Abstract
Objective
Despite the high HIV associated burden, Mozambique lacks data on HIV counselling and testing (HCT) costs. To help guide national HIV/AIDS programs, we estimated the cost per test for voluntary counselling and testing (VCT) from the patient’s perspective and the costs per person tested and per HIV-positive individual linked to care to the healthcare provider for VCT, provider-initiated counselling and testing (PICT) and home-based testing (HBT). We also assessed the cost-effectiveness of these strategies for linking patients to care.
Methods
Data from a cohort study conducted in the Manhiça District were used to derive costs and linkage-to-care outcomes of the three HCT strategies. A decision tree was used to model HCT costs according to the likelihood of HCT linking individuals to care and to obtain the incremental cost-effectiveness ratios (ICERs) of PICT and HBT with VCT as the comparator. Sensitivity analyses were performed to assess robustness of base-case findings.
Findings
Based on costs and valuations in 2015, average and median VCT costs to the patient per individual tested were US$1.34 and US$1.08, respectively. Costs per individual tested were greatest for HBT (US$11.07), followed by VCT (US$7.79), and PICT (US$7.14). The costs per HIV-positive individual linked to care followed a similar trend. PICT was not cost-effective in comparison with VCT at a willingness-to-accept threshold of US$4.53, but only marginally given a corresponding base-case ICER of US$4.15, while HBT was dominated, with higher costs and lower impact than VCT. Base-case results for the comparison between PICT and VCT presented great uncertainty, whereas findings for HBT were robust.
Conclusion
PICT and VCT are likely equally cost-effective in Manhiça. We recommend that VCT be offered as the predominant HCT strategy in Mozambique, but expansion of PICT could be considered in limited-resource areas. HBT without facilitated linkage or reduced costs is unlikely to be cost-effective.
Similar content being viewed by others
Introduction
Timely HIV diagnosis and linkage to care are essential for improved HIV outcomes [1] but are generally not achieved across sub-Saharan Africa (SSA) [2, 3]. Haber et al. showed that in Kwazulu-Natal, the transition from receiving an HIV-positive diagnosis to care is the weakest in the HIV care continuum [4]. A systematic review reported that, among HIV diagnosed individuals, only one-third of ART-eligible patients were receiving treatment [5]. Cost-effective HIV counselling and testing (HCT) strategies are needed to link more people living with HIV (PLHIV) to care. Few cost-effectiveness analyses (CEAs) on HCT strategies examining linkage to care as an outcome have been conducted, although existing reports have indicated that facility-based strategies are likely more cost-effective than community-based strategies [6, 7].
In Mozambique, where the adult HIV prevalence is among the highest in the world, only 61% PLHIV know their HIV status, and 54% are receiving ART [8]. At the time of this study, Mozambique did not have universal HIV testing [9]. In the country, community-based strategies such as home-based testing (HBT) are infrequently offered [10]. Voluntary counselling and testing (VCT), initiated by the patient at the health facility, has been a mainstay for HCT while provider-initiated counselling and testing (PICT) is the standard approach for healthcare services [9]. In Mozambique as well as in other settings with high burden HIV, PICT lacks optimization strategies in order to reach its full potential [11]. A recent cohort study conducted in Manhiça District found that VCT was associated with the greatest proportion of PLHIV linked to care, followed by PICT and HBT [12]. Importantly, the study procedures did not influence the linkage-to-care beyond the HCT and facility-based referral.
Economic evidence in relation to costs and cost-effectiveness of these HCT strategies in linking PLHIV to care is lacking. By drawing on prospective data from the Manhiça cohort study [12], we estimate the costs of providing HCT strategies in Mozambique and examine the cost-effectiveness of PICT and HBT compared to VCT for initiating linkage to care. In doing so, we compared the level of engagement each HCT strategy entails against the outcome.
In the literature, unit costs of HCT strategies from the provider’s perspective are derived from program costs and usually reported as average cost per person tested and/or average cost per HIV-positive individual identified. The former is more relevant for our study and shall be examined in detail for VCT, PICT, and HBT. Estimates of unit costs per person tested vary. For example, VCT costs in Kenya, Swaziland, Tanzania, and Uganda were reported to be US$8.27–US$28.93 [13,14,15,16,17], and PICT costs were lower (US$5.71–US$11.68) [13,14,15]. In Kenya, South Africa, and Uganda, several studies reported HBT costs ranging from US$5.00 to US$29.00 per client tested, similar to the range reported for VCT [14, 15, 18,19,20]. Importantly, costs are not directly comparable across studies because the underlying assumptions and contexts may differ. Findings from our study can help inform policymakers on effective yet affordable national-level HCT that could help identify more PLHIV and link them to care in Mozambique.
Methods
Manhiça cohort study
In 2012, HIV prevalence and incidence in Manhiça district were estimated to be 40% and 3.6 infections/100 person-years, respectively [21, 22]. The Manhiça cohort study enrolled 1122 participants with a new HIV-positive diagnosis (May 2014–June 2015), following routine VCT and outpatient PICT at the Manhiça District Hospital and door-to-door HBT by trained healthcare workers (Appendix 1). VCT and PICT resulted in significantly higher proportions of PLHIV linked to care, defined as enrollment in care at the reference district hospital and with a CD4 count registered within the first 3 months after HIV diagnosis, than HBT. Nonetheless, HBT reached a distinct population living in extreme poverty who were in greatest need for facilitated linkage interventions. Details of the study methods and procedures have been described elsewhere [12].
Cost estimate methods
We employed a micro-costing (bottom-up) approach [23] to estimate the financial and economic costs of HCT provision incurred in the cohort study from the provider’s perspective. As VCT and PICT were routinely offered to the public at the time of the study, estimated costs were referenced from routine health system costs. HBT-associated costs were assessed separately as HBT was not a routine testing strategy. Nevertheless, we examined only recurrent costs and not start-up costs for HBT as there was already an existing structure for carrying out door-to-door interventions e.g. community vaccination.
To determine financial costs, we processed data on capital (e.g. buildings, equipment, and vehicles) and recurrent (personnel, supplies, test-kits, and transport) costs collected May 2014–June 2015. We utilized time and motion data to determine the financial costs of personnel and transport. Time data tracked the time taken by counsellors to travel to and between participants’ houses during HBT and to conduct each counselling session either at the District Hospital or at each participant’s house. On the other hand, motion data included travelling speeds to determine fuel costs. We did not include training costs because HCT in the cohort study was provided by healthcare workers who were not specially trained.
The cost per VCT attendance from the patient’s perspective was determined by a similar micro-costing approach using self-reported explicit costs and implicit costs. Implicit costs were calculated by valuing the patients’ time spent travelling to and waiting at the VCT facility using the average monthly minimum wage in Mozambique, expressed as an hourly wage and assuming an average of 176 work hours (22 days × 8 h/day) per month. We assumed patients would not incur any additional costs for HBT and PICT.
Data sources
A questionnaire was used to elicit demographic information (Appendix 2). From the patient’s perspective, data were collected from patients accessing VCT by using a specific questionnaire (Appendix 3). From the provider perspective, data were collected from VCT, HBT, and PICT using a separate questionnaire (Appendix 4). Some of the provider resources used (e.g. time to perform the test) were collected for all patients receiving the test (as their HIV status was not known a priory), but only HIV-positive patients were retained for ethical reasons. Where information on costs was not available through questionnaires (e.g. building, furniture, and operation and maintenance costs), we approximated them as a percentage of total recurrent costs based on results from a study by Mwenge et al. [24] in Malawi and Zimbabwe, which share similar sociodemographic and economic profiles as Mozambique [25, 26].
Data analysis
For cost estimate analysis, we included data on all individuals who tested HIV positive (n = 1277), including non-enrolled individuals (n = 155) who had received a HIV-positive test result previously in a concomitant study. These 155 patients were tested using the same procedure as with the other participants in the main cohort study and were included in our sample size. Of the 1277 patients, 350 were enrolled from VCT and were included in cost estimates from the patients’ perspective. Time data for the following variables were highly negatively skewed due to measurement errors during data collection: travelling to individual houses, performing the test, waiting for test results, and explaining the results. We deemed the 85th percentile to be an appropriate upper limit to capture a reasonable proportion of these data without including outlying values, replacing observations above this percentile with the value at the 85th percentile. All data analyses were conducted using Microsoft Excel 2016 (V.16.14.1) and Stata (V.13.1: Stata Corporation).
We performed descriptive statistical analysis to compute mean (with standard deviation) and median (with maximum and minimum ranges) costs per person tested positive from both the patient’s and provider’s perspective. All costs were expressed in 2015 US$ at an exchange rate of 33.00 Mozambique New Metical (MT) per US$ [27].
Determination of cost per individual tested
The cost of testing each individual was determined by summing costs of each individual resource, obtained by multiplying the quantities of each resource expended with their approximated unit costs (Appendix 5).
Implicit costs to patients were calculated by valuing their time spent travelling to and waiting at the VCT facility, using the average monthly minimum wage in Mozambique [28]. Capital costs were factored as a proportion of total costs. Fuel costs were calculated using motion data assuming an average travelling speed of 50 km/hour and an average fuel consumption of 0.143 L/km, based on 2013 estimates from the Global Fuel Economy Initiative [29].
Determination of HCT costs and cost-effectiveness
A decision tree model (Appendix 6) was designed for the CEA to determine cost-effectiveness ratios (CERs) and incremental cost-effectiveness ratios (ICERs). We defined effectiveness as linkage to care based on the cohort study’s definition. Our primary outcome measure was incremental cost per enrolled individual linked to care. The model’s time horizon of 1 year mirrored the duration of the cohort study.
The model captured all steps of the HIV care cascade for both VCT and PICT from diagnosis to retention in care after 12 months of follow-up. For HBT, the model additionally captured steps before the HCT process, from being reached through HBT to obtaining consent. One-year cumulative proportions, reported as the percentage uptake at each step of the HIV care cascade (figures reported in Appendix 1), were directly converted into conditional probabilities for parameterizing the decision tree (Table 1).
The key assumptions of the model were:
-
(1)
Linear, unidirectional transitions along the care cascade; uptake at each step must be conditional on the previous step;
-
(2)
Only early treatment uptake (≤ 3 months post-diagnosis) at each step was modelled; and.
-
(3)
Costs incurred for individuals who cannot be reached through or deemed ineligible for HBT are inconsequential to total program costs.
We calculated the expected average costs and linkage-to-care proportion per person tested for each HCT strategy, by summing costs and outcomes of each branch of the tree weighted by their associated probabilities of occurrence. A ratio of average costs and average expected linkage-to-care proportion was calculated to determine expected HCT linkage-to-care costs.
Unlike the derivation of CERs, data only for enrolled individuals was used to determine ICERs to facilitate accurate comparisons of effectiveness. We determined ICERs by dividing the difference in expected costs over the difference in the expected proportion of enrolled individuals linked to care.
Sensitivity analysis
Our univariate sensitivity analysis varied key cost-related parameters within predefined sensitivity ranges (Appendix 7) to explore the robustness of results. Lacking published data, we empirically adjusted base-case values by ± 20%, referencing ranges used by Mwenge et al. in their determination of HCT costs in three SSA countries [24].
We performed deterministic and probabilistic sensitivity analyses (DSA and PSA) as part of the CEA. In the DSA, probabilities and average costs per test were varied at the maximum and minimum values defined by their respective distributions (Table 1). In the PSA, we performed 2000s-order Monte-Carlo simulations and plotted each result on a cost-effectiveness plane. Cost-effectiveness acceptability curves (CEACs) were constructed to determine the cost-effectiveness threshold.
Results
Costs
Costs to the provider
Base-case median costs were higher for VCT per individual tested (US$7.82; range, US$4.54–US$15.14) than for PICT per individual tested (US$7.29; range, US$2.30–US$14.67) but were lower than HBT per individual tested (US$11.62; range, US$4.32–US$19.83; Table 2). The small difference in costs between the two facility-based strategies (VCT & PICT) can be attributed to higher personnel costs for VCT which probably resulted from a longer time spent on HCT. As expected, HBT costed more than facility-based strategies, driven by higher personnel costs and transport costs. Like VCT and PICT costs, cost component proportions of HBT costs were almost equal: personnel (32.2%), supplies (36.6%) and transport (29.6%). Resources used are reported by HCT strategy in Appendix 8.
Costs to the patient
The median base-case total cost to the patient per VCT visit was US$1.08 (range, US$0.00–US$19.58). A breakdown of total costs into explicit (median, US$0; range US$0–US$18.62) and implicit costs (median, US$0.86; range, US$0.00–US$4.65) showed most costs (~ 80%) were implicit, which reflected waiting times and travelling times to the hospital (Appendix 9).
Sensitivity analysis
Average and median costs of VCT and PICT from the provider’s perspective were most sensitive to variations in operation and maintenance, and capital costs (Appendix 10). However, closer examination revealed this was largely a result of high estimates obtained from reports in Kenya and Uganda, which were unlikely to represent real costs in Mozambique [13, 14].
Although unit costs of VCT and PICT were less sensitive to test-kit prices, the large extent of overlap between them in the sensitivity analysis suggested that accurate determination of these prices is crucial, since the order of costs could differ should assumptions change. On the other hand, HBT costs were most sensitive to the choice of percentile cut-off for the upper limit of several time-related variables. Median HBT cost was especially sensitive to the low estimate, varying from the base-case value by 41%. Base-case average and median VCT costs from the patient’s perspective were generally robust (Appendix 11).
HCT costs and cost-effectiveness of HCT to link to care
Base-case results
The costs per HIV-positive individual linked to care, covering both testing and linkage cost, were estimated at US$289.67 for VCT, US$121.46 for PICT, and US$643.37 for HBT (Table 3). PICT was less expensive than VCT but also resulted in a lower proportion of PLHIV linked to care. As PICT is less costly but also less efficacious than VCT, PICT ICER of US$4.15 could be interpreted as savings per indivual not linked to care. PICT falls in the low cost/worse outcome quadrant of the cost-effectiveness plane (Appendix 12). In comparison with VCT, the HBT ICER (−US$8.57) was in the high cost/worse outcome quadrant.
Sensitivity analyses
HCT costs per individual linked to care were most sensitive to the average cost per test (Appendices 13, 14). However, within the narrower ranges elicited from the sensitivity analysis for unit costs, base-case linkage-to-care costs for VCT and PICT were robust. Unfortunately, there was still great uncertainty in the determined HCT costs of HBT.
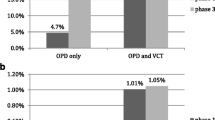
Similarly, ICERs were most sensitive to unit costs per test although they too were fairly robust within the narrower ranges obtained from the sensitivity analysis for unit costs (Appendix 15). Both the DSA and PSA showed significant uncertainty in determining the cost-effectiveness of PICT in relation to VCT, notwithstanding considerations of the cost-effectiveness threshold. HBT, however, was likely a dominated strategy. The probabilistic results were similar to the deterministic findings (Fig. 1).
Plots of 2000s-order Monte-Carlo simulations of incremental cost per proportion linked to care gained on high cost/worse outcome and low cost/worse outcome quadrants of the cost-effectiveness plane. a Monte-Carlo simulations for the comparison between PICT and VCT; b Monte-Carlo simulations for the comparison between HBT and VCT. *Interpretation of ICERs in the low cost/worse outcome quadrant is dependent on the WTA threshold. #ICERs in the high cost/worse outcome quadrant represent a dominated scenario for the strategy under comparison. Note: The red ellipse of confidence encircles 95% of the bootstrapped ICERs, and black solid lines represent quasi 95% confidence intervals a ICERs have almost equal chance of falling into the high cost/worse outcome and low cost/worse outcome quadrants. b ICERs are more likely to fall in the high cost/worse outcome quadrant. PICT provider-initiated counselling and testing, HBT home-based testing; VCT voluntary counselling and testing, ICER incremental cost-effectiveness ratio, WTA willingness to accept
The interpretation of ICERs in the low cost/worse outcome quadrant for the PICT comparison is dependent on the minimum willingness-to-accept (WTA) for every individual successfully linked to care. As there was no clearly defined WTA threshold, a CEAC was constructed (Fig. 2). Since the elicited threshold of US$4.53 was greater than the base-case and average ICER in the PSA, we concluded PICT was not cost-effective relative to VCT, although this result was only marginal. Moreover, both the DSA and PSA indicated significant uncertainty in this result. Interestingly, both strategies had almost equal likelihood of being cost-effective when the cost-effectiveness threshold was mapped on the Monte-Carlo plot (Appendix 16). A CEAC was not produced for the comparison between HBT and VCT because HBT was clearly dominated (high cost/worse outcome) at all cost-effectiveness thresholds above zero, i.e., the corresponding CEAC is a flat horizontal line at y = 0.
CEAC of the comparison between PICT and VCT. The interpretation of ICERs in the low cost/worse outcome quadrant is dependent on the cost-effectiveness threshold or the minimum WTA. PICT was initially the most cost-effective strategy up until a WTA of US$4.53. At higher WTA, VCT was undoubtly the more cost-effective strategy. CEAC cost-effectivenss acceptability curves, PICT provider-initiated counselling and testing, VCT voluntary counselling and testing, ICER incremental cost-effectiveness ratio, WTA willingness to accept
Discussion
To our knowledge, this is the first study in Mozambique to estimate costs and cost-effectiveness of VCT, PICT, and HBT. We found the median cost per VCT attendance to be as low as US$1.00, largely comprising implicit costs. This is commensurate with VCT prices and patients’ willingness-to-pay reported elsewhere [34, 35], suggesting that the costs to patients were reasonable. However, differences in health systems, wage structure, and socioeconomic conditions between countries may lead to different valuations of explicit and implicit costs.
We found the average cost to the provider per individual tested and derived costs per HIV-positive patient linked to care to be greatest for HBT, followed by VCT and PICT. Both the magnitude and trend of costs elicited were mostly consistent with the available literature for neighboring SSA countries (in 2009 prices), with the exception of the study by Menzies et al. (in 2007 prices) [13,14,15]. Notwithstanding considerations for effectiveness, PICT is the cheapest for potential HCT scale-up in areas with inadequate coverage. However, in resource-limited Mozambique, HCT scale-up requires more than mere consideration of HCT costs as improvement of existing healthcare infrastructure and expansion of the healthcare workforce are also needed.
We found HBT to be substantially more expensive than VCT and PICT. This was not consistent with the available literature. Five studies across Uganda, Kenya, and South Africa reported HBT costs ranging from US$5.00–US$29.00 per client tested that were in several cases lower than reported VCT and PICT costs [14, 15, 18,19,20]. A difference in cost analysis approach likely accounts for this discrepancy, since reported cost estimates from a program perspective are more likely to capture economies of scale accurately, particularly for HBT. Another reason could be the numerous far-lying residential areas in Manhiça [21], which probably required substantial resources for HBT.
CEA results suggested PICT was not cost-effective to link PLHIV to care, relative to VCT; more precisely, PICT was less expensive but also less effective than VCT. However, this result was only marginal. Moreover, the lack of robustness in the base-case results of the CEA comparing PICT and VCT, coupled with the fact that PICT was consistently reported to be cheaper than VCT [13, 15] yet with almost comparable linkage-to-care proportions [6, 36], suggests a high possibility that PICT could be considered cost-effective as well, especially in areas with limited resources. PICT could be considered for expansion and scale-up, depending on the context and available resources, in line with regional trends [37,38,39,40]. For example, in remote areas where health facilities may be understaffed, PICT could be expanded to include the general population to lower costs of HCT but still yield reasonable linkage-to-care proportions. Conversely, in areas with more resources and likely higher WTA, PICT could be limited.
As expected, HBT was more expensive and had a lower expected linkage-to-care proportion than VCT. This was consistent with several studies [19, 41,42,43,44,45,46]. However, other reports showed high linkage-to-care proportions for HBT (47.5%–70.0%) [47,48,49,50,51]. Although definitions of linkage to care were inconsistent in the literature, Kiene et al. highlighted an obvious but important trend: HBT programs that facilitate linkage perform better than those that do not [52]. Sharma et al.’s systematic review of 126 studies confirmed this trend, showing high linkages to care for strategies that facilitated linkages [6]. Similarly, Gilbert et al. found community-based TB and HIV integrated screening and linkcage to care strategies to be cost-effective in South Africa [53]. Moreover, the Manhiça cohort study investigators also hypothesized that strategies to facilitate linkage to care were important for cost-effectiveness [12]. HBT could be cost-effective if integrated with facilitated linkage strategies.
Our study had limitations. Because data were only available for PLHIV, we modelled total program costs. The inability to determine real program costs may limit the usefulness of our findings for policymakers [54]. Moreover, the lack of methodological consistency between our study and published studies may result in overestimates and bias cost comparisons. In Mozambique, some HIV-testing costs are borne by the government and others by international donors; our study did not distinguish between the two. In addition, analysis of costs to the provider did not include other costs, such as training, supply chain, and program management. HBT, as analyzed in this study, referred to door-to-door universal testing, and results cannot be extrapolated to other forms of community testing, such as index case testing, which is prominent in SSA testing programs.
Results from this study are hardly generalizable to other countries. Manhiça is a small, semi-rural district in Mozambique where HCT services are offered free-of-charge at district hospitals. It is unclear how the imposition of charges, like in Kenya and Tanzania [34, 35], would influence HCT uptake and linkage-to-care. The representativeness and precision of this study’s findings may also be limited since only data from a single cohort study were used, and findings are subject to limitations in that study. For example, López-Varela et al. acknowledged that attrition in linkage to care in the cohort study could have been overestimated due to poor record keeping. However, such overestimation is likely lower than in other studies because the authors used data from the Health and Disease Surveillance System [12].
Because our dataset lacked detailed cost information, we were unable to evaluate the combination of VCT with either PICT or HBT against standalone VCT. Future studies, however, could investigate such combinations and provide information to policymakers on how best to improve existing HIV-testing policies in Mozambique.
A CEA may be unsuitable for assessing the utility of HBT to meet targets for HIV eradication. CEAs are often designed to maximize efficiency at the expense of achieving distributive equality and equity [55]. Therefore, active HCT approaches, such as HBT, are seldom favored over more passive strategies due to their high unit costs per outcome achieved. Nevertheless, such strategies play a crucial role in achieving HIV eradication. HBT might not be cost-effective but may be equitable because HBT can reach populations distinct from those reached by facility-based strategies [12]. CEAs can address health equity concerns either through an equity impact analysis or an equity trade-off analysis as introduced by Cookson et al. [56] Round et al.’s analytical framework, which uses equity weights in decision analyses, may be useful [57]. Addressing equity is relevant for HCT strategies because factors like age, sex, and socioeconomic status may result in differential rates of uptake and linkage to care [12, 58, 59].
Despite these limitations, this study generates, for the first time, information for HIV healthcare policy decision making in Southern Mozambique, a setting characterized by one of the highest community based HIV prevalences in the world (i.e., 40%). From the research perspective, this project calls for the need to test the cost-effectiveness of comprehensive home-based strategies including not only screening but also linkage to care and promotion of ART adherence. A similar combination prevention approach involving universal HIV testing and treatment has recently been assessed to be a cost-effective strategy at thresholds greater than US$800 per DALY averted in Zambia and South Africa [60]. This may be seen as a reasonable threshold also for Mozambique, considering the traditional threshold of three times the gross domestic product (GDP) per capita and that the GDP per capita of Mozambique is just below US$500. However, site specific studies should be carried out to obtain valuable information.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Kranzer K, Zeinecker J, Ginsberg P, Orrell C, Kalawe NN, Lawn SD, Bekker L, Wood R. Linkage to HIV care and antiretroviral therapy in Cape Town, South Africa. PLoS ONE. 2010;5(11): e13801.
Naik R, Doherty T, Jackson D, Tabana H, Swanevelder S, Thea DM, Feeley FG, Fox MP. Linkage to care following a home-based HIV counselling and testing intervention in rural South Africa. J Int AIDS Soc. 2015;18(1):19843.
Elul B, Lahuerta M, Abacassamo F, Lamb MR, Ahoua L, McNairy ML, Tomo M, Horowitz D, Sutton R, Mussa A, Gurr D, Jani I. A combination strategy for enhancing linkage to and retention in HIV care among adults newly diagnosed with HIV in Mozambique: study protocol for a site-randomised implementation science study. BMC Infect Dis. 2014;14:549.
Haber N, Tanser F, Bor J, Naidu K, Mutevedzi T, Herbst K, Porter K, Pillay D, Bärnighausen T. From HIV infection to therapeutic response: a population-based longitudinal HIV cascade-of-care study in KwaZulu-Natal, South Africa. Lancet HIV. 2017;4(5):e223–30.
Rosen S, Fox MP. Retention in HIV care between testing and treatment in sub-Saharan Africa: a systematic review. PLoS Med. 2011;8(7): e1001056.
Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature. 2015;528(7580):S85.
Sanga ES, Lerebo W, Mushi AK, Clowes P, Olomi W, Maboko L, Zarowsky C. Linkage into care among newly diagnosed HIV-positive individuals tested through outreach and facility-based HIV testing models in Mbeya, Tanzania: a prospective mixed-method cohort study. BMJ Open. 2017;7(4): e013733.
Provider initiated counselling and testing for health: Health professionals’ views on implementation at a primary health care level in Matola District, Mozambique. http://www.ev4gh.net/wp-content/uploads/2013/09/Gilda-Gondola-Sitefane-Abstract-pdf.pdf Accessed 15 Jun 2018
Republica de Moçambique, Conselho Nacional de Combate ao HIV e SIDA, Plano Estratégico Nacional de Resposta ao HIV e SIDA 2015–2019, Maputo, 2015. http://www.misau.gov.mz/index.php/planos-estrategicos-do-hiv Accessed Aug 2020
PEPFAR. Mozambique Operational Plan (COP/ROP) 2017 strategic direction summary. PEPFAR; 2017. https://www.pepfar.gov/documents/organization/272018.pdf Accessed 17 Aug 2018
Mshweshwe-Pakela N, Mabuto T, Ntombela N, Hlongwane M, Kubeka G, Kerrigan DL, Hoffmann CJ. Facilitators and barriers to implementing provider-initiated HIV counselling and testing at the clinic-level in Ekurhuleni District, South Africa. Implement Sci Commun. 2022. https://doi.org/10.1186/s43058-022-00269-3.
Lopez-Varela E, Fuente-Soro L, Augusto OJ, Sacoor C, Nhacolo A, Karajeanes E, Vaz P, Naniche D. The continuum of HIV care in rural Mozambique: the implications of HIV testing modality on linkage and retention. J Acquir Immune Defic Syndr. 2018;78(5):527–35.
Obure CD, Vassall A, Michaels C, Terris-Prestholt F, Mayhew S, Stackpool-Moore L, Warren C, Watts C. Optimising the cost and delivery of HIV counselling and testing services in Kenya and Swaziland. Sex Transm Infect. 2012;88(7):498–503.
Mulogo EM, Batwala V, Nuwaha F, Aden AS, Baine OS. Cost effectiveness of facility and home based HIV voluntary counseling and testing strategies in rural Uganda. Afr Health Sci. 2013;13(2):423–9.
Menzies N, Abang B, Wanyenze R, Nuwaha F, Mugisha B, Coutinho A, Bunnell R, Mermin J, Blandford JM. The costs and effectiveness of four HIV counseling and testing strategies in Uganda. AIDS. 2009;23(3):395–401.
Sweat M, Gregorich S, Sangiwa G, Furlonge C, Balmer D, Kamenga C, Grinstead O, Coates T. Cost-effectiveness of voluntary HIV-1 counselling and testing in reducing sexual transmission of HIV-1 in Kenya and Tanzania. Lancet. 2000;356(9224):113–21.
Terris-Prestholt F, Kumaranayake L, Foster S, Kamali A, Kinsman J, Basajja V, Nalweyso N, Quigley M, Kengeya-Kayondo J, Whitworth J. The role of community acceptance over time for costs of HIV and STI prevention interventions: analysis of the Masaka Intervention Trial, Uganda, 1996–1999. Sex Transm Dis. 2006;33(4):000–000.
Negin J, Wariero J, Mutuo P, Jan S, Pronyk P. Feasibility, acceptability and cost of home-based HIV testing in rural Kenya. Trop Med Int Health. 2009;14(8):849–55.
Tumwesigye E, Wana G, Kasasa S, Muganzi E, Nuwaha F. High uptake of home-based, district-wide, HIV counseling and testing in Uganda. AIDS Patient Care STDS. 2010;24(11):735–41.
Tabana H, Nkonki L, Hongoro C, Doherty T, Ekström AM, Naik R, Zembe-Mkabile W, Jackson D, Thorson A. A cost-effectiveness analysis of a home-based HIV counselling and testing intervention versus the standard (facility based) HIV testing strategy in rural South Africa. PLoS ONE. 2015;10(8): e0135048.
González R, Munguambe K, Aponte J, Bavo C, Nhalungo D, Macete E, Alonso P, Menéndez C, Naniche D. High HIV prevalence in a southern semi-rural area of Mozambique: a community-based survey. HIV Med. 2012;13(10):581–8.
González R, Augusto OJ, Munguambe K, Pierrat C, Pedro EN, Sacoor C, De Lazzari E, Aponte JJ, Macete E, Alonso PL, Menendez C, Naniche D. HIV Incidence and spatial clustering in a rural area of Southern Mozambique. PLoS ONE. 2015;10(7): e0132053.
Frick KD. Micro-costing quantity data collection methods. Med Care. 2009;47(7 Suppl 1):S76–81.
Mwenge L, Sande L, Mangenah C, Ahmed N, Kanema S, d’Elbée M, Sibanda E, Kalua T, Ncube G, Johnson CC, Hatzold K, Cowan FM, Corbett EL, Ayles H, Maheswaran H, Terris-Presthold F. Costs of facility-based HIV testing in Malawi, Zambia and Zimbabwe. PLoS ONE. 2017;12(10): e0185740.
CIA factbook. Mozambique vs. Zimbabwe. https://www.indexmundi.com/factbook/compare/mozambique.zimbabwe Accessed 19 Jun 2018
CIA factbook. Mozambique vs. Malawi. https://www.indexmundi.com/factbook/compare/mozambique.malawi Accessed 19 Jun 2018
OANDA. Currency Converter. https://www.oanda.com/currency/converter/ Accessed 19 Jun 2018
Lawyers from TTA-Sociedade de Advogados and, PLMJ. National Minimum Wages 2016–2017. Maputo, Mozambique: PLMJ International Legal Network; 2016. https://www.plmj.com/xms/files/newsletters/2016/junho/Mozambique_-_National_minimum_wages_2016___2017.pdf Accessed 17 Aug 2018
Akumu J. Overview of the Global Fuel Economy Initiative. http://wedocs.unep.org/bitstream/item/21675/Overview%20of%20the%20Global%20Fuel%20Economy%20Initiative%2C%20Jane%20Akumu%2C%20UN%20Environment.pdf?sequence=2 Accessed 19 Jun 2018
Management Sciences for Health, World Health Organisation. International drug price indicator guide 2014. World Health Organisation; 2015. http://apps.who.int/medicinedocs/documents/s21982en/s21982en.pdf Accessed 19 Jun 2018
Larson B, Schnippel K, Ndibongo BLL, Fox MPRS. How to estimate the cost of point-of-care CD4 testing in program settings: an example using the Alere Pima™ analyzer in South Africa. PLoS ONE. 2012;7(4): e35444.
Mettler Toledo. Tips 250 μL 1000/Pkg RC-250. https://www.mt.com/gb/en/home/products/pipettes/bioclean-pipette-tip/packaging/bagged-tips/RC-250.html Accessed 19 Jun 2018
Worldbank. Mozambique: Pump price for gasoline (US $/liter). http://www.factfish.com/statistic-country/mozambique/pump%20price%20for%20gasoline Accessed 19 Jun 2018
Thielman NM, Chu HY, Ostermann J, Itemba DK, Mgonja A, Mtweve S, Bartlett JA, Shao JF, Crump JA. Cost-effectiveness of free HIV voluntary counseling and testing through a community-based AIDS service organization in Northern Tanzania. Am J Public Health. 2006;96(1):114–9.
Forsythe S, Arthur G, Ngatia G, Mutemi R, Odhiambo J, Gilks C. Assessing the cost and willingness to pay for voluntary HIV counselling and testing in Kenya. Health Policy Plan. 2002;17(2):187–95.
Leon N, Mathews C, Lewin S, Osler M, Boulle A, Lombard C. A comparison of linkage to HIV care after provider-initiated HIV testing and counselling (PITC) versus voluntary HIV counselling and testing (VCT) for patients with sexually transmitted infections in Cape Town, South Africa. BMC Health Serv Res. 2014;14(1):350.
Wanyenze RK, Nawavvu C, Namale AS, Mayanja B, Bunnell R, Abang B, Amanyire G, Sewankambo NK, Kamya MR. Acceptability of routine HIV counselling and testing, and HIV seroprevalence in Ugandan hospitals. Bull World Health Organ. 2008;86(4):302–9.
Kamoto K, Makombe SD, Nkhata A, Jahn A, Moses P, Schouten EJ, Harries AD. HIV testing and antiretroviral therapy in government and mission hospitals in Malawi: 2002–2007. Malawi Med J. 2008;20(1):4–6.
Perez F, Zvandaziva C, Engelsmann B, Dabis F. Acceptability of routine HIV testing (“opt-out”) in antenatal services in two rural districts of Zimbabwe. J Acquir Immune Defic Syndr. 2006;41(4):514–20.
Baggaley R, Hensen B, Ajose O, Grabbe KL, Wong VJ, Schilsky A, Lo Y-R, Lule F, Granich R, Hargreaves J. From caution to urgency: the evolution of HIV testing and counselling in Africa. Bull World Health Organ. 2012;90:652-658B.
Parker LA, Jobanputra K, Rusike L, Mazibuko S, Okello V, Kerschberger B, Jouquet G, Cyr J, Teck R. Feasibility and effectiveness of two community-based HIV testing models in rural Swaziland. Trop Med Int Health. 2015;20(7):893–902.
Labhardt ND, Motlomelo M, Cerutti B, Pfeiffer K, Kamele M, Hobbins MA, Ehmer J. Home-based versus mobile clinic HIV testing and counseling in rural Lesotho: a cluster-randomized trial. PLoS Med. 2014;11(12): e1001768.
Iwuji CC, Orne-Gliemann J, Larmarange J, Okesola N, Tanser F, Thiebaut R, Rekacewicz C, Newell ML, Dabis F. Uptake of home-based HIV testing, linkage to care, and community attitudes about ART in rural KwaZulu-Natal, South Africa: descriptive results from the first phase of the ANRS 12249 TasP cluster-randomised trial. PLoS Med. 2016;13(8): e1002107.
Plazy M, Farouki KE, Iwuji C, Okesola N, Orne-Gliemann J, Larmarange J, Lert F, Newell ML, Dabis F, Dray-Spira R. Access to HIV care in the context of universal test and treat: challenges within the ANRS 12249 TasP cluster-randomized trial in rural South Africa. J Int AIDS Soc. 2016;19(1):20913.
Naik R, Zembe W, Adigun F, Jackson E, Tabana H, Jackson D, Feeley F, Doherty T. What influences linkage to care after home-based HIV counseling and testing? AIDS Behav. 2018;22(3):722–32.
Medley A, Ackers M, Amolloh M, Owuor P, Muttai H, Audi B, Sewe M, Laserson K. Early uptake of HIV clinical care after testing HIV-positive during home-based testing and counseling in western Kenya. AIDS Behav. 2013;17(1):224–34.
Smith JA, Sharma M, Levin C, Baeten JM, van Rooyen H, Celum C, Hallett TB, Barnabas RV. Cost-effectiveness of community-based strategies for HIV. Lancet HIV. 2015;2(4):e159-168.
Asiimwe S, Ross JM, Arinaitwe A, Tumusiime O, Turyamureeba B, Roberts DA, O’Malley G, Barnabas RV. Expanding HIV testing and linkage to care in southwestern Uganda with community health extension workers. J Int AIDS Soc. 2017;20(Suppl 4):21633.
Barnabas RV, van Rooyen H, Tumwesigye E, Murnane PM, Baeten JM, Humphries H, Turyamureeba B, Joseph P, Krows M, Hughes JP, Celum C. Initiation of antiretroviral therapy and viral suppression after home HIV testing and counselling in KwaZulu-Natal, South Africa, and Mbarara district, Uganda: a prospective, observational intervention study. Lancet HIV. 2014;1(2):e68–76.
van Rooyen H, Barnabas RV, Baeten JM, Phakathi Z, Joseph P, Krows M, Hong T, Murnane PM, Hughes J, Celum C. High HIV testing uptake and linkage to care in a novel program of home-based HIV counseling and testing with facilitated referral in KwaZulu-Natal, South Africa. J Acquir Immune Defic Syndr. 2013;64(1):e1–8.
Maman D, Ben-Farhat J, Chilima B, Masiku C, Salumu L, Ford N, Mendiharat P, Szumilin E, Masson S, Etard JF. Factors associated with HIV status awareness and linkage to care following home based testing in rural Malawi. Trop Med Int Health. 2016;21(11):1442–51.
Kiene SM, Kalichman SC, Sileo KM, Menzies NA, Naigino R, Lin CD, Bateganya MH, Lule H, Wanyenze RK. Efficacy of an enhanced linkage to HIV care intervention at improving linkage to HIV care and achieving viral suppression following home-based HIV testing in rural Uganda: study protocol for the Ekkubo/PATH cluster randomised controlled trial. BMC Infect Dis. 2017;17(1):460.
Gilbert JA, Shenoi SV, Moll AP, Friedland GH, Paltiel AD, Galvani AP. Cost-effectiveness of community-based TB/HIV screening and linkage to care in rural South Africa. PLoS ONE. 2016;11(12): e0165614. https://doi.org/10.1371/journal.pone.0165614.
Koop G. Analysis of economic data. 4th ed. Chichester: Wiley; 2013.
Kelleher JP. Efficiency and equity in health: philosophical considerations. Encyclopedia of Health Economics, vol. 1. Amsterdam: Elsevier; 2014. p. 259–66.
Cookson R, Mirelman AJ, Griffin S, Asaria M, Dawkins B, Norheim OF, Verguet S, Culyer AJ. Using cost-effectiveness analysis to address health equity concerns. Value Health. 2017;20(2):206–12.
Round J, Paulden M. Incorporating equity in economic evaluations: a multi-attribute equity state approach. Eur J Health Econ. 2018;19(4):489–98.
Osoti AO, John-Stewart G, Kiarie JN, Barbra R, Kinuthia J, Krakowiak D, Farquhar C. Home-based HIV testing for men preferred over clinic-based testing by pregnant women and their male partners, a nested cross-sectional study. BMC Infect Dis. 2015;15(1):298.
Geoffroy E, Schell E, Jere J, Khozomba N. Going door-to-door to reach men and young people with HIV testing services to achieve the 90–90-90 treatment targets. Public Health Action. 2017;7(2):95–9.
Thomas R, Probert WJM, Sauter R, Mwenge L, Singh S, Kanema S, Vanqa N, Harper A, Burger R, Cori A, Pickles M, Bell-Mandla N, Yang B, Bwalya J, Phiri M, Shanaube K, Floyd S, Donnell D, Bock P, Ayles H, Fidler S, Hayes RJ, Fraser C, Hauck K. Cost and cost-effectiveness of a universal HIV testing and treatment intervention in Zambia and South Africa: evidence and projctions from the HPTN 071 (PopART) trial. Lancet Global Health. 2021;9:e668–80.
Acknowledgements
This study was made possible with support from the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) under the terms of CoAg GH000479 (Scaling-up HIV counselling & testing services in a rural population by strengthening the health demographic surveillance system, in Manhiça, Mozambique). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies. ISGlobal is a member of the CERCA Programme, Generalitat de Catalunya. We thank the personnel of the VCT, HBT, and PICT of the Manhiça District Hospital and CISM for their collaboration in collecting data. Data analysis and manuscript writing was done in the context of the Master of Public Health programme at the Imperial College London.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JHC cleaned the data, performed the economic analysis, and was also a major contributor in writing the manuscript. RT and ES provided guidance on the method of data anlaysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Mozambican National Bioethics Committee and the Institutional Review Boards at the Hospital Clinic of Barcelona (Spain) and the Manhiça Health Research Centre. It was also reviewed according to Centers for Disease Control and Prevention (CDC) human research protection procedures and was determined to be research; however, CDC was not engaged directly with research participants. The purpose of the main study was explained to participants, and written informed consent was obtained.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendices
Appendix 1: Schematic of cohort study with figures used in the economic evaluation
Numbers in Fig. 3 are used in the cohort decision model presented in Fig. 1.
Steps involved in the enrollment of participants into the study across all three HIV counselling and testing strategies. [16] Attrition at each step was quantified. VCT voluntary counselling and testing, PICT provider-initiated counselling and testing, HBT home-based testing
Appendix 2: Copy of the questionnaire administered to study participants to elicit demographic information
Questionnaire was administered in Portuguese.

Appendix 3: Copy of the questionnaire administered to study participants to elicit cost-related information for voluntary counselling and testing (VCT) from the patient’s perspective
Questionnaire was administered in Portuguese.

Appendix 4: Copy of questionnaire used to collect time data, and data on health system resources used for voluntary counselling and testing (VCT), provider-initiated counselling and testing (PICT), or home-based testing (HBT)

Appendix 5: Unit costs (US$) of various resource categories employed in the micro-cost estimate approach, along with their low and high estimates as determined from individual sources (Manhiça District, Mozambique)
Resource | Unit cost, US$ | Low estimate, US$ | High estimate, US$ | Source |
|---|---|---|---|---|
Patient’s perspective | ||||
National monthly minimum wage (for agriculture and fisheries)a | 101.35 | 99.04 | 114.56 | [28] |
Provider’s perspective | ||||
Determine HIV rapid test kit | 1.07 | 0.98 | 1.16 | [30] |
Unigold HIV rapid test kit | 3.18 | 2.59 | 4.79 | [30] |
Lancets | 0.02 | No data | No data | CISM private communicationb |
Gloves | 0.01 | No data | No data | [31] |
Pipettes | 0.04 | No data | No data | [32] |
Nurse monthly wage | 792.00 | No data | No data | CISM private communicationb |
Nurse assistant monthly wage | 400.00 | No data | No data | CISM private communicationb |
Counsellor monthly wage | 258.32 | No data | No data | CISM private communicationb |
Fuel, per litrec | 1.55 | 1.20 | 1.60 | [33] |
Appendix 6: A cohort decision-analytic model (decision tree) comparing HCT strategies for linking HIV-positive patients to care in Manhiça District, Mozambique
See Fig.
Each branch depicts individual steps of the HIV care cascade as described in the cohort study and is conditional on the previous step. The blue square node represents a decision node, green circular nodes represent chance nodes, and red triangles illustrate terminal nodes. HCT HIV counselling and testing, PICT provider-initiated counselling and testing, HBT home-based testing, VCT voluntary counselling and testing
Appendix 7: Range of input values explored in the univariate sensitivity analysis for each assumption (input) made in the determination of costs per individual tested
Inputs | Input values | Source of estimates | ||
|---|---|---|---|---|
Base-case | Low estimate | High estimate | ||
Patient’s perspective | ||||
Minimum monthly wage, US$ | 101.35 | 99.04 | 114.56 | From Appendix 5 |
Monthly number of working hours | 176 | 141 (−20%) | 211 (+ 20%) | Empiric determinationb |
Provider’s perspective | ||||
Percentile cut-off for upper limit of variables | 85th | 80th | 90th | Empiric determinationb |
HIV test kit prices, US$ | (Determine = 1.07; Unigold = 3.18) | (Determine = 0.98; Unigold = 2.59) | (Determine = 1.16; Unigold = 4.79) | From Appendix 5 |
Percentage of total costs as capital costs | 3.27 | 3.00 | 14.23a | |
Percentage of recurrent costs as O & M costs | 1.65 | 0.55 | 28.72a | |
Nurse monthly wage, US$ | 792.00 | 633.60 (−20%) | 950.40 (+ 20%) | Empiric determinationb |
Nurse assistant monthly wage, US$ | 400.00 | 320.00 (−20%) | 480.00 (+ 20%) | Empiric determinationb |
Counsellor monthly wage, US$ | 258.32 | 206.66 (−20%) | 309.98 (+ 20%) | Empiric determinationb |
2014 fuel prices, US$/l | 1.55 | 1.20 | 1.60 | From Appendix 5 |
Travelling speed, km/h | 50 | 40 (−20%) | 60 (+ 20%) | Empiric determinationb |
Fuel consumption, l/km | 0.143 | 0.114 (−20%) | 0.171 (+ 20%) | Empiric determinationb |
Appendix 8: Quantities of resources used in each testing modality
Testing modality | Quantity by test strategy (cost in the case of transportation, food and drinks, and others) Mean values and standard deviation are reported | ||
|---|---|---|---|
VCT | PICT | HBT | |
Patient’s perspective | |||
Transport (bus, taxi, etc.), US$ | 0.19 (0.35) | – | − |
Drink + Food, US$ | 0 (0.25) | − | − |
Waiting time (hours) | 0.95 (0.94) | − | − |
Travelling time (hours) | 0.82 (0.71) | − | − |
Any other direct cost, US$ | 0.1 (1.05) | − | − |
“Determine” HIV rapid test kit (number) | 1 (0) | 1 (0) | 1.03 (0.27) |
Provider’s perpective | |||
“Unigold” HIV rapid test kit (number) | 1 (0) | 1 (0) | 1.01 (0.12) |
Lancets (number) | 1 (0) | 1 (0) | 1.04 (0.21) |
Gloves (number) | 1 (0) | 1(0) | 1.16 (0.38) |
Pipettes (number) | 1 (0) | 1 (0) | 1 (0) |
Personnel time (minutes)a | 46.53 (12.64) | 30.72 (12.60) | 58.45 (15.30) |
Kilometers to reach the patient | − | − | 13.7 (12.75) |
Appendix 9: Box and whiskers plot of median explicit and implicit costs of voluntary counselling and testing, in US$, to the patient
See Fig.
Total cost was driven largely by implicit costs. It can thus be inferred that transport, food and drink costs were insignificant in comparison to opportunity costs of waiting and travelling times. Two anomalous values for explicit cost are not shown: 12.76 and 18.62. Values for implicit costs outside the interquartile range: 3.46, 3.74, 4.03 and 4.65. The value of zero for implicit costs reflect minimal travelling and waiting times, which was the case for a couple of patients
5.
Appendix 10: Sensitivity analysis of average and median costs per person tested
See Fig.
Tornado plots of average and median costs per person tested when assumptions were varied between the high and low estimates. a Average costs of VCT, b Median costs of VCT, c Average costs of PICT, d Median costs of PICT, e Average costs of HBT, f Median costs of HBT. Varying nurses’ monthly wage did not affect median cost of VCT and average cost of HBT. *Black vertical lines represent base-case costs
6.
Appendix 11: Impact of varying assumptions on base-case average and median costs of VCT from the patient’s perspective among participants who tested HIV-positive
Parameter | Average cost (SD), US$ | Median cost (range), US$ |
|---|---|---|
Base-case analysis | 1.34 (1.46) | 1.08 (0.00–19.58) |
Monthly minimum wagea | ||
Low estimate = US$99.04 | 1.32 (1.45) | 1.07 (0.00–19.56) |
High estimate = US$114.56 | 1.47 (1.50) | 1.19 (0.00–19.70) |
Number of working hours per montha | ||
Low estimate = 141 h | 1.59 (1.55) | 1.32 (0.00–19.82) |
High estimate = 211 h | 1.17 (1.40) | 0.96 (0.00–19.42) |
Appendix 12: Cost-effectiveness plane depicting the four quadrants in which ICERs may reside
See Fig.
7.
Appendix 13: Tornado plots illustrating fluctuations in linkage-to-care costs between the minimum (low) and maximum (high) values of individual model parameters in the univariate sensitivity analysis
See Fig.
a Linkage-to-care costs of VCT, b Linkage-to-care costs of PICT, c Linkage-to-care costs of HBT. *Black vertical lines represent base-case results. #Percentage change from base-case costs quantifies the impact of varying cost per test between strategies. VCT voluntary counselling and testing, PICT provider-initiated counselling and testing, HBT home-based testing
8.
Appendix 14: Impact of varying probabilities and costs used to parameterise the decision tree on linkage-to-care costs of VCT, PICT, and HBT from the provider’s perspective, US$
Model parameters | VCT | PICT | HBT | |||
|---|---|---|---|---|---|---|
Min parameter valuea | Max parameter valuea | Min parameter valuea | Max parameter valuea | Min parameter valuea | Max parameter valuea | |
Probabilities | ||||||
Positive test result | 322.24 (+ 11.24%) | 263.38 (−9.08%) | 132.47 (+ 9.06%) | 111.79 (−7.96%) | 813.86 (+ 14.40%) | 547.15 (−7.53%) |
Enrolled into study | 344.07 (+ 18.78%) | 251.99 (−13.01%) | 141.39 (+ 16.41%) | 107.69 (−11.34%) | – | – |
Enrolled into care | 298.50 (+ 3.05%) | 285.88 (−1.31%) | 130.18 (+ 7.18%) | 116.06 (−4.45%) | 835.64 (+ 20.24%) | 535.66 (−15.97%) |
Attended first consultation | 312.83 (+ 8.00%) | 276.09 (−4.69%) | 133.15 (+ 9.62%) | 112.75 (−7.17%) | 736.03 (+ 26.50%) | 594.93 (−14.96%) |
Linked to care | 335.18 (+ 15.71%) | 258.26 (−10.84%) | 143.59 (+ 18.22%) | 107.47 (−11.52%) | 773.58 (+ 29.88%) | 540.62 (−16.74%) |
Costs | ||||||
VCT | 146.14 (−49.55%) | 474.41 (+ 63.78%) | – | – | – | – |
PICT | – | – | 53.45 (−56.00%) | 197.81 (+ 62.86%) | – | – |
HBT | – | – | – | – | 136.11 (−78.84%) | 1554.44 (+ 141.61%) |
Appendix 15: Tornado plots illustrating fluctuations in ICERs between the minimum (low) and maximum (high) values of individual model parameters in univariate sensitivity analysis
See Fig.
a ICERs for the comparison between PICT and VCT, b ICERs for the comparison between HBT and VCT. *Black vertical solid lines represent base-case results. Note: the area shaded red covers all negative ICERs and represents a dominated scenario by VCT for the strategy under comparison. Black dotted lines demarcate the range of ICERs for each comparison that would result from the corresponding ranges of HCT unit costs. a The shaded area between the lower black dotted line and the origin represents the likelihood that base-case ICER was not robust and a dominated scenario for PICT. b The area enclosed by both dotted lines lie within the shaded region, suggesting base-case findings that HBT was dominated were robust up to this range of unit costs. VCT voluntary counselling and testing, PICT provider-initiated counselling and testing, HBT home-based testing, ICER incremental cost-effectiveness ratios
9.
Appendix 16: Mapping the WTA threshold on the Monte-Carlo plot for the comparison between PICT and VCT
See Fig.
*ICERs in the south-west quadrant depict when the cost-effectiveness of PICT is dependent on the WTA threshold. #ICERs in the north-west quadrant represent a dominated scenario for PICT. The red ellipse of confidence encircles 95% of the bootstrapped ICERs while black solid lines represent quasi 95% confidence intervals. There is an almost equal chance for ICERs to fall either side of the threshold within the region bounded by the quasi 95% confidence intervals, implying that PICT have equal likelihood of being cost-effective or not relative to VCT. WTA willingness-to-accept, VCT voluntary counselling and testing, PICT provider-initiated counselling and testing, ICER incremental cost-effectiveness ratio
10.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Choo, J.H., Lopez-Varela, E., Fuente-Soro, L. et al. Costs and cost-effectiveness of HIV counselling and testing modalities in Southern Mozambique. Cost Eff Resour Alloc 20, 49 (2022). https://doi.org/10.1186/s12962-022-00378-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-022-00378-9