncanonical signaling [156]. Notably, the RANKL-RANK-osteoprotegerin(OPG) system significantly influences bone remodeling. RANKL facilitates osteoclast differentiation, whereas OPG prevents osteoclast differentiation by inhibiting RANKL from binding to RANK [157]. IκBs, which are NF-κB inhibitory proteins, sequester p65/p50 heterodimeric complexes in the cytoplasm of unstimulated cells [155, 158]. The IKK complex (IKKα, IKKβ, and IKKγ) phosphorylates IκBs in response to RANKL stimulation, which causes the degradation of IκBs. As a result, the released NF-κB p65/p50 dimers undergo phosphorylation, facilitating nuclear translocation where they orchestrate the transcriptional regulation of downstream target genes crucial for osteoclast differentiation [159] (Fig. 6).
The involvement of O-GlcNAcylation and NF-κB in autophagy and oxidative stress in bone remodeling. ROS induces the degeneration of Iκb, enhancing the nuclear translocation of NF-κB p65/p50, consequently promoting osteoclast differentiation. Autophagy is regulated by the IKK/NF-κB signaling axis in a context-dependent manner influenced by stimuli and the environment. The O-GlcNAcylation of IKKβ and p65 can facilitate the activation of NF-κB
ROS activates NF-κB signaling and induces pro-inflammatory cytokines and chemokines [160]. Notably, ROS generated from purine nucleotide catabolism prompts the synthesis of RANKL in osteoblasts, fostering osteoclastogenesis, a recognized risk factor for osteoporosis [161]. Therefore, developing drugs that inhibit the NF-κB signaling pathway is of great significance for suppressing osteoclastogenesis and promoting osteogenesis [162]. For example, melatonin was shown to increase cartilage matrix formation and inhibit chondrocyte apoptosis by modulating the NF-κB signaling pathways to repair antioxidant defense system damage [163].
ROS/NF-κB/autophagy signaling
Recent research showed that NF-κB may represent a pivotal therapeutic approach for sensitizing tumor cells to apoptosis through autophagy [164]. Of note, autophagy is also involved in NF-κB signaling during bone remodeling [165, 166]. The NF-κB pathway can directly augment autophagy by promoting the expression of key autophagy-related proteins, including ATG5, LC3, and Beclin1 [167]. These proteins were reported to be highly involved in osteoclast activity [168, 169], and inhibiting the NF-κB pathway reduced autophagy in pre-osteoclasts [170]. Conversely, NF-κΒ has the potential to inhibit autophagocytosis by either up-regulating the expression of autophagy repressors, like the Bcl-2 family and mTOR, or suppressing autophagy promoters, such as ROS, BNIP3, JNK1, and p53 [171,172,173]. In turn, autophagy was found to control the NF-κB pathway, primarily by degrading IKK and NF-κB-inducing kinase components [174].
Notably, p62 is implicated in NF-κB signaling and cytoskeletal reorganization. p62 activates NF-κB signaling under stimulation by interleukin 1, RANKL, and nerve growth factor [175], illustrating the pathophysiological significance of NF-κB signaling in autophagy. Recently, therapeutic strategies for bone remodeling have been designed to stimulate the formation of autophagosomes while inhibiting NF-κB signaling and RANKL-induced osteoclast differentiation based on autophagy and NF-κB signaling [165]. In general, the effect of O-GlcNAcylation on bone remodeling through NF-κB signaling depends on changes in autophagy levels.
O-GlcNAcylation of ROS/NF-κB/autophagy signaling
O-GlcNAcylation interacts with the NF-κB signaling pathway in various cell types to respond to distinct stress environments [176]. Increased levels of O-GlcNAcylation protein in the heart attenuated the activation of the NF-κB signaling pathway, potentially contributing to ameliorating oxidative stress following hemorrhagic shock [177]. Similarly, increased levels of O-GlcNAcylation exerted a suppressive effect on lipopolysaccharide-induced NF-κB activation in lung tissue [178]. A recent study reported an up-regulation of O-GlcNAcylation during osteoclast differentiation. Additionally, decreasing the O-GlcNAcylation of p65 and nuclear factor of activated T cells c1 (NFATc1) was demonstrated to inhibit their nuclear translocation, consequently hindering osteoclast differentiation [179].
The O-GlcNAcylation of IKKβ at S733 was reported to augment NF-κB activation by preventing phosphorylation [176]. Similarly, elevated O-GlcNAcylation of IKKα and p65 enhanced p65 activity and NF-κB transcription [180], whereas OGT gene knockdown produced the opposite results [181]. Further analysis showed that T322 and T352 were O-GlcNAcylation sites on p65, and the process was facilitated by hyperglycemic circumstances [182]. In addition, NF-κB signaling was inactivated by inhibiting O-GlcNAc production in the inflammatory environment, ultimately increasing the level of autophagy to reduce the inflammatory response [183]. Biomaterials that reduce the activation of NF-κB in BMSCs while enhancing autophagy flux have been developed to treat alveolar bone defects caused by diabetes [184]. Although O-GlcNAcylation is closely related to NF-κB signaling, limited studies have elucidated the mechanism in bone tissue. Thus, these investigations could offer novel insight into bone remodeling under oxidative stress.
Concluding remarks and perspectives
Long-term exposure to ROS induced by oxidative stress suppresses the survival and proliferation of BMSCs and osteoblasts while contributing to osteoclast differentiation. It is the main process inhibiting bone remodeling in osteoporosis, MRONJ, and bone fractures. During this mechanism, autophagy is activated by oxidative stress signaling pathways and plays a protective role. Existing research demonstrates that O-GlcNAcylation influences autophagy and the expression of antioxidant genes to mitigate oxidative stress, thereby diminishing bone resorption and contributing to bone remodeling. However, the impact of O-GlcNAcylation on autophagy during oxidative stress varies among individuals and depends on the collective influence of diverse disease states and signal transduction pathways.
The precise O-GlcNAcylation modification sites in autophagy-related oxidative stress signaling pathways involved in bone remodeling regulation need further investigation. Identifying these sites may open avenues for designing targeted peptides and nanocarriers, which can be enhanced using lectins or antibodies to actively target O-GlcNAc. Additionally, exploring whether the HBP pathway can regulate O-GlcNAcylation to mitigate oxidative stress-induced osteoporosis in diabetic patients also warrants further investigation. Despite being in its infancy, accumulating evidence suggests that O-GlcNAcylation is a promising therapeutic target and provides novel ideas for diagnostic biomarkers for bone-related disorders.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- O-GlcNAcylation:
-
O-linked N-acetylglucosamine protein modification
- PTM:
-
Post-translational modification
- ROS:
-
Reactive oxidative species
- BMSCs:
-
Bone marrow-derived mesenchymal stem cells
- MRONJ:
-
Medication-related osteonecrosis of the jaw
- OGT:
-
O-GlcNAc transferase
- OGA:
-
O-GlcNAcase
- UDP-GlcNAc:
-
Uridine-5′-diphosphate-N-acetylglucosamine
- HBP:
-
Hexosamine biosynthetic pathway
- ATG:
-
Autophagy-related
- Nrf2:
-
Nuclear factor erythroid 2‐related factor 2
- RANKL:
-
Receptor activator of NF-κB ligand ligand
- ULK:
-
UNC51-like kinase
- FoxO:
-
Forkhead box transcription factor O
- VPS15:
-
Vacuolar protein sorting 15
- PI3P:
-
Phosphatidylinositol 3-phosphate
- LC3:
-
Microtubule-associated protein 1 light chain 3
- SNARE:
-
Soluble N-ethylmaleimide-sensitive factor attachment protein receptors
- AREs:
-
Antioxidant response elements
- Keap1:
-
Kelch‐like ECH‐associated protein 1
- CUL3:
-
CULLIN3
- HCF1:
-
Host Cell Factor-1
- FoxO:
-
Forkhead box class O
- TCF:
-
T cell factor
- PRG4:
-
Joint lubricant proteoglycan 4
- AMPK:
-
AMPactivated protein kinase
- Mtor :
-
Mammalian target of rapamycin
- 4E-BP1:
-
4E-binding protein 1
- S6K1:
-
S6 kinase1
- OPG:
-
Osteoprotegerin
- NFATc1:
-
Nuclear factor of activated T cells c1
References
Tang J-Y, Ou-Yang F, Hou M-F, Huang H-W, Wang H-R, Li K-T, et al. Oxidative stress-modulating drugs have preferential anticancer effects - involving the regulation of apoptosis, DNA damage, endoplasmic reticulum stress, autophagy, metabolism, and migration. Semin Cancer Biol. 2019;58:109–17.
Zou Z, Chang H, Li H, Wang S. Induction of reactive oxygen species: an emerging approach for cancer therapy. Apoptosis. 2017;22:1321–35.
Mobasheri A, Matta C, Zákány R, Musumeci G. Chondrosenescence: definition, hallmarks and potential role in the pathogenesis of osteoarthritis. Maturitas. 2015;80:237–44.
Weivoda MM, Bradley EW. Macrophages and Bone Remodeling. J Bone Miner Res. 2023;38:359–69.
Kang Q, Yang C. Oxidative stress and diabetic retinopathy: Molecular mechanisms, pathogenetic role and therapeutic implications. Redox Biol. 2020;37:101799.
On S-W, Cho S-W, Byun S-H, Yang B-E. Various Therapeutic Methods for the Treatment of Medication-Related Osteonecrosis of the Jaw (MRONJ) and Their Limitations: A Narrative Review on New Molecular and Cellular Therapeutic Approaches. Antioxidants (Basel). 2021;10:680.
Yang Y, Sun Y, Mao W-W, Zhang H, Ni B, Jiang L. Oxidative stress induces downregulation of TP53INP2 and suppresses osteogenic differentiation of BMSCs during osteoporosis through the autophagy degradation pathway. Free Radic Biol Med. 2021;166:226–37.
Kaur J, Debnath J. Autophagy at the crossroads of catabolism and anabolism. Nat Rev Mol Cell Biol. 2015;16:461–72.
Stolz A, Ernst A, Dikic I. Cargo recognition and trafficking in selective autophagy. Nat Cell Biol. 2014;16:495–501.
Mizushima N, Levine B, Cuervo AM, Klionsky DJ. Autophagy fights disease through cellular self-digestion. Nature. 2008;451:1069–75.
Wang S, Deng Z, Ma Y, Jin J, Qi F, Li S, et al. The Role of Autophagy and Mitophagy in Bone Metabolic Disorders. Int J Biol Sci. 2020;16:2675–91.
Yang X, Qian K. Protein O-GlcNAcylation: emerging mechanisms and functions. Nat Rev Mol Cell Biol. 2017;18:452–65.
Zhu Z, Ren W, Li S, Gao L, Zhi K. Functional significance of O-linked N-acetylglucosamine protein modification in regulating autophagy. Pharmacol Res. 2024;202:107120.
Zhang Z, Huang Z, Awad M, Elsalanty M, Cray J, Ball LE, et al. O-GlcNAc glycosylation orchestrates fate decision and niche function of bone marrow stromal progenitors. Elife. 2023;12:e85464.
Taira TM, Ramos-Junior ES, Melo PH, Costa-Silva CC, Alteen MG, Vocadlo DJ, et al. HBP/O-GlcNAcylation Metabolic Axis Regulates Bone Resorption Outcome. J Dent Res. 2023;102:440–9.
Xiong W-J, Lai X-L, Lu J, Li L-S, Zhang J-X, Duan X. O-GlcNAcylation orchestrates porcine oocyte maturation through maintaining mitochondrial dynamics and function. Mol Hum Reprod. 2024;30:gaae003.
Wende AR, Young ME, Chatham J, Zhang J, Rajasekaran NS, Darley-Usmar VM. Redox biology and the interface between bioenergetics, autophagy and circadian control of metabolism. Free Radic Biol Med. 2016;100:94–107.
Mannino MP, Hart GW. The Beginner’s Guide to O-GlcNAc: From Nutrient Sensitive Pathway Regulation to Its Impact on the Immune System. Front Immunol. 2022;13:828648.
Ferrer CM, Sodi VL, Reginato MJ. O-GlcNAcylation in Cancer Biology: Linking Metabolism and Signaling. J Mol Biol. 2016;428:3282–94.
Ma J, Hou C, Wu C. Demystifying the O-GlcNAc Code: A Systems View. Chem Rev. 2022;122:15822–64.
Decourcelle A, Leprince D, Dehennaut V. Regulation of Polycomb Repression by O-GlcNAcylation: Linking Nutrition to Epigenetic Reprogramming in Embryonic Development and Cancer. Front Endocrinol (Lausanne). 2019;10:117.
Song H, Ma J, Bian Z, Chen S, Zhu J, Wang J, et al. Global profiling of O-GlcNAcylated and/or phosphorylated proteins in hepatoblastoma. Signal Transduct Target Ther. 2019;4:40.
Ruan H-B, Nie Y, Yang X. Regulation of protein degradation by O-GlcNAcylation: crosstalk with ubiquitination. Mol Cell Proteomics. 2013;12:3489–97.
Yi W, Clark PM, Mason DE, Keenan MC, Hill C, Goddard WA, et al. Phosphofructokinase 1 glycosylation regulates cell growth and metabolism. Science. 2012;337:975–80.
Yang YR, Song M, Lee H, Jeon Y, Choi E-J, Jang H-J, et al. O-GlcNAcase is essential for embryonic development and maintenance of genomic stability. Aging Cell. 2012;11:439–48.
Wauquier F, Leotoing L, Coxam V, Guicheux J, Wittrant Y. Oxidative stress in bone remodelling and disease. Trends Mol Med. 2009;15:468–77.
Nandy A, Richards A, Thapa S, Akhmetshina A, Narayani N, Rendina-Ruedy E. Altered Osteoblast Metabolism with Aging Results in Lipid Accumulation and Oxidative Stress Mediated Bone Loss. Aging Dis. 2024;15:767–86.
Arafa E-SA, Elgendy NO, Elhemely MA, Abdelaleem EA, Mohamed WR. Diosmin mitigates dexamethasone-induced osteoporosis in vivo: Role of Runx2, RANKL/OPG, and oxidative stress. Biomed Pharmacother. 2023;161:114461.
Xue P, Hu X, Chang E, Wang L, Chen M, Wu T-H, et al. Deficiency of optineurin enhances osteoclast differentiation by attenuating the NRF2-mediated antioxidant response. Exp Mol Med. 2021;53:667–80.
Lima VV, Spitler K, Choi H, Webb RC, Tostes RC. O-GlcNAcylation and oxidation of proteins: is signalling in the cardiovascular system becoming sweeter? Clin Sci (Lond). 2012;123:473–86.
Pagesy P, Bouaboud A, Feng Z, Hulin P, Issad T. Short O-GlcNAcase is targeted to the mitochondria and regulates mitochondrial reactive oxygen species level. Cells. 2022;11:1827.
Chen P-H, Chi J-T, Boyce M. Functional crosstalk among oxidative stress and O-GlcNAc signaling pathways. Glycobiology. 2018;28:556–64.
Li K, Xie Y, You M, Huang L, Zheng X. Plasma sprayed cerium oxide coating inhibits H2O2-induced oxidative stress and supports cell viability. J Mater Sci Mater Med. 2016;27:100.
Zachara NE, O’Donnell N, Cheung WD, Mercer JJ, Marth JD, Hart GW. Dynamic O-GlcNAc modification of nucleocytoplasmic proteins in response to stress. A survival response of mammalian cells. J Biol Chem. 2004;279:30133–42.
Zhang C-C, Li Y, Jiang C-Y, Le Q-M, Liu X, Ma L, et al. O-GlcNAcylation mediates H2O2-induced apoptosis through regulation of STAT3 and FOXO1. Acta Pharmacol Sin. 2024;45:714–27.
Ou W, Liang Y, Qin Y, Wu W, Xie M, Zhang Y, et al. Hypoxic acclimation improves cardiac redox homeostasis and protects heart against ischemia-reperfusion injury through upregulation of O-GlcNAcylation. Redox Biol. 2021;43:101994.
Romagnoli C, Marcucci G, Favilli F, Zonefrati R, Mavilia C, Galli G, et al. Role of GSH/GSSG redox couple in osteogenic activity and osteoclastogenic markers of human osteoblast-like SaOS-2 cells. FEBS J. 2013;280:867–79.
Nakagawa T, Furukawa Y, Hayashi T, Nomura A, Yokoe S, Moriwaki K, et al. Augmented O-GlcNAcylation attenuates intermittent hypoxia-induced cardiac remodeling through the suppression of NFAT and NF-κB activities in mice. Hypertens Res. 2019;42:1858–71.
Zeng X, He L, Wang S, Wang K, Zhang Y, Tao L, et al. Aconine inhibits RANKL-induced osteoclast differentiation in RAW264.7 cells by suppressing NF-κB and NFATc1 activation and DC-STAMP expression. Acta Pharmacol Sin. 2016;37:255–63.
Xue Q, Yan R, Ji S, Yu S. Regulation of mitochondrial network homeostasis by O-GlcNAcylation. Mitochondrion. 2022;65:45–55.
Wang J, Zhang Y, Cao J, Wang Y, Anwar N, Zhang Z, et al. The role of autophagy in bone metabolism and clinical significance. Autophagy. 2023;19:2409–27.
Ceccariglia S, Cargnoni A, Silini AR, Parolini O. Autophagy: a potential key contributor to the therapeutic action of mesenchymal stem cells. Autophagy. 2020;16:28–37.
Yang L, Xiao L, Gao W, Huang X, Wei F, Zhang Q, et al. Macrophages at low-inflammatory status improved osteogenesis via autophagy regulation. Tissue Eng Part A. 2021. https://doi.org/10.1089/ten.tea.2021.0015.
Vidergar R, Biswas SK. Metabolic regulation of Cathepsin B in tumor macrophages drives their pro-metastatic function. Cancer Cell. 2022;40:1079–81.
Atashi F, Modarressi A, Pepper MS. The role of reactive oxygen species in mesenchymal stem cell adipogenic and osteogenic differentiation: a review. Stem Cells Dev. 2015;24:1150–63.
Xu Y, Shen J, Ran Z. Emerging views of mitophagy in immunity and autoimmune diseases. Autophagy. 2020;16:3–17.
Guo Y, Jia X, Cui Y, Song Y, Wang S, Geng Y, et al. Sirt3-mediated mitophagy regulates AGEs-induced BMSCs senescence and senile osteoporosis. Redox Biol. 2021;41:101915.
Murakami K, Kurotaki D, Kawase W, Soma S, Fukuchi Y, Kunimoto H, et al. OGT Regulates Hematopoietic Stem Cell Maintenance via PINK1-Dependent Mitophagy. Cell Rep. 2021;34:108579.
Xie X, Hu L, Mi B, Xue H, Hu Y, Panayi AC, et al. Metformin alleviates bone loss in ovariectomized mice through inhibition of autophagy of osteoclast precursors mediated by E2F1. Cell Commun Signal. 2022;20:165.
Kim MY, Kim YS, Kim M, Choi MY, Roh GS, Lee DH, et al. Metformin inhibits cervical cancer cell proliferation via decreased AMPK O-GlcNAcylation. Anim Cells Syst (Seoul). 2019;23:302–9.
Li H, Li D, Ma Z, Qian Z, Kang X, Jin X, et al. Defective autophagy in osteoblasts induces endoplasmic reticulum stress and causes remarkable bone loss. Autophagy. 2018;14:1726–41.
Lamb CA, Yoshimori T, Tooze SA. The autophagosome: origins unknown, biogenesis complex. Nat Rev Mol Cell Biol. 2013;14:759–74.
Galluzzi L, Bravo-San Pedro JM, Levine B, Green DR, Kroemer G. Pharmacological modulation of autophagy: therapeutic potential and persisting obstacles. Nat Rev Drug Discov. 2017;16:487–511.
Mizushima N. The role of the Atg1/ULK1 complex in autophagy regulation. Curr Opin Cell Biol. 2010;22:132–9.
Zachari M, Ganley IG. The mammalian ULK1 complex and autophagy initiation. Essays Biochem. 2017;61:585–96.
Levine B, Deretic V. Unveiling the roles of autophagy in innate and adaptive immunity. Nat Rev Immunol. 2007;7:767–77.
Diao J, Liu R, Rong Y, Zhao M, Zhang J, Lai Y, et al. ATG14 promotes membrane tethering and fusion of autophagosomes to endolysosomes. Nature. 2015;520:563–6.
Nakatogawa H, Oh-oka K, Ohsumi Y. Lipidation of Atg8: how is substrate specificity determined without a canonical E3 enzyme? Autophagy. 2008;4:911–3.
Zhao YG, Codogno P, Zhang H. Machinery, regulation and pathophysiological implications of autophagosome maturation. Nat Rev Mol Cell Biol. 2021;22:733–50.
Johansen T, Lamark T. Selective autophagy mediated by autophagic adapter proteins. Autophagy. 2011;7:279–96.
Pyo KE, Kim CR, Lee M, Kim J-S, Kim KI, Baek SH. ULK1 O-GlcNAcylation Is Crucial for Activating VPS34 via ATG14L during Autophagy Initiation. Cell Rep. 2018;25:2878-2890.e4.
Zhang S, Xie Y, Yan F, Zhang Y, Yang Z, Chen Z, et al. Negative pressure wound therapy improves bone regeneration by promoting osteogenic differentiation via the AMPK-ULK1-autophagy axis. Autophagy. 2022;18:2229–45.
Park NY, Jo DS, Cho D-H. Post-Translational Modifications of ATG4B in the Regulation of Autophagy. Cells. 2022;11:1330.
Hiura F, Kawabata Y, Aoki T, Mizokami A, Jimi E. Inhibition of the ATG4-LC3 pathway suppressed osteoclast maturation. Biochem Biophys Res Commun. 2022;632:40–7.
Jo YK, Park NY, Park SJ, Kim B-G, Shin JH, Jo DS, et al. O-GlcNAcylation of ATG4B positively regulates autophagy by increasing its hydroxylase activity. Oncotarget. 2016;7:57186–96.
Marsh SA, Powell PC, Dell’italia LJ, Chatham JC. Cardiac O-GlcNAcylation blunts autophagic signaling in the diabetic heart. Life Sci. 2013;92:648–56.
Arai A, Kim S, Goldshteyn V, Kim T, Park N-H, Wang C-Y, et al. Beclin1 Modulates Bone Homeostasis by Regulating Osteoclast and Chondrocyte Differentiation. J Bone Miner Res. 2019;34:1753–66.
Zhou F, Yang X, Zhao H, Liu Y, Feng Y, An R, et al. Down-regulation of OGT promotes cisplatin resistance by inducing autophagy in ovarian cancer. Theranostics. 2018;8:5200–12.
Pellegrini FR, De Martino S, Fianco G, Ventura I, Valente D, Fiore M, et al. Blockage of autophagosome-lysosome fusion through SNAP29 O-GlcNAcylation promotes apoptosis via ROS production. Autophagy. 2023;19:2078–93.
Park S, Lee Y, Pak JW, Kim H, Choi H, Kim J, et al. O-GlcNAc modification is essential for the regulation of autophagy in Drosophila melanogaster. Cell Mol Life Sci. 2015;72:3173–83.
DeSelm CJ, Miller BC, Zou W, Beatty WL, van Meel E, Takahata Y, et al. Autophagy proteins regulate the secretory component of osteoclastic bone resorption. Dev Cell. 2011;21:966–74.
Yu H, Wen L, Mu Y. O-GlcNAcylation Is Essential for Autophagy in Cardiomyocytes. Oxid Med Cell Longev. 2020;2020:5602396.
Guo B, Liang Q, Li L, Hu Z, Wu F, Zhang P, et al. O-GlcNAc-modification of SNAP-29 regulates autophagosome maturation. Nat Cell Biol. 2014;16:1215–26.
Kawai S, Michikami I, Kitagaki J, Hata K, Kiyonari H, Abe T, et al. Syntaxin 4a Regulates Matrix Vesicle-Mediated Bone Matrix Production by Osteoblasts. J Bone Miner Res. 2017;32:440–8.
Mihaylova MM, Shaw RJ. The AMPK signalling pathway coordinates cell growth, autophagy and metabolism. Nat Cell Biol. 2011;13:1016–23.
Guo H, Ouyang Y, Yin H, Cui H, Deng H, Liu H, et al. Induction of autophagy via the ROS-dependent AMPK-mTOR pathway protects copper-induced spermatogenesis disorder. Redox Biol. 2022;49:102227.
Liu GY, Sabatini DM. mTOR at the nexus of nutrition, growth, ageing and disease. Nat Rev Mol Cell Biol. 2020;21:183–203.
Chun Y, Kim J. AMPK-mTOR Signaling and Cellular Adaptations in Hypoxia. Int J Mol Sci. 2021;22:9765.
Hinchy EC, Gruszczyk AV, Willows R, Navaratnam N, Hall AR, Bates G, et al. Mitochondria-derived ROS activate AMP-activated protein kinase (AMPK) indirectly. J Biol Chem. 2018;293:17208–17.
Wang S, Song P, Zou M-H. AMP-activated protein kinase, stress responses and cardiovascular diseases. Clin Sci (Lond). 2012;122:555–73.
Jiang P, Ren L, Zhi L, Yu Z, Lv F, Xu F, et al. Negative regulation of AMPK signaling by high glucose via E3 ubiquitin ligase MG53. Mol Cell. 2021;81:629-637.e5.
Kim K, Kim JH, Kim I, Seong S, Koh J-T, Kim N. Sestrin2 inhibits RANKL-induced osteoclastogenesis through AMPK activation and ROS inhibition. Free Radic Biol Med. 2024;211:77–88.
Kundu M. ULK1, mammalian target of rapamycin, and mitochondria: linking nutrient availability and autophagy. Antioxid Redox Signal. 2011;14:1953–8.
Kim J, Kundu M, Viollet B, Guan K-L. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat Cell Biol. 2011;13:132–41.
Zhou Y, Yan J, Qiao L, Zeng J, Cao F, Sheng X, et al. Bone Marrow Mesenchymal Stem Cell-Derived Exosomes Ameliorate Aging-Induced BTB Impairment in Porcine Testes by Activating Autophagy and Inhibiting ROS/NLRP3 Inflammasomes via the AMPK/mTOR Signaling Pathway. Antioxidants (Basel). 2024;13:183.
Cai J, Zhang L-C, Zhao R-J, Pu L-M, Chen K-Y, Nasim AA, et al. Chelerythrine ameliorates rheumatoid arthritis by modulating the AMPK/mTOR/ULK-1 signaling pathway. Phytomedicine. 2022;104:154140.
Liu W, Zhao Y, Wang G, Feng S, Ge X, Ye W, et al. TRIM22 inhibits osteosarcoma progression through destabilizing NRF2 and thus activation of ROS/AMPK/mTOR/autophagy signaling. Redox Biol. 2022;53:102344.
Packer M. Foetal recapitulation of nutrient surplus signalling by O-GlcNAcylation and the failing heart. Eur J Heart Fail. 2023;25:1199–212.
Liu Y, Xu B, Hu Y, Liu P, Lian S, Lv H, et al. O-GlcNAc / Akt pathway regulates glucose metabolism and reduces apoptosis in liver of piglets with acute cold stress. Cryobiology. 2021;100:125–32.
Bullen JW, Balsbaugh JL, Chanda D, Shabanowitz J, Hunt DF, Neumann D, et al. Cross-talk between two essential nutrient-sensitive enzymes: O-GlcNAc transferase (OGT) and AMP-activated protein kinase (AMPK). J Biol Chem. 2014;289:10592–606.
Jin L, Yuan F, Dai G, Yao Q, Xiang H, Wang L, et al. Blockage of O-linked GlcNAcylation induces AMPK-dependent autophagy in bladder cancer cells. Cell Mol Biol Lett. 2020;25:17.
Murata K, Morino K, Ida S, Ohashi N, Lemecha M, Park S-Y, et al. Lack of O-GlcNAcylation enhances exercise-dependent glucose utilization potentially through AMP-activated protein kinase activation in skeletal muscle. Biochem Biophys Res Commun. 2018;495:2098–104.
Kim YS, Kim M, Choi MY, Lee DH, Roh GS, Kim HJ, et al. Alpha-lipoic acid reduces retinal cell death in diabetic mice. Biochem Biophys Res Commun. 2018;503:1307–14.
Latorre-Muro P, Puigserver P. A sweet way to regulate cellular growth: OGT and mTOR join forces. Mol Cell. 2023;83:2832–3.
Wang X, Lin Y, Liu S, Zhu Y, Lu K, Broering R, et al. O-GlcNAcylation modulates HBV replication through regulating cellular autophagy at multiple levels. FASEB J. 2020;34:14473–89.
Park S, Pak J, Jang I, Cho JW. Inhibition of mTOR affects protein stability of OGT. Biochem Biophys Res Commun. 2014;453:208–12.
Very N, Steenackers A, Dubuquoy C, Vermuse J, Dubuquoy L, Lefebvre T, et al. Cross regulation between mTOR signaling and O-GlcNAcylation. J Bioenerg Biomembr. 2018;50:213–22.
Xu C, Pan X, Wang D, Guan Y, Yang W, Chen X, et al. O-GlcNAcylation of Raptor transduces glucose signals to mTORC1. Mol Cell. 2023;83:3027-3040.e11.
Wang J, Xu C, Zhang J, Bao Y, Tang Y, Lv X, et al. RhoA promotes osteoclastogenesis and regulates bone remodeling through mTOR-NFATc1 signaling. Mol Med. 2023;29:49.
Yang Y, Li X, Luan HH, Zhang B, Zhang K, Nam JH, et al. OGT suppresses S6K1-mediated macrophage inflammation and metabolic disturbance. Proc Natl Acad Sci U S A. 2020;117:16616–25.
Zhu L, He S, Huang L, Ren D, Nie T, Tao K, et al. Chaperone-mediated autophagy degrades Keap1 and promotes Nrf2-mediated antioxidative response. Aging Cell. 2022;21:e13616.
Yamamoto M, Kensler TW, Motohashi H. The KEAP1-NRF2 System: a Thiol-Based Sensor-Effector Apparatus for Maintaining Redox Homeostasis. Physiol Rev. 2018;98:1169–203.
Zhang DD, Lo S-C, Cross JV, Templeton DJ, Hannink M. Keap1 is a redox-regulated substrate adaptor protein for a Cul3-dependent ubiquitin ligase complex. Mol Cell Biol. 2004;24:10941–53.
Sánchez-de-Diego C, Pedrazza L, Pimenta-Lopes C, Martinez-Martinez A, Dahdah N, Valer JA, et al. NRF2 function in osteocytes is required for bone homeostasis and drives osteocytic gene expression. Redox Biol. 2021;40:101845.
Sun X, Xie Z, Hu B, Zhang B, Ma Y, Pan X, et al. The Nrf2 activator RTA-408 attenuates osteoclastogenesis by inhibiting STING dependent NF-κb signaling. Redox Biol. 2020;28:101309.
Lamark T, Svenning S, Johansen T. Regulation of selective autophagy: the p62/SQSTM1 paradigm. Essays Biochem. 2017;61:609–24.
Komatsu M, Kurokawa H, Waguri S, Taguchi K, Kobayashi A, Ichimura Y, et al. The selective autophagy substrate p62 activates the stress responsive transcription factor Nrf2 through inactivation of Keap1. Nat Cell Biol. 2010;12:213–23.
Kumar AV, Mills J, Lapierre LR. Selective Autophagy Receptor p62/SQSTM1, a Pivotal Player in Stress and Aging. Front Cell Dev Biol. 2022;10:793328.
Sánchez-Martín P, Komatsu M. p62/SQSTM1 - steering the cell through health and disease. J Cell Sci. 2018;131:jcs222836.
Zhang W, Feng C, Jiang H. Novel target for treating Alzheimer’s Diseases: Crosstalk between the Nrf2 pathway and autophagy. Ageing Res Rev. 2021;65:101207.
Dikic I. Proteasomal and Autophagic Degradation Systems. Annu Rev Biochem. 2017;86:193–224.
Wang D, Xu C, Yang W, Chen J, Ou Y, Guan Y, et al. E3 ligase RNF167 and deubiquitinase STAMBPL1 modulate mTOR and cancer progression. Mol Cell. 2022;82:770-784.e9.
Liao K, Su X, Lei K, Liu Z, Lu L, Wu Q, et al. Sinomenine protects bone from destruction to ameliorate arthritis via activating p62Thr269/Ser272-Keap1-Nrf2 feedback loop. Biomed Pharmacother. 2021;135:111195.
Chen P-H, Smith TJ, Wu J, Siesser PF, Bisnett BJ, Khan F, et al. Glycosylation of KEAP1 links nutrient sensing to redox stress signaling. EMBO J. 2017;36:2233–50.
Xu T-H, Du Y, Sheng Z, Li Y, Qiu X, Tian B, et al. OGT-Mediated KEAP1 Glycosylation Accelerates NRF2 Degradation Leading to High Phosphate-Induced Vascular Calcification in Chronic Kidney Disease. Front Physiol. 2020;11:1092.
Huang W, Chen L, Zhu K, Wang D. Oncogenic microRNA-181d binding to OGT contributes to resistance of ovarian cancer cells to cisplatin. Cell Death Discov. 2021;7:379.
Wang Y-F, Chang Y-Y, Zhang X-M, Gao M-T, Zhang Q-L, Li X, et al. Salidroside protects against osteoporosis in ovariectomized rats by inhibiting oxidative stress and promoting osteogenesis via Nrf2 activation. Phytomedicine. 2022;99:154020.
Costa RM, Dias MC, Alves JV, Silva JLM, Rodrigues D, Silva JF, et al. Pharmacological activation of nuclear factor erythroid 2-related factor-2 prevents hyperglycemia-induced renal oxidative damage: Possible involvement of O-GlcNAcylation. Biochem Pharmacol. 2024;220:115982.
Han JW, Valdez JL, Ho DV, Lee CS, Kim HM, Wang X, et al. Nuclear factor-erythroid-2 related transcription factor-1 (Nrf1) is regulated by O-GlcNAc transferase. Free Radic Biol Med. 2017;110:196–205.
Li X, Zhang Z, Li L, Gong W, Lazenby AJ, Swanson BJ, et al. Myeloid-derived cullin 3 promotes STAT3 phosphorylation by inhibiting OGT expression and protects against intestinal inflammation. J Exp Med. 2017;214:1093–109.
Han I, Oh ES, Kudlow JE. Responsiveness of the state of O-linked N-acetylglucosamine modification of nuclear pore protein p62 to the extracellular glucose concentration. Biochem J. 2000;350(Pt 1):109–14.
Vocadlo DJ, Hang HC, Kim E-J, Hanover JA, Bertozzi CR. A chemical approach for identifying O-GlcNAc-modified proteins in cells. Proc Natl Acad Sci U S A. 2003;100:9116–21.
Lubas WA, Smith M, Starr CM, Hanover JA. Analysis of nuclear pore protein p62 glycosylation. Biochemistry. 1995;34:1686–94.
Kops GJPL, Dansen TB, Polderman PE, Saarloos I, Wirtz KWA, Coffer PJ, et al. Forkhead transcription factor FOXO3a protects quiescent cells from oxidative stress. Nature. 2002;419:316–21.
Tan W-Q, Wang K, Lv D-Y, Li P-F. Foxo3a inhibits cardiomyocyte hypertrophy through transactivating catalase. J Biol Chem. 2008;283:29730–9.
Wang X, Tian Y, Liang X, Yin C, Huai Y, Zhao Y, et al. Bergamottin promotes osteoblast differentiation and bone formation via activating the Wnt/β-catenin signaling pathway. Food Funct. 2022;13:2913–24.
Almeida M, Han L, Martin-Millan M, O’Brien CA, Manolagas SC. Oxidative stress antagonizes Wnt signaling in osteoblast precursors by diverting beta-catenin from T cell factor- to forkhead box O-mediated transcription. J Biol Chem. 2007;282:27298–305.
Klotz L-O, Sánchez-Ramos C, Prieto-Arroyo I, Urbánek P, Steinbrenner H, Monsalve M. Redox regulation of FoxO transcription factors. Redox Biol. 2015;6:51–72.
Lehtinen MK, Yuan Z, Boag PR, Yang Y, Villén J, Becker EBE, et al. A conserved MST-FOXO signaling pathway mediates oxidative-stress responses and extends life span. Cell. 2006;125:987–1001.
Ho K-K, McGuire VA, Koo C-Y, Muir KW, de Olano N, Maifoshie E, et al. Phosphorylation of FOXO3a on Ser-7 by p38 promotes its nuclear localization in response to doxorubicin. J Biol Chem. 2012;287:1545–55.
Ma X, Su P, Yin C, Lin X, Wang X, Gao Y, et al. The Roles of FoxO Transcription Factors in Regulation of Bone Cells Function. Int J Mol Sci. 2020;21:692.
Bartell SM, Kim H-N, Ambrogini E, Han L, Iyer S, Serra Ucer S, et al. FoxO proteins restrain osteoclastogenesis and bone resorption by attenuating H2O2 accumulation. Nat Commun. 2014;5:3773.
Iyer S, Ambrogini E, Bartell SM, Han L, Roberson PK, de Cabo R, et al. FOXOs attenuate bone formation by suppressing Wnt signaling. J Clin Invest. 2013;123:3409–19.
Fan W, Imamura T, Sonoda N, Sears DD, Patsouris D, Kim JJ, et al. FOXO1 transrepresses peroxisome proliferator-activated receptor gamma transactivation, coordinating an insulin-induced feed-forward response in adipocytes. J Biol Chem. 2009;284:12188–97.
Zhang Z, Kuang Y, Ma K, Li Y, Liu X, Shi Y, et al. Gclc overexpression inhibits apoptosis of bone marrow mesenchymal stem cells through the PI3K/AKT/Foxo1 pathway to alleviate inflammation in acute lung injury. Int Immunopharmacol. 2022;110:109017.
Xiong Y, Zhang Y, Zhou F, Liu Y, Yi Z, Gong P, et al. FOXO1 differentially regulates bone formation in young and aged mice. Cell Signal. 2022;99:110438.
Gómez-Puerto MC, Verhagen LP, Braat AK, Lam EW-F, Coffer PJ, Lorenowicz MJ. Activation of autophagy by FOXO3 regulates redox homeostasis during osteogenic differentiation. Autophagy. 2016;12:1804.
Lee KI, Choi S, Matsuzaki T, Alvarez-Garcia O, Olmer M, Grogan SP, et al. FOXO1 and FOXO3 transcription factors have unique functions in meniscus development and homeostasis during aging and osteoarthritis. Proc Natl Acad Sci U S A. 2020;117:3135–43.
Yoshida T, Delafontaine P. Mechanisms of IGF-1-Mediated Regulation of Skeletal Muscle Hypertrophy and Atrophy. Cells. 2020;9:1970.
Ohzono H, Hu Y, Nagira K, Kanaya H, Okubo N, Olmer M, et al. Targeting FoxO transcription factors with HDAC inhibitors for the treatment of osteoarthritis. Ann Rheum Dis. 2023;82:262–71.
Sandri M. FOXOphagy path to inducing stress resistance and cell survival. Nat Cell Biol. 2012;14:786–8.
Nakae J, Oki M, Cao Y. The FoxO transcription factors and metabolic regulation. FEBS Lett. 2008;582:54–67.
McClain DA, Lubas WA, Cooksey RC, Hazel M, Parker GJ, Love DC, et al. Altered glycan-dependent signaling induces insulin resistance and hyperleptinemia. Proc Natl Acad Sci U S A. 2002;99:10695–9.
Vosseller K, Wells L, Lane MD, Hart GW. Elevated nucleocytoplasmic glycosylation by O-GlcNAc results in insulin resistance associated with defects in Akt activation in 3T3-L1 adipocytes. Proc Natl Acad Sci U S A. 2002;99:5313–8.
Housley MP, Rodgers JT, Udeshi ND, Kelly TJ, Shabanowitz J, Hunt DF, et al. O-GlcNAc regulates FoxO activation in response to glucose. J Biol Chem. 2008;283:16283–92.
Haefliger S, Genevay M, Bihl M, Marone R, Baumhoer D, Papaloizos M, et al. FOXO1 gene involvement in a non-rhabdomyosarcomatous neoplasm. Virchows Arch. 2021;479:1031–6.
Boldig K, Montanarella M, Fu W, So JM, Lucke JC, Taylor K, et al. Myoepithelioma-like hyalinizing epithelioid tumor of the foot with OGT-FOX03 fusion gene: Imaging findings, surgical implications, and pathological correlates. Radiol Case Rep. 2023;18:926–31.
Zhang M, Sui W, Xing Y, Cheng J, Cheng C, Xue F, et al. Angiotensin IV attenuates diabetic cardiomyopathy via suppressing FoxO1-induced excessive autophagy, apoptosis and fibrosis. Theranostics. 2021;11:8624–39.
Iyer S, Han L, Ambrogini E, Yavropoulou M, Fowlkes J, Manolagas SC, et al. Deletion of Fox O1, 3, and 4 in Osteoblast Progenitors Attenuates the Loss of Cancellous Bone Mass in a Mouse Model of Type 1 Diabetes. J Bone Miner Res. 2017;32:60–9.
Zhu Y, Hart GW. Dual-specificity RNA aptamers enable manipulation of target-specific O-GlcNAcylation and unveil functions of O-GlcNAc on β-catenin. Cell. 2023;186:428-445.e27.
Gao S, Miao Y, Liu Y, Liu X, Fan X, Lin Y, et al. Reciprocal Regulation Between O-GlcNAcylation and β-Catenin Facilitates Cell Viability and Inhibits Apoptosis in Liver Cancer. DNA Cell Biol. 2019;38:286–96.
Shen H, Zhao X, Chen J, Qu W, Huang X, Wang M, et al. O-GlcNAc transferase Ogt regulates embryonic neuronal development through modulating Wnt/β-catenin signaling. Hum Mol Genet. 2021;31:57–68.
Olivier-Van Stichelen S, Dehennaut V, Buzy A, Zachayus J-L, Guinez C, Mir A-M, et al. O-GlcNAcylation stabilizes β-catenin through direct competition with phosphorylation at threonine 41. FASEB J. 2014;28:3325–38.
Deng L, Yi S, Yin X, Li Y, Luan Q. MFN2 knockdown promotes osteogenic differentiation of iPSC-MSCs through aerobic glycolysis mediated by the Wnt/β-catenin signaling pathway. Stem Cell Res Ther. 2022;13:162.
Vallabhapurapu S, Karin M. Regulation and function of NF-kappaB transcription factors in the immune system. Annu Rev Immunol. 2009;27:693–733.
Boyce BF. Advances in the regulation of osteoclasts and osteoclast functions. J Dent Res. 2013;92:860–7.
Udagawa N, Koide M, Nakamura M, Nakamichi Y, Yamashita T, Uehara S, et al. Osteoclast differentiation by RANKL and OPG signaling pathways. J Bone Miner Metab. 2021;39:19–26.
Hayden MS, Ghosh S. Shared principles in NF-kappaB signaling. Cell. 2008;132:344–62.
Boyce BF, Yao Z, Xing L. Functions of nuclear factor kappaB in bone. Ann N Y Acad Sci. 2010;1192:367–75.
Özcan E, Saygun NI, Ilıkçı R, Karslıoğlu Y, Muşabak U, Yeşillik S. Increased visfatin expression is associated with nuclear factor-kappa B and phosphatidylinositol 3-kinase in periodontal inflammation. Clin Oral Investig. 2017;21:1113–21.
Zhang C, Li H, Li J, Hu J, Yang K, Tao L. Oxidative stress: A common pathological state in a high-risk population for osteoporosis. Biomed Pharmacother. 2023;163:114834.
Jin K, Zheng L, Ye L, Xie Z, Gao J, Lou C, et al. Chicago sky blue 6B (CSB6B), an allosteric inhibitor of macrophage migration inhibitory factor (MIF), suppresses osteoclastogenesis and promotes osteogenesis through the inhibition of the NF-κB signaling pathway. Biochem Pharmacol. 2021;192:114734.
Zhang Y, Liu T, Yang H, He F, Zhu X. Melatonin: A novel candidate for the treatment of osteoarthritis. Ageing Res Rev. 2022;78:101635.
Verzella D, Pescatore A, Capece D, Vecchiotti D, Ursini MV, Franzoso G, et al. Life, death, and autophagy in cancer: NF-κB turns up everywhere. Cell Death Dis. 2020;11:210.
Arnst J, Jing Z, Cohen C, Ha S-W, Viggeswarapu M, Beck GR. Bioactive silica nanoparticles target autophagy, NF-κB, and MAPK pathways to inhibit osteoclastogenesis. Biomaterials. 2023;301:122238.
Hu R, Luo H, Ji Y, Wang Z, Zheng P, Ouyang H, et al. Activation of NLRP3 signaling contributes to cadmium-induced bone defects, associated with autophagic flux obstruction. Sci Total Environ. 2023;893:164787.
Nivon M, Richet E, Codogno P, Arrigo A-P, Kretz-Remy C. Autophagy activation by NFkappaB is essential for cell survival after heat shock. Autophagy. 2009;5:766–83.
Na W, Lee E-J, Kang M-K, Kim Y-H, Kim DY, Oh H, et al. Aesculetin Inhibits Osteoclastic Bone Resorption through Blocking Ruffled Border Formation and Lysosomal Trafficking. Int J Mol Sci. 2020;21:8581.
Ke D, Yu Y, Li C, Han J, Xu J. Phosphorylation of BCL2 at the Ser70 site mediates RANKL-induced osteoclast precursor autophagy and osteoclastogenesis. Mol Med. 2022;28:22.
Wu D, Sun X, Zhao Y, Liu Y, Gan Z, Zhang Z, et al. Strontium Ranelate Inhibits Osteoclastogenesis through NF-κB-Pathway-Dependent Autophagy. Bioengineering (Basel). 2023;10:365.
Sarkar S, Korolchuk VI, Renna M, Imarisio S, Fleming A, Williams A, et al. Complex inhibitory effects of nitric oxide on autophagy. Mol Cell. 2011;43:19–32.
Balaburski GM, Hontz RD, Murphy ME. p53 and ARF: unexpected players in autophagy. Trends Cell Biol. 2010;20:363–9.
Djavaheri-Mergny M, Amelotti M, Mathieu J, Besançon F, Bauvy C, Souquère S, et al. NF-kappaB activation represses tumor necrosis factor-alpha-induced autophagy. J Biol Chem. 2006;281:30373–82.
Qing G, Yan P, Xiao G. Hsp90 inhibition results in autophagy-mediated proteasome-independent degradation of IkappaB kinase (IKK). Cell Res. 2006;16:895–901.
Komatsu M, Kageyama S, Ichimura Y. p62/SQSTM1/A170: physiology and pathology. Pharmacol Res. 2012;66:457–62.
Dong H, Liu Z, Wen H. Protein O-GlcNAcylation Regulates Innate Immune Cell Function. Front Immunol. 2022;13:805018.
Zou L, Yang S, Champattanachai V, Hu S, Chaudry IH, Marchase RB, et al. Glucosamine improves cardiac function following trauma-hemorrhage by increased protein O-GlcNAcylation and attenuation of NF-{kappa}B signaling. Am J Physiol Heart Circ Physiol. 2009;296:H515-523.
Hwang J-S, Kim K-H, Park J, Kim S-M, Cho H, Lee Y, et al. Glucosamine improves survival in a mouse model of sepsis and attenuates sepsis-induced lung injury and inflammation. J Biol Chem. 2019;294:608–22.
Kim MJ, Kim HS, Lee S, Min KY, Choi WS, You JS. Hexosamine Biosynthetic Pathway-Derived O-GlcNAcylation Is Critical for RANKL-Mediated Osteoclast Differentiation. Int J Mol Sci. 2021;22:8888.
Zhang D, Cai Y, Chen M, Gao L, Shen Y, Huang Z. OGT-mediated O-GlcNAcylation promotes NF-κB activation and inflammation in acute pancreatitis. Inflamm Res. 2015;64:943–52.
Ma Z, Vocadlo DJ, Vosseller K. Hyper-O-GlcNAcylation is anti-apoptotic and maintains constitutive NF-κB activity in pancreatic cancer cells. J Biol Chem. 2013;288:15121–30.
Yang WH, Park SY, Nam HW, Kim DH, Kang JG, Kang ES, et al. NFkappaB activation is associated with its O-GlcNAcylation state under hyperglycemic conditions. Proc Natl Acad Sci U S A. 2008;105:17345–50.
Sun Q-H, Wang Y-S, Liu G, Zhou H-L, Jian Y-P, Liu M-D, et al. Enhanced O-linked Glcnacylation in Crohn’s disease promotes intestinal inflammation. EBioMedicine. 2020;53:102693.
Tian P, Zhao L, Kim J, Li X, Liu C, Cui X, et al. Dual stimulus responsive borosilicate glass (BSG) scaffolds promote diabetic alveolar bone defectsrepair by modulating macrophage phenotype. Bioact Mater. 2023;26:231–48.
Acknowledgements
Not applicable.
Funding
This study was funded by National Natural Science Foundation of China (No.42176096, 42176097), Natural Science Foundation of Shandong Province (No. ZR2021MD065, ZR2021MH305, ZR2022MH223), TaiShan Scholars Foundation of Shandong Province (No. tsqn202306397), State Administration of Traditional Chinese Medicine Science and Technology department co-construction of science and technology project (No. GZY-KJS-SD-2023–078), Medical and Health Science and Technology Development Project of Shandong Province(202308021296), Qingdao Medical and Health Excellent Subject Leader.
Author information
Authors and Affiliations
Contributions
Li SQ: Study conception and design, data collection, writing – original draft. Ren WH: Data collection, writing – review & editing, and visualization. Zheng JJ: Data collection and writing – review & editing. Li SM: Data collection and visualization. Zhi KQ: Supervision and funding acquisition. Gao L: Study conception and design, supervision, and funding acquisition. All authors approved the final manuscript to be published.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, S., Ren, W., Zheng, J. et al. Role of O-linked N-acetylglucosamine protein modification in oxidative stress-induced autophagy: a novel target for bone remodeling. Cell Commun Signal 22, 358 (2024). https://doi.org/10.1186/s12964-024-01734-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12964-024-01734-3