Abstract
Background
Mental illnesses account for a considerable proportion of the global burden of disease. Economic evaluation of public policies and interventions aimed at mental health is crucial to inform decisions and improve the provision of healthcare services, but experts highlight that nowadays the cost implications of mental illness are not properly quantified. The objective was to measure the costs of excess use of all healthcare services by 1- to 30-year-olds in the Basque population as a function of whether or not they had a mental disorder diagnosis.
Methods
A real-world data study was used to identify diagnoses of mental disorders and to measure resource use in the Basque Health Service Registry in 2018. Diagnoses were aggregated into eight diagnostic clusters: anxiety, attention deficit hyperactivity disorder, conduct disorders, mood disorders, substance use, psychosis and personality disorders, eating disorders, and self-harm. We calculated the costs incurred by each individual by multiplying the resource use by the unit costs. Annual costs for each cluster were compared with those for individuals with no diagnosed mental disorders through entropy balancing and two-part models which adjusted for socioeconomic status (SES).
Results
Of the 609,381 individuals included, 96,671 (15.9%) had ≥ 1 mental disorder diagnosis. The annual cost per person was two-fold higher in the group diagnosed with mental disorders (€699.7) than that with no diagnoses (€274.6). For all clusters, annual excess costs associated with mental disorders were significant. The adjustment also evidenced a social gradient in healthcare costs, individuals with lower SES consuming more resources than those with medium and higher SES across all clusters. Nonetheless, the effect of being diagnosed with a mental disorder had a greater impact on the mean and excess costs than SES.
Conclusions
Results were consistent in showing that young people with mental disorders place a greater burden on healthcare services. Excess costs were higher for severe mental disorders like self-harm and psychoses, and lower SES individuals incurred, overall, more than twice the costs per person with no diagnoses. A socioeconomic gradient was notable, excess costs being higher in low SES individuals than those with a high-to-medium SES. Differences by sex were also statistically significant but their sizes were smaller than those related to SES.
Similar content being viewed by others
Background
Mental illnesses account for a considerable proportion (10%) of the global burden of disease [1, 2]. The literature suggests that preventive interventions at early age are key to tackle adverse conditions experienced during childhood and adolescence and contribute to better levels of health in adulthood [3]. Therefore, economic evaluation of public policies and interventions aimed to reduce the burden is crucial to inform decisions about what is the best use of the limited resources available in order to maximize the health benefits [4]. Nonetheless, the cost of mental disorders is a poorly understood driver of decision-making about which interventions should be implemented in mental health [5, 6]. More economic evaluations in the field of mental illness have started to be conducted [7,8,9,10], but their limited use in decision-making contrasts with the importance placed on this type of research in the incorporation of preventive treatments and interventions in cancer and cardiovascular diseases [11,12,13]. Moreover, experts highlight that the cost implications are not adequately measured and large evidence gaps still exist regarding the economic case for mental health care [14], including inequalities by gender and socioeconomic status (SES) [6].
In this context, data are needed on excess healthcare costs associated with mental disorders for various purposes, such as conducting economic evaluations and measuring the burden [15]. To measure disease-specific burden, average costs should be disaggregated by the type of mental disorder and compared with those for similar populations without such disorders [15,16,17,18]. That is, there is a need to know not only the average cost but also the incremental cost in relation to the population without mental health diagnoses [17, 18]. In this sense, if a new intervention can modify the costs or benefits in health associated to a given mental disorder, the burden of the new scenario proposed by the intervention can be obtained and compared with the current scenario in order to guide decision-making [5, 6].
Currently, the relatively few data available are based on surveys collecting self-reported data from samples of patients with diagnoses of specific mental disorders [8, 17,18,19]. In this field, there is a lack of real-world data (RWD) studies, despite such research having been recognized by experts as a key source of information for understanding disease-specific resource use [20]. As RWD provide information on individual resource use for an entire population, analysis of these types of data makes it possible to measure population costs [21]. In turn, having population data disaggregated at the individual level, accurate unit costs can be provided to be used to estimate the economic burden of health disorders and to carry out subsequent cost analysis of interventions [3]. RWD also help explore differences in health, since groups that make greater use of health resources are generally those that have poorer health status [22, 23]. The monitoring of health disparities allows us to measure progress toward achieving health equity and social justice [24]. As people diagnosed with a mental disorder tend to use health services more than the general population, health service use may reveal trends in disparities in mental health [25, 26].
Besides mental disorders, inequities in resource use can also be associated with SES and mental disorders in populations that are strongly determined by socioeconomic characteristics [23, 27, 28]. Moreover, due to a greater vulnerability to environmental stress in the early stages of life, social determinants have more impact on children, adolescents and young adults [29, 30]. Therefore, knowing the joint impact of mental disorders and SES on healthcare costs would help to assess both, their burden and their relationship with social determinants [31].
Given all this, the objective of this study was to measure the excess use of healthcare resources and healthcare costs of people between 1 and 30 years of age in the Basque population, adjusted for SES and sex, as a function of whether or not they are diagnosed with some type of mental disorder.
Methods
A retrospective observational study was conducted to identify diagnoses of mental disorders and to measure resource use based on data from the Basque Health Service. The Basque Country is an industrialized northern region of Spain with a population of 2.2 million. In Spain, powers for managing health services are decentralised to the regions, and the health system recognises a universal right to healthcare under a Beveridge model. The Basque Health Service provides comprehensive healthcare to the entire Basque population. The protocol of the study was approved by the Clinical Research Ethics Committee of the Basque Country (number PI2019078).
The Basque Health Service registry contains information on all psychiatric and somatic inpatient and outpatient encounters (admissions and consultations), primary care contacts and emergency room visits. Diagnoses are recorded using codes from the ninth and tenth revisions of the International Classifications of Diseases (ICD-9 and ICD-10). In the study, the definition of lifetime prevalence of Kessler et al. was applied, who estimated it as the proportion of respondents who had ever been diagnosed with a given disorder up to their age at interview [32]. Based on this prevalence-based approach, we calculated, first, the resources used (primary care, mental health centres, hospitals and pharmacy) and, second, the corresponding direct costs. By merging diagnoses and resource use in the population registry, we obtained individual data for the whole population disaggregated by clusters of mental disorders.
The study population was all individuals who, as of 31 December 2018, were between 1 and 30 years old and registered with the Basque Health Service. Among this population, patients who had been diagnosed with any mental disorder at any point in their lifetime were identified by checking all lifetime episodes of primary care and hospital care. Diagnoses were aggregated into eight diagnostic clusters: anxiety (anxiety + acute stress reactions + adaptation reactions), attention deficit hyperactivity disorder (ADHD), conduct disorders, mood disorders (depression + bipolar disorder), substance use, psychosis and personality disorders, eating disorders, and self-harm. In addition, as patients from private practice seek drug reimbursement through the public system, we searched for individuals who had any relevant chronic prescriptions through Anatomical Therapeutic Chemical (ATC) codes for antidepressants (N06A group) or antipsychotics (N05A group) in individuals without a mental disorder diagnosis in the public health service records to include them in the clusters of mood disorders and psychosis respectively. In the identification process, we used the ICD-9, ICD-10 and ATC classification system codes (listed in Additional file 1: Table S1).
The variables included in the study were: age, sex and income level based on drug co-payment, and diagnosis cluster. In addition, all the resource use of the target population was extracted for the year 2018. That way, the resource use profile of the general population was estimated. Data collected in primary care included all contacts with nurses and general practitioners at healthcare centres, at home or by telephone. For hospital care, we took into account all contacts with outpatient clinics, as well as with emergency and inpatient services. All the drugs prescribed to individuals were also considered. The information about the unit costs of different healthcare resources for 2018 in euros (EUR, €) was obtained from the accounting system of the Basque Health Service (Additional file 1: Table S2) and included all types of healthcare resources [salaries, diagnosis costs (Lab, Rx), equipment, investments, infrastructure (heating, electricity, cleaning services, etc.) and pharmacy].
To assess SES, we considered drug co-payment categories which are established based on household income (Additional file 1: Table S3). The contribution levels for the co-payment of medicines in the Spanish Health System were established in 2012 based on three criteria: income, age and degree of illness. Children, adolescents and young adults were assigned the most disadvantaged SES level (low SES) if the head of their household was exempt from co-payment or was retired, the most advantaged SES level (high SES) if the head of the household had an annual income from paid work equal or higher than €18,000, and otherwise, to a third category (medium SES), for heads of household with annual incomes from paid work lower than €18,000 [27].
We calculated the costs incurred by each individual multiplying the resource use by the unit costs. As individual data were available, the cost per patient was disaggregated into primary care, hospital care and pharmacy costs for each diagnostic cluster.
Statistical analysis
In the initial step, univariate statistical analysis was performed to compare the sociodemographic features of individuals with and without mental disorders. Fisher’s exact test was used for categorical variables with two categories and expected values less than or equal to 5, and otherwise a chi-square test. In the case of age, since it is a continuous variable with a normal distribution, the comparison of means was carried out using Student’s t test.
In a second step, each diagnostic cluster was compared with the population with no diagnosed mental disorders to measure the excess cost using statistical models. In total, 10 independent statistical models were created: one for each diagnostic cluster, one for having two diagnoses or more, and one for having any mental disorder. Before developing the models, the data were pre-processed. When using nonrandomized studies to estimate costs, it must be taken into account that selection is influenced by individual characteristics. Since initial characteristics were likely to be different in the groups with and without mental disorders, they were balanced to ensure that they were comparable in terms of initial characteristics (age group, sex and SES) and independent of background characteristics. For that purpose, an entropy balancing technique was used to adjust the covariate distribution of the group with no diagnosed mental disorders by reweighting. This technique is based on a maximum entropy reweighting scheme and allows the pre-processing of data in observational studies with binary variables of interest [18, 33]. The technique reweighted the data from no diagnosed mental disorders units to match a set of moments that was computed from the data from the group with mental disorders. Hence, the covariate distribution obtained was more similar to that in the group with mental disorders. In that way, the covariate distributions in the reweighted data satisfied the balance conditions specified by the research team and the resulting weights were used to carry out an analysis comparing the two groups, where confounding factors between them were removed. As ten different models were built to analyse excess costs, covariate distribution adjustment using entropy balancing was also performed once per model.
To measure the excess costs, it would not have been appropriate to use ordinary least squares regression models [34], since the costs did not follow a normal distribution and a substantial number of individuals had zero costs. Therefore, to obtain the excess costs for each mental health cluster and adjusted for the selected characteristics, regression analysis was performed using two-part models [18, 34, 35]. In the first part, the adjusted probability, p(x), that the cost was higher than zero was fitted with a logit regression model. In the second part, generalized linear models with a log link function and gamma distribution were used to calculate the mean cost values of the population with costs greater than zero. An advantage of two-part models is that their results are easy to interpret since they estimate the magnitude of the differences between groups (in our case, in costs) and not only if the compared means differ. As the estimated costs depend on the combination of the different covariates, they produce the average costs for each cluster and the adjusted excess costs.
All the statistical analyses were carried out using R (version 3.3.2) and Stata (version 14) statistical programs with a significance level of 95%. Specifically, the initial univariate statistical analysis was performed with R, which is free, while the entropy balancing and two-part models were performed with Stata, to take advantage of dedicated packages available, namely, ebalance and twopm, respectively [36, 37].
Results
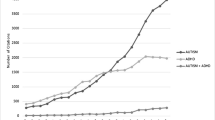
The total population in the age range between 1 and 30 years included in the Basque Health Service database contained 609,381 individuals, of which 96,671 (15.9%) had been diagnosed with at least one mental disorder at some point in their lifetime (Table 1). The SES distribution confirmed the social gradient in mental disorders, the prevalence rising from low SES to medium and high SES groups (also in Table 1). The lifetime prevalence of mental disorders and the use of resources in the population studied disaggregated by diagnostic cluster are presented in Table 2 and Additional file 1: Table S4 disaggregated by cluster. They show that the gradient according to SES is a pattern repeated in all the diagnostic clusters. Anxiety was the most prevalent type of mental disorder, diagnoses in this cluster being recorded in 6.6% of the population under 30 years. Individuals with more than one diagnosis appear in various clusters. Among the entire population with mental disorders, 20% had two or more diagnoses. Notably, Table 2 shows the greater use of healthcare resources by people with diagnosed mental disorders. Their rate of admission to psychiatric wards was higher (0.7%) than that in people with no diagnoses (0.0%). But notably their rate of admission to general wards was also nearly two-fold higher (5.4% versus 2.8% in the population with no diagnosed mental disorders). Individuals with mental disorders also incurred noticeably higher annual drug prescription costs (€115.6 versus €33.7).
The annual costs per person disaggregated by diagnostic group and cost component are listed in Table 3 and Additional file 1: Table S5. Hospital costs represented three quarters of the total cost. As patients with more than one diagnosis may be included in various clusters, the overall mean does not match the weighted average of the clusters. The total healthcare cost per person in the diagnosed group (€699.7) was more than twice that in the group with no diagnoses (€274.6). The clusters that consumed the most resources were self-harm, with mean costs of €4543.7, followed by psychosis and personality disorders with costs of €2359.8 and mood disorders with costs of €1874.7.
For all the models developed, the balance achieved by entropy balancing (Additional file 1: Tables S6–15), the two-part models with their parameters (Additional file 1: Tables S16–25) and the results on mean and excess cost of the combined statistical analysis are provided in the supplementary material (Additional file 1: Tables S26–35). To summarise our results here, we present the mean and excess costs per patient by diagnostic cluster and disaggregated by SES in Table 4, sex in Table 5 and age-group in Table 6. For all clusters, annual excess costs in the groups of patients with mental disorders were more than double those in the groups with no diagnosed mental disorders. Tables 5, 6 also show the differences in adjusted costs by sex and age group. For all clusters, annual excess costs were higher in women than in men. Disaggregation by age group did not render a fully consistent pattern, but in general, younger age groups incurred lower excess costs.
Discussion
To our knowledge, this is the first study showing individual excess costs of persons with mental diagnoses and adjusted for SES and sex covering a general population of 609,381 individuals younger than 30 years old. Children, adolescents and young adults diagnosed with mental disorders used health services more and this implied a high excess cost, the annual cost per diagnosed person being, overall, more than twice the cost per person with no diagnoses. A socioeconomic gradient was notable, excess costs being higher in individuals with low SES than those with high-to-medium SES. The low SES category (7.8%) grouped the adolescents and young people in households with no income with those whose health cardholder was on benefits and exempt from payment or retired regardless of their income (i.e., with an income lower or higher than €18,000). The rationale for this can be seen in Additional file 1: Table S3 which shows that adolescents and young people depending on a retired cardholder had a higher prevalence of mental disorders (24.2% and 20.5%) and consistent with SES relying not only on income but also on family structure. Differences by sex were also statistically significant but their sizes were smaller than those related to SES. Our cluster-disaggregated prevalence results for 18-year-olds are consistent with those described in Denmark in a population registry base study [38].
The healthcare costs were comprehensive as they included hospital care, primary care and pharmacy. Roughly three quarters of the costs per patient were hospital-related costs, which included those for emergency services and specialized outpatient clinics as well as hospital ward admissions. In another registry-based study, Christensen et al. estimated the total healthcare cost of all persons living in Denmark with a diagnosis of mental disorder [39]. When comparing with their mean annual healthcare costs, as would be expected for a country with lower salaries, our annual costs were in a lower range, but the ratio between the annual healthcare costs in diagnosed and non-diagnosed individuals was roughly three in both studies. When analysing the results on annual excess healthcare costs, they also found that schizophrenia and drug use disorders incurred the highest ones. However, the different age range of the two populations hampered the comparison with our results as we limited our study to individuals from 1 to 30 years and the somatic burden is much higher in older cohorts [40].
On the other hand, the mean total costs were within the range of the real per capita health spending by age group in Spain estimated by top-down methods and the estimated annual costs were also quite similar in both studies [41]. The excess costs were important in all three cost components, differences in hospital costs being greater in absolute terms, but the relative difference in pharmacy was also considerable. Drug prescription costs were 3.4 times higher in the group with mental diagnoses, revealing the use of psychoactive drugs in all age groups under 30 years.
Two diagnosis clusters generated the highest costs per individual, self-harm with costs of €4543.7 and psychosis and personality disorders with costs of €2359.8. After statistical adjustment using the two-part models, they continued to be the clusters with the highest average and highest excess costs. When disaggregating by SES, the social gradient is reflected in the statistical models and the top figure of €6,302 was obtained for the self-harm cluster in the low SES group. The differences by SES are striking in all the clusters and especially between, on the one hand, low SES, and, on the other, medium and high SES categories (Table 2 and Additional file 1: Table S4) [42]. At this point it is important to remark that, as long as universal coverage is provided, any citizen has guaranteed access to health services. Nevertheless, it is possible that differences found may undervalue the whole reality when looking to the literature. Findings that children from low SES families respond more strongly to cost sharing policies such as co-payments [43], acting as a barrier when seeking healthcare assistance, suggest that there can be an underestimation in this group. Moreover, social and cultural factors like stigma and negative perceptions surrounding mental illness can also influence the use of healthcare system, especially conditioning the access of the most vulnerable groups [44]. Therefore, actual differences between SES groups could even increase.
When looking over the effect of sex, the total spending by females is greater than by males in coherence with the literature [45, 46]. In the same way, the analyses revealed that, in terms of excess cost, women’s also had higher numbers in each diagnostic cluster. The higher total and excess costs found in females can be explained because women tend to use more the healthcare services in general [45, 46]. There are differences in cluster prevalence by sex, but they did not bias the excess cost calculation thanks to the adjustment achieved with the two-part models.
It is noteworthy that individuals with mental disorders incurred higher costs not only for mental healthcare but also for somatic healthcare. A similar pattern of use has been found elsewhere among under 18-year-olds diagnosed with a mental disorder [47]. In adults, the higher resource use has been partially attributed to chronic comorbidities [48], but specific explanations are required for young people with very few chronic physical conditions. As suggested by the literature, a possible justification can be that the presence of a mental disorder was associated with an increased risk of subsequent medical conditions [49]. Different studies also indicate that parental coping with a mental illness is related to the mental health of their children [50,51,52], as well as with the increase in their healthcare services use [53, 54]. However, it must be taken into account that people with mental health disorders are a heterogeneous group with different health and social needs, where the drivers of their higher resource use are likely to be multifactorial [48]. It must also be considered that healthcare use and cost estimates in adolescents and young adults may be underestimated, as long as practitioners can be reluctant to diagnose certain disorders, especially more severe ones, until the patient reaches an older age [55, 56]. Therefore, initiatives should be developed to improve early recognition and mental health support for young people, seeking both to improve their care and potentially reduce inappropriate care and costs [57].
The availability of data on the excess costs of mental disorders opens an opportunity for undertaking studies on the effectiveness and cost-effectiveness of preventive interventions in adolescents [3]. In particular, reducing the incidence of self-harm, psychoses and personality disorders and mood disorders should be considered a public health priority, because these disorders are associated with disability, and also have serious economic consequences. The relevance of these findings is underlined by the effect of the coronavirus disease 2019 pandemic on the mental health of adolescents and has major implications for prevention planning [58, 59]. Preventive interventions for self-harm and suicide must be included in the guidelines to safeguard the mental health of adolescents and young adults affected by the pandemic and the measures restricting social mobility, with a focus on measures to mitigate anxiety, depression, and stigma, among other conditions.
Limitations and strengths
Our study was carried out from the perspective of the health system and therefore our data lack the weight of other categories such as social, judicial and educational costs. We acknowledge that a fully comprehensive approach to estimating the burden of mental disorders must incorporate a societal perspective by covering all cost categories assessed in top-down cost-of-illness studies such as data on crime, accidents and social care [17, 60]. Moreover, informal costs due to caregivers’ time should be accepted as part of the economic burden of mental disorders but so far these key components are not recorded in registries [61]. Our figures for excess costs would have been even higher if those cost categories had been measured [18]. Further, while the economic impact of informal care is important, so is the suffering and loss of quality of life of siblings who endure the care of children, adolescents and young adults with mental disorders [61]. Wittenberg et al. described this situation highlighting “health as a family affair” [61].
Another limitation of the study was the lack of validation of the diagnoses. As in other observational studies, the cohort effect may bias the results [38]. Our dataset is based on the integration of information on all the diagnoses of individuals recorded in the electronic health record of the public health service in their contacts with primary, hospital inpatient, emergency and outpatient care. This approach yielded consistent results in the diagnosis of dementia in various European countries [62]. In the Basque Country, nearly universal health coverage is provided, but in the age range studied, 20% of the population also have private insurance. This cost component is absent in our database and therefore its size was not considered. The percentage of high-income individuals with double coverage (public and private) is greater in high SES people, and they may opt to use private rather than public providers, and hence, the differences by SES may be biased [63]. The lack of adjustment for comorbidities was also a potential limitation. Nonetheless, in these early stages of life, social determinants have a greater impact on health than physical chronic conditions [29]. Finally, another limitation of the study was the definition of the different clusters of mental disorders. Our approach to classifying mental disorders roughly followed the categories defined by Dalsgaard et al. for the same purpose also using ICD-10 codes and a population registry [38]. In contrast, self-reported symptoms in surveys are converted into codes from the successive versions of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), to estimate prevalence indicators [32].
Besides its limitations, our study has important strengths. As the data were derived from a population-based registry covering the whole population, it provides a recent and comprehensive estimate of the direct medical costs for a population of more than half a million individuals under 30 years of age. Furthermore, the registry contained the contacts with healthcare providers in all the public settings in the Basque Country. A similar approach has been successfully applied in Denmark to estimate incidence rates of mental disorders [38, 64]. The joint use of Basque administrative and clinical databases allowed us to obtain population-based cost estimates across the entire healthcare system avoiding the selection bias associated with small samples from psychiatric settings. Another strength is the availability of all contacts to measure the resource use at the patient level directly, instead of relying on patient-reported healthcare use or top-down approaches [7, 16, 17, 65].
The current availability of information from electronic health records enables the undertaking of observational studies based on RWD that allow the measurement of actual resource use and costs. Nevertheless, the high external validity of these types of study may be weakened given their non-random design, where the baseline characteristics of the groups to be compared can differ due to selection bias. To overcome this issue, pre-processing techniques like entropy balancing or propensity score matching are crucial to adjust the covariate distribution of the control group by the reweighting or discarding of units [33, 66, 67]. Such techniques make the distribution more similar to the one in the comparison group. In this case, entropy balancing was used to carry out this task. In contrast to other pre-processing methods, this technique tackles the adjustment problem backwards and estimates the set of weights that satisfies the balance constraints that involve the first, second and higher moments of the covariate distributions as well as interactions. Because of that, a high degree of covariate balance can be obtained. Moreover, since entropy balancing weights show smooth variation across units, its appeal lies in its capacity to optimize the balance in the covariate distribution while retaining the maximum amount of information. Finally, compared to other techniques like propensity score matching, it can be faster computationally speaking, it being possible to obtain the weights within a few seconds even in large databases.
Conclusions
This study provides estimates of the excess economic costs of mental disorders for the first time in the Spanish population between 1 and 30 years of age based on a general population registry. Results are consistent in showing that young people with mental disorders place a greater burden on healthcare providers compared to population without mental disorders, and that the costs are especially high for severe mental disorders like self-harm and psychoses. Additionally, the results on excess healthcare costs obtained may facilitate future economic evaluations of interventions targeting adolescents and young adults, supporting decision-making in order to improve the provision of mental healthcare services.
Availability of data and materials
Data were provided by the Basque Health Service. Our data sharing agreement stipulates that they cannot be shared with any third party.
Abbreviations
- RWD:
-
Real-world data
- SES:
-
Socioeconomic status
- ADHD:
-
Attention deficit hyperactivity disorder
- ATC:
-
Anatomical therapeutic chemical
- ICD:
-
International classifications of diseases
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease study 2019. Lancet. 2020;396:1204–22.
Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease study 2010. PLoS ONE. 2015;10:e0116820.
Las Hayas C, Izco-Basurko I, Fullaondo A, Gabrielli S, Zwiefka A, Hjemdal O, et al. UPRIGHT, a resilience-based intervention to promote mental well-being in schools: study rationale and methodology for a European randomized controlled trial. BMC Public Health. 2019;19:1413.
Neumann PJ, Ganiats TG, Russell LB, Sanders GD, Siegel JE, editors. Cost-effectiveness in health and medicine. New York: Oxford University Press; 2016.
Knapp M. Economic evaluations and interventions for children and adolescents with mental health problems. J Child Psychol Psychiatry. 1997;38:3–25.
Knapp M, Wong G. Economics and mental health: the current scenario. World Psychiatry. 2020;19:3–14.
Shearer J, Byford S. The basics of economic evaluation in mental healthcare. BJPsych Adv. 2015;21:345–53.
Smit F, Cuijpers P, Oostenbrink J, Batelaan N, de Graaf R, Beekman A. Costs of nine common mental disorders: implications for curative and preventive psychiatry. J Ment Health Policy Econ. 2006;9:193–200.
Le LK-D, Esturas AC, Mihalopoulos C, Chiotelis O, Bucholc J, Chatterton ML, et al. Cost-effectiveness evidence of mental health prevention and promotion interventions: a systematic review of economic evaluations. PLoS Med. 2021;18:e1003606.
Mihalopoulos C, Chatterton ML. Economic evaluations of interventions designed to prevent mental disorders: a systematic review. Early Interv Psychiatry. 2015;9:85–92.
Arrospide A, Rue M, van Ravesteyn NT, Comas M, Soto-Gordoa M, Sarriugarte G, et al. Economic evaluation of the breast cancer screening programme in the Basque Country: retrospective cost-effectiveness and budget impact analysis. BMC Cancer. 2016;16:344.
Soto-Gordoa M, Arrospide A, Moreno-Izco F, Martínez-Lage P, Castilla I, Mar J. Projecting burden of dementia in Spain, 2010–2050: impact of modifying risk factors. J Alzheimers Dis. 2015;48:721–30.
Arrospide A, Ibarrondo O, Castilla I, Larrañaga I, Mar J. Development and validation of a discrete event simulation model to evaluate the cardiovascular impact of population policies for obesity. Med Decis Making. 2022;42:241–4.
Caldwell DM, Davies SR, Thorn JC, Palmer JC, Caro P, Hetrick SE, et al. School-based interventions to prevent anxiety, depression and conduct disorder in children and young people: a systematic review and network meta-analysis. Public Health Res. 2021;9:1–284.
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005.
Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy. 2009;93:85–92.
Łaszewska A, Wancata J, Jahn R, Simon J. The excess economic burden of mental disorders: findings from a cross-sectional prevalence survey in Austria. Eur J Health Econ. 2020;21:1075–89.
Dams J, Buchholz A, Kraus L, Reimer J, Scherbaum N, Konnopka A, et al. Excess costs of alcohol-dependent patients in German psychiatric care compared with matched non-alcohol-dependent individuals from the general population: a secondary analysis of two datasets. BMJ Open. 2018;8:e020563.
Parés-Badell O, Barbaglia G, Jerinic P, Gustavsson A, Salvador-Carulla L, Alonso J. Cost of disorders of the brain in Spain. PLoS ONE. 2014;9:e105471.
Garrison LP, Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR real-world data task force report. Value Health. 2007;10:326–35.
Ibarrondo O, Lizeaga G, Martínez-Llorente JM, Larrañaga I, Soto-Gordoa M, Álvarez-López I. Health care costs of breast, prostate, colorectal and lung cancer care by clinical stage and cost component. Gac Sanit. 2022;36:246–52.
Soto-Gordoa M, Arrospide A, Millán E, Calvo M, Igartua JI, Esnaola S, et al. Gender and socioeconomic inequalities in the implementation of the Basque programme for multimorbid patients. Eur J Public Health. 2019;29:681–6.
Mar J, Arrospide A, Soto-Gordoa M, Iruin Á, Tainta M, Gabilondo A, et al. Dementia-related neuropsychiatric symptoms: inequalities in pharmacological treatment and institutionalization. Neuropsychiatr Dis Treat. 2019;15:2027–34.
Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014;129(Suppl 2):5–8.
Koopmans GT, Donker MCH, Rutten FHH. Common mental disorders and use of general health services: a review of the literature on population-based studies. Acta Psychiatr Scand. 2005;111:341–50.
Tusa N, Koponen H, Kautiainen H, Korniloff K, Raatikainen I, Elfving P, et al. The profiles of health care utilization among a non-depressed population and patients with depressive symptoms with and without clinical depression. Scand J Prim Health Care. 2019;37:312–8.
Oliver-Parra A, Dalmau-Bueno A, Ruiz-Muñoz D, García-Altés A. Relationship between parents’ mental disorders and socioeconomic status and offspring’s psychopathology: a cross-sectional study. PLoS ONE. 2020;15:e0240681.
Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, et al. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. 2018;5:357–69.
Reiss F, Meyrose A-K, Otto C, Lampert T, Klasen F, Ravens-Sieberer U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: results of the German BELLA cohort-study. PLoS ONE. 2019;14:e0213700.
Appleyard K, Egeland B, van Dulmen MHM, Sroufe LA. When more is not better: the role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry. 2005;46:235–45.
Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–104.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602.
Hainmueller J. Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Polit Anal. 2012;20:25–46.
Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic evaluation in clinical trials. Oxford: Oxford University Press; 2014.
Dams J, König H-H, Bleibler F, Hoyer J, Wiltink J, Beutel ME, et al. Excess costs of social anxiety disorder in Germany. J Affect Disord. 2017;213:23–9.
Hainmueller J, Xu Y. ebalance: a Stata package for entropy balancing. J Stat Softw. 2013;54:1–18.
Belloti F. twopm: two-part models. Stata J. 2015;15:3–20.
Dalsgaard S, Thorsteinsson E, Trabjerg BB, Schullehner J, Plana-Ripoll O, Brikell I, et al. Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiat. 2020;77:155–64.
Christensen MK, McGrath JJ, Momen NC, Whiteford HA, Weye N, Agerbo E, et al. The cost of mental disorders in Denmark: a register-based study. Npj Mental Health Res. 2022;1:1.
Weye N, Momen NC, Whiteford HA, Christensen MK, Iburg KM, Santomauro DF, et al. The contribution of general medical conditions to the non-fatal burden of mental disorders: register-based cohort study in Denmark. BJPsych Open. 2022;8:e180.
Blanco Moreno Á, Urbanos Garrido R, Thuissard Vasallo IJ. Real per capita health spending by age and sex in Spain (1998–2008): changes and effects on public healthcare expenditure projections. Gac Sanit. 2013;27:220–5.
Mar J, Larrañaga I, Ibarrondo O, González-Pinto A, las Hayas C, Fullaondo A, et al. Socioeconomic and gender inequalities in mental disorders among adolescents and young adults. J Psychiatry Ment Health. 2022. https://doi.org/10.1016/j.rpsm.2022.07.001.
Nilsson A, Paul A. Patient cost-sharing, socioeconomic status, and children’s health care utilization 2018. J Health Econ. 2018;59:109–24.
Gulliver A, Griffiths K, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113.
Owens GM. Gender differences in health care expenditures, resource utilization, and quality of care. J Manag Care Pharm. 2008;14:2–6.
Cylus J, Hartman M, Washington B, Andrews K, Catlin A. Pronounced gender and age differences are evident in personal health care spending per person. Health Aff. 2011;30:153–60.
Jacobson AM, Goldberg ID, Burns BJ, Hoeper EW, Hankin JR, Hewitt K. Diagnosed mental disorder in children and use of health services in four organized health care settings. Am J Psychiatry. 1980;137:559–65.
Sporinova B, Manns B, Tonelli M, Hemmelgarn B, MacMaster F, Mitchell N, et al. Association of mental health disorders with health care utilization and costs among adults with chronic disease. JAMA Netw Open. 2019;2:e199910.
Momen NC, Plana-Ripoll O, Agerbo E, Benros ME, Børglum AD, Christensen MK, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. 2020;382:1721–31.
Pierce M, Hope HF, Kolade A, Gellatly J, Osam CS, Perchard R, et al. Effects of parental mental illness on children’s physical health: systematic review and meta-analysis. Br J Psychiatry. 2020;217:354–63.
Mattejat F, Remschmidt H. The children of mentally ill parents. Dtsch Arztebl Int. 2008;105:413–8.
Sell M, Radicke A, Adema B, Daubmann A, Kilian R, Stiawa M, et al. Parents with mental illness: parental coping behavior and its association with children’s mental health. Front Psychiatry. 2021;12:737861.
Heuckendorff S, Johansen MN, Johnsen SP, Overgaard C, Fonager K. Parental mental health conditions and use of healthcare services in children the first year of life- a register-based, nationwide study. BMC Public Health. 2021;21:557.
Waldmann T, Stiawa M, Dinc Ü, Saglam G, Busmann M, Daubmann A, et al. Costs of health and social services use in children of parents with mental illness. Child Adolesc Psychiatry Ment Health. 2021;15:10.
Baumann AE. Stigmatization, social distance and exclusion because of mental illness: the individual with mental illness as a “stranger.” Int Rev Psychiatry. 2007;19:131–5.
Thornicroft G, Rose D, Kassam A. Discrimination in health care against people with mental illness. Int Rev Psychiatry. 2007;19:113–22.
Saunders NR, Gandhi S, Chen S, Vigod S, Fung K, De Souza C, et al. Health care use and costs of children, adolescents, and young adults with somatic symptom and related disorders. JAMA Netw Open. 2020;3:e2011295.
Ougrin D. Debate: emergency mental health presentations of young people during the COVID-19 lockdown. Child Adolesc Ment Health. 2020;25:171–2.
Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2021;30:1–2.
Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001;323:191.
Wittenberg E, Prosser LA. Health as a family affair. N Engl J Med. 2016;374:1804–6.
Mar J, Gorostiza A, Arrospide A, Larrañaga I, Alberdi A, Cernuda C, et al. Estimation of the epidemiology of dementia and associated neuropsychiatric symptoms by applying machine learning to real-world data. Rev Psiquiatr Salud Ment. 2022;15:167–75.
Cantarero-Prieto D, Pascual-Sáez M, Gonzalez-Prieto N. Effect of having private health insurance on the use of health care services: the case of Spain. BMC Health Serv Res. 2017;17:716.
Steinhausen H-C, Jakobsen H. Incidence rates of treated mental disorders in childhood and adolescence in a complete nationwide birth cohort. J Clin Psychiatry. 2019;80:17m12012.
Oliva-Moreno J, López-Bastida J, Montejo-González AL, Osuna-Guerrero R, Duque-González B. The socioeconomic costs of mental illness in Spain. Eur J Health Econ. 2009;10:361–9.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424.
Diamond A, Sekhon JS. Genetic matching for estimating causal effects: a general multivariate matching method for achieving balance in observational studies. Rev Econ Stat. 2012;95:932–45.
Acknowledgements
We acknowledge the help of Ideas Need Communicating Language Services in improving the use of English in the manuscript.
Funding
This work did not receive specific funds to be carried out.
Author information
Authors and Affiliations
Contributions
IL and JM conceived and designed the research. IL, MS-G and OI obtained the data, performed the analyses interpreted the data and drafted the results and corresponding methods sections. JM and LM-B reviewed and designed methods to classify mental disorders and drafted introduction and discussion sections of the manuscript and approved the final version. All authors revised the manuscript for important intellectual content and approved the final version. Further, they all had full access to all the data used in the study and accepted responsibility to submit for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in line with the principles of the Declaration of Helsinki and received approval from the Ethics and Clinical Research Committee of Euskadi (study code PI2019078), which allowed performing the study without informed consent given the anonymized nature of data and the sample size.
Consent for publication
Not applicable.
Competing interests
The authors have no biomedical financial interests or potential competing interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Healthcare Costs of Mental Disorders in Children, Adolescents and Young Adults in the Basque Population Registry Adjusted for Socioeconomic Status and Sex. Additional file 1 contains information about the ICD and ATC codes used to define each mental disorder category, the unit costs used, the distribution of prevalence of mental disorders by co-payment categories, the cost per patient of direct healthcare costs disaggregated by age and diagnostic group, the covariate balance achieved by entropy balancing, the two-part model parameters for each mental disorder category, and the mean and excess cost per patient of direct healthcare costs for each mental disorder category disaggregated by sex, age group and SES.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Larrañaga, I., Ibarrondo, O., Mar-Barrutia, L. et al. Excess healthcare costs of mental disorders in children, adolescents and young adults in the Basque population registry adjusted for socioeconomic status and sex. Cost Eff Resour Alloc 21, 18 (2023). https://doi.org/10.1186/s12962-023-00428-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-023-00428-w