Abstract
Background
Emerging evidence suggests that structured and progressive exercise underpinned by a cognitive behavioural approach can improve functional outcomes in patients with neurogenic claudication (NC). However, evidence surrounding its economic benefits is lacking.
Objectives
To estimate the economic costs, health-related quality of life outcomes and cost-effectiveness of a physical and psychological group intervention (BOOST programme) versus best practice advice (BPA) in older adults with NC.
Methods
An economic evaluation was conducted based on data from a pragmatic, multicentre, superiority, randomised controlled trial. The base-case economic evaluation took the form of an intention-to-treat analysis conducted from a UK National Health Service (NHS) and personal social services (PSS) perspective and separately from a societal perspective. Costs (£ 2018–2019 prices) were collected prospectively over a 12 month follow-up period. A bivariate regression of costs and quality-adjusted life-years (QALYs), with multiple imputation of missing data, was conducted to estimate the incremental cost per QALY gained and the incremental net monetary benefit (INMB) of the BOOST programme in comparison to BPA. Sensitivity and pre-specified subgroup analyses explored uncertainty and heterogeneity in cost-effectiveness estimates.
Results
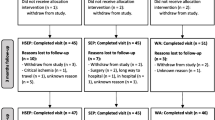
Participants (N = 435) were randomised to the BOOST programme (n = 292) or BPA (n = 143). Mean (standard error [SE]) NHS and PSS costs over 12 months were £1,974 (£118) in the BOOST arm versus £1,827 (£169) in the BPA arm (p = 0.474). Mean (SE) QALY estimates were 0.620 (0.009) versus 0.599 (0.006), respectively (p = 0.093). The probability that the BOOST programme is cost-effective ranged between 67 and 83% (NHS and PSS perspective) and 79–89% (societal perspective) at cost-effectiveness thresholds between £15,000 and £30,000 per QALY gained. INMBs ranged between £145 and £464 at similar cost-effectiveness thresholds. The cost-effectiveness results remained robust to sensitivity analyses.
Conclusions
The BOOST programme resulted in modest QALY gains over the 12 month follow-up period. Future studies with longer intervention and follow-up periods are needed to address uncertainty around the health-related quality of life impacts and cost-effectiveness of such programmes.
Trial registration This study has been registered in the International Standard Randomised Controlled Trial Number registry, reference number ISRCTN12698674. Registered on 10 November 2015.
Similar content being viewed by others
Background
Treatment options for neurogenic claudication (NC) in older adults remain limited. Although medication and surgery are options, each possesses distinct disadvantages. Medication in older adults has potential side effects, including risk of falls, whilst surgery exposes older people to risk of wound infections and cardiorespiratory complications [1]. Physiotherapy is a viable alternative often offered as part of conservative care alongside medication [2]. However, the evidence base in support of physiotherapy is currently weak with published systematic reviews based on small, often single-centre trials, with short follow-up periods [2]. There is emerging evidence that interventions combining structured exercise and a cognitive behavioural approach can improve walking ability and physical function [3, 4]. However, data on the impact of these programmes on overall health-related quality of life (HRQoL) are limited and, to the best of our knowledge, the economic implications of delivering these types of structured programmes for older adults with NC have not been explored. Published evidence indicates that the costs of physiotherapy delivered, group-based, structured exercise programmes can be excessive based on data from other patient groups [5]. In the face of continued scarcity of health care resources, it is important to understand the economic costs, health benefits and cost-effectiveness of group-based exercise programmes in older patients with NC.
This study evaluates the economic outcomes, including the cost-effectiveness, of the Better Outcomes for Older people with Spinal Trouble (BOOST) programme, a physiotherapist delivered physical and psychological intervention for older adults with NC, compared to best practice advice (BPA).
Methods
Trial background
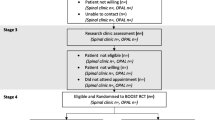
The BOOST Trial was a pragmatic, multicentre, superiority randomised controlled trial (RCT), and the protocol has been published previously [6]. In brief, community-dwelling adults, aged 65 years and over, who reported symptoms consistent with NC were eligible and were identified through spinal clinics (primary and secondary care) and general practice records. The trial had a pre-specified target sample size of 402 participants [6]. Recruitment occurred between 01 August 2016 and 29 August 2018 at 15 trial sites in England. Participants were randomised (2:1 ratio) to either the BOOST programme or BPA using a secure, telephone randomisation service. The primary clinical outcome was the Oswestry Disability Index (ODI) at 12 months and other important outcomes included pain, HRQoL outcomes, physical activity and strength [6]. Economic data were collected at baseline and as part of the study follow-up at 6 and 12 months.
Comparator interventions
The experimental intervention was a combined physical and psychological group programme (BOOST programme) that included an individual assessment followed by a supervised component delivered by a physiotherapist in up to twelve 90 min group sessions over 12 weeks. Group sessions involved education and discussion using a cognitive behavioural approach (30 min) followed by individually tailored group exercises (60 min) [7]. The exercises targeted muscle strength, balance, and flexibility whilst the walking circuit aimed to increase walking self-efficacy, dynamic balance and mobility. Participants were introduced to twice-weekly home exercises during session five and asked to undertake these during and beyond the formal programme. Physiotherapists conducted follow-up telephone reviews approximately 1 and 2 months after completing the supervised sessions, to promote adherence with the home exercises.
The control intervention was BPA delivered during individual physiotherapy appointments. Each participant underwent an assessment of symptom presentation and walking ability to tailor the advice and education provided. Verbal and written advice and education were provided, including education about NC, being physically active, use of medications, when to seek more advice and prescription of up to four home exercises. The control intervention was ideally delivered in one session. However, if needed, two review appointments were permitted to re-enforce advice and review exercises or walking aids. Physiotherapists could not provide treatments such as manual therapy, acupuncture or structured exercise sessions.
Overview of economic analyses
The economic analyses involved evaluation of economic costs, HRQoL outcomes and cost-effectiveness of the BOOST programme where cost-effectiveness was expressed in terms of incremental cost per quality-adjusted life year (QALY) gained. The base-case economic evaluation took the form of an intention-to-treat, imputed analysis conducted from a UK National Health Service (NHS) and personal social services (PSS) perspective in line with the National Institute for Health and Care Excellence (NICE) reference case [8]. The NHS payer perspective considers intervention-related treatment costs and other health service resource use and costs associated with the managing the disease whilst a personal social services perspective includes services provided by local authorities for several vulnerable groups, including older people. A 12 month time horizon for the economic evaluation was used mirroring the trial follow-up period and therefore no discounting was required.
Costs
Three broad resource use and costs categories were estimated: (i) costs associated with each intervention delivery; (ii) health and personal social service use during the 12 months’ follow-up; and (iii) societal resource use and costs including economic values of lost productivity (e.g., lost income by participants and their carers) (Additional file 1: Table S1) (Appendix). All costs were expressed in pounds sterling and valued in 2018–19 prices. Where required, costs were inflated or deflated to 2018–19 prices using the NHS Cost Inflation Index (NHSCII) [9].
Intervention costs
Direct intervention costs were costs associated with the delivery of the BOOST programme. These included: (1) development and training costs; (2) staff costs including those associated with direct participant contact and non-contact time (i.e., time used to set up the sessions, indirect administrative activities, and intervention-related supervision activities); and (3) equipment costs (Additional file 1: Table S2) (Appendix). Unit costs for staff were obtained from the Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care 2019 compendium and were multiplied by the time taken to perform a specified activity (e.g., conduct a group session). All resource use data related to the group sessions were recorded on activity logs completed by physiotherapists and exercise assistants including: (i) the time taken to deliver sessions, (ii) number of participants in attendance and, (iii) number and grade of physiotherapists in attendance. Costs of equipment were obtained directly from the trial’s expenditure records and from the NHS Supply Chain Catalogue 2018 [10]. An annual equivalent cost of equipment was obtained by annuitising capital costs of each item over its useful life span, applying a discount rate of 3.5% per annum.
NHS and PSS costs. Participants (or their next-of-kin) reported health and social service resource use through questionnaires administered at 6- and 12 months post-randomisation. These resource inputs were valued using unit costs identified through national cost compendia in accordance with NICE’s Guide to the Methods of Technology Appraisal 2013 [8]. Unit cost data were derived based on the Department of Health and Social Care’s Reference Costs 2017–18 schedules [11], the PSSRU Unit Costs of Health and Social Care 2019 compendium [12], 2018 volumes of the British National Formulary [13], and the NHS Supply Chain Catalogue 2018 [10].
Societal costs
Analyses from a societal perspective additionally encompassed economic values for work absences (by patients and their caregivers), travel costs and privately incurred health expenditures. We included economic values of work absences by caregivers as caregivers of elderly frail people are potentially at increased risk of disrupted engagement within the labour market. Although data on the value of carers’ time is sparse, available data suggest that a 1% increase in hours of care translates, on average, into slightly more than a 1% decrease in hours of work [14]. Economic values of work absences were estimated as a product of the number of participant-reported days off work (for themselves and their caregivers) and national average daily earnings delineated by age, gender and occupational sector derived from the Office for National Statistics’ Annual Survey for Hours and Earnings [15]. Travel costs and privately incurred health expenditures were self-reported by trial participants.
Health-related quality of life outcomes
HRQoL was assessed using the EuroQol EQ-5D-5L instrument [16] completed at baseline, and at 6 and 12 months post-randomisation. The EQ-5D-5L instrument defines HRQoL in terms of five dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression), each with five levels of severity. Responses to the EQ-5D-5L descriptive system were mapped onto the EQ-5D-3L value set using the van Hout et al. interim cross-walk algorithm [17], as recommended by NICE in England and Wales [18]. Patient-level QALYs were estimated using the area under the curve approach, assuming linear interpolation between the utility scores, i.e., the preference-based values attached to the health states generated from the EQ-5D-5L descriptive system.
Handling of missing data
Multiple imputation by chained equations was used to predict missing costs and health utility scores based on the assumption that data were missing at random (MAR). The MAR assumption was tested through a series of logistic regression analyses comparing participants’ characteristics for those with and without missing endpoint data. Imputation was achieved using predictive mean matching, which has the advantage of preserving non-linear relationships and correlations between variables within the data. Fifty imputed datasets were generated to inform the base-case and subsequent sensitivity and subgroup analyses. Parameter estimates were pooled across the imputed datasets using Rubin’s rules [19] to account for between- and within-imputation components of variance terms associated with parameter estimates.
Cost-effectiveness analysis
Mean resource use, cost and health utility values were compared between the trial groups using two sample t-tests. Differences between groups, along with confidence intervals (CIs), were estimated using non-parametric bootstrap estimates (10,000 replications). Mean incremental costs and mean incremental QALYs were estimated using seemingly unrelated regression (SUR) methods that account for the correlation between costs and outcomes [20]. The SUR was adjusted for covariates (baseline utilities, gender). Following imputation, non-parametric bootstrap methods were used to generate the joint distribution of costs and outcomes and to populate a cost-effectiveness plane. The incremental cost-effectiveness ratio (ICER) for the BOOST programme was compared with BPA by dividing the between-group difference in adjusted mean total costs by the between-group difference in adjusted mean QALYs. Mean ICER values were compared against cost-effectiveness threshold values (i.e. society’s willingness to pay for an additional QALY) ranging between £15,000 and £30,000 per QALY gained in line with NICE guidance [21]. ICER values lower than the threshold are considered cost-effective for use in the UK NHS. The incremental net monetary benefit (INMB) of switching from BPA to the BOOST programme was calculated at each of the cost-effectiveness threshold values. The net monetary benefit is the economic benefit of an intervention (expressed in monetary terms) net of all costs. A positive incremental NMB suggests that, on average, the BOOST programme is cost-effective compared with BPA, at the given cost-effectiveness threshold.
Sensitivity and subgroup analyses
Pre-specified sensitivity analyses were undertaken to assess the impact of alternative aspects of the cost-effectiveness of the BOOST programme and included restricting the analyses to complete cases (i.e. the sample of participants with no missing costs or outcome data at any time point) and replicating the analysis from a societal perspective. Pre-specified subgroup analyses were conducted by age (65–74 years/75 years +); gender (male/female); baseline ODI scores (< = 22, > 22); baseline Tilburg Frailty Index (TFI) scores (0–4, not frail/5 + , frail) (17); baseline Fear Avoidance Beliefs Questionnaire (FAB) scores (0–14, less fear/15 + , more fear) (18); and baseline hand grip strength (HGS) (men: < 30/30 + ; women < 20/20 +).
Results
Study population and data completeness
Baseline characteristics of participants were well-matched between the randomised groups (Table 1). The exception was the proportion of people classified as frail according to the TFI (11% higher in BPA group), but other markers of frailty including walking capacity (measured by the 6 Min Walk Test), physical performance (measured by the Short Physical Performance Battery) and HGS were similar. Complete QALY profiles were available for 357 (82%) participants based on the participant-reported EQ-5D-5L. Completion of health resource use data for the economic evaluation was similar at each time-point between the BOOST and BPA groups.
Cost of intervention
Mean total intervention costs for all 12 sessions are presented within each group at each site (Additional file 1: Tables S3, S4) (Appendix). These varied between £242 (Site 15 group 1) and £911 (Site 1 group 1). The average costs per group session per participant (including administrative costs) varied from approximately £11.80 (Site 4, group 3) to £67.00 (Site 1, group 1). The mean cost per participant was generally lower across all sites if the target number of participants (n = 6) had been achieved.
Resource utilization
For health and personal social service use, shown in (Additional file 1: Tables S5, S6), there were non-significant differences between the two groups in utilisation of hospital inpatient and outpatient care, community based health care and social services, and days off work.
Total economic costs
For the base-case analysis, mean NHS and PSS costs, inclusive of intervention costs, over the entire follow-up period were £1974.06 for the BOOST programme versus £1826.64 for the BPA group (Table 3). There was a non-significant cost difference in favour of the BPA group of £147.42 (95% CI £− 419 to 714).
Mean total societal costs, for the entire follow-up period, inclusive of the intervention cost, were £2176.01 in the intervention group compared with £2140.54 in the BPA group (Table 4). This generated a mean cost difference of £35.47 (95% CI: − £469.57 to 540.51) in favour of the BPA group. Societal costs (excluding NHS and PSS costs) were higher in the BPA group and primarily driven by economic valuation of time taken off work by patients and carers in the BPA group. Considering that the mean number of days off work was similar between the two groups and only a relatively small number of patients/carers took time off work, the mean values are skewed by a few individuals (Additional file 1: Figure S1). The estimates of economic costs for non-imputed (complete) cases are shown in Additional file 1: Tables S7, S8 and follow the same pattern as the imputed base case analysis.
Health‑related quality of life outcomes
The adjusted mean (SE) participant-reported QALY estimate for to between 79%-89% across cost-effectiveness thresholds to between 79%-89% across cost-effectiveness thresholds the base case analysis over 12 months favoured the BOOST programme (0.621 (0.009) versus 0.599 (0.006); between group difference 0.021 (95% CI 0 to 0.044)) (Additional file 1: Table S9). These gains were driven by a between group difference in EQ-5D utility scores at 6 months (0.039; [95% CI 0.008 to 0.07]), which narrowed at 12 months (0.009; [95% CI − 0.027 to 0.045]).
Cost‑effectiveness results: base‑case analysis
NHS and PSS Perspective. The base-case economic evaluation indicated that the BOOST programme was associated with marginally higher NHS and PSS costs (£147, 95% CI − 419 to 714) and an increase in QALYs (0.020, 95% CI − 0.003 to 0.045). The mean ICER for the BOOST programme was estimated at £7,211 per QALY gained, i.e. on average, the BOOST programme was associated with a higher cost and an increase in QALYs. The associated mean INMB at cost-effectiveness thresholds of £15,000, £20,000 and £30,000 per QALY were £145, £244 and £464, respectively (Table 5). The base-case mean INMB was > 0, suggesting that the BOOST programme would result in an average net economic gain of approximately £244 (INMB = £244, 95% CI − £570 to £1058). The probability of cost-effectiveness for the BOOST programme was estimated as 67%, 78% and 83% at cost-effectiveness thresholds of £15,000, £20,000 and £30,000 per QALY, respectively. The joint distribution of costs and outcomes for the base-case analysis is presented graphically in Fig. 1. The cost-effectiveness acceptability curve is shown in Fig. 2.
Sensitivity and subgroup analyses
The sensitivity analysis conducted from a societal perspective increased the probability that the BOOST programme is cost-effective to between 79 and 89% across cost-effectiveness thresholds (Table 5). The sensitivity analysis based on complete cases supported the base-case finding that the BOOST programme was associated with higher costs and increase in QALYs (Table 5). The pre-planned subgroup analyses showed evidence that the BOOST programme was more cost-effective in the following subgroups: males, participants aged 64–74 years, participants with a baseline ODI < = 22, participants with higher HGs (> = 30 in men; > = 20 women),participants with higher fear avoidance, and participants classified as frail based on Tilburg Frailty Index (TFI < 5).
Discussion
This trial-based economic evaluation revealed that the BOOST programme led, on average, to a modest increase in health-related quality of life, at a small increased cost, over a 12 month period. The resulting ICER from an NHSS and PSS perspective of £7,211 per QALY gained falls favourably below the recommended NICE cost-effectiveness threshold of £20,000 per QALY though the uncertainty around the mean ICER was large. From a societal perspective, the BOOST programme was more cost-effective with a mean ICER of £1745 per QALY gained.
We undertook a robust analysis, based in general on good completion of follow up questionnaires. We used two perspectives to estimate cost-effectiveness. The NHS and PSS perspective adopted within the base-case analysis considered all costs related to providing health and related care. The societal perspective also considered economic values of work absences by the trial participants and their informal carers; the latter is often a vital lifeline to older people with NC. Complete case and imputed analyses were broadly consistent in outcomes. Imputed analyses gave a more conservative estimate, most likely due to greater numbers of frail, older women dropping out of follow up. The evidence of HRQoL benefits add to the emerging evidence base from good quality clinical trials that demonstrate improvements in mobility from similar programmes [3]. In additional to improvements in HRQoL, the BOOST programme also resulted in improvements in mobility over a 12 month period and improvements in pain related disability over a 6 month period [22].
Without economic modelling beyond the current parameters of the trial, the longer-term cost-effectiveness of the BOOST programme cannot be ascertained. However, the pattern of rising and then declining HRQoL gains over the year-long follow-up period suggest that it is unlikely that, without further intervention the effects will be sustained over a longer time-horizon. Recent evidence from the REACT study showed that long-term exercise programmes (i.e., those lasting at least 1 year) can improve physical functioning among older adults in real-world community settings in the UK, with benefits that are sustained for at least 24 months [23]. The group-based exercises in the REACT study were delivered over the entire 12 month period compared to the group-based component of the BOOST programme which lasted 12 weeks (with participants continuing exercises independently up to 12 months). Delivery of the group-based component of the BOOST programme over a longer period and assessment of economic outcomes over a longer follow-up period may therefore have generated a different pattern of results.
We noted that the intervention appears less cost-effective in participants who were older and more disabled by pain and in females. These participants may have greater challenges with attending and complying with the intervention. Compliance with the group intervention, defined as attending at least 9 out of 12 group sessions, seemed to be one of the key factors driving the effectiveness of the BOOST programme. The difference in the main outcome measure was larger, favoured the BOOST programme and reached the predefined clinically significant threshold (5 points on the ODI) at 6 months when compliance with group intervention was considered. As with all sub-group analyses, these should be considered exploratory only, and our primary estimates account for all people regardless of their compliance to the intervention and follow up. We used a pragmatic approach to sampling, and hence our findings should be generalisable. We limited entry to the trial to those greater than 65 years. Neurogenic claudication is generally associated with ageing, and incidence below 65 years declines.
There is limited evidence for cost-effectiveness of structured and progressive exercises for patients with NC in the broader literature. The cost-effectiveness studies that have been conducted in this population group have focussed on cost-effectiveness of surgical treatment of spinal stenosis (in patients with symptoms of NC) [24], or assessed physiotherapy as part of a ‘conservative care’ package (alongside pain medications and epidural injections) [25]. Two recently published RCTs examined programmes similar to the BOOST programme [3, 4]. Both studies assessed HRQoL via the SF-36 health-related quality of life questionnaire and neither reported costs associated with the structured exercise programmes or their downstream resource consequences. To the best of our knowledge, this economic evaluation is based on the largest RCT of its kind reported to date.
Strengths of the current economic evaluation are that the trial was prospectively designed for a cost-effectiveness analysis using individual-level data to reach a confirmatory conclusion regarding a physiotherapy-delivered physical and psychological group intervention in older adults with NC. A rigorous evaluation of the costs associated with the delivery of the BOOST programme is presented, based on prospective (observed) data on the time it took staff to run the group sessions, administrative costs, equipment costs and follow-up costs. In a non-trial (real) setting, costs of delivering the intervention may be lower as there will be less administrative burden of completing treatment logs and hence less time needed to run the groups.
There are some limitations to this economic evaluation. Firstly, utility measurements were collected at only two time-points post-randomisation. Evidence suggests that the timing of assessment can significantly influence cost-effectiveness results when using the EQ-5D, particularly when participants experience recurrent health fluctuations [26]. In such cases, the linear interpolation of utility data may fail to reflect HRQoL fluctuations over short periods and the uncertainty is compounded by missing data. Secondly, resource use data were retrospectively recalled by participants, and this could have led to recall bias, though we cannot predict the direction of this bias. Findings form literature are mixed, suggesting that resource use may be under-reported, over-reported or they may be good agreement between patient/carer recall and data extracted from medical records, depending on how well the resource use measures are structured [27]. Because the recall periods and questionnaires were standardised across randomised groups, retrospective recall is unlikely to have biased results in favour of one group. Thirdly, our approaches to collecting resource use data did not disentangle resource use associated with NC from resource use associated with broader health factors. Fourthly, constrained trial resources precluded an assessment of the health-related quality of life outcomes of carers and therefore these potential externalities were excluded from the sensitivity analysis conducted from a societal perspective.
Conclusion
The BOOST programme resulted in modest QALY gains over a short-term (12 month) follow-up period. Future studies with longer intervention and follow-up periods are needed to address uncertainty around the health-related quality of life impacts and cost-effectiveness of such programmes.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author upon reasonable request.
Change history
21 March 2023
This article has been corrected since original publication; please see the linked erratum for further details.
11 April 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12962-023-00431-1
Abbreviations
- BOOST:
-
Better outcomes for older people with spinal trouble
- BPA:
-
Best practice advice
- CIs:
-
Confidence intervals
- FAB:
-
Fear avoidance beliefs questionnaire
- HGS:
-
Hand grip strength
- HRQoL:
-
Health-related quality of life
- ICER:
-
Incremental cost-effectiveness ratio
- INMB:
-
Incremental net monetary benefit
- MAR:
-
Missing at random
- NC:
-
Neurogenic claudication
- NHS:
-
National health service
- NHSCII:
-
NHS cost inflation index
- NICE:
-
National institute for health and care excellence
- ODI:
-
Oswestry disability index
- PSS:
-
Personal social services
- PSSRU:
-
Personal social services research unit
- QALY:
-
Quality-adjusted life year
- RCT:
-
Randomised controlled trial
- SE:
-
Standard error
- SUR:
-
Seemingly unrelated regression
- TFI:
-
Tilburg frailty index
References
Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus nonsurgical treatment for lumbar spinal stenosis. Spine. 2016;41:E857-e868.
Ammendolia C, Stuber KJ, Rok E, Rampersaud R, Kennedy CA, Pennick V, Steenstra IA, de Bruin LK, Furlan AD. Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD010712.
Ammendolia C, Côté P, Southerst D, Schneider M, Budgell B, Bombardier C, Hawker G, Rampersaud YR. Comprehensive nonsurgical treatment versus self-directed care to improve walking ability in lumbar spinal stenosis: a randomized trial. Arch Phys Med Rehabil. 2018;99:2408-2419.e2402.
Minetama M, Kawakami M, Teraguchi M, Kagotani R, Mera Y, Sumiya T, Nakagawa M, Yamamoto Y, Matsuo S, Sakon N, et al. Supervised physical therapy versus unsupervised exercise for patients with lumbar spinal stenosis: 1-year follow-up of a randomized controlled trial. Clin Rehabil. 2021;35:964–75.
Khan I, Petrou S, Khan K, Mistry D, Lall R, Sheehan B, Lamb S. Does structured exercise improve cognitive impairment in people with mild to moderate dementia? a cost-effectiveness analysis from a confirmatory randomised controlled trial: the dementia and physical activity (DAPA) trial. Pharmaco Economics Open. 2019;3:215–27.
Williamson E, Ward L, Vadher K, Dutton SJ, Parker B, Petrou S, Hutchinson CE, Gagen R, Arden NK, Barker K. Better outcomes for older people with spinal trouble (boost) trial: a randomised controlled trial of a combined physical and psychological intervention for older adults with neurogenic claudication, a protocol. BMJ Open. 2018;8:e022205.
Ward L, Williamson E, Hansen Z, French DP, Boniface G, Rogers D, Lamb SE. Development and delivery of the BOOST (better outcomes for older adults with spinal trouble) intervention for older adults with neurogenic claudication. Physiotherapy. 2019;105:262–74.
National Institute for Health and Care Excellence (NICE): Guide to the methods of technology appraisal (Chapter 5). National Institute for Health and Care Excellence (NICE) 2013.
Curtis LA, Burns A. Unit costs of health and social care 2020. Canterbury: Personal Social Services Research Unit, University of Kent; 2020.
NHS. NHS supply chain. London: NHS Digital; 2018.
NHS England.: National schedule of NHS costs 2018/19. 2021.
Curtis LA, Burns A. Unit costs of health and social care 2019. Canterbury: University of Kent Personal Social Services Research Unit; 2019.
British National Formulary [https://www.evidence.nhs.uk/formulary/bnf/current]
Colombo F, Llena-Nozal A, Mercier J, Tjadens (2011) Help wanted?: providing and paying for long-term care, OECD health policy studies, OECD publishing, Paris. https://doi.org/10.1787/9789264097759-en.
Office for National Statistics. Employee earnings in the UK 2018. London: Office for National Statistics; 2018.
EuroQol Research Foundation: EQ-5D-5L user guide. 2019. https://webarchive.nationalarchives.gov.uk/ukgwa/20200501111101mp_/https://improvement.nhs.uk/documents/6486/2_-_National_schedule_of_NHS_costs_V2.xlsx. Accessed 7 Feb 2023.
van Hout B, Janssen M, Feng Y-S, Kohlmann T, Busschbach J, Golicki D, Lloyd A, Scalone L, Kind P, Pickard ASJVih. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Val Health. 2012;15:708–15.
Position statement on use of the EQ-5D-5L value set for England (updated October 2019) [https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l]
Little R, Rubin D. Statistical analysis with missing data. New York: Wiley; 1987.
Zellner A, Huang DS. Further properties of efficient estimators for seemingly unrelated regression equations. Int Econ Rev. 1962;3:300–13.
NICE. Guide to the methods of technology appraisal. London: Springer; 2013.
Williamson E, Boniface G, Marian M, Dutton S, Garrett A, Morris A, Hansen Z, Ward L, Nicolson NJ, Rogers D, Barker KL, Fairbank J, Fitch J, French D, Comer C, Mallen C, Lamb S. The clinical effectiveness of a physiotherapy delivered physical and psychological group intervention for older adults with neurogenic claudication: the BOOST randomised controlled trial. J Gerontol A Biol Sci Med Sci. 2022;77:1654–64.
Stathi A, Greaves CJ, Thompson JL, Withall J, Ladlow P, Taylor G, Medina-Lara A, Snowsill T, Gray S, Green C, et al. Effect of a physical activity and behaviour maintenance programme on functional mobility decline in older adults: the REACT (retirement in action) randomised controlled trial. Lancet Public Health. 2022;7:e316–26.
Tosteson AN, Lurie JD, Tosteson TD, Skinner JS, Herkowitz H, Albert T, Boden SD, Bridwell K, Longley M, Andersson GB. Surgical treatment of spinal stenosis with and without degenerative spondylolisthesis: cost-effectiveness after 2 years. Ann Intern Med. 2008;149:845–53.
Skidmore G, Ackerman SJ, Bergin C, Ross D, Butler J, Suthar M, Rittenberg J. Cost-effectiveness of the X-STOP® interspinous spacer for lumbar spinal stenosis. Spine. 2011;36:E345–56.
Schilling C, Dowsey MM, Clarke PM, Choong PF. Using patient-reported outcomes for economic evaluation: getting the timing right. Value Health. 2016;19:945–50.
Ridyard CH, Hughes DA. Review of resource use measures in UK economic evaluations. unit costs of health and social care. Canterbury: Personal Social Services Research Unit. University of Kent; 2015.
Acknowledgements
Thank you to BOOST Research Team for their assistance with undertaking this study. BOOST programme management staff and researchers: Angela Garrett and Graham Boniface.
Funding
This research was funded by the NIHR Programme Grants for Applied Research (reference: PTC-RP-PG-0213-20002; Chief Investigator Sarah E Lamb). This research was supported by the National Institute for Health Research Applied Research Collaboration Oxford and Thames Valley at Oxford Health NHS Foundation Trust. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
MM was the trial health economist and is lead author. She conducted the health economics analysis and drafted the manuscript. KK assisted with the costing analysis. SD and IRM were involved in writing this manuscript and were the trial statisticians. EW was a co-applicant on the grant awarded by the NIHR Programme Grants for Applied Research and was involved in the design of the BOOST study and its implementation. SEL is the Chief Investigator, and the guarantor. SP was a co-applicant and oversaw the design, conduct and analysis of the health economic study and is the senior author. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the BOOST trial was given by the London-Brent National Research Ethics Committee (REC number 16/LO/0349) on March 3, 2016. All participants provided written informed consent prior to enrolment in the trial.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Unit costs for broader resource items (£, 2018–19). Table S2. Unit costs of standard materials used to deliver intervention. Table S3. Total cost of delivering intervention by site and group. Table S4. Mean staff cost (£, 2019) per session per participant. Table S5. Health resource use by trial allocation, category and study period for complete cases at 6months post-randomisation. Table S6. Health resource use by trial allocation, category and study period for complete cases at 12 months post-randomisation. Table S7. Economic costs by trial allocation arm and cost component category for the entire follow-up period for the NHS PSS perspective among complete cases (£, 2018–19 prices). Table S8. Economic costs by trial allocation arm and cost component category for the entire follow-up period for the societal perspective among complete cases (£, 2018–19 prices). Table S9. Patient reported EQ-5D-5L utility scores and QALYs (Imputed Analysis). Figure S1. Economic losses due to lost days of work by participants and/carers (£, 2018–19)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Maredza, M., Khan, K., Marian, I.R. et al. Economic costs, health-related quality of life outcomes and cost-utility of a physical and psychological group intervention targeted at older adults with neurogenic claudication. Cost Eff Resour Alloc 21, 14 (2023). https://doi.org/10.1186/s12962-022-00410-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-022-00410-y