Abstract
Background
Many individuals suffer from normal tension glaucoma (NTG) in China. This study utilized Markov models to evaluate the cost-utility of applying many medications and surgery for mild-stage NTG when disease progression occurred at a mild stage.
Methods
A 10-year decision-analytic Markov model was developed for the cost-utility analysis of treating mild-stage NTG with surgery and increased application of medication. We hypothesized that all 100,000 samples with a mean age of 64 were in mild stages of NTG. Transitional probabilities from the mild to moderate to severe stages and the basic parameters acquired from the CNTGS were calculated. Incremental cost-utility ratios (ICUR) were calculated for treating all patients with NTG by probabilistic sensitivity analysis (PSA) and Monte Carlo simulation. One-way sensitivity analysis were conducted by adjusting the progression rate, cost of medications or trabeculectomy, cost of follow-up, and surgical acceptance rate.
Results
The ICUR of treating mild stage NTG with medication over 10 years was $12743.93 per quality-adjusted life years (QALYs). The ICUR for treating mild stage NTG patients with a 25% and 50% surgery rate with medication were $8798.93 and $4851.93 per QALYs, respectively. In this model, the cost-utility of treating NTG was sensitive to disease progression rate, surgical treatment rate, and medication costs.
Conclusions
According to the results of the cost-utility analysis, it was a reasonable and advantageous strategy to administer a lot of medication and surgery for NTG in the mild stages of the disease. In the model, the greater the probability of patients undergoing surgery, the strategy becomes more valuable.
Similar content being viewed by others
Background
Glaucoma is the primary cause of irreversible blindness worldwide, affecting approximately 76 million people by 2020 and over 111 million by 2040 [1]. The prevalence of glaucoma varies between 2.3 and 3.6% in the Chinese population [2]. In China, primary glaucoma is estimated to affect 9.4 million people aged 40 years and above, with 5.2 million blind in at least one eye and 1.7 million blind bilaterally [3]. Primary open-angle glaucoma (POAG) is the most common type prevalent in Africans and Caucasians [4]. However, several population-based studies demonstrated that the age-adjusted rate of Chinese POAG was similar to that of Western countries [5].
Normal tension glaucoma (NTG), which is generally defined as individuals with glaucomatous optic nerve cupping and field loss accompanied by normal intraocular pressure (IOP) [6], constitutes a significant proportion of POAG [7]. The Collaborative Normal-Tension Glaucoma Study (CNTGS), a large multicenter clinical trial, reported that a 30% IOP reduction could delay the visual field (VF) progression of NTG [8]. The Low-pressure Glaucoma Treatment Study (LoGTS) reported that VF loss was significantly less likely to occur in treated NTG [9]. Currently, IOP reduction is the predominant strategy for delaying the progression of NTG. In the United States, the total annual healthcare costs for one POAG patient range from $1570 to $2070 [10], and the direct medical costs for glaucoma exceeded $2.9 billion [11]. Glaucoma imposes a significant economic burden on families and society and reduces the patient’s quality of life [12].
According to Tang’s study [13], medications were assumed to be prescribed to patients with mild POAG in China. Patients with severe or moderate POAG were assumed to be treated by trabeculectomy. This was the current method of treatment. The average cost of initial treatment and follow-up for treatment for mild stage POAG was $256, while for moderate and severe stages, it was $345 and $230. In our study, this treatment method was regarded as the traditional method.
According to the CNTGS study, a 30% initial sustained baseline IOP reduction is a preferable treatment approach for minimizing costs and disease development, and medication and surgery are the primary methods for decreasing the IOP treatment by 30%. Patients are more willing for medication than surgery in the Chinese population. A substantial amount of medication was required to maintain a 30% reduction in baseline IOP. Nonetheless, medication adherence was insufficient to control the progression of NTG [14]. Although surgery cost much more in the first year, the therapeutic efficacy was satisfying and long-lasting [15].
In our study, the intervention consisted of administering several medications and undergoing surgery for NTG when the disease progresses to a mild stage, which was defined as a positive treatment method. To improve patient’s quality of life and balance the use of healthcare resources, the Markov model for analytical cost-utility analysis (CUA) was used to compare the positive treatment approach with the conventional treatment approach. Utility values can be used to calculate quality-adjusted life years (QALYs), which quantitatively represent the patient’s quality of life. The Markov model is a common model to perform CUA for decision-making [13].
In the Chinese population, no cost-utility analysis has demonstrated whether treating NTG by decreasing IOP by 30% from baseline was reasonable. For developing health care policy and allocating health care resources for glaucoma management, consideration of the economic burden of NTG and its impact on the quality of life and the treatment strategy for NTG was crucial. The purpose of this study was to use the Markov model to conduct a CEA of positive treatment methods, particularly trabeculectomy in China.
Methods
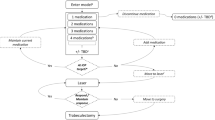
Because the probability of progression over 10 years was projected from the CNTG study results[16], in this study, a 10-year Markov decision model was developed using Excel (Microsoft, 2019). We hypothesized that all 100,000 NTG samples aged 64 were in the mild stage of the disease. In this model, every subject in the cohort was enrolled with progression risks, medical-related costs, and the benefits associated with each treatment, and their health status changed as the disease progressed. The model included three stages of NTG, ranging from mild to moderate to severe, and each stage was associated with mortality, as shown in Fig. 1. The cycle stage of the model was set at one year, and Monte Carlo simulation, random sampling, and trials were performed. Cost and quality-adjusted life years (QALYs) were calculated for each patient as the disease progressed through this model. A half-cycle [] correction was applied to both costs and benefits [17]. In this study, 100,000 samples were run for each path in the Markov cycle tree for Probabilistic sensitivity analysis [13, 18]. According to Lee et al., the surgical rates in POAG ranged from 28.4% to 34.9% [19], the percentage of treating NTG by trabeculectomy instead of medication therapy was estimated to be between 25 and 50%. Considering the surgical failure rate and the fact that some postoperative patients require medication and maintenance, we set PSA running with five times and ten times the surgery cost improves the model’s fault tolerance.
The Incremental cost-utility radios (ICUR) calculation formula is as follows:
ICUR was the primary outcome of comparing the two treatments (traditional and positive treatment methods, as indicated in the introduction) used in this study. And ICUR was later compared against the countries’ willingness to pay threshold, set at 1 GDP per capita. The per capita gross domestic product (GDP) for China was estimated to be $12692.90 in 2023, according to China’s statistical data. If ICUR was less than GDP, the favorable treatment approach was considered worthwhile. If ICUR was less than three times GDP, the positive treatment option was evaluated for clinical application [20].
Ethical statement
This article compiled published articles for data analysis and does not include any studies involving humans/animals/plants. Therefore, informed consent was waived after institutional review board (IRB) approval. This study was a secondary analysis of data from other studies (references 20, 24, 42) that are publicly available, and it did not require ethical approval.
Markov model: medical aspect
As POAG is a long-term, chronic disease, no study directly reported the transition probability of each stage every year. However, according to the findings of CNTGs [16], the 5-year progression rate for patients receiving mild treatment (aimed to lower IOP by 30% from initial) was 20%. At five years, the progression rate of NTG was 20% in the treated group and 60% in the observation group, similar to the 66% reported in Rei’s study [21] for Japanese patients. Therefore, we can calculate transition probability for each stage every year based on the formula rate: Multi-year probabilities to rates via the formula rate = − Ln (1—t-year probability) / t years, and then calculate the 1-year probabilities through 1-year probability = e(− rate ∗ 1), where t > 1, we determined that the 1-year progression rate was 4%. Then, we set the baseline MD score to be approximately − 5.9 dB, and the mean MD slope of progression was 0.9 dB/y [22]. After that, the transition probability matrix from mild to moderate and moderate to severe stages can be obtained over 10 years (Table 1). The final application of the formula rate of multi-year probabilities was to obtain the transition rate for different stages every year; it was 8.5%/y for mild to moderate and 3.5%/y for moderate to severe. Mild, moderate, and severe stages were defined by Humphrey mean deviation (MD) values between − 0.01 to − 6 dB, − 6.01 to − 12 dB, and − 12.01 to − 20 dB, respectively [23]. This represented the transition probability of the treatment for lowering IOP by 30% from the initial level.
The time horizon set for modeling was set at 10 years. The frequency of continuous follow-up visits was recommended by the American Academy of Ophthalmology Preferred Practice Pattern [24]. When patients were in the mild stage, both the treatment and observation groups had two follow-up visits, including a Visual field test (VF), Optical Coherence Tomography (OCT), Disc photography (DP), Slit-lamp bio-microscopy and Non-contact Tonometer, and three follow-up visits (including VF, OCT, and DP) when the disease progressed and in the remaining years.
To calculate quality-adjusted life years (QALYs), utilities for each glaucoma stage were estimated. The utility was a preference-based measure of the quality of life-related to a healthy state. Following the Hodapp Anderson-Parrish (HAP) classification criteria, stage utilities were presumed to be 0.80 for people with mild POAG, 0.75 for those with moderate POAG, and 0.71 for those with severe POAG [25].
The plan for traditional treatment method was a follow-up for mild NTG. Patients with moderate or severe NTG were presumed to be treated with trabeculectomy and postoperative medications for six weeks. Among them, 20% were assumed to fail the surgery and require long-term topical medical therapy, and the mild-to-moderate rate was 14.9%/y, and the moderate-to-severe was 5.6%/y, according to Tang’s study [13]. According to the findings of Cheng’s study, timolol and latanoprost were the two most effective IOP-lowering agents in NTG patients, assuming that patients would need dual therapy and some would require triple therapy to achieve target IOP [26, 27]. As per the Ocular Hypertension Treatment Study, the ratio of patients who were prescribed two (timolol and latanoprost) vs. three (Azopt, latanoprost, and Alphagan) medicines was 3:1 [18, 28] For the rest of the years, if the disease progresses persistently, 1.5 times of the normal dosage of medicine would be prescribed. For surgery, trabeculectomy, as the classic surgery [15] was chosen as the optimal method. Patients whose IOP were unstable after surgery would receive two (timolol and latanoprost) or three (Azopt, latanoprost, and Alphagan) medicines assumed 3:1. All costs for medication, surgery, and examination were collected in Chinese yuan but converted into US dollars using the 2021 China Statistical Yearbook exchange rate of 7.04 yuan per dollar.
Markov model: economic aspect
This study only considered the direct costs from the payer’s perspective. The input included diagnostic tests, medication, and trabeculectomy. The costs for the medications and surgeries (Table 1) were obtained from the tertiary hospital-Huzhou Eye Hospital. These costs are regulated by the Chinese Government and vary little among institutions within the same tier of the healthcare system. Annual medication consumption was estimated based on an analysis by Rylander [29], which included the number of drops per milliliter and common dosing patterns. All costs were given in US dollars using the average 2023 exchange rate (1 US dollar = 7.04 RMB) [30]. Following the National Institute for Health and Care Excellence (NICE) recommendations [31], all costs were discounted at a rate of 3.5% per year, and utility was discounted at the same rate. Major input parameters of the current Markov Model are listed in Table 1, and all the costs of NTG patients are summarized in Table 2. Because the cost of initial and consecutive treatment was acquired from Tang’ study in 2019 [13], we recalculated the cost up to 2023 at 3.5% increase rate per year.
Statistical analysis
We set the surgery rate at 50% and then performed one-way analyses for the Markov model by varying the vital input in a positive treatment method. Based on the complication or failure rate of surgery and medication, ± 20% change cost was calculated. The probability of disease state transfer in response to positive treatment was unstable, with a calculated change rate of ± 50%. [21] Probabilistic sensitivity analysis was also performed. As the standard deviation for a cost input, utility, and translation rate was missing, we assumed that 10% of the standard deviation was based on the mean value. The presumed variation range and distributions for transitional probabilities, cost, and utility are shown in Additional file 1: Appendix 1, 2 and 3.
Results
The ICUR of treating mild stage NTG with medication over 10 years was $12743.93 per quality-adjusted life years (QALYs). The ICUR for treating mild stage NTG patients with a 25% and 50% surgery rate with medication were $8798.93 and $4851.93 per QALYs, respectively. The results of one-way sensitivity analyses at 50% surgery rate with medication strategy are shown in Table 3, and Fig. 2 displays the top three related factors for this model. Table 4 represents the PSA results of running the model with 5 and 10 times the surgery cost, the ICRU with surgery rate set at 25% were $10567.80 and $12780.13, respectively. When the surgery rate was set at 50%, the ICRU were $8391.67 and $12816.40, respectively.
Tornado plot of 10-year accumulated incremental costs of the effectiveness of one-way sensitivity analysis. Low-value scenario: Surgery rate 25%; Transfer probability from mild to moderate NTG decrease 50%; Cost of eye drops decrease 20%. High-value scenario: Surgery rate 50%; Transfer probability from mild to moderate NTG increase 50%; Cost of eye drops increase 20%
Discussion
In NTG, decreasing IOP was significantly more strongly associated with progressive axonal loss and retinal ganglion cell damage [18]. In a natural disease state, the progression rate and visual field loss are low; consequently, many patients do not consider this condition seriously enough to seek treatment. However, without appropriate and long-term treatment, the disease progressed more rapidly in 60% of patients compared to 20% of those who received treatment [22]. Consideration of the economic burden of NTG and its impact on quality of life was crucial for the development of health care policy and allocation of health care resources for glaucoma management. The purpose of this study was to use the Markov model to perform CUA of positive treatment methods, particularly trabeculectomy in China.
Our study showed an incremental cost-utility ratio (ICUR) of $12743.93 per QALYs when comparing the positive treatment method by medication to the conventional treatment method. The ICUR for treating NTG patients with a 25 and 50% rate for surgery with medication was $8798.93 and $4851.93 per QALYs, respectively, indicating that increasing the rate of trabeculectomy therapy would be a very worthwhile strategy, consistent with the findings of the previous study [32]. Specifically, in Li’s model [18], it was cost-effective to treat NTG patients with a mild treatment (medication or surgery). Considering the gradual progression of NTG, medication is more expensive, whereas trabeculectomy ensures greater efficacy [33] while avoiding the need for long-term treatment, thereby reducing cost. Similar to Li’s study, the cost-effectiveness decision in our models for NTG was sensitive to the progression of NTG, the costs of eyedrops, trabeculectomy, and follow-up, along with the trabeculectomy rate [18]. At the same time, we set up 5 and 10 times the cost of surgery into the model, and the results still indicated that surgery is a worthwhile choice strategy. This indicated that the positive treatment method, especially surgery in our model, has a very high fault tolerance in the event of surgical failure or subsequent treatment.
Surgery would be recommended for glaucoma patients. However, medication seems convenient for patients. According to research, the number of medications, their prolonged use, and exposure to preservatives are risk factors for the development of ocular surface disease in glaucoma patients [34]. According to Wiafe’s report [32], considering the lack of resources and competing for opportunity costs, lifelong medical therapy was impractical. Additionally, medicines were mainly found in pharmacies in large cities, so patients in rural or remote areas could not procure them easily. Medication adherence was unsatisfactory (about 20%) in a developed country [14]. It was reported that the daily cost of an eye drug such as latanoprost was US $0.87 in the developed world [35] and possibly even more in developing countries. Surgery was the cost-effective treatment for the mild stage of glaucoma patients [36]. The cost of surgery to reduce intraocular pressure has decreased over time. The cost is higher during the first three years, but when considering the number of years people live and the cost of drugs for those years, surgery is a relatively worthwhile treatment option in developing countries.
As it was a simulated study and with the analogy to many other cost-effectiveness analyses, there are several limitations to our model. Firstly, only direct costs were considered. Indirect costs such as patient’s time spent attending follow-up appointments and lost productivity due to time off were not considered. However, we can disregard this because our model set the age at 64. Additionally, patient compliance was not considered in this study, which would affect the medication cost. However, this had little effect on our model because our results indicated that surgery may be more effective.
Conclusions
This was the first study to provide economic evidence on how to treat Chinese NTG patients cost-effectively. A better understanding of risk factors and treatment options for glaucoma patients would be helpful in improving patient’s health-related quality of life and optimizing resource allocation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- NTG:
-
Normal tension glaucoma
- VFL:
-
Visual field loss
- IOP:
-
Intraocular pressure
- CNTGS:
-
Collaborative normal-tension glaucoma study group
- ICUR:
-
Incremental cost-utility ratios
- PSA:
-
Probabilistic sensitivity analysis
- QALYs:
-
Quality-adjusted life years
- POAG:
-
Primary open-angle glaucoma
- LoGTS:
-
Low-pressure glaucoma treatment study
- VF:
-
Visual field
- OCT:
-
Optical coherence tomography
- DP:
-
Disc photography
References
Tham Y-C, Li X, Wongi TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040 a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–90.
Wei Qu, Li Y, Song W, et al. Prevalence and risk factors for angle-closure disease in a rural Northeast China population: a population-based survey in Bin County. Harbin Acta Ophthalmol. 2011;89(6):515–20.
Quigley HA. Broman AT: the number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–7.
Buhrmann RR, Quigley HA, Barron Y, et al. Prevalence of glaucoma in a rural East African population. Invest Ophthalmol Vis Sci. 2000;41(1):40–8.
He M, Foster PJ, Ge J, et al. Prevalence and clinical characteristics of glaucoma in adult Chinese: a population-based study in Liwan District Guangzhou. Invest Ophthalmol Visual Sci. 2006;47(7):2782–8.
Werner E, Spaeth G, Douglas G. Progressive normal-tension glaucoma. I Anal J Glaucoma. 1996;5(6):422–6.
Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006;113(9):1613–7.
Schulzer M, Alward WL, Feldman F, et al. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126(4):487–97.
Krupin T, Liebmann JM, Greenfield DS, et al. A randomized trial of brimonidine versus timolol in preserving visual function: results from the low-pressure Glaucoma treatment study. Am J Ophthalmol. 2011;151(4):671–81.
Pasquale LR, Dolgitser M, Wentzloff JN, et al. Health Care Charges for Patients with Ocular Hypertension or Primary Open-angle Glaucoma. Ophthalmology. 2008;115(4):633–8.
Rein DB, Zhang P, Wirth KE, et al. The economic burden of major adult visual disorders in the United States. Arch Ophthalmol. 2006;124(12):1754–60.
McKean-Cowdin R, Wang Y, Wu J. Impact of visual field loss on health-related quality of life in glaucoma: the Los Angeles Latino Eye Study. Ophthalmology. 2008;115(6):941–8.
Tang J, Liang Y, O’Neill C, et al. Cost-effectiveness and cost-utility of population-based glaucoma screening in China: a decision-analytic Markov model. Lancet Global Health. 2019;7(7):968–78.
Newman-Casey PA, Blachley T, Lee PP. Patterns of glaucoma medication adherence over four years of follow-up. Ophthalmology. 2015;122(10):2010–21.
Shigeeda T, Tomidokoro A, Araie M, et al. Long-term follow-up of visual field progression after trabeculectomy in progressive normal-tension glaucoma. Ophthalmology. 2002;109:766–70.
Group CN-TGS. Comparison of Glaucomatous Progression Between Untreated Patients With NormalTension Glaucoma and Patients With Therapeutically Reduced Intraocular Pressures. Am J Ophthalmol. 1998;126(4):487–97.
Brigg A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13(4):397–409.
Li EY, Tham CC, Chi SC, et al. Cost-effectiveness of treating normal tension glaucoma. Invest Ophthalmol Vis Sci. 2013;54(5):3394–9.
Lee PP, Kelly SP, Mills RP, et al. Glaucoma in the United States and Europe: predicting costs and surgical rates based upon stage of disease. J Glaucoma. 2007;16:471–8.
Hutubessy R, Chisholm D, Edejer TT. Generalized costeffectiveness analysis for nationallevel prioritysetting in the health sector. Cost Eff Resour Alloc. 2003;1:8.
Sakata R, Yoshitomi T, Iwase A, et al. Factors associated with progression of Japanese open-angle glaucoma with lower normal intraocular pressure. Ophthalmology. 2019;126(8):1107–16.
Anderson DRDS, Schulzer M. Natural history of normal-tension glaucoma. Ophthalmology. 2001;108:247–53.
Sun X, Zhang S, Wang N. Utility assessment among patients of primary angle closure/glaucoma in China: a preliminary study. Br J Ophthalmol. 2009;93(7):871–4.
Edlin R, McCabe C, Hulme C, Hall P, Wright J. Cost effectiveness modelling for health technology assessment. 2015. https://doi.org/10.1007/978-3-319-15744-3.
Burr JM, Mowatt G, Hernandez R, et al. The clinical effectiveness and costeffectiveness of screening for open angle glaucoma:a systematic review and economic evaluation. Health Technol Assess. 2007;11(41):1–190.
Cheng J-W, Cai J-P, Wei R-L. Meta-analysis of medical intervention for normal tension glaucoma. Ophthalmology. 2009;116:1243–9.
Garway-Heath DF, Crabb DP, Bunce C, et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385(9975):1295–304.
Stewart WC, Stewart JA, Nassar QJ, et al. Cost-effectiveness of treating ocular hypertension. Ophthalmology. 2008;115(1):94–8.
Nathan R. RYLANDER, VOLD SD: cost analysis of glaucoma medications. Am J Ophthalmol. 2008;145(1):106–13.
China TWotPsBo: http://www.pbc.gov.cn/. Accessed 23 Jan 2024.
NICE: Nice process and methods guides. Guide to the methods of technology appraisal. London: National Institute for Health and Care Excellence; 2013.
Boateng W. Economics of surgery worldwide developing countries. Glaucoma. Amsterdam: Elsevier; 2015. p. 683–6.
Gedde SJ, Feuer WJ, Lim KS, et al. Treatment outcomes in the primary tube versus trabeculectomy study after 3 years of follow-up. Ophthalmology. 2020;127(3):333–45.
Rossi GC, Pasinetti GM, Scudeller L, et al. Risk factors to develop ocular surface disease in treated glaucoma or ocular hypertension patients. Eur J Ophthalmol. 2013;23(3):296–302.
Shaarawy T, Mermoud A. Atlas of glaucoma surgery. London: Anshan Ltd; 2006. p. 7.
Ainsworth JR, Jay JL. Cost analysis of early trabeculectomy versus conventional management in primary open angle glaucoma. Eye. 1991;5(3):322–8.
Acknowledgements
This study benefitted from prior cohort research. The author gratefully acknowledges all relevant researchers for the data provided and published.
Funding
None.
Author information
Authors and Affiliations
Contributions
LW developed the research question and revised the manuscript before submission. DS conducted data analysis and drafted the first version of text. All authors participated in the development of the review process, data analysis, and text revision, and they all provided final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is a second analysis above the data from other studies (references 20, 24, and 42) which is publicly available and there is no participate and ethics approval for this study.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Appendix S1. Variation range and distributions assumed for the transitional probabilities between treatment A and treatment B. Appendix S2. Variation range and distributions assumed for Treatment A and B cost. Appendix S3. Variation range and distributions assumed for utilization. Appendix S4. Costs of Treatment in Clinical Management of Normal Tension Glaucoma. Appendix S5. Estimates for utility, mortality, and other parameters.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, D., Wang, L. Cost-utility analysis of treating mild stage normal tension glaucoma by surgery in China: a decision-analytic Markov model. Cost Eff Resour Alloc 22, 13 (2024). https://doi.org/10.1186/s12962-024-00523-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-024-00523-6