Abstract
Background
Prostate cancer (PCa) causes a substantial health and financial burden worldwide, underscoring the need for efficient mass screening approaches. This study attempts to evaluate the Net Cost-Benefit Index (NCBI) of PCa screening in Iran to offer insights for informed decision-making and resource allocation.
Method
The Net Cost-Benefit Index (NCBI) was calculated for four age groups (40 years and above) using a decision-analysis model. Two screening strategies, prostate-specific antigen (PSA) solely and PSA with Digital Rectal Examination (DRE), were evaluated from the health system perspective. A retrospective assessment of 1402 prostate cancer (PCa) patients’ profiles were conducted, and direct medical and non-medical costs were calculated based on the 2021 official tariff rates, patient records, and interviews. The monetary value of mass screening was determined through Willingness to Pay (WTP) assessments, which served as a measure for the benefit aspect.
Result
The combined PSA and DRE strategy of screening is cost-effective, yields up to $3 saving in costs per case and emerges as the dominant strategy over PSA alone. Screening for men aged 70 and above does not meet economic justification, indicated by a negative Net Cost-Benefit Index (NCBI). The 40–49 age group exhibits the highest net benefit, $13.81 based on basic information and $13.54 based on comprehensive information. Sensitivity analysis strongly supports the cost-effectiveness of the combined screening approach.
Conclusion
This study advocates prostate cancer screening with PSA and DRE, is economically justified for men aged 40–69. The results of the study recommend that policymakers prioritize resource allocation for PCa screening programs based on age and budget constraints. Men’s willingness to pay, especially for the 40–49 age group which had the highest net benefit, leverages their financial participation in screening services. Additionally, screening services for other age groups, such as 50–54 or 55–59, can be provided either for free or at a reduced cost.
Similar content being viewed by others
Introduction
Cancer is one of the leading causes of death in the world. In the year 2020, Global forecasts expected a 45% increase in cancer in developing countries [1]. Cancer has a significant effect on the financial situation of patients and their families. It is estimated that 16.1 million people are living with cancer, faceing out-of-pocket payments 61% higher than patients with no history of cancer ($ 1,000 vs. $ 622). Cancer also has significant indirect costs in terms of lost revenue. An analysis of 493,000 deaths caused by cancer in people aged 16 to 84 in the United States in 2015 showed that $ 94.4 billion was lost in revenue [2].
Over the past decade, prostate cancer (PCa) has experienced rapid growth in Iran, emerging as one of the most prevalent types of cancers [3]. PCa imposes a substantial financial burden on healthcare systems worldwide. Treatment and hospitalization costs for PCa patients in European countries range between 106.7 and 179 million US dollars annually, while in the United States, they soar to 9.862 billion dollars. In Canada, the annual, inclusive of hospitalization and treatment, stands at 103.1 million dollars in 1998, whereas in Australia it was 101.1 million dollars between 1993 and 1994 [4]. In 2009, healthcare costs associated with prostate cancer across the EU totaled €8.43 billion [5]. The societal costs attributed to prostate cancer in Stockholm in 2016 were estimated at €64 million Euros, 62% of which related to direct medical costs [6].
Early detection of cancer not only yields positive clinical outcomes by reducing patient mortality rates and enhancing their quality of life, but also positively impacts treatment modalities and their financial implications. Numerous studies have demonstrated that early diagnosis leads to reduced treatment expenses. The cost of caring for cancer patients in their final years is significantly higher than caring costs during the initial phase following diagnosis [4] or the expenses associated with early-stage treatment [7, 8]. An economic burden study conducted in Iran found that patients with advanced-stage prostate cancer incur substantial treatment costs, whereas these expenses are two to three times lower in the early stages of treatment [3]. This discrepancy led to annual savings of $26 billion for early cancer detection in the United States [9]. Furthermore, early diagnosis enables patients to maintain their occupational activities by reducing treatment durations and incurring lower treatment costs [10].
Despite increasing prevalence and mortality rates of PCa in some developing countries, evidence shows that mortality rates in some high-income countries have declined as a result of early detection. This early detection is attributed to the common use of different early detection methods in these countries [11], clearly demonstrating the importance of early diagnostic measures, including screening [12].
Previous studies have shown that PCa screening causes a significant (about 21%) reduction in the mortality rate of PCa patients in Australia [13] in Iran [12, 14] and even in Europe, despite the high prevalence rate [15].
Prostate cancer (PCa) in Iran has imposed a significant financial burden, which totaled around $25.8 million in 2019 [16]. This disease has had an increasing incidence rate in this country. PCa incidence increases with age, and it is very common from the age of 50. Therefore, as the Iranian baby boom of the 1980s has reached their 40s, the aging of the population will accelerate and it is expected that PCa incidence will have an increasing trend in Iran. Consequently, the combination of the high burden of this disease and the resulting high economic burden, along with the increasing aging of the population, shows the importance of providing a screening program.
In order to make decisions about the implementation of screening programs, it is necessary to consider the evidence-based economic evaluation of implementing this program in terms of costs and benefits [17]. This is the main objective of this study.
Using WTP is a common method to measure the benefit alongside detecting the acceptance of strategies in economic evaluation and cost benefit analysis of implementing cancer interventions [17,18,19]. Also, the willingness to pay approach has the capacity to compute false positive and negative results of diagnostic tests, which help promote the accuracy of evaluation indicators and the elimination of potential biases [20]. Based on these propositions, in this study the willingness to pay approach has been used as a benefit index to estimate the NCBI of PCa screening for different age groups.
Method and design
The foundations of calculating the Net cost-benefit index (NCBI) of prostate cancer (PCa) screening in Iranian men aged 40 and above relied on costs and benefits information. We retrospectively explored the SEPAS Iranian Health Ministry database to extract and compute costs, utilizing a decision tree within a one-year time horizon. Additionally, the monetary value of screening for prostate cancer was extracted from an earlier study conducted by the authors which used the Willingness to pay method.
The analysis was carried out from the health system perspective, and all costs were reported in United State Dollars (1$ = 230,000 IRR, based on the market exchange rate) [21]. To account for the Iranian inflation rate and the banking system interest rate (serving as the risk-free rate) over the last 40 years, a discount rate of 20% was applied to intertemporal calculations.
Population
We identified all patients specifically seeking services in hospitals during 2021 and undergoing treatments with action codes related to prostate cancer (PCa) to form our study sample. This group comprised 1402 patients, and their recorded data were extracted from the Iranian Health System Database (SEPAS).
To estimate the Iranian population requiring screening for PCa in 2021, we extrapolated from pertinent population data derived from the 2016 Iran population and housing census [22]. This extrapolation considered the population growth rate between the two most recent census years conducted in Iran (2011 and 2016).
Model structure
The model structure for our prostate cancer screening study compares two diagnostic tests: screening with a PSA test and screening with a combination of PSA and DRE tests. The decision tree (Fig. 1) and the associated probabilities (Table 1) were developed through a meticulous review of existing studies.
An expert panel, including four health economists and twelve urologists, customized the model to the context of this study, adjusting probabilities based on PSA cut-offs and different age groups. This tailored approach ensures the accuracy and relevance of our findings.
Resource use and unit costs
In this study, we considered both direct medical and non-medical costs when calculating the prostate cancer screening cost.
Direct Medical Costs:
Direct medical costs included resource utilization for diagnosis, treatment, and associated complications.
The treatment costs for different prostate cancer (PCa) stages—low-, moderate-, and advanced-risk — included expenses related to prostatectomy surgery, radiotherapy, hormone therapy, and active surveillance regimens.
The complications costs, including bleeding, infection, sexual problems, urinary retention, cardiovascular issues, hot flashes, weakness, and lethargy, were comprehensively addressed in our study.
For inpatient resource utilization, we used action codes from the RVU book, extracting costs based on action codes from the SEPAS Iranian Health Ministry database and national tariffs.
The diagnostic costs were thoroughly considered for PSA, DRE, and biopsy tests, with the related resource use extracted from patient profiles and their unit costs derived from national tariffs.
Direct Non-Medical Costs:
The direct non-medical costs of PCa treatment were sourced from a relevant study estimating the economic burden of PCa in Iran.
The direct non-medical costs of PCa diagnosis were measured through phone interviews with a stochastic sample of 240 patients, covering transportation, travel, accommodation, and food expenses.
The total cost was defined as the combined sum of direct medical and non-medical costs. In each branch of our decision tree, average costs were computed by multiplying the costs associated with each node by their respective probabilities.
Benefit
The assessment of benefits for prostate cancer screening in the current study builds upon insights gained from our prior research [27]. In this study, we utilized the willingness-to-pay method, incorporating two distinct sets of information. Participants’ monetary valuations were elicited through scenarios that presented comprehensive details, including both basic and complementary information related to prostate cancer diagnosis and treatment methods.
By employing this nuanced approach, we aimed to capture a more comprehensive understanding of individuals’ willingness to invest in prostate cancer screening. The combination of fundamental knowledge and supplementary insights provided participants with a holistic perspective, allowing for a more informed assessment of the perceived benefits associated with early detection.
This refined methodology ensures that our evaluation not only delves into the economic aspect of willingness to pay but also considers the impact of comprehensive information on participants’ decision-making processes. As a result, this study contributes a more nuanced and insightful perspective to the assessment of the benefits associated with prostate cancer screening.
Net cost-benefit index
The Net Cost-Benefit Index (NCBI) was computed for all population and five distinct age groups of men (40–49, 50–54, 55–69, 70–79, and 80 & above) using the following formula:
NCBI = Benefit(Average of men’s willingness to pay)– Cost(Average cost of PCa screening)
NCBI for prostate cancer (PCa) screening was determined under four conditions, encompassing two strategies for cost and two scenarios for benefit.
In interpreting the Net Cost-Benefit Index (NCBI), a positive value indicates that the average willingness-to-pay for prostate cancer (PCa) screening exceeds the average cost, suggesting a net benefit. Conversely, a negative value implies that the average cost outweighs the average willingness-to-pay. The calculation was performed under four conditions, considering different cost strategies and benefit scenarios, providing a comprehensive perspective on the economic implications of PCa screening across various age groups.
Sensitivity analysis
A comprehensive one-way sensitivity analysis was undertaken, systematically varying the potential complications associated with both the screening and treatment processes by ± 20%. This rigorous exploration aimed to evaluate the impact of uncertainties surrounding complication rates on the findings of the present study. Subsequently, the robustness and reliability of the results were examined through an in-depth assessment of the Net Cost-Benefit Index (NCBI).
Results
The population of Iranian men aged 40 years and older in 2021 are shown in Table 2 below.
Costs of prostate cancer screening
The results of the cost calculation with two different strategies indicate that the total cost of screening using PSA is approximately $127 million, while the cost of screening using both PSA and DRE equals approximately $90 million. Consequently, the cost of implementing this program with the combined DRE and PSA test is approximately 30% less as compared with conducting it with the PSA test alone (Table 3).
The average cost of screening only through PSA was $10 per man, and it reduced to $7 per man with the inclusion of both PSA and DRE. Decomposing the total cost by diagnosis, treatment, and complications reveals that, in both strategies, medical direct costs of treatment constitute the largest share of total costs.
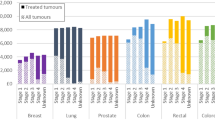
Cost of prostate cancer screening by different age groups
As the total and average costs were lower in the PSA and DRE screening strategy, the calculation of PCa screening costs was conducted separately for each age group based solely on this approach. According to Table 4, the highest total screening costs were observed in men aged 40–49. Additionally, screening for men aged 40–69 had the lowest average cost, while the highest average cost was observed in men aged 80 and above.
Men’s willingness to pay by different age groups
The men’s willingness to pay across age groups, which was extracted from our prior study, is outlined in Table 5. For more details, refer to the relevant study [27].
Cost-benefit analysis
Based on Willingness to Pay (WTP) using both basic and complementary information, PCa screening with PSA for all men showed NCBI values of $9.14 and $7.67 per screened case, respectively. Additionally, PCa screening with PSA and DRE had NCBI values of $11.1 and $9.7 for men with basic and complementary information, respectively (Table 5).
The NCBI starts positively at $9.14 for basic information in the case of PSA screening. It decreases to $7.67 for complementary information, but remains positive, signifying a favorable balance between screening cost with PSA and the benefit measured by willingness to pay. On the other hand, for screening through PSA and DRE, the NCBI increases to $11.1 with basic information and $9.7 with complementary information. This clear trend indicates that screening through PSA and DRE emerges as the dominant strategy for prostate cancer (PCa) screening.
The NCBI for the dominant strategy with basic information is positive, indicating a favorable balance between the screening cost with PSA and DRE and the benefit measured by willingness to pay. However, the inclusion of complementary information results in a decrease in the NCBI for all men and all age groups.
The NCBI remains positive for individuals aged 40–69, suggesting a benefit outweighing the cost. The highest NCBI is observed in the youngest age group (40–49), reaching $13.8 for basic information and $13.5 for complementary information. This discrepancy indicates that basic information contributes to a more favorable balance in this age group. In contrast, the lowest Net Cost-Benefit Index is observed in individuals aged 70 and above, showing a negative value and indicating a less favorable balance. The highest net negative benefit was observed in the 80 + age group.
This result illustrates a consistent decreasing trend for both basic and complementary information as age increases.
Sensitivity analysis
Sensitivity analysis was conducted focusing on the combined PSA and DRE screening strategy, as illustrated in Figs. 2 and 3 below.
The results of the sensitivity analysis revealed that the NCBI for each prostate cancer (PCa) screening did not undergo significant changes. The findings remained robust and consistent despite the variations introduced. Importantly, the sign of NCBI remained unchanged for all age groups, regardless of the availability of basic or complementary information.
In summary, the sensitivity analysis demonstrated the resilience of the results, emphasizing the stability and reliability of the NCBI across different scenarios and age groups, even when subjected to variations in the potential complications of the screening and treatment processes.
Sensitivity analysis for NCBI of men PCa screening by PSA and DRE: in case of Basic Information. DRC: Decrease Radiotherapy Complication, IRC: Increase Radiotherapy Complication, DSC: Decrease Surgery Complication, ISC: Increase Surgery Complication, DBC: Decrease Biopsy Complication, IBC: Increase Biopsy Complication
Sensitivity analysis for NCBI of men PCa screening by PSA and DRE: in case of Complementary Information. DRC: Decrease Radiotherapy Complication, IRC: Increase Radiotherapy Complication, DSC: Decrease Surgery Complication, ISC: Increase Surgery Complication, DBC: Decrease Biopsy Complication, IBC: Increase Biopsy Complication
Discussion
Our exploration into prostate cancer screening, specifically using Prostate-Specific Antigen (PSA) and Digital Rectal Examination (DRE), has unraveled diverse economic implications. In this section, we provide a concise overview of our main findings before delving into the details. Our analysis centers on the NCBI and its variations across age groups, offering valuable insights into the economic feasibility and considerations for these screening strategies.
Incorporating Digital Rectal Examination (DRE) alongside Prostate-Specific Antigen (PSA) screening has been shown to offer significant economic benefits, owing to its heightened sensitivity, specificity, and diagnostic accuracy in detecting prostate cancer [21]. Numerous studies have highlighted the enhanced accuracy achieved when PSA is combined with DRE in prostate cancer detection [28,29,30,31,32]. While the exact reduction in unnecessary biopsies may vary - reported to be 12% in the study by Littrup [33] and even higher in our own research - our analysis emphasizes the tangible economic advantages derived from integrating DRE into the screening process. These findings are in line with recommendations put forth by the World Health Organization (WHO) [30], which advocate the joint utilization of PSA and DRE as a prudent and economically viable approach. Similarly, several studies [34,35,36] have lent support to the effectiveness of combining PSA with DRE for improved prostate cancer detection, a conclusion further bolstered by our own investigation.
Notably, the NCBI screening was positive for all men, indicating economic justifiability but their result was different for different age groups.
Despite accounting for different PSA threshold levels in various age groups, adding DRE to screening leads to notable variations in total and average costs and the NCBI across age categories in both screening scenarios. The results underscore the impact of age group composition on the economic outcomes of prostate cancer screening, aligning with the findings in literature [26].
The study gauged the benefits of early detection through Willingness to Pay (WTP), revealing that, in screening with DRE and PSA tests, the population aged 40–69 experienced a net positive benefit when provided complementary information, particularly in the age range of 40–54 it is high. This can be attributed to the reduction in WTP variance, and the cost-effectiveness achieved by combining DRE with PSA testing. In comparison to the relevant study by Rao [20], our approach, which takes into account false positive and negative results in willingness-to-pay (WTP) assessments, enhances the reliability of the findings.
Screening for men aged 70 and above was consistently deemed economically unjustified. The lowest NCBIs were observed in the 70–79 and 80 + age groups, likely influenced by reduced WTP due to limited income post-retirement, shorter life expectancy, higher probabilities of comorbidities, and increased screening costs. The findings are consistent with the existing literature, which recommends that screening beyond a certain age should be stopped to overcome overdiagnosis and associated high costs [26, 37].
Conversely, the age groups of 40–49 and 50–54 exhibited the highest NCBI, emphasizing the economic feasibility of screening in these cohorts, especially in a situation without financial limitations. However, it’s essential to note that despite the positive NCBI in the 40–49 age group, caution is warranted in situations with financial limitations. Various studies and guidelines, such as those by the European Urological Association (EAU), recommend initiating screening at age 50 [38]. The recommendation by other aligns with the consensus that initiating prostate cancer screening at the age of 50 and older is optimal, with no additional benefits observed for men commencing screening at age 40 instead of 50 [39]. The apparent contradiction with previous studies concerning this age group may stem from two primary aspects. Firstly, our study measured benefits based on stated Willingness to Pay (WTP), while prior studies utilized alternative criteria [20, 40, 41], just one study [18] found to have used WTP for measuring benefit just for PSA test as screening intervention. Secondly, previous studies aimed to enhance the probability of early detection, while our approach gauged the value of early detection from the perspective of men.
The sensitivity analysis results bolster the credibility of our study, affirming the consistent economic justification of PSA and DRE screening across diverse age groups. Our sensitivity analysis findings align with previous research [42], which evaluated a range of probabilities for potential complications, further reinforcing our study’s alignment with existing literature.
The study suggests that policymakers should carefully assess the impact of increased information levels on the target population’s willingness to participate in screening. It highlights that additional information may not necessarily lead to a significant improvement in screening acceptance and attendance [27], questioning the need for substantial financial resources to enhance public awareness initiatives.
Limitations
-
It was not possible to interview patients in extracting direct non-medical costs during the treatment phase. As the data was extracted from the SEPAS system of the Ministry of Health and due to ethical considerations, patients’ personal information such as their job, address and telephone number were not available to the research team. Therefore, this information was extracted from other studies conducted for Iran.
-
The costs of complications consist of cases that occur shortly after treatment and do not include the cost of subsequent visits.
-
Due to the very low probability of biopsy complications, no bills were found in the SEPAS system to the relevant action code. The unit cost of these complications was calculated based on the government tariff and was considered the same for the studied sample.
Conclusion
In conclusion, this study strongly advocates the implementation of prostate cancer screening through the combined use of PSA and DRE. The findings suggest that, without financial limitations, screening for men between the ages of 40–69 is economically justified. However, when considering financial resource limitations, it is advisable to prioritize screening based on suggested age categories. Specifically, various studies and guidelines recommend initiating screening at age 50. Following these recommendations, the suggested age priorities for screening based on our results are as follows: men aged 50–54 as the primary priority, followed by men aged 55–69 as the secondary priority, and men aged 40–49 as the tertiary priority. These recommendations carry vital policy implications, suggesting that allocating public resources to screening men aged 69 and above (and those under 40) may not be economically justified. Moreover, the results provide a rationale for health insurers to consider covering the cost of prostate cancer screening, offsetting treatment costs, and justifying the investment. Considering Willingness to Pay (WTP) as the basis for benefit calculation, it becomes evident that the first to third age priorities present the highest potential for out-of-pocket payments for screening. In the absence of sufficient resources from health insurers and government budgets, individuals within these age groups may be more inclined to bear the screening costs, providing an opportunity for the government to complement the screening program. While this study was conducted statically over a specific period, its results can also be analyzed in a dynamic context. The initiation and continuation of the screening program may foster a preventive habit among current 40-year-old men, who would undergo screening 29 times annually until reaching the age of 69. This habitual engagement, coupled with ongoing justification programs, may lead to a sustained desire for screening even after the age of 69. In such a scenario, out-of-pocket payments might not hinder continued screening unless individuals are dealing with other chronic conditions or do not foresee a longer life for any reason.
The present study recommends policymakers evaluate the impact of increased information on participation in screening. It suggests that more information might not significantly enhance attendance, raising doubts about the necessity for substantial financial resources in public awareness initiatives.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
- NCBIs:
-
Net Cost-Benefit Index
- PCa:
-
Prostate Cancer
- PSA:
-
Prostate Specific Antigen
- DRE:
-
Digital Rectal Examination
- WTP:
-
Willingness to Pay
- CVM:
-
Contingent Valuation Method
References
Kanavos P. The rising burden of cancer in the developing world. Ann Oncol. 2006;17:viii15–23.
Ekwueme DU. Annual out-of-pocket expenditures and financial hardship among cancer survivors aged 18–64 years—United States, 2011–2016. MMWR Morbidity Mortal Wkly Rep. 2019;68.
Mojahedian MM, Toroski M, Keshavarz K, Aghili M, Zeyghami S, Nikfar S. Estimating the cost of illness of prostate cancer in Iran. Clin Ther. 2019;41(1):50–8.
Roehrborn CG, Black LK. The economic burden of prostate cancer. BJU Int. 2011;108(6):806–13.
Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14(12):1165–74.
Hao S, Östensson E, Eklund M, Grönberg H, Nordström T, Heintz E, et al. The economic burden of prostate cancer–a Swedish prevalence-based register study. BMC Health Serv Res. 2020;20:1–15.
Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(7):1304–12.
Gretzer MB, Partin AW. PSA levels and the probability of prostate cancer on biopsy. Eur Urol Supplements. 2002;1(6):21–7.
Ezell S. Seizing the transformative opportunity of multi-cancer early detection. Information Technology and Innovation Foundation; 2021.
Organization WH. Early cancer diagnosis saves lives, cuts treatment costs. World Health Organization; 2017.
Taitt HE. Global trends and prostate cancer: a review of incidence, detection, and mortality as influenced by race, ethnicity, and geographic location. Am J Men’s Health. 2018;12(6):1807–23.
KOLAH DS, Sajadi A, Radmard AR, KHADEMI H. Five common cancers in Iran. Arch Iran Med. 2010;13(2):143–6.
Lew J-B, Feletto E, Wade S, Caruana M, Kang Y-J, Nickson C et al. Benefits, harms and cost-effectiveness of cancer screening in Australia: an overview of modelling estimates. Public Health Res Pract. 2019;29(2).
Rafimanesh H, Ghoncheh M, Salehinia H, Mohammadian Hafashjani A. Epidemiology of prostate cancer and its incidence trends in Iran. J Sabzevar Univ Med Sci. 2016;23(2):320–7.
Chen F-z. Zhao X-k. Prostate cancer: current treatment and prevention strategies. Iran Red Crescent Med J. 2013;15(4):279.
Foroughi Moghadam MJ, Ayati M, Rangchian M, Pourmand G, Haddad P, Nikoofar A, et al. Economic burden of prostate cancer in Iran: measuring costs and quality of life. Middle East J Cancer. 2019;10(2):139–55.
Abdi F, Alinia C, Taghizadeh Afshari A, Yusefzadeh H. Cost–benefit analysis of kidney transplant in patients with chronic kidney disease: a case study in Iran. Cost Eff Resource Allocation. 2022;20(1):1–9.
Umeh IB, Ogbuagu CN, Okafor C, Abhulimen V, Abiahu JA, Biambo AA, et al. Cost–benefit analysis of a Population–Based prostate–specific Antigen Mass Testing for early detection of prostate Cancer in Anambra State, Nigeria: A Health Provider’s perspective. Niger J Med. 2022;31(6):672–80.
Meshkani Z, Moradi N, Aboutorabi A, Farabi H, Moini N. A cost-benefit analysis of genetic screening test for breast cancer in Iran. BMC Cancer. 2024;24(1):279.
Carlsson P, Pedersen KV, Varenhorst E. Costs and benefits of early detection of prostatic cancer. Health Policy. 1990;16(3):241–53.
Iran CBotIRo. Electronic Trading System [ http://www.sanarate.ir].
Iran SCo. Findings of the 2016 National Population and Housing Census Tehran. 2017. [ http://www.amar.org.ir].
Andriole GL, Levin DL, Crawford ED, Gelmann EP, Pinsky PF, Chia D, et al. Prostate Cancer Screening in the prostate, lung, colorectal and ovarian (PLCO) Cancer Screening Trial: findings from the initial screening round of a randomized trial. J Natl Cancer Inst. 2005;97(6):433–8.
Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol. 2010;28(7):1117.
Berger AP, Gozzi C, Steiner H, Frauscher F, Varkarakis J, Rogatsch H, et al. Complication rate of transrectal ultrasound guided prostate biopsy: a comparison among 3 protocols with 6, 10 and 15 cores. J Urol. 2004;171(4):1478–81.
Rao K, Liang S, Cardamone M, Joshu CE, Marmen K, Bhavsar N, et al. Cost implications of PSA screening differ by age. BMC Urol. 2018;18(1):1–8.
Farabi H, Moradi N, Ahmadzadeh A, Agamir SMK, Mohammadi A, Rezapour A. Factor associated with willingness to pay for prevention of cancer: a study of prostate cancer screening. Cost Eff Resource Allocation. 2023;21(1):89.
Matumaini H, Mmbaga B, Amsi P, Lukambagire A, Ngowi B, Nyindo M, THE DIAGNOSTIC ACCURACY OF COMBINED PROSTATE-SPECIFIC ANTIGEN (PSA). AND DIGITAL RECTAL EXAMINATION (DRE) IN PROSTATE CANCER IN NORTHERN TANZANIA. East Afr Med J. 2022;99(6).
Moul JW. Comparison of DRE and PSA in the detection of prostate Cancer. J Urol. 2017;197(2).
Catalona WJ, Richie JP, Ahmann FR, Hudson MLA, Scardino PT, Flanigan RC, et al. Comparison of digital rectal examination and serum prostate specific antigen in the early detection of prostate cancer: results of a multicenter clinical trial of 6,630 men. J Urol. 2017;197(2S):S200–7.
Poyet C, Nieboer D, Bhindi B, Kulkarni GS, Wiederkehr C, Wettstein MS, et al. Prostate cancer risk prediction using the novel versions of the European Randomised study for screening of prostate Cancer (ERSPC) and prostate Cancer Prevention Trial (PCPT) risk calculators: independent validation and comparison in a contemporary European cohort. BJU Int. 2016;117(3):401–8.
Halpern JA, Oromendia C, Shoag JE, Mittal S, Cosiano MF, Ballman KV, et al. Use of digital rectal examination as an adjunct to prostate specific antigen in the detection of clinically significant prostate cancer. J Urol. 2018;199(4):947–53.
Littrup PJ, Kane RA, Mettlin CJ, Murphy GP, Lee F, Toi A, et al. Cost-effective prostate cancer detection. Reduction of low‐yield biopsies. Cancer. 1994;74(12):3146–58.
Crawford ED, Leewansangtong S, Goktas S, Holthaus K, Baier M. Efficiency of prostate-specific antigen and digital rectal examination in screening, using 4.0 ng/ml and age-specific reference range as a cutoff for abnormal values. Prostate. 1999;38(4):296–302.
Galić J, Karner I, Cenan L, Tucak A, Hegedus I, Pasini J, et al. Comparison of digital rectal examination and prostate specific antigen in early detection of prostate cancer. Coll Antropol. 2003;27(Suppl 1):61–6.
Ozah E, Imasogie DE. The diagnostic accuracy of prostate-specific Antigen and Digital Rectal Examination in the diagnosis of prostate Cancer at the University of Benin Teaching Hospital. J West Afr Coll Surg. 2023;13(3):91–5.
Heijnsdijk EA, de Carvalho TM, Auvinen A, Zappa M, Nelen V, Kwiatkowski M, et al. Cost-effectiveness of prostate cancer screening: a simulation study based on ERSPC data. J Natl Cancer Inst. 2015;107(1):366.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71(4):618–29.
Weight CJ, Kim SP, Jacobson DJ, McGree ME, Karnes RJ, Sauver JS. Men (aged 40–49 years) with a single baseline prostate-specific antigen below 1.0 ng/mL have a very low long-term risk of prostate cancer: results from a prospectively screened population cohort. Urology. 2013;82(6):1211–9.
Ellison L, Cheli CD, Bright S, Veltri RW, Partin AW. Cost-benefit analysis of total, free/total, and complexed prostate-specific antigen for prostate cancer screening. Urology. 2002;60(4):42–6.
Littrup PJ, Goodman AC, Mettlin CJ. The benefit and cost of prostate cancer early detection. Cancer J Clin. 1993;43(3):134–49.
Benoit RM, Grönberg H, Naslund MJ. A quantitative analysis of the costs and benefits of prostate cancer screening. Prostate Cancer Prostatic Dis. 2001;4(3):138–45.
Acknowledgements
Not applicable.
Funding
This research received no external funding sources. It was conducted as part of a PhD thesis supported by the Health Management and Economics Research Center affiliated with Iran University of Medical Sciences (Project No. 97–4–37–16524, Ethical Code: IR.IUMS.REC.1398.911).
Author information
Authors and Affiliations
Contributions
The study was conceptualized and executed by HF, who designed the model, collected necessary data, and conducted the analysis. AR and NM provided oversight for the economic evaluation structure, while AA, NM, and AR served as economic expert panel members. Clinical expertise was contributed by SMKA and AM, who served as clinical expert panel members. Data analysis and result interpretation were carried out by HF and AA. HF took the lead in drafting the manuscript, and the final version received input, approval, and contributions from all team members. Each author takes personal accountability for their contributions and commits to addressing any concerns about the accuracy or integrity of the work. All authors have collectively agreed to investigate and resolve any such questions and document the resolution in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farabi, H., Moradi, N., Ahmadzadeh, A. et al. A cost-benefit analysis of mass prostate cancer screening. Cost Eff Resour Alloc 22, 37 (2024). https://doi.org/10.1186/s12962-024-00553-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-024-00553-0