Abstract
Cisplatin (CDDP) is a widely used first-line chemotherapeutic drug in various cancers. However, CDDP resistance is frequently observed in cancer patients. Therefore, it is required to evaluate the molecular mechanisms associated with CDDP resistance to improve prognosis among cancer patients. Integrins are critical factors involved in tumor metastasis that regulate cell-matrix and cell-cell interactions. They modulate several cellular mechanisms including proliferation, invasion, angiogenesis, polarity, and chemo resistance. Modification of integrin expression levels can be associated with both tumor progression and inhibition. Integrins are also involved in drug resistance of various solid tumors through modulation of the tumor cell interactions with interstitial matrix and extracellular matrix (ECM). Therefore, in the present review we discussed the role of integrin protein family in regulation of CDDP response in tumor cells. It has been reported that integrins mainly promoted the CDDP resistance through interaction with PI3K/AKT, MAPK, and WNT signaling pathways. They also regulated the CDDP mediated apoptosis in tumor cells. This review paves the way to suggest the integrins as the reliable therapeutic targets to improve CDDP response in tumor cells.
Similar content being viewed by others
Background
Tumor cell metastasis involves a series of sequential stages including spreading from the initial tumor, circulating through the bloodstream, and distant metastasis [1]. Tumor cells employ a variety of molecules to modulate their interactions with microenvironment. Integrins are critical factors involved in tumor metastasis that regulate cell-matrix and cell-cell interactions [2]. Extracellular matrix (ECM) is involved in oncogenesis, microenvironment remodeling, chemo-resistance, and tumor invasion [3, 4]. The integrin protein family comprises α- and β-subunits, which constitute cellular surface transmembrane receptors that are involved in cellular adhesion. They modulate several cellular mechanisms including proliferation, invasion, angiogenesis, polarity, and chemo resistance [5, 6]. Modification of integrin expression levels is contributed with both tumor progression and inhibition [7,8,9]. Up regulation of integrin subtypes such as β1, αv, and α4/5 are associated with tumor cell aggressiveness [10,11,12,13]. Integrin-associated intra-cellular signaling pathways are initially prompted by triggering focal adhesion kinase (FAK) to activate the Src kinases family that subsequently induce Ras/RAF/MEK/ERK or PI3K/Akt signaling pathways [14,15,16]. Integrin also induces cell proliferation through the GSK3β/Wnt axis [17]. Cisplatin (CDDP) as a widely used first-line chemotherapeutic drug accumulates in mitochondria and corrupts the mitochondrial function and structure [18], and therefore alters the level of metabolites associated with the glycolysis pathway and tricarboxylic acid cycle (TCA) cycle [19, 20]. Cisplatin can react with sulfhydryl groups of proteins and purine base in DNA. It binds with the purine bases to interfere with DNA repair that results in apoptosis induction in tumor cells [21, 22]. Cisplatin also promotes the generation of reactive oxygen species that induce apoptosis besides DNA damage [23]. Cisplatin is effective against the different tumor types including germ cell tumors, sarcomas, carcinomas, and lymphomas. However, there is a high rate of CDDP resistance and side effects in cancer patients [24]. Various cellular and molecular mechanisms such as drug efflux, detoxification, and increased DNA repair are involved in chemo resistance of tumor cells [25,26,27,28,29]. Integrins are involved in the drug resistance of various solid tumors [30,31,32] and hematological cancers [33,34,35] through modulation of the tumor cell interactions with interstitial matrix and ECM. Cell adhesion-mediated drug resistance (CAM-DR) facilitates prompt adaptation of tumor cells for extended survival [36]. ITGA7 inhibition reduced cisplatin resistance and sphere-forming ability of tumor cells [37]. MiR-199a-3p promoted the CDDP sensitivity of ovarian tumor cells through ITGB8 targeting [38]. ITGB1 induced tumor cell viability in various cancers by stimulating chemo resistance [30, 39, 40]. Several pre-clinical studies have already shown promising anti-tumor effects for integrin-associated treatments such as peptides, plant-derived molecules, and monoclonal antibodies. Moreover, the potential anti-tumor actions of a number of these agents have also been studied through clinical trials [41,42,43,44]. Monoclonal antibody against beta 1 integrin promoted the efficacy of cisplatin therapy in tumor cells [45]. Therefore, in the present review we discussed the molecular mechanisms of integrin protein family during CDDP response in tumor cells to introduce them as the reliable targets to improve the CDDP efficiency in cancer patients (Table 1). PubMed, Google Scholar, Scopus, and Web of Science were used for data retrieval that was limited to 15 Jan 2024. The following keywords were used: “integrin”, “cisplatin”, and “cancer”.
PI3K/AKT signaling pathway
Integrin protein family has a key role in CDDP response by regulation of PI3K/AKT pathway (Fig. 1). RhoA and Rac small GTPase are involved in regulation of actin rearrangements and cell migration [46,47,48]. RhoA-GTP which is the active from of RhoA enhances the aggregation of stress fibers and promotes new focal adhesions [49]. FAK activated AKT to induce actin polymerization and the formation of filopodia. Accordingly, CDDP promoted the FAK/AKT axis, which was associated with enhanced filopodia formation in cell lines. In addition, there was a dose-dependent over-expression of Rac-GTP and RhoA-GTP in CDDP-treated cells. Finally, CDDP-treated tumor cells have shown an enhanced activation of migratory proteins such as Rac, Rho A, AKT, and FAK and an over-expression of migration-associated integrins such as αv, α4, and β1/β5 [50]. Integrin β1 (ITGB1) interacts with focal adhesion kinase (FAK) to stimulate FAK phosphorylation [42, 51], subsequently triggering several signaling pathways such as integrin, c-Src, protein kinase B (Akt), and paxillin [52,53,54]. ITGB1 reversed the effects of 5-FU and CDDP in reducing proliferation and inducing apoptosis in HCC cells via FAK/Akt axis [55]. Integrin β1 up regulation was associated with higher stage, tumor recurrence, and poor prognosis in triple-negative breast cancer (TNBC) patients. Integrin β1 expression was also correlated with levels of phosphorylated AKT and FAK. Inhibition of Integrin β1 enhanced cisplatin sensitivity while reduced FAK and AKT activity in breast tumor cells [56]. Suppression of Integrin β1 inhibited esophageal squamous-cell carcinomas (ESCC) cell mobility as well as lymph nodal and pulmonary metastasis. Integrin β1 employed its pro-invasion role by modulating the FAK/Rac1 axis. In addition, ESCC cells lacking Integrin β1 were sensitized to CDDP treatment while remaining unresponsive to paclitaxel [57]. ECM1 modulates gastric tumor cell glucose metabolism and invasion via the ITB4/FAK/SOX2/HIF-1α axis [58]. Moreover, ECM1 modulates the architecture of actin cytoskeleton, which results in breast tumor cell invasion [59]. ECM1a modulated CDDP resistance and tumor formation by activating the AKT/FAK/Paxillin/Rac/cytoskeletal axis and stimulating the CD326 via various mechanisms such as alternative splicing through hnRNPLL, enhancing tumor cell stemness via ABCG1, and interacting with integrin αXβ2 through the Gly-Pro-Arg (GPR) motif. ECM1b stimulated myosin phosphorylation via inducing the AKT/FAK/Paxillin/Rac axis. Consequently, myosin phosphorylation is a potential participant in downstream of the ECM1/integrin αXβ2 axis. ABCG1 phosphorylated AKT2 to trigger the interaction of ECM1a and integrin αXβ2 [60]. ITGB5 stimulated intra-cellular pathways via promoting and utilizing integrin-related kinases such as FAK. FAK interacts with Src to participate in ITGB5-mediated response to Ras and VEGF transformation in fibroblasts [14, 61, 62]. Cisplatin inhibited cervical and breast tumor cell proliferation and growth by reducing the glucose metabolism. ITGB5 facilitated tumor cell glycolysis by promoting the FAK/p-FAK axis. ITGB5 significantly suppressed the anti-tumor properties of CDDP. ITGB5 promoted the FAK axis to stimulate tumor cell glycolysis while suppressed CDDP anti-tumor properties [63]. Integrin α5β1 is overexpressed in tumor vessel luminal surface and is involved in angiogenesis [64, 65]. Integrin α5β1 is contributed with tumor cell metastasis via modulating the matrix metalloproteinases (MMPs), cell adhesion, and actin cytoskeleton modification [66,67,68,69]. Integrin α5β1-induced cell adhesion triggers cell adhesion-mediated drug resistance (CAM-DR) and reduces the apoptosis and response of human myeloma cells to gamma-irradiation and DNA damage agents [70]. Proteins with Arg-Gly-Asp (RGD) binding region along with their integrin receptors have key roles in cellular adhesion. Integrin α5β1 is a main recognition receptor for RGD peptide motifs and Integrin β1 pathway is an important contributor to tension-associated metastasis [71]. There was Integrin α5β1 up regulation in ESCC tissues, which was correlated with poor prognosis. Inhibition of Integrin β1 and L1CAM diminished AKT activation and CDDP resistance [72]. Galectin-1 is a member of β-galactoside-binding lectins and contributes to many biological mechanisms including cell proliferation, cell invasion and adhesion, immunosuppression, and angiogenesis [73]. GAL1 induces tumor progression through activation of FAK/PI3K/AKT/mTOR axis [74]. There were integrin α5β1 and GAL1 up regulations in squamous cervical cancer stromal and tumor cells following neoadjuvant chemotherapy (NACT). In addition, patients with inadequate CDDP-based NACT response exhibited elevated levels of stromal integrin α5β1 and GAL1 as compared with controls. Therefore, integrin α5β1 plays a role in cervical cancer chemo resistance by inhibiting apoptosis [75].
mTOR is a serine/threonine kinase that is involved in autophagy, cell growth, ferroptosis, and metabolism by incorporating various components including nutrient status and growth factors [76,77,78]. EFNB2 is a ligand for Eph receptors that is involved in angiogenesis and tumor metastasis [79, 80]. ITGA5 stimulated tumor progression via up regulating EFNB2 in laryngeal squamous cell carcinoma (LSCC). There was mTORC1-ITGA5-EFNB2 axis up regulation in LSCC tissues, which was associated with poor prognosis. ITGA5 knockdown inhibited tumor growth while promoting CDDP sensitivity in LSCC cells. HIF-1α as an mTORC1 target was also found as a mediator of ITGA5 transcription in LSCC cells. Additionally, EFNB2 was found as an ITGA5 downstream gene in LSCC cells. ITGA5 knockdown in LSCC cells resulted in Jagged1 down regulation and Notch axis suppression. The mTORC1-mediated ITGA5 up regulation increased the levels of EFNB2 expressions via activation of the Jagged1/Notch axis in LSCC cells [81]. Neuropilin-1 (NRP1) acts as a co-receptor for VEGF during vascular formation and for class-3 semaphorin proteins through neuronal guidance [82,83,84]. Neuropilin-1 modulates neuronal cell migration and chemo repulsion by transducing semaphorin3A pathway via plexin-A1 [85, 86]. NRP1 antagonist suppressed the migration of ACHN and A549 carcinoma cells. NRP1 interacted with integrin-b1 to stimulate the adhesion of tumor cells to matrix proteins. NRP1 antagonist also enhanced the tumor cell sensitivity toward CDDP, paclitaxel, and 5-FU [87].
NG2 is a membrane associated proteoglycan produced by progenitor cells in various tissues [88]. NG2/MPG is implicated in multiple crucial mechanisms during the proliferation and metastasis of tumor cells such as cell responses to growth factors [89, 90] and cell migration [91, 92]. NG2/MPG induced chemo resistance by stimulating the PI3K/Akt axis through integrins. NG2/MPG-induced activation of α3β1 led to the transduction of survival signals by promoting the PI3K/Akt axis [93]. Adipocytes are abundantly found in the omentum to supply the fatty acids required for tumor growth. Therefore, targeting metabolism and transport of lipids might pave the way for new OC treatments [94]. STC1 is a glycoprotein hormone found in multiple tissues including the kidney [95], skeletal muscles [96], and spleen [97]. Elevated STC1 expression was seen in several cancers [98,99,100]. STC1 enhanced lipid metabolism by stimulating lipid-associated genes like perilipin1, TOM20, and UCP1. STC1 attached to ITGB6 to trigger the PI3K axis, which was mediated by FOXC2. Moreover, inhibition of STC1 and the FOXC2/ITGB6 pathway in ovarian cancer (OC) was associated with CDDP resistance [101]. Retinoic acid–related orphan receptor C (RORC) belongs to nuclear orphan receptors and acts as a DNA-binding factor [102]. There was RORC down regulation in bladder tumor tissues, which was associated with chemo-resistance and tumor stage. RORC was contributed with increased PD-L1 expression and abnormal signaling in bladder tumor cells. In addition, RORC modulated bladder tumor cell proliferation, chemo-resistance, and glucose metabolism by inhibiting the PD-L1/ITGB6/STAT3 pathway. RORC also enhanced CDDP sensitivity via the mitochondrial apoptosis axis [103].
Generally, integrins have a key role in CDDP resistance via direct activation of PI3K/AKT pathway by FAK/AKT axis. AKT also up regulates the integrins in a positive feedback. Moreover, integrins have indirect roles in CDDP resistance by up regulation of growth factors and subsequent increased activation of PI3K/AKT pathway.
MAPK and Wnt/β-catenin signaling pathways
Integrin protein family has a key role in CDDP response by regulation of MAPK and WNT signaling pathways (Fig. 2). Focal adhesion (FA) complex transfers the modulatory signals and mechanical forces between the ECM and cell [104]. Integrins, focal adhesion kinase (FAK), and Paxillin (PXN) constitute a pivotal part of FA complex. PXN triggers the activation of MAPK/ERK axis to promote CDDP resistance and Bcl-2 expression [105]. Integrin αvβ6 is exclusively expressed on normal epithelium, however it is also significantly over-expressed through tissue repair, morphogenesis, and tumor formation [106]. Integrin αvβ6 directly connects to ERK2 to prevent the cell phosphatase-induced deactivation of ERK2 that up regulates MMP-3 and MMP-9 by phosphorylating Ets-1 [107]. Integrin αvβ6 was associated with CDDP resistance, colony formation, and prognosis in hilar cholangiocarcinoma. Additionally, there was an integrin αvβ6 up regulation in hilar cholangiocarcinoma tissues, which was associated with advanced TNM stage, lymph nodal invasion, and poor differentiation. Moreover, integrin αvβ6 induced cisplatin resistance in cholangiocarcinoma cells via the ERK/MAPK axis [108]. Integrin αV subunit is found in numerous tumor cells and modulates cell-cell and cell-matrix interactions [109, 110]. It affects various cellular mechanisms such as apoptosis, survival, and proliferation [111,112,113]. Chloride intracellular channel 1 (CLIC1) acts as an ion protein channel that modulates apoptosis, cellular cycle, platelet release, neurogenesis, and bone formation [114, 115]. Chloride channels significantly participate in tumor development as it was reported that the involvement of some or potentially all chloride channels is crucial for tumor cell proliferation and metastasis [116]. Accordingly, CLIC1 was up regulated in oral squamous cell carcinoma (OSCC) tissues, which was correlated with tumor size, higher stage, and poor prognosis. CLIC1 knockdown mitigated OSCC cell proliferation and viability while enhancing apoptosis and CDDP response. CLIC1 inhibition diminished E-cadherin expression and incremented the levels of MMP-2, MMP-9, ITGB1, ITGαv, vimentin, and p-ERK. Moreover, an elevated expression of CASP3, CASP9, and p-p38 along with increased apoptosis were seen following CLIC1 inhibition. CLIC1 was contributed with OSCC cell metastasis by promoting MAPK/p38 and ERK signaling pathways through interacting with integrins [117].
Homeobox genes participate in oncogenesis by interacting with various signaling pathways [118, 119]. HOXD3 stimulated drug resistance and stemness in breast tumor cells via the Wnt/β-catenin axis through integrin β3 [120]. FSTL1 is a glycoprotein, which was initially recognized as a TGF-β1-inducible factor and a part of the family of Follistatin-SPARC [121]. However, FSTL1 interactions with signaling pathways extend beyond TGFβ. Multiple studies indicated that it participates in automodulatory feedback loops involving various factors such as IL1β, MMP-2, and BMPs [122]. MiR-137 was involved in the modulation of FSTL1/integrin β3/Wnt/β-catenin pathway. FSTL1 stimulated tumorigenesis by activating the Wnt/β-catenin axis via integrin β3. MiR-137 targeted FSTL1 to inhibit the Wnt/β-catenin that resulted in reduced drug resistance and breast tumor cell stemness [123]. Keratins are a subgroup of epithelial-specific intermediate filaments that modulate cellular adhesion and invasion by stabilizing hemidesmosomes via interacting with plectin/integrins complex [124, 125]. KRT17 promoted the integrin β4 expression. KRT17 regulated the integrin β4 and α6. KRT17 modulated OSCC drug resistance and stemness by regulating the integrin/FAK/Src/ERK/β-catenin axis. MiR-485-5p diminished sphere formation and reduced expression of CSC markers by KRT17 targeting [126]. ITGB4 was up regulated in secretory, classical, and primitive subgroups of lung squamous cell carcinoma (LUSC), which was associated with poor prognosis. ITGB4 targeting inhibited SOX2 expression in SOX2-expressing CSCs while enhancing cisplatin sensitivity. Accordingly, the knockdown of ITGB4 attenuated acetylation of H3K27 in the SOX2 promoter that resulted in SOX2 down regulation [127].
Generally, integrins activate the ERK that directly promotes CDDP resistance. ERK can also promote CDDP resistance by the inhibition of GSK3b that results in WNT signaling activation. Therefore, integrins can induce CDDP resistance by an interaction between the MAPK/ERK and WNT signaling pathways. On the other hand, integrins are also activators of the β-catenin that promotes CDDP resistance by WNT signaling pathway.
DNA repair, apoptosis, and drug efflux
Homologous recombination (HR) and non-homologous end joining (NHEJ) are known as key repair pathways during response to cisplatin-mediated DNA damage [128]. HR acts as a high-fidelity repair axis that relies on a DNA template for the double-strand breaks (DSB) repair and therefore primarily functions during the G2 and S phases of the cellular cycle. In contrast, NHEJ functions without requiring a DNA template which allows it to act in any phase of the cell cycle but makes it more susceptible to errors [129]. BRCA1 as a key component of the HR pathway modulates cell proliferation and DNA damage repair by creating heterodimers with BARD1. Down regulation of BRCA1/BARD1 is correlated with the inhibition of DNA damage repair and enhanced sensitivity to DNA-damaging chemotherapy regimens in various tumors [99, 130, 131]. In addition, PI3K/AKT axis promotes DNA damage repair via up regulating BRCA1 and BARD1 [99, 132]. Integrin α5 regulated CDDP-induced apoptosis by up regulating BARD1 through the FAK/PI3K/AKT axis. Additionally, α5 inhibition sensitized the ESCC cells to CDDP by stimulating apoptosis and diminishing DNA damage repair [133]. Integrin α6β4 is known as a laminin receptor with a notably higher expression in TNBC compared with HER2-amplified or hormone-positive breast tumors [134]. Integrin α6β4 promotes p53 to cause Akt cleavage, p21 over-expression, and apoptosis [135,136,137]. 53BP1 is an important downstream effector of DNA-PK and p53 that can modify cisplatin sensitivity and is used for deciding between NHEJ and HR [138,139,140]. DNA-PK and p53 mutations are significantly involved in integrin α6β4-mediated CDDP sensitivity of TNBC cells. Integrin α6β4 promoted CDDP sensitivity while inhibited HR via modulating p53 and DNA-PK and accumulation of cells in the S phase. Additionally, integrin α6β4 was involved in CDDP sensitivity by stimulating 53BP1 phosphorylation through DNA-PK [141]. Direct interaction of two major elements of the FA complex including ITGB4 and PXN was associated with CDDP resistance in lung tumor cells. There was a cross-talk among molecules that modulate FA complex and EMT as it was shown that EMT-related pathways including TGF-β and Smad were associated with PXN and ITGB4 knockdown. ITGB4 and PXN were involved in the modulation of VDAC1 and USP1 transcriptions, which were contributed with CDDP sensitivity and tumor proliferation. Suppression of ITGB4/PXN or USP1/VDAC1 enhanced the oxygen consumption in mitochondria that resulted in elevated ROS formation and DNA damage. ITGB4/PXN suppression promoted CDDP sensitivity by inhibiting DNA repair processes via USP1 [142].
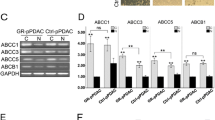
Integrin protein family has a key role in regulation of CDDP mediated apoptosis in tumor cells (Fig. 3). P53 activation is significantly involved in DNA repair, and suppression of p53 aggressive types results in DNA damage-mediated apoptosis [143,144,145]. Integrin β4 suppressed DNA damage-mediated activation of p53, while integrin β4 knockdown enhanced colorectal cancer (CRC) sensitivity to CDDP [146]. Throughout apoptosis-related signaling, CASP-8 and CASP-9 serve as initiator caspases and activate downstream genes such as CASP-3, CASP-6, and CASP-7 that degrade particular substrates including cytoskeletal DNA and proteins, and nuclear laminas to ultimately cause apoptosis [147]. α6-integrin promoted CDDP sensitivity and apoptosis in NCCIT cells via inducing adhesion of tumor cells to laminin and thereby activating apoptotic factors such as CASP-3, CASP-6, and AIF [148]. MiR-302b promoted CDDP response by regulating E2F/YY1/ITGA6 pathway in TNBC cells [149]. Collagens are major parts of the tumor microenvironment that interact with integrins to induce chemo resistance in several malignancies [30, 150,151,152]. Collagen type XI alpha 1 (COL11A1) is expressed mostly in recurrent and chemo-resistant ovarian cancers and also a subgroup of tumor-adjacent cancer associated fibroblasts (CAFs) [153,154,155]. Integrins and DDRs interact to increase integrin binding ability to collagens [156]. COL11A1 suppressed CDDP-induced apoptosis in ovarian tumor cells by promoting apoptosis inhibitor proteins such as BIRC2, BIRC3, and XIAP via discoidin domain receptor 2 (DDR2)-Src-PI3K/Akt-NF-kB axis through α1β1 integrin. COL11A1 induced IAP expression by activating NF-kB via the PI3K/Akt axis [157]. TGFβ1-induced protein (TGFBI) contributes to the binding of integrins to ECM components including fibronectin, collagen, and laminin, which is associated with the activation of cell adhesion, proliferation, and metastasis [158]. TGFBI up regulation was correlated with elevated chemo-sensitivity to several agents. Blocking the binding of TGFBI to αvβ3 integrin in Non-small cell lung cancer (NSCLC) cells reduced the TGFBI pro-apoptotic actions. TGFBI stimulated apoptosis in NSCLC cells via the proteolytic fragments derived from TGFBI. TGFBI-induced apoptosis occurred via the up regulation of caspase-3, caspase-7, and caspase-8 and the attachment of TGFBI-derived proteolytic fragments to αvβ3 integrin [159]. The α2β1-COL1 interaction down regulated ITGB1. There were BCRP, MRP1, and P-gp up regulations following tumor cell therapy with COL1. Additionally, a novel pathway was found in which ABC transporters were activated via ITGB1-mediated cell adhesion to COL1 in breast tumors [160]. PLOD2 acts as a crucial enzyme involved in collagen lysyl hydroxylation [161, 162]. PLOD2 enhances tumor metastasis by inducing Integrin β1 hydroxylation [163]. It also stimulates oral squamous cell carcinoma metastasis by activating Integrin β1 via regulating the IL-6/STAT3 axis [164]. PLOD2 knockdown repressed CD44 and CD133 levels and laryngeal cancer (LC) cell stemness. PLOD2 modulated tumorigenesis and LC cell stemness in cisplatin-resistant nude mice through Integrin β1. In addition, PLOD2 silencing reduced tumor progression and stemness in CDDP-resistant LC cells by suppressing P-gp and MRP1 through Integrin β1 [165].
Generally, integrins reduce CDDP-mediated apoptosis by activation of XIAP following the interaction with DDR2. They also inhibit the p53 to reduce Cytochrome C release from mitochondria that suppresses CDDP-mediated apoptosis in tumor cells. On the other hand, integrins can also promote the CDDP-mediated apoptosis by direct activation of CASP8 and CASP3. Therefore, integrins have dual functions in regulation of CDDP-mediated apoptosis that result in CDDP resistance in ovarian cancer while CDDP sensitivity in lung cancer.
Conclusions
Integrins are involved in drug resistance of various solid tumors through modulation of the tumor cell interactions with interstitial matrix and ECM. Therefore, in the present review we discussed the role of integrin protein family in regulation of CDDP response in tumor cells. It has been shown that integrins mainly induced the CDDP resistance via interaction with PI3K/AKT, MAPK, and WNT signaling pathways. This review paves the way to suggest the integrins as the reliable therapeutic targets to improve CDDP response in tumor cells. However, more clinical trials and animal studies are required to use integrins as the therapeutic targets in cancer patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CAM-DR:
-
Cell adhesion-mediated drug resistance
- CLIC1:
-
Chloride intracellular channel 1
- CDDP:
-
Cisplatin
- CRC:
-
Colorectal cancer
- DDR2:
-
Discoidin domain receptor 2
- DSB:
-
Double-strand breaks
- ESCC:
-
Esophageal squamous-cell carcinomas
- ECM:
-
Extracellular matrix
- FAK:
-
Focal adhesion kinase
- FAK:
-
Focal adhesion kinase
- HR:
-
Homologous recombination
- ITGB1:
-
Integrin β1
- LSCC:
-
Laryngeal squamous cell carcinoma
- LUSC:
-
Lung squamous cell carcinoma
- MMPs:
-
Matrix metalloproteinases
- NACT:
-
Neoadjuvant chemotherapy
- NRP1:
-
Neuropilin-1
- NHEJ:
-
Non-homologous end joining
- OSCC:
-
Oral squamous cell carcinoma
- OC:
-
Ovarian cancer
- PXN:
-
Paxillin
- RORC:
-
Retinoic acid–related orphan receptor C
- TGFBI:
-
TGFβ1-induced protein
- TCA:
-
Tricarboxylic acid cycle
- TNBC:
-
Triple-negative breast cancer
References
Gupta GP, Massagué J. Cancer metastasis: building a framework. Cell. 2006;127(4):679–95.
Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110(6):673–87.
Lu P, Weaver VM, Werb Z. The extracellular matrix: a dynamic niche in cancer progression. J Cell Biol. 2012;196(4):395–406.
Maharati A, Moghbeli M. PI3K/AKT signaling pathway as a critical regulator of epithelial-mesenchymal transition in colorectal tumor cells. Cell Commun Signal. 2023;21(1):201.
Naci D, Vuori K, Aoudjit F. Alpha2beta1 integrin in cancer development and chemoresistance. Semin Cancer Biol. 2015;35:145–53.
Iwamoto DV, Calderwood DA. Regulation of integrin-mediated adhesions. Curr Opin Cell Biol. 2015;36:41–7.
Dedhar S, Hannigan GE. Integrin cytoplasmic interactions and bidirectional transmembrane signalling. Curr Opin Cell Biol. 1996;8(5):657–69.
Hemler ME, Mannion BA, Berditchevski F. Association of TM4SF proteins with integrins: relevance to cancer. Biochim Biophys Acta. 1996;1287(2–3):67–71.
Plath T, Detjen K, Welzel M, von Marschall Z, Murphy D, Schirner M, et al. A novel function for the tumor suppressor p16(INK4a): induction of anoikis via upregulation of the alpha(5)beta(1) fibronectin receptor. J Cell Biol. 2000;150(6):1467–78.
Sawada K, Mitra AK, Radjabi AR, Bhaskar V, Kistner EO, Tretiakova M, et al. Loss of E-cadherin promotes ovarian cancer metastasis via alpha 5-integrin, which is a therapeutic target. Cancer Res. 2008;68(7):2329–39.
Takayama S, Ishii S, Ikeda T, Masamura S, Doi M, Kitajima M. The relationship between bone metastasis from human breast cancer and integrin alpha(v)beta3 expression. Anticancer Res. 2005;25(1a):79–83.
Shibue T, Weinberg RA. Integrin beta1-focal adhesion kinase signaling directs the proliferation of metastatic cancer cells disseminated in the lungs. Proc Natl Acad Sci U S A. 2009;106(25):10290–5.
Holzmann B, Gosslar U, Bittner M. Alpha 4 integrins and tumor metastasis. Curr Top Microbiol Immunol. 1998;231:125–41.
Bianchi-Smiraglia A, Paesante S, Bakin AV. Integrin β5 contributes to the tumorigenic potential of breast cancer cells through the Src-FAK and MEK-ERK signaling pathways. Oncogene. 2013;32(25):3049–58.
Hou S, Isaji T, Hang Q, Im S, Fukuda T, Gu J. Distinct effects of β1 integrin on cell proliferation and cellular signaling in MDA-MB-231 breast cancer cells. Sci Rep. 2016;6(1):18430.
Li W, Liu Z, Zhao C, Zhai L. Binding of MMP-9-degraded fibronectin to β6 integrin promotes invasion via the FAK-Src-related Erk1/2 and PI3K/Akt/Smad-1/5/8 pathways in breast cancer. Oncol Rep. 2015;34(3):1345–52.
De P, Carlson JH, Wu H, Marcus A, Leyland-Jones B, Dey N. Wnt-beta-catenin pathway signals metastasis-associated tumor cell phenotypes in triple negative breast cancers. Oncotarget. 2016;7(28):43124.
Dzamitika S, Salerno M, Pereira-Maia E, Le Moyec L, Garnier-Suillerot A. Preferential energy- and potential-dependent accumulation of cisplatin-gutathione complexes in human cancer cell lines (GLC4 and K562): a likely role of mitochondria. J Bioenerg Biomembr. 2006;38(1):11–21.
Xu EY, Perlina A, Vu H, Troth SP, Brennan RJ, Aslamkhan AG, et al. Integrated pathway analysis of rat urine metabolic profiles and kidney transcriptomic profiles to elucidate the systems toxicology of model nephrotoxicants. Chem Res Toxicol. 2008;21(8):1548–61.
Alborzinia H, Can S, Holenya P, Scholl C, Lederer E, Kitanovic I, et al. Real-time monitoring of cisplatin-induced cell death. PLoS ONE. 2011;6(5):e19714.
Maharati A, Moghbeli M. Forkhead box proteins as the critical regulators of cisplatin response in tumor cells. Eur J Pharmacol. 2023;956:175937.
Moghbeli M. MicroRNAs as the pivotal regulators of cisplatin resistance in osteosarcoma. Pathol Res Pract. 2023;249:154743.
Brozovic A, Ambriovic-Ristov A, Osmak M. The relationship between cisplatin-induced reactive oxygen species, glutathione, and BCL-2 and resistance to cisplatin. Crit Rev Toxicol. 2010;40(4):347–59.
Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014;740:364–78.
Zangouei AS, Rahimi HR, Mojarrad M, Moghbeli M. Non coding RNAs as the critical factors in chemo resistance of bladder tumor cells. Diagn Pathol. 2020;15(1):136.
Zangouei AS, Moghbeli M. MicroRNAs as the critical regulators of cisplatin resistance in gastric tumor cells. Genes Environ. 2021;43(1):21.
Zangouei AS, Alimardani M, Moghbeli M. MicroRNAs as the critical regulators of doxorubicin resistance in breast tumor cells. Cancer Cell Int. 2021;21(1):213.
Navaei ZN, Khalili-Tanha G, Zangouei AS, Abbaszadegan MR, Moghbeli M. PI3K/AKT signaling pathway as a critical regulator of cisplatin response in tumor cells. Oncol Res. 2021;29(4):235–50.
Moghbeli M. MicroRNAs as the critical regulators of cisplatin resistance in ovarian cancer cells. J Ovarian Res. 2021;14(1):127.
Aoudjit F, Vuori K. Integrin signaling inhibits paclitaxel-induced apoptosis in breast cancer cells. Oncogene. 2001;20(36):4995–5004.
Uhm JH, Dooley NP, Kyritsis AP, Rao JS, Gladson CL. Vitronectin, a glioma-derived extracellular matrix protein, protects tumor cells from apoptotic death. Clin Cancer Res. 1999;5(6):1587–94.
Sethi T, Rintoul RC, Moore SM, MacKinnon AC, Salter D, Choo C, et al. Extracellular matrix proteins protect small cell lung cancer cells against apoptosis: a mechanism for small cell lung cancer growth and drug resistance in vivo. Nat Med. 1999;5(6):662–8.
Matsunaga T, Fukai F, Miura S, Nakane Y, Owaki T, Kodama H, et al. Combination therapy of an anticancer drug with the FNIII14 peptide of fibronectin effectively overcomes cell adhesion-mediated drug resistance of acute myelogenous leukemia. Leukemia. 2008;22(2):353–60.
Taylor ST, Hickman JA, Dive C. Epigenetic determinants of resistance to etoposide regulation of Bcl-X(L) and Bax by tumor microenvironmental factors. J Natl Cancer Inst. 2000;92(1):18–23.
Mudry RE, Fortney JE, York T, Hall BM, Gibson LF. Stromal cells regulate survival of B-lineage leukemic cells during chemotherapy. Blood. 2000;96(5):1926–32.
Meads MB, Gatenby RA, Dalton WS. Environment-mediated drug resistance: a major contributor to minimal residual disease. Nat Rev Cancer. 2009;9(9):665–74.
Lv Z, Yang Y, Yang C. Integrin α7 correlates with worse clinical features and prognosis, and its knockdown inhibits cell proliferation and stemness in tongue squamous cell carcinoma. Int J Oncol. 2020;56(1):69–84.
Cui Y, Wu F, Tian D, Wang T, Lu T, Huang X, et al. miR-199a-3p enhances cisplatin sensitivity of ovarian cancer cells by targeting ITGB8. Oncol Rep. 2018;39(4):1649–57.
Hodkinson PS, Elliott T, Wong WS, Rintoul RC, Mackinnon AC, Haslett C, et al. ECM overrides DNA damage-induced cell cycle arrest and apoptosis in small-cell lung cancer cells through beta1 integrin-dependent activation of PI3-kinase. Cell Death Differ. 2006;13(10):1776–88.
Morozevich GE, Kozlova NI, Preobrazhenskaya ME, Ushakova NA, Eltsov IA, Shtil AA, et al. The role of beta1 integrin subfamily in anchorage-dependent apoptosis of breast carcinoma cells differing in multidrug resistance. Biochem (Mosc). 2006;71(5):489–95.
Aksorn N, Chanvorachote P. Integrin as a molecular target for anti-cancer approaches in lung cancer. Anticancer Res. 2019;39(2):541–8.
Desgrosellier JS, Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer. 2010;10(1):9–22.
Janiszewska M, Primi MC, Izard T. Cell adhesion in cancer: beyond the migration of single cells. J Biol Chem. 2020;295(8):2495–505.
Li M, Wang Y, Li M, Wu X, Setrerrahmane S, Xu H. Integrins as attractive targets for cancer therapeutics. Acta Pharm Sinica B. 2021;11(9):2726–37.
Kim MY, Cho WD, Hong KP, Choi da B, Hong JW, Kim S, et al. Novel monoclonal antibody against beta 1 integrin enhances cisplatin efficacy in human lung adenocarcinoma cells. J Biomed Res. 2016;30(3):217–24.
Parri M, Chiarugi P. Rac and rho GTPases in cancer cell motility control. Cell Commun Signal. 2010;8:23.
O’Connor K, Chen M. Dynamic functions of RhoA in tumor cell migration and invasion. Small GTPases. 2013;4(3):141–7.
Spiering D, Hodgson L. Dynamics of the rho-family small GTPases in actin regulation and motility. Cell Adh Migr. 2011;5(2):170–80.
Burridge K, Chrzanowska-Wodnicka M. Focal adhesions, contractility, and signaling. Annu Rev Cell Dev Biol. 1996;12:463–518.
Maiuthed A, Chanvorachote P. Cisplatin at sub-toxic levels mediates integrin switch in lung cancer cells. Anticancer Res. 2014;34(12):7111–7.
Zhao XK, Cheng Y, Liang Cheng M, Yu L, Mu M, Li H, et al. Focal adhesion kinase regulates Fibroblast Migration via Integrin beta-1 and plays a Central Role in Fibrosis. Sci Rep. 2016;6:19276.
Tai YL, Chen LC, Shen TL. Emerging roles of focal adhesion kinase in cancer. Biomed Res Int. 2015;2015:690690.
Casar B, Rimann I, Kato H, Shattil SJ, Quigley JP, Deryugina EI. In vivo cleaved CDCP1 promotes early tumor dissemination via complexing with activated β1 integrin and induction of FAK/PI3K/Akt motility signaling. Oncogene. 2014;33(2):255–68.
Kanteti R, Batra SK, Lennon FE, Salgia R. FAK and paxillin, two potential targets in pancreatic cancer. Oncotarget. 2016;7(21):31586–601.
Tian T, Li CL, Fu X, Wang SH, Lu J, Guo H, et al. β1 integrin-mediated multicellular resistance in hepatocellular carcinoma through activation of the FAK/Akt pathway. J Int Med Res. 2018;46(4):1311–25.
Yin HL, Wu CC, Lin CH, Chai CY, Hou MF, Chang SJ et al. β1 integrin as a prognostic and predictive marker in Triple-negative breast Cancer. Int J Mol Sci. 2016;17(9).
Xu Z, Zou L, Ma G, Wu X, Huang F, Feng T, et al. Integrin β1 is a critical effector in promoting metastasis and chemo-resistance of esophageal squamous cell carcinoma. Am J Cancer Res. 2017;7(3):531–42.
Gan L, Meng J, Xu M, Liu M, Qi Y, Tan C, et al. Extracellular matrix protein 1 promotes cell metastasis and glucose metabolism by inducing integrin β4/FAK/SOX2/HIF-1α signaling pathway in gastric cancer. Oncogene. 2018;37(6):744–55.
Gómez-Contreras P, Ramiro-Díaz JM, Sierra A, Stipp C, Domann FE, Weigel RJ, et al. Extracellular matrix 1 (ECM1) regulates the actin cytoskeletal architecture of aggressive breast cancer cells in part via S100A4 and rho-family GTPases. Clin Exp Metastasis. 2017;34(1):37–49.
Yin H, Wang J, Li H, Yu Y, Wang X, Lu L, et al. Extracellular matrix protein-1 secretory isoform promotes ovarian cancer through increasing alternative mRNA splicing and stemness. Nat Commun. 2021;12(1):4230.
Lau SK, Shields DJ, Murphy EA, Desgrosellier JS, Anand S, Huang M, et al. EGFR-mediated carcinoma cell metastasis mediated by integrin αvβ5 depends on activation of c-Src and cleavage of MUC1. PLoS ONE. 2012;7(5):e36753.
Bianchi A, Gervasi ME, Bakin A. Role of β5-integrin in epithelial-mesenchymal transition in response to TGF-β. Cell Cycle. 2010;9(8):1647–59.
Wang S, Xie J, Li J, Liu F, Wu X, Wang Z. Cisplatin suppresses the growth and proliferation of breast and cervical cancer cell lines by inhibiting integrin β5-mediated glycolysis. Am J Cancer Res. 2016;6(5):1108–17.
Magnussen A, Kasman IM, Norberg S, Baluk P, Murray R, McDonald DM. Rapid access of antibodies to alpha5beta1 integrin overexpressed on the luminal surface of tumor blood vessels. Cancer Res. 2005;65(7):2712–21.
Kim S, Bell K, Mousa SA, Varner JA. Regulation of angiogenesis in vivo by ligation of integrin alpha5beta1 with the central cell-binding domain of fibronectin. Am J Pathol. 2000;156(4):1345–62.
Sil H, Sen T, Chatterjee A. Fibronectin-integrin (alpha5beta1) modulates migration and invasion of murine melanoma cell line B16F10 by involving MMP-9. Oncol Res. 2011;19(7):335–48.
Kiwanuka E, Andersson L, Caterson EJ, Junker JP, Gerdin B, Eriksson E. CCN2 promotes keratinocyte adhesion and migration via integrin α5β1. Exp Cell Res. 2013;319(19):2938–46.
Kesanakurti D, Chetty C, Dinh DH, Gujrati M, Rao JS. Role of MMP-2 in the regulation of IL-6/Stat3 survival signaling via interaction with α5β1 integrin in glioma. Oncogene. 2013;32(3):327–40.
Paul NR, Allen JL, Chapman A, Morlan-Mairal M, Zindy E, Jacquemet G, et al. α5β1 integrin recycling promotes Arp2/3-independent cancer cell invasion via the formin FHOD3. J Cell Biol. 2015;210(6):1013–31.
Damiano JS, Hazlehurst LA, Dalton WS. Cell adhesion-mediated drug resistance (CAM-DR) protects the K562 chronic myelogenous leukemia cell line from apoptosis induced by BCR/ABL inhibition, cytotoxic drugs, and gamma-irradiation. Leukemia. 2001;15(8):1232–9.
Miroshnikova YA, Rozenberg GI, Cassereau L, Pickup M, Mouw JK, Ou G, et al. α5β1-Integrin promotes tension-dependent mammary epithelial cell invasion by engaging the fibronectin synergy site. Mol Biol Cell. 2017;28(22):2958–77.
Xie YH, Ran LQ, Wu ZY, Sun C, Xu XE, Zou HY, et al. Role of integrin β1 in the progression and chemo-resistance of esophageal squamous cell carcinoma. J Cancer. 2022;13(7):2074–85.
Blanchard H, Bum-Erdene K, Bohari MH, Yu X. Galectin-1 inhibitors and their potential therapeutic applications: a patent review. Expert Opin Ther Pat. 2016;26(5):537–54.
Su YL, Luo HL, Huang CC, Liu TT, Huang EY, Sung MT et al. Galectin-1 overexpression activates the FAK/PI3K/AKT/mTOR pathway and is correlated with Upper urinary urothelial carcinoma progression and survival. Cells. 2020;9(4).
Zhu H, Chen A, Li S, Tao X, Sheng B, Chetry M et al. Predictive role of galectin-1 and integrin α5β1 in cisplatin-based neoadjuvant chemotherapy of bulky squamous cervical cancer. Biosci Rep. 2017;37(5).
Narita M, Young AR, Arakawa S, Samarajiwa SA, Nakashima T, Yoshida S, et al. Spatial coupling of mTOR and autophagy augments secretory phenotypes. Science. 2011;332(6032):966–70.
Liu GY, Sabatini DM. mTOR at the nexus of nutrition, growth, ageing and disease. Nat Rev Mol Cell Biol. 2020;21(4):183–203.
Maharati A, Moghbeli M. Long non-coding RNAs as the critical regulators of PI3K/AKT, TGF-beta, and MAPK signaling pathways during breast tumor progression. J Transl Med. 2023;21(1):556.
Zhu F, Dai SN, Xu DL, Hou CQ, Liu TT, Chen QY, et al. EFNB2 facilitates cell proliferation, migration, and invasion in pancreatic ductal adenocarcinoma via the p53/p21 pathway and EMT. Biomed Pharmacother. 2020;125:109972.
Krusche B, Ottone C, Clements MP, Johnstone ER, Goetsch K, Lieven H et al. EphrinB2 drives perivascular invasion and proliferation of glioblastoma stem-like cells. Elife. 2016;5.
Li D, Sun A, Zhang L, Ding Z, Yi F, Yang X, et al. Elevated ITGA5 facilitates hyperactivated mTORC1-mediated progression of laryngeal squamous cell carcinoma via upregulation of EFNB2. Theranostics. 2022;12(17):7431–49.
Geretti E, Shimizu A, Klagsbrun M. Neuropilin structure governs VEGF and semaphorin binding and regulates angiogenesis. Angiogenesis. 2008;11(1):31–9.
Larrivée B, Freitas C, Suchting S, Brunet I, Eichmann A. Guidance of vascular development: lessons from the nervous system. Circ Res. 2009;104(4):428–41.
Pellet-Many C, Frankel P, Jia H, Zachary I. Neuropilins: structure, function and role in disease. Biochem J. 2008;411(2):211–26.
Kolodkin AL, Levengood DV, Rowe EG, Tai YT, Giger RJ, Ginty DD. Neuropilin is a semaphorin III receptor. Cell. 1997;90(4):753–62.
Takahashi T, Fournier A, Nakamura F, Wang LH, Murakami Y, Kalb RG, et al. Plexin-neuropilin-1 complexes form functional semaphorin-3A receptors. Cell. 1999;99(1):59–69.
Jia H, Cheng L, Tickner M, Bagherzadeh A, Selwood D, Zachary I. Neuropilin-1 antagonism in human carcinoma cells inhibits migration and enhances chemosensitivity. Br J Cancer. 2010;102(3):541–52.
Stallcup WB. The NG2 proteoglycan: past insights and future prospects. J Neurocytol. 2002;31(6–7):423–35.
Grako KA, Ochiya T, Barritt D, Nishiyama A, Stallcup WB. PDGF (alpha)-receptor is unresponsive to PDGF-AA in aortic smooth muscle cells from the NG2 knockout mouse. J Cell Sci. 1999;112(Pt 6):905–15.
Goretzki L, Burg MA, Grako KA, Stallcup WB. High-affinity binding of basic fibroblast growth factor and platelet-derived growth factor-AA to the core protein of the NG2 proteoglycan. J Biol Chem. 1999;274(24):16831–7.
Makagiansar IT, Williams S, Mustelin T, Stallcup WB. Differential phosphorylation of NG2 proteoglycan by ERK and PKCalpha helps balance cell proliferation and migration. J Cell Biol. 2007;178(1):155–65.
Makagiansar IT, Williams S, Dahlin-Huppe K, Fukushi J, Mustelin T, Stallcup WB. Phosphorylation of NG2 proteoglycan by protein kinase C-alpha regulates polarized membrane distribution and cell motility. J Biol Chem. 2004;279(53):55262–70.
Chekenya M, Krakstad C, Svendsen A, Netland IA, Staalesen V, Tysnes BB, et al. The progenitor cell marker NG2/MPG promotes chemoresistance by activation of integrin-dependent PI3K/Akt signaling. Oncogene. 2008;27(39):5182–94.
Nieman KM, Kenny HA, Penicka CV, Ladanyi A, Buell-Gutbrod R, Zillhardt MR, et al. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat Med. 2011;17(11):1498–503.
Wagner GF, Guiraudon CC, Milliken C, Copp DH. Immunological and biological evidence for a stanniocalcin-like hormone in human kidney. Proc Natl Acad Sci U S A. 1995;92(6):1871–5.
Jiang WQ, Chang AC, Satoh M, Furuichi Y, Tam PP, Reddel RR. The distribution of stanniocalcin 1 protein in fetal mouse tissues suggests a role in bone and muscle development. J Endocrinol. 2000;165(2):457–66.
Kanellis J, Bick R, Garcia G, Truong L, Tsao CC, Etemadmoghadam D, et al. Stanniocalcin-1, an inhibitor of macrophage chemotaxis and chemokinesis. Am J Physiol Ren Physiol. 2004;286(2):F356–62.
Chan KK, Leung CO, Wong CC, Ho DW, Chok KS, Lai CL, et al. Secretory stanniocalcin 1 promotes metastasis of hepatocellular carcinoma through activation of JNK signaling pathway. Cancer Lett. 2017;403:330–8.
Li Y, He ZC, Zhang XN, Liu Q, Chen C, Zhu Z, et al. Stanniocalcin-1 augments stem-like traits of glioblastoma cells through binding and activating NOTCH1. Cancer Lett. 2018;416:66–74.
Brantley KD, Kjærsgaard A, Cronin-Fenton D, Yacoub R, Nielsen AS, Lauridsen KL, et al. Stanniocalcin expression as a predictor of late breast Cancer recurrence. Cancer Epidemiol Biomarkers Prev. 2018;27(6):653–9.
Lin F, Li X, Wang X, Sun H, Wang Z, Wang X. Stanniocalcin 1 promotes metastasis, lipid metabolism and cisplatin chemoresistance via the FOXC2/ITGB6 signaling axis in ovarian cancer. J Exp Clin Cancer Res. 2022;41(1):129.
Benoit G, Cooney A, Giguere V, Ingraham H, Lazar M, Muscat G, et al. International Union of Pharmacology. LXVI. Orphan nuclear receptors. Pharmacol Rev. 2006;58(4):798–836.
Cao D, Qi Z, Pang Y, Li H, Xie H, Wu J, et al. Retinoic acid-related orphan receptor C regulates proliferation, Glycolysis, and Chemoresistance via the PD-L1/ITGB6/STAT3 Signaling Axis in bladder Cancer. Cancer Res. 2019;79(10):2604–18.
Chen CS, Alonso JL, Ostuni E, Whitesides GM, Ingber DE. Cell shape provides global control of focal adhesion assembly. Biochem Biophys Res Commun. 2003;307(2):355–61.
Wu DW, Wu TC, Wu JY, Cheng YW, Chen YC, Lee MC, et al. Phosphorylation of paxillin confers cisplatin resistance in non-small cell lung cancer via activating ERK-mediated Bcl-2 expression. Oncogene. 2014;33(35):4385–95.
Bandyopadhyay A, Raghavan S. Defining the role of integrin alphavbeta6 in cancer. Curr Drug Targets. 2009;10(7):645–52.
Peng C, Gao H, Niu Z, Wang B, Tan Z, Niu W, et al. Integrin αvβ6 and transcriptional factor Ets-1 act as prognostic indicators in colorectal cancer. Cell Biosci. 2014;4(1):53.
Sun Q, Dong X, Shang Y, Sun F, Niu J, Li F. Integrin αvβ6 predicts poor prognosis and promotes resistance to cisplatin in hilar cholangiocarcinoma. Pathol Res Pract. 2020;216(7):153022.
Sakamoto Y, Ogita H, Komura H, Takai Y. Involvement of nectin in inactivation of integrin alpha(v)beta(3) after the establishment of cell-cell adhesion. J Biol Chem. 2008;283(1):496–505.
Sakamoto Y, Ogita H, Hirota T, Kawakatsu T, Fukuyama T, Yasumi M, et al. Interaction of integrin alpha(v)beta3 with nectin. Implication in cross-talk between cell-matrix and cell-cell junctions. J Biol Chem. 2006;281(28):19631–44.
Voland C, Bord A, Péleraux A, Pénarier G, Carrière D, Galiègue S, et al. Repression of cell cycle-related proteins by oxaliplatin but not cisplatin in human colon cancer cells. Mol Cancer Ther. 2006;5(9):2149–57.
Howells LM, Mitra A, Manson MM. Comparison of oxaliplatin- and curcumin-mediated antiproliferative effects in colorectal cell lines. Int J Cancer. 2007;121(1):175–83.
Vellon L, Menendez JA, Lupu R. A bidirectional alpha(v)beta(3) integrin-ERK1/ERK2 MAPK connection regulates the proliferation of breast cancer cells. Mol Carcinog. 2006;45(10):795–804.
Novarino G, Fabrizi C, Tonini R, Denti MA, Malchiodi-Albedi F, Lauro GM, et al. Involvement of the intracellular ion channel CLIC1 in microglia-mediated beta-amyloid-induced neurotoxicity. J Neurosci. 2004;24(23):5322–30.
Saeki K, Yasugi E, Okuma E, Breit SN, Nakamura M, Toda T, et al. Proteomic analysis on insulin signaling in human hematopoietic cells: identification of CLIC1 and SRp20 as novel downstream effectors of insulin. Am J Physiol Endocrinol Metab. 2005;289(3):E419–28.
Peretti M, Angelini M, Savalli N, Florio T, Yuspa SH, Mazzanti M. Chloride channels in cancer: focus on chloride intracellular channel 1 and 4 (CLIC1 AND CLIC4) proteins in tumor development and as novel therapeutic targets. Biochim Biophys Acta. 2015;1848(10 Pt B):2523–31.
Feng J, Xu J, Xu Y, Xiong J, Xiao T, Jiang C, et al. CLIC1 promotes the progression of oral squamous cell carcinoma via integrins/ERK pathways. Am J Transl Res. 2019;11(2):557–71.
Bhatlekar S, Fields JZ, Boman BM. HOX genes and their role in the development of human cancers. J Mol Med (Berl). 2014;92(8):811–23.
Hur H, Lee JY, Yun HJ, Park BW, Kim MH. Analysis of HOX gene expression patterns in human breast cancer. Mol Biotechnol. 2014;56(1):64–71.
Zhang Y, Zhang Q, Cao Z, Huang Y, Cheng S, Pang D. HOXD3 plays a critical role in breast Cancer Stemness and Drug Resistance. Cell Physiol Biochem. 2018;46(4):1737–47.
Shibanuma M, Mashimo J, Mita A, Kuroki T, Nose K. Cloning from a mouse osteoblastic cell line of a set of transforming-growth-factor-beta 1-regulated genes, one of which seems to encode a follistatin-related polypeptide. Eur J Biochem. 1993;217(1):13–9.
Sylva M, Moorman AF, van den Hoff MJ. Follistatin-like 1 in vertebrate development. Birth Defects Res C Embryo Today. 2013;99(1):61–9.
Cheng S, Huang Y, Lou C, He Y, Zhang Y, Zhang Q. FSTL1 enhances chemoresistance and maintains stemness in breast cancer cells via integrin β3/Wnt signaling under miR-137 regulation. Cancer Biol Ther. 2019;20(3):328–37.
de Pereda JM, Lillo MP, Sonnenberg A. Structural basis of the interaction between integrin alpha6beta4 and plectin at the hemidesmosomes. Embo j. 2009;28(8):1180–90.
Schweizer J, Bowden PE, Coulombe PA, Langbein L, Lane EB, Magin TM, et al. New consensus nomenclature for mammalian keratins. J Cell Biol. 2006;174(2):169–74.
Jang TH, Huang WC, Tung SL, Lin SC, Chen PM, Cho CY, et al. MicroRNA-485-5p targets keratin 17 to regulate oral cancer stemness and chemoresistance via the integrin/FAK/Src/ERK/β-catenin pathway. J Biomed Sci. 2022;29(1):42.
Guo L, Mohanty A, Singhal S, Srivastava S, Nam A, Warden C, et al. Targeting ITGB4/SOX2-driven lung cancer stem cells using proteasome inhibitors. iScience. 2023;26(8):107302.
Galluzzi L, Senovilla L, Vitale I, Michels J, Martins I, Kepp O, et al. Molecular mechanisms of cisplatin resistance. Oncogene. 2012;31(15):1869–83.
Her J, Bunting SF. How cells ensure correct repair of DNA double-strand breaks. J Biol Chem. 2018;293(27):10502–11.
Chetrit A, Hirsh-Yechezkel G, Ben-David Y, Lubin F, Friedman E, Sadetzki S. Effect of BRCA1/2 mutations on long-term survival of patients with invasive ovarian cancer: the national Israeli study of ovarian cancer. J Clin Oncol. 2008;26(1):20–5.
Dai CH, Li J, Chen P, Jiang HG, Wu M, Chen YC. RNA interferences targeting the Fanconi anemia/BRCA pathway upstream genes reverse cisplatin resistance in drug-resistant lung cancer cells. J Biomed Sci. 2015;22(1):77.
Ibrahim YH, García-García C, Serra V, He L, Torres-Lockhart K, Prat A, et al. PI3K inhibition impairs BRCA1/2 expression and sensitizes BRCA-proficient triple-negative breast cancer to PARP inhibition. Cancer Discov. 2012;2(11):1036–47.
Hou S, Jin W, Xiao W, Deng B, Wu D, Zhi J, et al. Integrin α5 promotes migration and cisplatin resistance in esophageal squamous cell carcinoma cells. Am J Cancer Res. 2019;9(12):2774–88.
Lu S, Simin K, Khan A, Mercurio AM. Analysis of integrin beta4 expression in human breast cancer: association with basal-like tumors and prognostic significance. Clin Cancer Res. 2008;14(4):1050–8.
Bachelder RE, Marchetti A, Falcioni R, Soddu S, Mercurio AM. Activation of p53 function in carcinoma cells by the alpha6beta4 integrin. J Biol Chem. 1999;274(29):20733–7.
Bachelder RE, Ribick MJ, Marchetti A, Falcioni R, Soddu S, Davis KR, et al. p53 inhibits α6β4 integrin survival signaling by promoting the caspase 3–dependent cleavage of AKT/PKB. J Cell Biol. 1999;147(5):1063–72.
Clarke AS, Lotz MM, Chao C, Mercurio AM. Activation of the p21 pathway of growth arrest and apoptosis by the beta 4 integrin cytoplasmic domain. J Biol Chem. 1995;270(39):22673–6.
Panier S, Boulton SJ. Double-strand break repair: 53BP1 comes into focus. Nat Rev Mol Cell Biol. 2014;15(1):7–18.
Zimmermann M, de Lange T. 53BP1: pro choice in DNA repair. Trends Cell Biol. 2014;24(2):108–17.
Bunting SF, Callén E, Wong N, Chen HT, Polato F, Gunn A, et al. 53BP1 inhibits homologous recombination in Brca1-deficient cells by blocking resection of DNA breaks. Cell. 2010;141(2):243–54.
Chen M, Marrs B, Qi L, Knifley T, Weiss HL, D’Orazio JA, et al. Integrin α6β4 signals through DNA damage response pathway to sensitize breast cancer cells to cisplatin. Front Oncol. 2022;12:1043538.
Mohanty A, Nam A, Pozhitkov A, Yang L, Srivastava S, Nathan A, et al. A non-genetic mechanism involving the integrin β4/Paxillin Axis contributes to Chemoresistance in Lung Cancer. iScience. 2020;23(9):101496.
Tran TQ, Lowman XH, Reid MA, Mendez-Dorantes C, Pan M, Yang Y, et al. Tumor-associated mutant p53 promotes cancer cell survival upon glutamine deprivation through p21 induction. Oncogene. 2017;36(14):1991–2001.
He J, Liang X, Luo F, Chen X, Xu X, Wang F, et al. P53 is involved in a three-Dimensional Architecture-mediated decrease in Chemosensitivity in Colon cancer. J Cancer. 2016;7(8):900–9.
Yogev O, Barker K, Sikka A, Almeida GS, Hallsworth A, Smith LM, et al. p53 loss in MYC-Driven neuroblastoma leads to metabolic adaptations supporting Radioresistance. Cancer Res. 2016;76(10):3025–35.
Wu J, Zhao R, Lin J, Liu B. Integrin β4 reduces DNA damage–induced p53 activation in colorectal cancer. Oncol Rep. 2018;40(4):2183–92.
Herr I, Debatin KM. Cellular stress response and apoptosis in cancer therapy. Blood. 2001;98(9):2603–14.
Andjilani M, Droz JP, Benahmed M, Tabone E. Alpha6 integrin subunit mediates laminin enhancement of cisplatin-induced apoptosis in testicular tumor germ cells. Int J Cancer. 2005;117(1):68–81.
Cataldo A, Romero-Cordoba S, Plantamura I, Cosentino G, Hidalgo-Miranda A, Tagliabue E et al. MiR-302b as a Combinatorial Therapeutic Approach to Improve Cisplatin Chemotherapy Efficacy in Human Triple-negative breast Cancer. Cancers (Basel). 2020;12(8).
Cohen E, Tendler T, Lu H, Hansen CK, Kertsman J, Barrios J, et al. Collagen I provides a survival advantage to MD-1483 head and neck squamous cell carcinoma cells through phosphoinositol 3-kinase signaling. Anticancer Res. 2013;33(2):379–86.
Sherman-Baust CA, Weeraratna AT, Rangel LB, Pizer ES, Cho KR, Schwartz DR, et al. Remodeling of the extracellular matrix through overexpression of collagen VI contributes to cisplatin resistance in ovarian cancer cells. Cancer Cell. 2003;3(4):377–86.
Egeblad M, Rasch MG, Weaver VM. Dynamic interplay between the collagen scaffold and tumor evolution. Curr Opin Cell Biol. 2010;22(5):697–706.
Cheon DJ, Tong Y, Sim MS, Dering J, Berel D, Cui X, et al. A collagen-remodeling gene signature regulated by TGF-β signaling is associated with metastasis and poor survival in serous ovarian cancer. Clin Cancer Res. 2014;20(3):711–23.
Jia D, Liu Z, Deng N, Tan TZ, Huang RY, Taylor-Harding B, et al. A COL11A1-correlated pan-cancer gene signature of activated fibroblasts for the prioritization of therapeutic targets. Cancer Lett. 2016;382(2):203–14.
García-Pravia C, Galván JA, Gutiérrez-Corral N, Solar-García L, García-Pérez E, García-Ocaña M, et al. Overexpression of COL11A1 by cancer-associated fibroblasts: clinical relevance of a stromal marker in pancreatic cancer. PLoS ONE. 2013;8(10):e78327.
Xu H, Bihan D, Chang F, Huang PH, Farndale RW, Leitinger B. Discoidin domain receptors promote α1β1- and α2β1-integrin mediated cell adhesion to collagen by enhancing integrin activation. PLoS ONE. 2012;7(12):e52209.
Rada M, Nallanthighal S, Cha J, Ryan K, Sage J, Eldred C, et al. Inhibitor of apoptosis proteins (IAPs) mediate collagen type XI alpha 1-driven cisplatin resistance in ovarian cancer. Oncogene. 2018;37(35):4809–20.
Kim JE, Kim SJ, Lee BH, Park RW, Kim KS, Kim IS. Identification of motifs for cell adhesion within the repeated domains of transforming growth factor-beta-induced gene, betaig-h3. J Biol Chem. 2000;275(40):30907–15.
Irigoyen M, Pajares MJ, Agorreta J, Ponz-Sarvisé M, Salvo E, Lozano MD, et al. TGFBI expression is associated with a better response to chemotherapy in NSCLC. Mol Cancer. 2010;9:130.
Baltes F, Pfeifer V, Silbermann K, Caspers J, von Wantoch K, Schlesinger M, et al. β(1)-Integrin binding to collagen type 1 transmits breast cancer cells into chemoresistance by activating ABC efflux transporters. Biochim Biophys Acta Mol Cell Res. 2020;1867(5):118663.
Cheriyamundath S, Kumar A, Gavert N, Brabletz T, Ben-Ze’ev A. The collagen-modifying enzyme PLOD2 is Induced and required during L1-Mediated Colon cancer progression. Int J Mol Sci. 2021;22(7).
Sun Y, Wang S, Zhang X, Wu Z, Li Z, Ding Z et al. Identification and validation of PLOD2 as an adverse prognostic biomarker for oral squamous cell carcinoma. Biomolecules. 2021;11(12).
Ueki Y, Saito K, Iioka H, Sakamoto I, Kanda Y, Sakaguchi M, et al. PLOD2 is essential to functional activation of integrin β1 for Invasion/Metastasis in Head and Neck squamous cell carcinomas. iScience. 2020;23(2):100850.
Saito K, Mitsui A, Sumardika IW, Yokoyama Y, Sakaguchi M, Kondo E. PLOD2-driven IL-6/STAT3 signaling promotes the invasion and metastasis of oral squamous cell carcinoma via activation of integrin β1. Int J Oncol. 2021;58(6).
Song M, Liu X, Li T, Zhang Y, Zhao X, Sun W, et al. Silencing PLOD2 attenuates cancer stem cell-like characteristics and cisplatin-resistant through integrin β1 in laryngeal cancer. Transl Oncol. 2022;22:101460.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
ANS was involved in drafting. MM designed, revised, and supervised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nasimi Shad, A., Moghbeli, M. Integrins as the pivotal regulators of cisplatin response in tumor cells. Cell Commun Signal 22, 265 (2024). https://doi.org/10.1186/s12964-024-01648-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12964-024-01648-0