Abstract
Background
Health Complex Model was implemented to provide primary health care services in urban, especially in slum areas. As a pilot at a provincial level, Chamran Health Complex offers healthcare for more than 57,000 residents of Tabriz. Despite the necessity of cost information in healthcare decision-making, there was limited knowledge about the unit cost of services. This study aims to analyze the cost and efficiency of health centers.
Methods
Activity-Based Costing method with direct and step-down allocation methods was adopted. We estimated unit costs in a hypothetical scenario according to national standards to quantify the gap between current and standard practice. Input-oriented Data Envelopment Analysis was administered to measure the efficiency of health centers.
Results
The total cost of the complex was $2,841,897, of which 67% ($1910373) and 33% ($931523) were accounted for direct and indirect costs, respectively. The vaccination center had the lowest ($9), and the occupational health center had the highest average unit cost ($76). The average technical efficiency of the health centers was 0.519, where the HC1 and HC3 showed the best performance.
Conclusion
There is remarkable variability in service costs across health centers, which must be addressed in performance management and contracting practices. Although we found a gap between current and standard practice in terms of staff and facilities according to national standards, Chamran Health Complex has an untouched capacity that can be utilized with better planning and without incurring additional costs. It raises the need for revising national standards by the Iran Ministry of Health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The increasing cost of healthcare is one of the most important reasons for inadequate access to essential health services [1]. Health systems worldwide have tried to deal with the issue by prioritizing primary healthcare services. Given the challenges regard to the quality and efficiency of health care [2], the Iranian health system has attempted to address the issue by initiating a series of health sector reforms, including the pilot of the Family Physician (FP) program in urban areas [3]. Since its establishment in 2005, the program was commissioned to prevent unnecessary specialist visits, control the over/underutilization of services and improve access to proper care in cities with a 20,000 population [4]. Several challenges have been attached to the FP program that put other reforms on the table for the Iranian health system [5]. According to Takian et al., the FP was built up based on a public sector mindset, raising the government’s share in healthcare provision [6]. This arrangement not only was against Iran’s fourth development plan but also has limited opportunities for private or non-governmental partnerships. In response to these criticisms, Tabriz University of Medical Sciences launched a new Public-Private Partnership PHC model called Health Complexes (HCs) in 2013. The program aimed to expand population coverage, benefits package, and financial protection through efficient management of service provision by public and private partnerships. While many considerations have been taken before the establishment of the HCs, its accounting system was built up based on public sector accounting principles, which can only identify and record the current expenses of an organization. This system might not always reflect the opportunity cost of the resources necessary to assess its economic performance and the value of money provided [7].
Cost analysis and efficiency measurement are widely used economic tools that guide decision-making regarding the best use of healthcare resources [8]. Activity-Based Costing (ABC) has been recommended by the panel of specialists and effectiveness evaluators as the best choice approach for costing purposes [9]. ABC has been classified as a “top-down micro-costing” method in the health economics literature because of its focus on activities and accurate assigning overhead costs to final products [10]. This highly cited costing method requires the health providers to collect sophisticated data about the step-by-step process and attach the activities performed in delivering services to each approach. Finally, the overhead costs are first allocated to cost pools, then traced to cost objects [11].
Despite the necessity of detailed cost information in economic decision-making [12], most of the literature in Iran has adopted gross costing methods or top-down methods, even claiming it is ABC [13]. The findings of these studies may not be transferred to the Tabriz HCs setting because of the methodological and transferability issues such as reporting costing results and heterogeneity in cost object selection. For example, most studies did not provide sufficient details about cost components and process costs, so it is impossible to attach the cost data to cost objects [14]. Due to these challenges, the current study aimed to calculate the cost of delivered services in five Chamran Health Complex (CHC) health centers through the ABC method and assess these centers’ economic performance through Data Envelopment Analysis. The study findings can be used in cost management and budget-setting practice and as a basis for further economic analysis.
Methods
Chamran Health Complex (CHC) is an integrated health center that provides primary health care for more than 57,000 householders under the urban coverage area of Tabriz city. The administrative office manages the complex activities through 5 health facilities (HC1, HC2, HC3, HC4, and HC5) throughout the Akhmaghaye district to ensure fair access to healthcare. More than 83 services ranging from GP visits, vaccination, disease control and surveillance, dental care, and a limited sort of specialist visits were provided by the Complex. The Tabriz University of Medical Sciences proposed this project to produce evidence regarding the Complex’s cost profile and economic performance as a first launched PPP program providing primary healthcare services. Calculating the cost of services at health centers is essential for optimal pricing and determining reasonable tariffs. Additionally, evaluating the efficiency and performance of these centers is crucial to ensure that resources are used proportionately at each level of service provision, thereby minimizing production costs.
The project was conducted in 4 steps. First, the team engaged with stakeholders to assess the ongoing data sources or patient records to determine which data collection method would provide the best-quality information. Data for service activities and process maps, time and workload, human and financial resources, equipment, and consumables were collected using paper-based forms or excel datasheets. To characterize the analysis unit, we categorized service departments into overhead, intermediate and final activity centers according to their role in service provision. The last activity center directly contacts patients to provide requested services. Intermediate activity center supports final activity centers during the care process; even it can provide intermediary services, for example, laboratory, radiology, cash, and bill wards. Overhead activity centers support intermediate and final activity centers; they are not in contact with patients while facilitating service provision. Second, the project team held several meetings at the activity centers and conducted face-to-face interviews with providers and staff to develop a logbook for each activity center. It included information about the staff time, equipment modality and cost, room dimensions, service modality, process map, time, and frequency of delivered services in the study year. Second, we measured cost items within activity centers by adopting a micro-costing approach to the time and volume of patient utilization of resources. Data for cost items (staff, capital investment, consumables, and energy consumption) were collected from Accounting Information System. Utilization data were collected from the Iranian Integrated Health Record Portal (SIB: HTTPS://sib.tbzmed.ac.ir).
Where data was not available, we used expert opinion, direct observation, and log forms for recording needed data. The third step allocated the total overhead and intermediate activity centers to the final activity centers. It delivered services using the step-down adjustment and direct allocation approaches. Since the estimated unit cost during the routine costing process reflects an ongoing but not standard practice arrangement, we hypothesized a standard scenario according to the Iranian Ministry of Health standards for medical staff and organizational structure. Then, all the calculations were re-executed to determine the optimum unit costs [15]. We used Purchasing Power Parity (PPP) 2015 to adjust unit costs in national currency and reported in international dollars [16]. In the fourth step, the economic performance of health facilities was assessed through efficiency analysis. Input-oriented data envelopment analysis (DEA), assuming a variable return to scale, was used to determine technical, scale, and managerial efficiency using the following linear programming formula:
Subject to:
Where N is the number of health centers available in the studied sample, I and K are the number of outputs and inputs, respectively, and Wj is the weights allocated to N health centers. A health center is constituted by N×1 of constant values showing the weights of the reference set. Sn is the technical efficiency of the nth health center, and Yij and Xzj are the ith output and the kth input of the jth health center. Net technical efficiency (managerial efficiency) was assessed by dividing technical efficiency (in VRS state) to scale efficiency. The inputs used in the model were salary and wage, equipment expenses, building expenses, and covered population, while the outputs were the total time spent on service provision [17]. Costing was performed in Microsoft Excel 2013, and efficiency analysis by Deap2.1.
Results
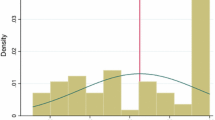
From October 2016 to June 2017, data was collected from five Health Centers (HC1-5) with at least 1000 unique observations per center. CHC comprises five centers that serve more the 57,000 population with a wide variety of preventive care, outpatient visits, and para clinical services without a more affordable charge. The complex spent $2,841,897, consisted of staff (80%), building (4.8%), equipment (2.1%), consumables (2.8%), energy (0.75%) and miscellaneousFootnote 1 (9.6%). HC1 absorbed the highest per capita budget ($70) among five health centers, while this share for HC2 was $20 (Table 1). There was great heterogeneity in calculated unit costs among health centers; for example, the unit cost of a Physician visit in HC2 was $15, compared to $38 (60% higher) in HC5. In general terms, the unit cost of services provided by HC1 is almost lower in 10 sample services. In contrast, the HC5 and HC4 generated unit cost values more than average in direct and step-down allocation methods (Table 1; Fig. 1).
Direct versus step-down allocation approach
Allocating overhead costs based on the direct and step-down approaches resulted in different unit costs in 4 of 10 sample services (pentavalent vaccination, tuberculosis screening, non-communicable disease screening, and physician visit). However, the mean comparison test results showed no difference in terms of allocation approach between average unit costs (P = 0.452) (Table 2; Fig. 2).
How much investment to achieve standard practice?
The total cost of the health complex was calculated at $3,002,214 after the execution of calculations in the standard scenario, meaning that the complex has to spend a further $160,317 to fulfill Ministry of Health standards for staff and construction. The investment would increase the unit costs by at least 25% in Health worker visits compared to 67% in Tuberculosis screening (Table 3).
Efficiency analysis
The efficiency of healthcare services in five health centers was analyzed using the DEA input-oriented efficiency model with the assumption of constant returns to scale. In total, 40% of health centers were technically efficient, of which 40% showed constant and the rest (60%) increasing return to scale. The managerial and scale efficiency was 0.893 and 0.546, respectively. The mean technical efficiency for the CHC was measured at 0.519, where HC4 showed the least (0.119), and HC1 and HC3 showed the highest technical efficiency (Table 4).
Excessive use of inputs by health centers was calculated as well. Figure zero indicates that the optimal and initial value of the production factors is the same; therefore, the difference between the actual and optimal use of production factors is zero. Only the HC4 has used unnecessary production factors, which range from (Table 5).
Discussion
We calculated the unit cost of services delivered in five health centers affiliated with the Chamran Health Complex (CHC), known for the first Public-Private Partnership (PPP) program in primary health care. The total budget allocated to the complex in the study period was $2,841,897, of which $1,910,373 (67%) was directly assigned to cost objects and the rest, $931,523 (33%), was allocated based on appropriate cost drivers. The unit cost of 10 sample services was reported and compared to whether there was no statistically significant difference between average unit costs in terms of overhead cost allocation approaches.
The heterogeneity in unit costs across five health centers might depend on the variation in the infrastructure or the performance of these centers. Understanding and managing the source of variabilities is essential; first, it helps managers trace inefficient points and address them by implementing productivity enhancement or cost containment strategies. Second, since the provision of services in the form of Health Complexes is the first PPP experience, the costing findings can shed light on fundamental differences in unit costs which can support decisions concerning the outsourcing and PPP contracts [18].
According to the World Health Organization report (2000), two-thirds of total costs typically belong to human resources. Likewise, a growing body of literature reported a 60 to 65% personnel cost rate [19]. This proportion is much higher in all five health centers highlighting the impact of human resources on final unit cost. Notwithstanding the high personnel costs, our results showed a gap between current human resources and the Iran Ministry of Health’s standards. If the complex wishes to fill the gap, $160,317 additional spending sounds necessary. These further costs were of particular concern, as the efficiency analysis demonstrated untouched capacity in all health centers; more spending seems not to be justifiable. We believe that the Iran Ministry of health’s national standards in human resources could be revised according to the health needs and service utilization at the local level.
According to the scenario analysis, investment in human resources and infrastructure according to MOH’s national standards will increase the unit cost by 36.4%. The highest 189% would influence the communicable disease department on average. Since the staff skills in this department are the same as Family Health and Vaccination departments, it seems that merging these departments would result in lower overhead costs and, consequently, unit costs.
Comparing the unit cost of services across health centers showed considerable variability in almost 70% of services. Part of this can be managed by proper planning, for example, job standardization and resource consumption management. However, part of these differences is due to the heterogeneity in sociodemographic characteristics and the geographical location of health facilities. For example, prolonged service time for the elderly or environmental health services in remote areas can produce higher unit costs. This variability needs to be reflected in budget allocation, reimbursement, and payment decisions. Previous studies highlighted such variability, which geared the establishment of new methodologies to estimate adjusted capitation payments. [20,21,22,23]
Exploring how allocation methods impact final unit costs, we detected that the average unit cost calculated from direct allocation methods was not different from the unit cost calculated from the step-down adjustment. This finding aligns with Carreras et al. [24], which concluded that the observed variation in disease cost depends mainly on direct costs, regardless of the cost allocation methodology. Unlike researchers interested in using the direct allocation method because of timing issues and its easiness, a comparison of services across health centers showed that the step-down allocation method seems to be more sensitive to resource consumption by cost centers and able to breakdown indirect costs into final services more accurately.
The mean technical efficiency measured 0.519, indicating inefficiency in health centers. Health centers have the potential to increase their efficiency by %48 with better management and performance without incurring additional costs. According to DEA results, 40% of health centers showed a constant return to scale, implying that a unit increase in inputs leads to an equivalent rise in output. The remaining 60% of health centers showed an increasing return to scale (output increases by more than the proportional increase in inputs). The managerial efficiency of the health centers was 0.893. This rate means that efficiency can be increased by 11% without increasing inputs and relying only on administrative decisions and employees’ efforts. The mean scale efficiency of the studied health centers was 0.546, and the scale efficiency score is less than one implies that the health centers are not operating at optimal scale or size.
There is a striking variability in service costs across health centers that must be addressed in performance management and contracting practices. Despite the existing gap between current and standard practice in terms of staff and facilities, which calls for extra investment in personnel and equipment recruitment, efficiency analysis highlights inefficiency in the Health Complex, which could be resolved by better planning without additional spending. Such a discrepancy raises the need for revising current national standards to ensure more efficient performance. It is worth noting that the newer costing methods like Activity Based Costing can realize the inefficient points in resource consumption by different processes in primary health care and guide better resource allocation decisions.
This study has several limitations that should be acknowledged. First, the reliance on available data from patient records and accounting systems may introduce biases, as incomplete or inaccurate data could affect the cost calculations and efficiency assessments. Additionally, the study’s focus on five health centers within the Chamran Health Complex may limit the generalizability of the findings to other regions or healthcare settings in Iran. Furthermore, the assumption of a standard scenario based on national guidelines may not fully account for local variations in healthcare delivery and resource utilization. Lastly, the analysis primarily emphasizes quantitative metrics, potentially overlooking qualitative factors that could influence healthcare outcomes and patient satisfaction. These limitations suggest the need for further research to validate the findings and explore additional dimensions of healthcare performance.
Based on the findings of this study, we propose the following recommendations. These recommendations aim to guide policymakers and healthcare administrators in enhancing the economic performance and efficiency of primary healthcare services in Iran.
Implement activity-based costing (ABC)
-
Health centers should adopt ABC as a standard practice for cost analysis to ensure a more accurate reflection of resource utilization. This approach will facilitate better decision-making regarding resource allocation and service pricing.
Enhance data collection methods
-
To improve the accuracy of cost assessments, health facilities should invest in robust data collection systems that capture detailed information about service delivery processes and resource consumption. Training staff on effective data management practices is also essential.
Standardize operational practices
-
The Iranian Ministry of Health should consider revising national healthcare standards to align with local service delivery realities. This will help ensure that health centers can meet established benchmarks while accommodating regional differences in healthcare needs.
Focus on efficiency improvement
-
Regular efficiency audits should be conducted at health centers to identify bottlenecks and areas for improvement. Implementing best practices in management and operational processes can help enhance service delivery and reduce costs.
Conclusion
This study highlights the significant challenges and opportunities within the Iranian healthcare system, particularly regarding the cost and efficiency of primary healthcare services provided by the Chamran Health Complex. By employing ABC and DEA, we identified substantial variability in service costs across the five health centers, revealing inefficiencies that could be addressed through better management practices.
The findings indicate that while the current expenditure of approximately $2.84 million is heavily weighted toward personnel costs, there remains a critical gap between actual and standard practices as defined by the Iranian Ministry of Health. An additional investment of $160,317 is necessary to meet these standards, yet the efficiency analysis suggests that a significant portion of this gap could potentially be closed through improved operational strategies rather than increased spending.
Moreover, the lack of statistical differences between direct and step-down cost allocation methods emphasizes the need for robust cost management practices that accurately reflect resource consumption. The study underscores the importance of revising national standards to align with local health needs and service utilization patterns, thus promoting more effective resource allocation.
In conclusion, the integration of advanced costing methodologies like ABC can inform decision-making processes, enhance the economic performance of health facilities, and ultimately improve access to quality healthcare services in Iran. Addressing the identified inefficiencies and standardizing practices will be crucial for achieving sustainable healthcare financing and enhancing the overall effectiveness of the health system.
Data availability
No datasets were generated or analysed during the current study.
Notes
. Contracts, transportation, copy, print, and catering.
References
Huang SL. Factors Influencing Healthcare Spending in Singapore: a regression model. Int J Comput Internet Manage. 2004;12(3).
Gulliford M, Morgan M. Access to Health Care. 1th ed. Routledge; 2003.
alishahi a, Jafari M. mahbobi m. Human resources, equipment and standards: Darrehshahr health network. 2020.
Hooshmand E, Nejatzadegan Z, Ebrahimipour H, Esmaily H, Vafaee Najar A. The challenges of the Family Physician Program in the North East of Iran from the perspective of managers and practitioners working on the plan. J FASA Univ Med Sci. 2020;9(4 f001270).
Shirjang AMS, Masoudi Asl I, Doshmangir L. Challenges and strategies of implementation Rural Family Physician in Iran: a qualitative study. Depiction Health. 2020;11(1):11.
Khayatzadeh-Mahani A, Takian A. Family physician program in Iran: considerations for adapting the policy in urban settings. Arch Iran Med. 2014;17(11):776–8.
Jafar Sadegh T, Majid K, Homayoun S-B, Alireza N, Leila N, Roya H et al. Health Complex Model as the start of a New Primary Healthcare Reform in Iran: part B: the intervention protocol. Iran J Public Health. 2019;48(1).
Shepard DS. Cost-effectiveness in Health and Medicine. By M.R. Gold, J.E Siegel, L.B. Russell, and M.C. Weinstein, editors. New York: Oxford University Press, 1996. The Journal of Mental Health Policy and Economics. 1999;2(2):91 – 2.
Fiedler JL, Villalobos CA, De Mattos AC. An activity-based cost analysis of the Honduras community-based, integrated child care (AIN-C) programme. Health Policy Plann. 2008;23(6):408–27.
Javid M, Hadian M, Ghaderi H, Ghaffari S, Salehi M. Application of the activity-based costing method for unit-cost calculation in a hospital. Glob J Health Sci. 2015;8(1):165–72.
Negrini D, Kettle A, Sheppard L, Mills GH, Edbrooke DL. The cost of a hospital ward in Europe: is there a methodology available to accurately measure the costs? J Health Organ Manag. 2004;18(2–3):195–206.
Chapko MK, Liu CF, Perkins M, Li YF, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ. 2009;18(10):1188–201.
Gholamhoseini MT, GOUDARZI R, Nikravesh A, Beig Zade Abassi F. Calculating the final cost of the educational services of Kerman School of Management and Information Sciences through activity-based costing. Iran J Med Educ. 2019;19(82 #p001049).
Everaert P BW, Sarens G, Anderson SR, Levant Y. Cost modeling in logistics using time-driven ABC experiences from a wholesaler. Int J Phys DISTRIBUTION LOGISTICS Manage. 2008;38(3–4):19.
Yarikkaya E, Özekinci S, Sargan A, Durmuş ŞE, Yildiz FR. A comparative study of activity-based costing vs. current pricing system for Pathology examinations at Okmeydani Training and Research Hospital, Turkey. Turk Patoloji Dergisi. 2017;33(1):17–24.
Islamic Republic of Iran Implied PPP Conversion Rate, LCU per USD [Internet]. 2021. https://data.nasdaq.com/data/ODA/IRN_PPPEX-islamic-republic-of-iran-implied-ppp-conversion-rate-lcu-per-usd
Yusefzadeh H, Hadian M, Gorji HA and Ghaderi H. Assessing the Factors Associated With Iran’s IntraIndustry Trade in Pharmaceuticals. GJHS. (2015) 7: 311.
McBain RK, Jerome G, Leandre F, Browning M, Warsh J, Shah M, et al. Activity-based costing of healthcare delivery, Haiti. Bull World Health Organ. 2018;96(1):10–7.
Organization WH. The world health report 2000: health systems: improving performance. geneva: World Health Organization; 2000.
Nosratnejad S, Esmaeili R, Tabrizi J, Mahboub-ahari A. Development of age-sex adjusted capitation payment: the experience of Iranian public health complexes. Int J Health Plann Manag. 2018;34.
Yusefzadeh H, Rezapour A, Lotfi F, Azar FE, Nabilo B, Gorji HA, Hadian M, Shahidisadeghi N and Karami A. A Study of Comparative Advantage and Intra-Industry Trade in the Pharmaceutical Industry of Iran. GJHS. (2015) 7: 295.
Zahroh AH, Putri RA, Shima L, Erdayani E, Martaliza R, Anggoro TP et al. Risk Adjustment of Capitation Payment System: What Can Indonesia Adopt from other Countries? 2019;2019:3(1).
Balogh S. Risk adjusted capitation is the basis for general practitioners’ renumeration. Orv Hetil. 2019;160:1057–63.
Carreras M, Goñi M, Ibern P, Coderch J, Vall-llosera L, Inoriza JM. Estimates of patient costs related with population morbidity: can indirect costs affect the results? Eur J Health Economics: HEPAC : Health Econ Prev care. 2010;12:289–95.
Acknowledgements
Authors would like to express their special thanks and gratitude to the Health Deputy staff in TUoMS, particularly those working in Chamran Health Complex. We respect and thank all research staff at the School of Management and Medical Informatics of TUoMS.
Funding
This work was financially supported by Tabriz University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
This project was carried out in collaboration with all authors. A.M.H. and S.Kh. contributed to the study protocol design. S.Kh. conducted the interviews and data collection. A.M.H., H.Y., and A.Gh. participated in the data analysis and interpretation of results. All of the authors participated in manuscript redaction. They read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Ethics Committee of Tabriz University of Medical Sciences in January 2018. TBZMED.REC.1394.981.
Consent for publication
Not applicable since the study does not contain any person’s data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mahboub-Ahar, A., Khanlari, S., Yusefzadeh, H. et al. Cost and efficiency analysis in Iranian primary health centers: a micro costing and data envelopment analysis. Cost Eff Resour Alloc 22, 56 (2024). https://doi.org/10.1186/s12962-024-00567-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-024-00567-8