Abstract
Background
An estimated 85% of research resources are wasted worldwide, while there is growing demand for context-based evidence-informed health policymaking. In low- and middle-income countries (LMICs), research uptake for health policymaking and practice is even lower, while little is known about the barriers to the translation of health evidence to policy and local implementation. We aimed to compile the current evidence on barriers to uptake of research in health policy and practice in LMICs using scoping review.
Methods
The scoping review followed the Preferred Reporting Items for Systematic Review and Meta-Analyses-extension for Scoping Reviews (PRISMA-ScR) and the Arksey and O'Malley framework. Both published evidence and grey literature on research uptake were systematically searched from major databases (PubMed, Cochrane Library, CINAHL (EBSCO), Global Health (Ovid)) and direct Google Scholar. Literature exploring barriers to uptake of research evidence in health policy and practice in LMICs were included and their key findings were synthesized using thematic areas to address the review question.
Results
A total of 4291 publications were retrieved in the initial search, of which 142 were included meeting the eligibility criteria. Overall, research uptake for policymaking and practice in LMICs was very low. The challenges to research uptake were related to lack of understanding of the local contexts, low political priority, poor stakeholder engagement and partnership, resource and capacity constraints, low system response for accountability and lack of communication and dissemination platforms.
Conclusion
Important barriers to research uptake, mainly limited contextual understanding and low participation of key stakeholders and ownership, have been identified. Understanding the local research and policy context and participatory evidence production and dissemination may promote research uptake for policy and practice. Institutions that bridge the chasm between knowledge formation, evidence synthesis and translation may play critical role in the translation process.
Similar content being viewed by others
Background
Globally, an estimated 85% of research resources are wasted due to errors, exaggeration and inefficiency [1, 2]. Contextual evidence synthesis is a fundamental component of evidence-informed health policymaking. Evidence synthesis relevant for the local context is needed to improve the health system’s performance and health outcomes [3]. Since the 1970s, both policymakers and researchers have given emphasis to the range of factors affecting health policymaking [4]. Evidence-informed policymaking is an interactive process that involves effective exchanges of knowledge between researchers and policymakers [5, 6]. It is aimed at minimizing policy failures in real world setting [7].
About 42% of research resource waste is avoidable through simple and inexpensive intervention [8]. However, multiple barriers exist, including poor access to good quality research, the low quantity of evidence in certain areas, lack of timeliness [9,10,11], information overload [12], and incompatibilities in priorities between researchers and policymakers [13]. The World Health Organization (WHO) recommends evidence-informed decision-making as having a key role in improving the effectiveness, efficiency, and equity of health policies and implementation [14]. Nevertheless, existing evidence is often not communicated in a timely way to decision-makers [3] resulting in wastage of resource invested in research [2, 15].
About 40–90% of research published from trials is not replicable [15,16,17], and no reliable evidence on the extent of research use, or its impact, exists [18]. These deficiencies highlight the need to create platforms for interaction between researchers and policy-makers as producers and as users of evidence [19]. This has been more apparent in the past two decades. Although evidence-informed health policymaking is central in achieving and sustaining innovative healthcare delivery in LMICs, priority-setting for health policy research remains an overlooked public health issue in LMICs [20]. There is a growing demand for platforms (centers used to create connection) dedicated to evidence uptake for policymaking both in high-income and LMICs [12, 21].
Research evidence is vital for policymaking, and the role of researchers in translating research evidence into policymaking is crucial [22]. Power relationships have significant impact on capacity development and on the links between research, policy and practice [23]. The multidisciplinary research approach has played a key role in the production of quality evidence of the complexity demand by policy [24], and has enhanced the engagement of various actors [25, 26]. Translation of evidence to policy needs collaboration among multidisciplinary scholars; collaboration between researchers and community representatives from diverse background and lay perspectives, and collaboration among community organizations across local, state, national, and international levels [24, 27, 28]. While there is some understanding of the critical barriers to research uptake and potential interventions, there is limited systematic knowledge of barriers to research uptake in LMICs. Therefore, the aim of this scoping review is to map barriers to research uptake for health policymaking in LMICs.
Review question(s)
-
What is the available evidence on barriers to uptake of research for policymaking in LMICs?
-
What are the challenges to research uptake for policymaking process in LMICs?
-
What recommendations might strengthen evidence uptake for policymaking in LMICs?
Methods
Scoping review methodology development
The scoping review followed the Preferred Reporting Items for Systematic Review and Meta-Analyses-extension for Scoping Reviews (PRISMA-ScR) [29,30,31,32,33] and the Arksey and O'Malley framework [34] to search published and grey literature. The completed PRISMA-ScR checklist [31] is presented as an additional file (Additional file 1).
Search strategy for identification of relevant studies
Relevant publications on research uptake for policymaking were identified from major databases (PubMed, Cochrane library, CNAHL(EBSCO), Global Health (Ovid), and direct search of Google Scholar and other sources, including sharing of high-quality evidence via email from authors and senior researchers. Only publications since 2000 were considered due to the growing interest in evidence-informed policy making over the last two decades [21]. Literature search was performed using Medical Subject Headings (MeSH) terms that considered participant, concept and context (PCC) (Table 1). Key terms used included “health evidence” OR “health research”, OR “policy making”, OR “evidence unit” OR “evidence translation center”, “research uptake” OR “evidence-informed health policymaking” AND “challenges of research uptake” OR “barriers to research uptake” OR “barriers to evidence to policy” OR “bottlenecks to research uptake” AND “low- and middle-income countries”. The search results were imported into EndNote citation manager [35] and duplicates were removed (Additional file 2).
Eligibility criteria
Inclusion criteria
-
Documents written in English
-
Published and relevant grey literature on evidence uptake to policy strategies
-
Evidence related to research uptake challenges and opportunities in LMICs. The LMICs were selected based on the World Bank’s country classification [36].
Exclusion criteria
-
Editorials, commentaries, fact sheets, conference abstracts and case-studies.
Screening and selection of studies
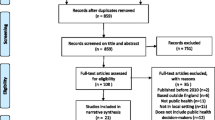
Publications were retrieved from selected databases, recorded using citation manager (EndNote), and duplicates were removed. Two authors (AS & EG) independently screened the title and abstracts of retrieved publications against the eligibility criteria, and based on review questions. Further appraisal assessed the methodological quality and findings before any article was included into the scoping review. Any disagreement between the two independent reviewers was resolved through consensus. If consensus was not reached, two of the senior authors (AF & TM) made a final decision based on the predetermined eligibility criteria. The screening and selection process of the scoping review was guided by the PRISMA flow diagram [29] (Fig. 1).
Data charting and synthesis
Basic descriptions of the included studies, including authors, date, aim of the article, type of study, key findings and recommendation for action, were abstracted and recorded in a Microsoft Word table (Additional file 3). Data charting was assisted by ATLAS.ti 9 for coding of the key findings related to research uptake and barriers in line with the review questions. The codes were merged to create themes and sub-themes using an inductive approach [31, 32] of barriers to research uptake for health policymaking in LMICs. We used hybrid scoping review approach through synthesis of the key findings from included relevant documents that were guided by both PRISMA-ScR [32] and the Arksey and O'Malley framework [37]. The meta-synthesis method was used to summarize the major barriers to research uptake and key recommendations to facilitate translation of evidence to policymaking in LMICs. These included the overall situation of research uptake, barriers to research uptake and strategies used to improve research uptake.
Results
Available evidence on research uptake
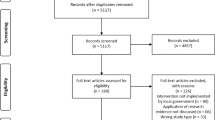
A total of 4291 relevant documents were retrieved from studies conducted in LMICs that were grouped based on the World Bank’s country classification [36] (Fig. 1). Of these, 142 met the inclusion criteria [3, 10, 12, 38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166], and a detailed description of the documents included is presented in a table (Additional file 3). Many of the publications indicated that research uptake for health policymaking and practice is still limited in LMICs [76,77,78,79,80,81,82,83,84,85,86,87,88, 90, 145].
Challenges for research uptake in LMICs
The challenges of research uptake for policymaking are presented thematically. Eight main themes emerged: understanding context, stakeholder engagement and partnership, building trust and ownership, research capacity, resource constraints and misuse of resources, platform for evidence production and translation, investment in research infrastructure development, and research uptake framework and accountability (Fig. 2). Thematic narrative synthesis was performed based on the key findings.
Understanding context
We found over 30 papers on the importance of understanding the research uptake context [49, 60, 71, 76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100, 102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122, 124, 145]. This included understanding of the political dimension and interest [3, 38, 49, 74, 75, 80, 84, 87, 91, 96, 97, 101, 106, 107, 117, 125,126,127,128,129,130,131,132,133, 135,136,137,138], political will [49, 60, 71, 115, 120, 139, 140] and political commitment [77, 92, 112,113,114, 117, 130, 138, 140,141,142,143,144, 146, 147], leadership [78, 85, 105, 139, 143,144,145, 148,149,150], and health policy research priority setting [38, 77,78,79, 83, 85, 88, 92, 106, 114, 115, 117, 138, 142, 146, 147, 151,152,153,154,155,156,157,158]. Poor understanding of the complexity of the health policymaking process, including the social and political environment [60, 71, 89, 91,92,93,94,95,96,97], has limited the opportunity for translation of evidence to policy. Recognizing the domains (process, content and outcome) of health policymaking is important so that useable evidence to inform policies and practices in local context is generated [79, 90, 98,99,100, 102, 103]. Understanding the actual context in terms of political environment will enable actual use of evidence [78, 84, 85, 108, 145], encourage institutional budgetary allocations for research [81, 86], research and policy priority setting [78, 84, 87], and support scale up for societal benefit [79, 80, 82,83,84, 88, 93, 104,105,106,107,108,109, 112]. Conversely, lack of credible context-specific health evidence [83, 94, 110, 111], weak local evidence, misunderstanding of decision-makers, lack of consideration of sociocultural or religious practices [60, 71, 113,114,115,116,117], weak involvement of advocacy coalitions, and evidence generators [118] have limited research uptake for health policymaking. Additionally, translation of evidence to policy needs mutual trust [49, 92, 119]. Lack of application of a holistic approach to evidence-based practice [113], lack of historical context [104, 120], and lack of alignment to dynamic political interests [121, 122, 124] are important contextual barriers to research uptake in LMICs. Three areas emerged from the broader theme of understanding the context of research uptake. These are political dimension, priority setting and leadership, and they are presented below.
Political dimension: Mapping the political dimensions and policy demand [3, 38, 49, 74, 75, 80, 84, 87, 91, 96, 97, 101, 106, 107, 117, 125,126,127,128,129,130,131,132,133, 135,136,137,138], understanding of political will and commitment [49, 60, 71, 77, 92, 112,113,114,115, 117, 120, 130, 138,139,140,141,142,143,144, 146, 147], policy interest of decisionmakers’ [38, 97, 107, 128, 130], and key policy and governance features [49, 80, 91, 131] are key drivers in evidence-informed health policymaking and implementation in LMICs. An in-depth understanding of the role of politics, how societies organize themselves in achieving collective health goals, and how different stakeholders interact in the health policymaking process [3, 74, 75, 96, 127, 128, 132, 133, 135,136,137] is critical in evidence translation planning. The action of policymakers may be influenced by external factors [38, 84, 97, 106, 107, 117, 128, 138] including the nature of policymaking [101], lack of political will [49, 60, 71, 115, 120, 139, 140], weak engagement of politicians [78, 143,144,145], and poor social service infrastructures [92, 113, 114, 140, 146, 147]. Similarly, political barriers [112], bureaucratic budget management [130], difficulty in convincing policymakers, and stakeholders [77], leadership and unclear policy direction [85, 105], all affected use of evidence. National stakeholders' perceptions, political will supporting the use of research evidence in decision-making [148], and not paying attention to structural, institutional and political condition [139, 149, 150] are critical barriers to health research use for policymaking in LMICs.
Priority setting: Priority setting [5, 15, 17, 22, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156] has been reported to have important impacts on research uptake for policymaking and practice improvement [77, 78, 83, 106, 142, 147, 151, 152, 156] and needs the involvement of key experts [106, 142, 147, 153], and policymakers [77, 78, 115, 152,153,154, 156] to anticipate organisational need for policymaking [83, 88, 151, 152, 156], and create a shared data administration system [38, 106]. Prioritized evidence that is aligned to ideas and actions of political priority [114, 117, 146] must be made readily available [88, 153]. Nevertheless, lack of clarity on the evidence required by policymakers in the health sector [85, 115], scarcity of dedicated units that collate research needs [85, 158] and contradiction around the scope of data needed for policymaking [79, 155] are critical barriers to health evidence translation to policy and practice in LMICs. Personal, institutional, local/national, and global priorities may compete and drive evidence translation either positively or negatively [58, 90, 115]. Stakeholders having competing priority on health research have limited efforts to address the complex health evidence translation process [78, 114, 131, 147, 159]. Policymakers' urgent needs for research evidence about health systems in LMICs have also been affected by personal financial interests, and groups competing for authority [131].
Leadership: Willingness and/or commitment of political leaders influence health research translation in LMICs [46, 57, 60, 71, 77,78,79, 81, 85, 87, 105, 109, 110, 117, 121, 128, 139, 143,144,145, 148,149,150,151, 154, 160, 163]. Evidence-informed health policymaking relies on good leadership [92, 138, 155, 157], leaders’ willingness and commitment [46, 77, 87, 139, 151, 154, 163], decision-makers’ shared vision [57] and involvement [60, 71]. Lack of supportive, integrated and participatory leadership for research [57, 79, 81], poor political leadership with low performance [110, 121], and poor research governance [88, 139] are some of the critical leadership related challenges. Identifying and fostering public health leaders [109] will help to reduce the bureaucratic and protracted nature of policymaking and practice [128, 160]. Lack of understanding of contextual factors among key players and the powers of stakeholders [41, 42, 49, 125] was identified as important challenges to using evidence for health policymaking.
Stakeholder engagement and partnership
Engagement of key stakeholders is a crucial strategy in translation of evidence to policy [10, 38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56, 75,76,77, 79,80,81,82, 84,85,86, 88, 90,91,92,93,94,95,96,97, 99,100,101, 105, 106, 108,109,110, 112, 114, 115, 117, 119,120,121,122,123, 129, 131,132,133, 136,137,138,139,140,141, 148,149,150,151,152,153,154, 156, 157, 159,160,161,162,163,164,165,166]. Lack of local stakeholder engagement is a major barrier to co-production of evidence to shape policy [40, 75, 82, 94, 109, 110, 121, 129, 131, 138, 140, 141, 149, 153, 159,160,161,162]. Translating research into policy and practice requires the intersectoral collaborative efforts of key stakeholders in LMICs [41, 54, 82, 85, 88, 112, 114, 120, 138, 149, 163]. The active engagement of funders, community organization, implementers and other stakeholders can be used to address the complex bureaucracy environment in LMICs [75, 76, 79, 82, 86, 90, 91, 109, 110, 115, 129, 132, 137, 151, 154, 160,161,162,163,164,165]. These stakeholders should be involved from the inception of project and throughout the research process. Such involvement takes into account local needs, encourages interactions, strengthens relationships, creates mutual accountability and promotes uptake of the evidence for policymaking [76, 77, 81, 85, 101, 105, 152, 163]. Likewise, evidence uptake for health policymaking needs strong public–private partnership [66, 99, 118, 123, 163], and advocacy for domestic funding, resource mobilization and collaboration [99, 163]. Stakeholder engagement is important to mitigate unmet needs [39, 91, 94, 101, 108, 122, 141, 149, 150, 166], build trust in the evidence [38, 108], and avoid duplication of efforts [38, 120, 139]. Some policymakers may not be willing to use research evidence [165]. Polarized stakeholders’ interests [117], low level of interaction between producers and users of research [43,44,45, 132, 141, 148], slow response to stakeholders’ requests for feedback [49, 131], and low sense of ownership [95, 106, 115, 163] led to poor research uptake for health policymaking. Relatively lower engagement of social scientists, and economists in the health research team [121, 159], and limited engagement of the media [97, 157] were also highlighted as important barriers. Poor inter-sectoral collaboration [51,52,53, 129, 133, 141] among public health researchers and political scientists working in international development has remained a challenge to evidence uptake.
Building trust and ownership
Concerns about the quality of evidence have limited research uptake for policymaking [10, 12, 43, 56, 58, 59, 62, 66,67,68, 74,75,76,77, 81, 84, 85, 92, 94, 97, 104, 105, 108, 109, 111, 112, 116, 117, 121, 123, 127, 128, 131, 139,140,141, 143,144,145, 148, 153, 156,157,158]. Lack of access to good quality, timely, and relevant research outputs is a barrier to evidence uptake [10, 43, 56, 66, 67, 76, 112, 141, 156]. Lack of research literacy [56, 105], poor perceived data quality [59, 105, 156], and unavailable or inaccessible research findings [92, 156] have detrimentally influenced health evidence to policy translation in LMICs. Evidence use is limited by organizational issues, lack of robust research skills, and innovative research designs [59, 67, 97, 109, 142, 153]. Lack of locally-relevant contextual research production [12, 59, 74, 77, 116, 117, 127, 128, 140, 143, 144, 158], poor presentation of research findings [158], lack of concrete evidence on cost-effectiveness of policies [56, 139], weak institutional capacity [117, 121, 145], and low stakeholder consultation [131] cause public distrust. In addition, the beliefs and power of diverse actors [68], perceptions around the quality of existing evidence [58, 75, 77], the resistant culture of evidence users’ [58, 62, 85, 111, 123, 156], low motivation of researchers [81, 97, 104], and lack of clarity [158] are barriers to research uptake. Likewise, weak support for science-based health innovation [93], absence of effective coordination, governance and supervision [62, 105, 121, 128], inadequate integration of research into translation [105, 109, 113], expert overload, and a weak health system [63, 121] are major barriers to evidence uptake.
Research capacity
Limited research capacity is a major challenge to research uptake for policymaking in LMICs [40, 41, 43, 49, 51, 54,55,56, 58,59,60,61,62,63, 66, 67, 71, 76, 77, 81, 83,84,85,86,87,88, 90,91,92, 97, 98, 101, 104, 105, 109,110,111,112,113, 115,116,117,118,119,120,121, 123, 130, 131, 134,135,136,137,138,139,140, 145,146,147, 150,151,152, 154, 155, 157, 160, 162,163,164,165]. Lack of technical competence among evidence producers and users [41, 59, 60, 71, 101, 109, 115, 121, 145, 146, 151] and lack of organizational capacity [40, 43, 47, 90, 104, 105, 117, 121, 131, 155] and inadequate infrastructure [60, 71] have significant impacts on research uptake. Untrained human resources [61, 62, 113], low research capacity to produce and use of evidence [85, 91], and limited researchers’ knowledge about research funding [81, 92, 116, 139], have all influenced health evidence to policy translation. Extensive capacity building, at the individual and organisational level [55, 60, 66, 71, 84, 85, 87, 92, 111, 118, 119, 130, 131, 150, 154, 157, 160, 164], for skilled human resource for research development [54, 55, 105, 112, 113, 120, 139, 152, 157] through in-service training [85, 86, 90, 112, 113, 146] is urgently required to improve use of research evidence. Funders need strong technical skills from researchers and integrated evidence translation [41, 110, 155]. Low levels of research understanding among evidence users have weakened research uptake for policymaking in LMICs [125, 146, 155, 157, 165].
The lack of skill that researchers have in research and translation [49, 51, 63, 66, 77, 97, 105, 134, 146], and similar skills gaps among evidence users [51, 56, 58, 62, 67, 76, 85, 98, 104, 109, 123, 146, 157], both impact research uptake in LMICs. In addition, staff shortages, high turnover [51, 60, 62, 71, 83, 91, 109], poor coordination and management, inadequate pre-service training, and insufficient specialist capacity pose challenges in translating evidence to policy. Health research uptake for policymaking and practice has suffered from low awareness, and misconceptions among evidence users [60, 62, 71, 101, 104, 112, 113, 121, 138, 139, 147]. Moreover, weak research supervision [55, 62], lack of evidence-based mentorship on new interventions [62, 81, 105, 111], and inadequate peer support in the healthcare [60, 71, 81] negatively influence evidence production and local implementation.
Resource constraints and misuse of resources
Resource constraints are a major barrier to uptake of research for policy and practice in LMICs. [40, 46, 47, 55, 60, 61, 69,70,71, 79, 81, 83,84,85, 87, 90, 91, 97, 101, 105, 111,112,113, 115, 120,121,122, 130, 131, 138, 139, 142, 156, 158, 159, 165]. Unreliable infrastructure [111, 112, 120, 139], scarce resources and increasing numbers of patients [47, 61, 79, 101, 111,112,113, 120], are identified barriers to research uptake. Inadequate long-term funding for research infrastructure [79, 81, 83, 84, 91, 97, 113, 115, 121, 139, 158] and lack of local research funds [47, 69, 70, 85, 113, 115, 122, 165] are major factors affecting evidence to policy translation. Budget process bureaucracy [105, 121], corruption [105], and limited transparency [121] also influence translation efforts. Rigidity in executing research budgets [69, 91, 130, 142, 165], and use of legal proceedings [130] have also worsened evidence uptake support in LMICs.
Platforms for evidence production and translation
Research uptake for health policy and practice requires an enabling platform for research priority setting and dissemination of findings [38, 49, 54,55,56,57, 60,61,62, 64, 66, 71, 77, 78, 80, 81, 84, 85, 87, 88, 90, 93,94,95, 105, 107, 109, 112,113,114,115, 117, 124, 128, 139, 145, 146, 148, 151, 153, 154, 156, 163], capacity strengthening and research leadership [38, 77, 85, 128]. A strong platform will facilitate engagement so that policy-makers can outline their priorities and expectations from researchers [55, 64, 77, 87, 90, 109, 154], conceptualize health research findings [80, 87, 95, 154], enhance dissemination findings [38, 80, 90, 153], networking [146], coordination [64, 85] and research utilization [66, 76, 84]. A major gap has existed in the dissemination and implementation of research findings for policy [66, 85, 90, 105, 107], in access to evidence [61, 85, 119, 128, 145, 146, 151], domestic knowledge exchange [49, 84, 113], interaction between stakeholders [66, 84, 94, 112, 113] and generating demand for evidence [139]. Inadequate health policy research infrastructure [60, 71, 78, 81, 85, 105, 109, 163], fragmentation of health information systems [95, 153, 156, 163], absence of robust institutional platforms [56, 85, 88, 114], poor access to health data [163], and lack of cost-effective technologies for health information [77, 105, 114, 117] negatively affect evidence to policy translation in LMICs. In addition, a platform for effective communication of research findings [49, 56, 66, 67, 76, 78, 82, 84, 85, 87, 97, 105, 109, 121, 128, 139, 141, 146, 150,151,152,153, 158, 160] allows policymakers to share their knowledge and experiences [78, 87, 152], and engage stakeholders [49, 139, 150, 151, 158, 160], and facilitate better packaging of key findings using plain and easy language [56, 82, 97, 146, 153] for active diffusion of innovation [109]. Limited availability of local data of the desired quality [56], researchers’ having communication and dissemination skills gaps [66, 67, 105], [49, 56, 97], poor engagement of stakeholders [66, 76, 85, 121, 128, 153], and low media use [153] are common communication barriers in LMICs.
Investment in research infrastructure development
Research infrastructure development [43,44,45,46, 60,61,62, 64, 67, 71, 74, 77,78,79, 81, 84, 86, 88, 90, 97, 101, 105, 108, 112, 113, 119, 121, 128, 129, 149, 151, 154, 155, 157, 163, 164], including financial support to acquire essential evidence [78, 90, 105], mobilize resources for research capacity building [77, 79, 101, 112, 113, 154, 155, 164], and cooperate with national and international institutions [113] is crucial to improve research uptake. Lack of basic infrastructure for research [79, 81] and healthcare [60, 62, 64, 71, 121], widespread perceptions of unfriendly organizational environment [60, 62, 71], and structural and technical constraints between institutions [46, 61, 67, 155, 163] have negatively influenced research uptake for policy. The fact that a large proportion of health research depends on the priority setting of donors [49, 55, 59, 64, 69, 70, 77, 78, 81, 83, 85, 91,92,93, 97, 109, 110, 115, 117, 130, 139, 140, 142, 146, 147, 154], may not allow the uptake of evidence [78, 83, 91, 139], that might affect national health priorities. Donor research support ranged from 47 to 94% of research investment in LMICs [83]. Even though increased funding for research [81] and long-term funding for better success [55] are desired, limited time [154] affects the quality of evidence produced and its translation to policy. Donor investment in health research has fallen below that required [142, 146], and funding sustainability concerns [64, 69, 77, 92, 110, 140] will compromise research uptake for policy in LMICs.
Evidence uptake framework and accountability
Developing a testable evidence uptake framework [38, 43, 44, 52, 62, 68, 75, 80, 82, 95, 96, 100, 102, 106, 122, 128, 136, 163] that allows in-depth integration of the fragmented body of knowledge [38, 44, 51, 62, 68, 75, 96, 100, 102, 136] will help to guide evidence uptake. System mapping to understand users’ perspectives, consult stakeholders, secure different funding streams, and design clear governance structures, leadership and staffing [82, 100] is a crucial component of effective evidence uptake. Poor information-based planning and decision-making, weak monitoring and lack of accountability and transparency [51, 62] are also barriers to effective research uptake. In addition, addressing bottle necks related to legal frameworks, policy, and system responses are critical to guide evidence use for policy [40, 51, 60, 62, 63, 66, 71, 72, 76, 78, 85, 86, 101, 108, 110,111,112,113, 128, 131, 139]. Enforcement and accountability of researchers and users [60, 66, 71, 76, 85, 88, 97, 108, 111, 112, 128, 131, 139] is not in place due to weak governance and regulation [60, 71, 86, 111, 113]. Though there are policy and institutional efforts to promote knowledge translation [97, 151, 155], other institutions in the health system can block these efforts, as can financial and organization pitfalls [60, 71, 90, 155], and weak national policy in the LMICs [45, 74, 84, 88, 155].
Recommendations to strengthen research uptake in LMICs
We have identified several pieces of evidence that forward key recommendations [41, 49, 54,55,56, 62,63,64,65,66,67, 73, 76,77,78, 81, 85, 87, 88, 90, 91, 93, 97, 104,105,106, 108, 110, 111, 113,114,115, 119,120,121, 128, 131, 134, 146, 148, 149, 151,152,153,154,155, 158, 160]. We have summarized these recommendations into six key areas of action: recognize the real context, establish evidence to policy platforms, collaborate with and engage stakeholders, increase advocacy and ownership, invest in research, and build endogenous capacity.
Evidence-to-policy platform: Establishing knowledge translation platforms [64, 65, 77, 85, 108, 148, 151], strengthening existing platform [54, 81], and developing health research literacy programs [49, 56, 85, 97, 119, 128, 155] are crucial to enhancing the quality of evidence production and use. Strengthening institutional platforms [43, 44, 86, 88, 119, 128, 129, 157], and integrated research capacity building [64, 67, 81, 84, 108, 149] are required to improve research uptake for policy in LMICs.
Recognize context: Understanding political dimension and contexts [62, 63, 105, 106, 110, 121, 128, 134, 153, 160] and disseminating research findings to ensure accessibility and availability of evidence to users [56, 66, 67, 85, 112, 131] play crucial roles in improving research uptake for policymaking. Sustainable advocacy for coalition, prioritization of key players [125], addressing stakeholders’ concerns [126], and identifying opportunities and mitigating constraints [127] are also fundamental to evidence-informed health policymaking and implementation in LMICs. Balancing personal, local, institutional, and global concerns and priorities tends to lead to a sense of ownership and responsibility concerning research findings [150].
Collaboration and stakeholders engagements: Engagement of stakeholders is a critical step in establishing strong multisectoral collaborations and partnerships and has a key role in improving evidence uptake for policymaking [10, 48, 50, 77, 96, 99, 100, 129, 133, 136, 137, 161, 162]. Strong networking and collaboration between stakeholders [49, 56, 85, 92, 93, 101, 112], forging alliances to raise capital and investment [41, 105, 121, 149, 153], strengthening partnerships [55, 94, 117, 122], increasing community participation [95, 122, 123, 138, 157], and enhancing health innovation in LMICs [119] are robust approaches to professional transformation [85, 101], and create opportunities for transparency and communication [131, 154, 164]. Strengthening partnerships and engaging stakeholders has key role in promoting use of research findings [41, 55, 62, 73, 76, 81, 85, 90, 105, 106, 111, 113,114,115, 131, 146, 151, 154, 158].
Advocacy and ownership: Building a sense of ownership through co-production of evidence [56,57,58,59, 61,62,63, 84, 93, 96, 105, 106, 109, 110, 113, 115, 121, 128, 131, 148, 150, 151, 154, 155, 157,158,159, 164], and spanning research and policy communities [155] are essential for producing high-quality contextual evidence. Designing research translation frameworks [113, 152], global health diplomacy [111, 120] and deliberate dialogue or diplomacy efforts to mainstream research uptake for policy [76, 85, 87, 91, 120] may also make significant contribution. Similarly, research uptake advisory groups at institutional level [49, 76, 87] will facilitate in-person discussions between researchers and policymakers [42, 43, 49, 56, 61, 77, 92, 97, 124, 128, 162, 163], strengthen implementation of research uptake [85, 124, 159], and help co-production research uptake agendas [49, 56, 61, 92, 155], make better use of media, and increase links to government [42, 76, 104, 110, 120, 130].
Invest in research: Investments in research infrastructure to strengthen and sustain institutional research capacity [78, 91, 93, 104, 155, 158] will contribute to quality evidence generation and use in LMICs. Efficient use of scarce resources [112], mobilizing domestic funding [40, 91, 130], domestic and international resource mobilization [109, 130, 142], supporting good quality research [85, 87, 138], physical and economic infrastructure at research institutions [122], are suggested to improve evidence translation in LMICs. Co-investment with national and international funding [93] and engaging donors and policymakers in research priority setting and implementation [49, 85, 115, 117, 147] may minimize funders’ influence and achieve mutual interests. In addition, establishing a research uptake advisory board [42, 49, 56, 76, 83,84,85, 87, 88, 104, 108, 110, 112, 120, 122, 124, 130, 153, 155, 159, 160, 163] is important for strengthening advocacy [42, 76, 83,84,85, 104, 108, 110, 120, 122, 130], stakeholder engagement [108], and understanding of the local context [84]. Establishing multidisciplinary research networks [110, 157], cross-learning for researchers [56, 128, 158], and integrated knowledge translation to advance engagement [157] are important strategies to increase research uptake for policymaking.
Endogenous capacity building: establishing a contextual model for capacity development will help to drive evidence uptake for policymaking [40, 43, 115, 135,136,137, 146, 154, 162, 163]. Research and translation mentorship [55, 60, 62, 64, 65, 71, 81, 83, 105, 111, 152, 164] and supportive supervision [64, 65, 83] play key roles in identifying potential evidence for policy. Making good quality data readily available in a digestible format [59, 76, 84, 108, 148, 157] is recommended to improve research uptake in LMICs.
Discussion
Considerable amount of evidence relevant to translation of evidence into policymaking in LMICs was identified. We found that the common barriers to research uptake are lack of understanding political dimension, low government priority, poor engagement of stakeholders, low investment in research, capacity and resource constraints, lack of ownership and trust in domestic research products, lack of a guiding research uptake framework, and lack of platform to bridge the research uptake gap in LMICs. Mapping to identify the most common forms of research use involves the direct application of research to policymaking and practice [166], and prior agenda-setting [20]. The barriers identified are consistent with the evidence, policy, and impact guiding framework of the WHO [14]. To optimize uptake of evidence in health policymaking, researchers should recognize policymakers’ priorities and prepare to engage them in long-term strategies, get their buy-ins, persuade them to act and secure a hierarchy of evidence underpinning policy [39, 167]. However, published evidence on health policy processes in LMICs is scarce, diverse, and fragmented.
We have identified common barriers limiting research uptake for health policymaking in low resource setting. Enhancing capacity for evidence-informed policy improves priority setting, filtration and amplification of evidence for policy-making and practice [20]. Institutional structures need to be improved [37, 168] through political will [169], multi-stakeholder partnership [37, 169], financial and human resources [37, 169], and evidence-based normative guidance [169]. International actors, development thinking, global partnership and networking are playing a tremendous role in research and policy. However, lack of empirical research and weak monitoring, evaluation and learning limits the impact of shaping policy with evidence in LMICs [23]. Deepening and extending health policy analysis work in LMICs requires greater levels of funding to support capacity development efforts and to generate systematic, coherent and rigorous evidence to underpin policy change [37, 170].
We identified key recommendations to improve research uptake for health policymaking in LMICs. Establishing evidence translation platforms, improving health policy research literacy and understanding the political dimension and context [171,172,173,174] are among the key recommendations to improve research uptake. Comprehensive evidence uptake approach is crucial [43, 52, 96, 128], including strong monitoring, evaluation and learning strategy of evidence to policy translation [80, 95, 102, 106, 122, 163], and evidence to policy intervention audit [62]. Likewise, engaging stakeholders from inception and /or pre-implementation [175] to dissemination is essential to understand the context of research uptake for health policymaking and practice in LMICs [38, 47, 49, 76, 80, 84, 114, 117, 121, 123, 149, 153, 160]. Establishing partnerships with global health funding organizations should prioritize the support of academic institutions’ capacity building initiatives, rigorous research, design dissemination strategies and establishing knowledge translation pathways [176].
Research uptake for health policymaking requires strategies to contextualize and balance global and local health research findings, to understand the complexity of producing high-quality research [177] and to appreciate the key role of stakeholders [177, 178] in the evidence to policymaking process [177]. Evidence producers, knowledge brokers, and end users of evidence are key actors at each phase of the research uptake process [179]. Development of context-oriented platform with the potential to facilitate research uptake for health policy making will need strong management networks and sustainable funding [37, 180]. Understanding of context [181, 182] and challenges is key to improving uptake of research for health policymaking [183]. Evidence uptake require a supportive process and mutual trust between practitioners and policy makers, and an incentive system in line with organizational vision and mission [184]. The active participation of community members and local leaders is crucial in giving opportunities to reflect their needs and interests, and to allow them to negotiate with the researcher on implementation of the study in their surroundings [173].
Stakeholder involvement will improve policy-maker confidence [58, 66], result in greater trust of local partners [94], and enhance patient and public participation [172]. An evidence to policy platform [185] for capacity strengthening [173, 186] of both evidence producers and users in implementation science will have a significant impact on research uptake [187]. Evidence to policy platform [185] play key roles in identifying effective communication strategies [188]. Systems approaches will make crucial contribution in improving efforts of translation of evidence to policy in LMICs [23, 189].
This scoping review has mainly focused on the translation of research evidence into policy. Evidence-informed practice was considered to be a manifestation of uptake; however, the evidence-to-policymaking process is far greater than evidence-informed practice or implementation.
Implications of the findings
This scoping review identified challenges to evidence uptake and possible strategies through which this might be strengthened. A range of studies were identified, including primary studies, trials, and syntheses. Mapping the availability of quality evidence and recognizing challenges to evidence translation will enhance policymaking and practice. Dedicated centers or platforms appear likely to facilitate evidence uptake in real settings. Stakeholders in the research production and translation ecosystem should use pragmatic approaches to assess the political context and priorities, enhance collaboration, invest in research infrastructure development and adapt contextual pathways for evidence uptake. These finding will guide the focus of a Unit for Health Evidence and Policy (UHEP) which is being established to serve as a platform for evidence translation in Ethiopia and beyond. Establishing a platform to bridge the gap between researchers and policy makers is crucial to utilize available evidence for health policymaking and practice.
Conclusion
We found substantial evidence on challenges to health research uptake for policymaking and practice in LMICs. Understanding of the national and international context and priorities, involving key stakeholders, resource and establishing a coordinating platform to facilitate capacity building, quality evidence production, communication and a framework for accountability are crucial to facilitate evidence uptake for policymaking. Barriers to poor evidence uptake for health policymaking have to be addressed through investing in research capacity building, partnership and stakeholder participation, co-mobilize resources, building trust and ownership on evidence production. This must be guided by a well-grounded theory of change framework to address barriers in LMICs. A platform for interaction and capacity building of key actors, including politicians, policy makers, academics, public health researchers and medical practitioners is essential to improve insight and establish a network for evidence sharing in LMICs.
Availability of data and materials
Data can be available upon formal request to the corresponding author.
Abbreviations
- CDT-Africa:
-
Centre for Innovative Drug Development & Therapeutic Trials for Africa
- LMICs:
-
Low- and middle-income countries
- RUTAG:
-
Research Uptake Advisory Group
- UHEP:
-
Unit for Health Evidence and Policy
- WHO:
-
World Health Organization
References
Ioannidis JPA. How to make more published research true. PLoS Med. 2014;11(10): e1001747.
Begley CG, Ioannidis JPA. Reproducibility in science: Improving the standard for basic and preclinical research. Circ Res. 2015;116(1):116–26.
WHO. Evidence synthesis for health policy and system: a method guide. Geneva, Switzerland; 2018.
Maurice K, Mary H, Steve H. Government and research: thirty years of evolution. Berlin: Springer Science & Business Media; 2006.
Rajabi F. Evidence-informed health policy making: the role of policy brief. Int J Prev Med. 2012;3(9):596–8.
Peirson L, Ciliska D, Dobbins M, Mowat D. Building capacity for evidence informed decision making in public health: a case study of organizational change. BMC Public Health. 2012;12(1):137.
House W. Policy analytical capacity and evidence-based policy-making: lessons from Canada. Br Med J (Clin Res Ed). 2009;52(2):153–75.
Yordanov Y, Dechartres A, Porcher R, Boutron I, Altman DG, Ravaud P. Avoidable waste of research related to inadequate methods in clinical trials. BMJ. 2015;350: h809.
Innvær S, Vist G, Trommald M, Oxman A. Health policy-makers’ perceptions of their use of evidence: a systematic review. J Heal Serv Res Policy. 2002;7(4):239–44.
Oliver K, Innvar S, Lorenc T, Woodman J, Thomas J. A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res. 2014;14:2.
Jewell CJ, Bero LA. “Developing good taste in evidence”: facilitators of and hindrances to evidence-informed health policymaking in state government. Milbank Q. 2008;86(2):177–208.
Brownson CR, Royer C, Ewing R, McBride TD. Researchers and policymakers: travelers in parallel universes. Am J Prev Med. 2006;30(2):164–72.
Uneke CJ, Ezeoha AE, Ndukwe CD, Oyibo PGOF. Promotion of evidence-informed health policymaking in Nigeria: bridging the gap between researchers and policymakers. Glob Public Heal An Int J Res Policy Pract. 2012;7(7):750.
WHO. Evidence, policy, impact. WHO guide for evidence-informed decision-making. Geneva: Wolrd Health Organization; 2021. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwi3mYa6r6D7AhVm_3MBHagiC1QQFnoECCsQAQ&url=https%3A%2F%2Fapps.who.int%2Firis%2Frest%2Fbitstreams%2F1405176%2Fretrieve&usg=AOvVaw19QEBvbAUc34SC5iuteGmI
Glasziou P, Altman DG, Bossuyt P, Boutron I, Clarke M, Julious S, et al. Reducing waste from incomplete or unusable reports of biomedical research. Lancet. 2014;383(9913):267–76. https://doi.org/10.1016/S0140-6736(13)62228-X.
Samuel S, König-Ries B. Understanding experiments and research practices for reproducibility: an exploratory study. PeerJ. 2021;9:1–26. https://doi.org/10.7717/peerj.11140.
Créquit P, Trinquart L, Yavchitz A, Ravaud P. Wasted research when systematic reviews fail to provide a complete and up-to-date evidence synthesis: the example of lung cancer. BMC Med. 2016;14:8. https://doi.org/10.1186/s12916-016-0555-0.
Orton L, Lloyd-Williams F, Taylor-Robinson D, O’Flaherty M, Capewell S. The use of research evidence in public health decision making processes: systematic review. PLoS ONE. 2011;6(7): e21704.
Trostle J, Bronfman M, Langer A. How do researchers influence decision-makers? Case studies of Mexican policies. Health Policy Plan. 1999;14(2):103–14.
Brooks C, Mirzoev T, Chowdhury D, Deuri SP, Madill A. Using evidence in mental health policy agenda-setting in low- and middle-income countries: a conceptual meta-framework from a scoping umbrella review. Health Policy Plan. 2023;30:876–93.
Gough D, Maidment C, Sharples J. UK what works centres: aims, methods and contexts. 2018. 1–156 p. https://eppi.ioe.ac.uk/cms/Default.aspx?tabid=3731
Hamalainen RM, Aro AR, de van Goor I, Lau CJ, Jakobsen MW, Chereches RM, et al. Exploring the use of research evidence in health-enhancing physical activity policies. Heal Res Policy Syst. 2015;13:43.
Franzen SRP, Chandler C, Lang T. Health research capacity development in low and middle income countries: reality or rhetoric? A systematic meta-narrative review of the qualitative literature. BMJ Open. 2017;7(1): e012332.
Strumińska-Kutra M, Scholl C. Taking power seriously: towards a power-sensitive approach for transdisciplinary action research. Futures. 2022;135(102881):1–9.
Masson JE, Soustre-Gacougnolle I, Perrin M, Schmitt C, Henaux M, Jaugey C, et al. Transdisciplinary participatory-action-research from questions to actionable knowledge for sustainable viticulture development. Humanit Soc Sci Commun. 2021;8(1):1–9.
Medina-García C, Nagarajan S, Van den Broeck P. The Leuven Gymkhana: transdisciplinary action research questioning socially innovative multi-actor collaborations in COVID times. Front Sustain Food Syst. 2022;6: 746974.
Loeb SJ, Penrod J, Kolanowski A, Hupcey JE, Haidet KK, Fick DM, McGonigle D, Yu F. Creating cross-disciplinary research alliances to advance nursing science. J Nurs Scholarsh. 2008;40(2):195–201. https://doi.org/10.1111/j.1547-5069.2008.00226.x.
Stokols D. Toward a science of transdisciplinary action research. Am J Community Psychol. 2006;38(Issue1-2):79–93. https://doi.org/10.1007/s10464-006-9060-5.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Tricco A, Zarin LE, O’Brien K, Colquhoun H, Levac D. Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) checklist. Ann Intern Med. 2018;169:467–73.
WHO. Health policy and systems research issues: Current trends and key lessons on how to improve the use of evidence in health policy. Global Public Health Policy. 2021. p. 379–87.
Westphaln KK, Regoeczi W, Masotya M, Vazquez-Westphaln B, Lounsbury K, McDavid L, et al. From Arksey and O’Malley and beyond: customizations to enhance a team-based, mixed approach to scoping review methodology. MethodsX. 2021;8: 101375. https://doi.org/10.1016/j.mex.2021.101375.
Rutgers. RUTGERS the state University of New Jersey. George F. Smith Library of the Health Sciences. EndNoteX8.0.1(BId 10444), Cite While You Write TM Patented technology U.S patent number 8,092,241. University of Ghana: 3091850168. 2017. http://www.libraries.rutgers.edu/sites/default/files/smith/pdf/EndNoteBasic.pdf
Fantom N, Serajuddin U. The World Bank’s Classification of Countries by Income. World Bank Group. Policy Research Working paper 7528. 2016.
Wang Q, Zhu Y, Li Y, Chu X, Li R, Hou L, et al. Facilitators, barriers and strategies for health-system guidance implementation: a critical interpretive synthesis protocol. Heal Res Policy Syst. 2022;20(1):105. https://doi.org/10.1186/s12961-022-00899-y.pdf.
Chiu TY, Yu HW, Goto R, Lai WL, Li HC, Tsai ET, et al. From fragmentation toward integration: a preliminary study of a new long-term care policy in a fast-aging country. BMC Geriatr. 2019;19(1):159. https://doi.org/10.1186/s12877-019-1172-5.pdf.
Cairney P, Oliver K. Evidence-based policymaking is not like evidence-based medicine, so how far should you go to bridge the divide between evidence and policy? Heal Res Policy Syst. 2017;15(35):1–11.
Orgill M, Nxumalo N, Amde W, Erasmus E, Lehmann U, Goudgeii J, et al. Health policy and systems research: needs, challenges and opportunities in South Africa – a university perspective. Public Heal An action Guid to Improv Heal. 2012;2012:151–60.
Badu E, O’Brien AP, Mitchell R, Osei A. A qualitative study of evidence-based therapeutic process in mental health services in Ghana- context-mechanisms-outcomes. BMC Heal Serv Res. 2021;21(1):1–15.
Mubyazi GM, Gonzalez-Block MA. Research influence on antimalarial drug policy change in Tanzania: case study of replacing chloroquine with sulfadoxine-pyrimethamine as the first-line drug. Malar J. 2005;4:51. https://doi.org/10.1186/1475-2875-4-51.pdf.
Yearwood AC. Applying a logical theory of change for strengthening research uptake in policy: a case study of the evidence informed decision making network of the Caribbean. Rev Panam Salud Publica/Pan Am J Public Heal. 2018;42:1–9.
Armstrong R, Waters E, Dobbins M, Anderson L, Moore L, Petticrew M, et al. Knowledge translation strategies to improve the use of evidence in public health decision making in local government: intervention design and implementation plan. Implement Sci. 2013;8(1):121.
Campbell DM, Redman S, Jorm L, Cooke M, Zwi AB, Rychetnik L. Increasing the use of evidence in health policy: Practice and views of policy makers and researchers. Aust New Zealand Health Policy. 2009;6(1):1–11.
Gyamfi J, Allegrante JP, Iwelunmor J, Williams O, Plange-Rhule J, Blackstone S, et al. Application of the consolidated framework for implementation research to examine nurses’ perception of the task shifting strategy for hypertension control trial in Ghana. BMC Heal Serv Res. 2020;20(1):1–11.
Lavis JN, Moynihan R, Oxman AD, Paulsen EJ. Evidence-informed health policy 4 - case descriptions of organizations that support the use of research evidence. Implement Sci. 2008;3:56. https://doi.org/10.1186/1748-5908-3-56.pdf.
Bennett S, Corluka A, Doherty J, Tangcharoensathien V, Patcharanarumol W, Jesani A, et al. Influencing policy change: The experience of health think tanks in low- and middle-income countries. Health Policy Plan. 2012;27(3):194–203.
Uzochukwu B, Mbachu C, Onwujekwe O, Okwuosa C, Etiaba E, Nyström ME, et al. Health policy and systems research and analysis in Nigeria: examining health policymakers’ and researchers’ capacity assets, needs and perspectives in south-east Nigeria. Asia Pac J Clin Oncol. 2016;14:13. https://doi.org/10.1186/s12961-016-0083-6.pdf.
Fekadu A, Oppenheim C, Manyazewal T, Nislow C, Woldeamanuel Y, Hailu A, et al. Understanding the key processes of excellence as a prerequisite to establishing academic centres of excellence in Africa. BMC Med Educ. 2021;21(1):1–10.
Petersen I, Marais D, Abdulmalik J, Ahuja S, Alem A, Chisholm D, et al. Strengthening mental health system governance in six low- and middle-income countries in Africa and South Asia: challenges, needs and potential strategies. Health Policy Plan. 2017;32(5):699–709.
Sumner A, Crichton J, Theobald S, Zulu E, Parkhurst J. What shapes research impact on policy? Understanding research uptake in sexual and reproductive health policy processes in resource poor contexts. Heal Res Policy Syst. 2011;9(Suppl 1):S3.
Bennett S, Glandon D, Rasanathan K. Governing multisectoral action for health in low-income and middleincome countries: unpacking the problem and rising to the challenge. BMJ Glob Heal. 2018;3:1–8.
Shidhaye R, Lund C, Chisholm D. Closing the treatment gap for mental, neurological and substance use disorders by strengthening existing health care platforms: strategies for delivery and integration of evidence-based interventions. Int J Ment Heal Syst. 2015;9:40. https://doi.org/10.1186/s13033-015-0031-9.pdf.
Ali MM, Haskins L, John V, Hatløy A, Luthuli S, Mapumulo S, et al. Establishing a postgraduate programme in nutritional epidemiology to strengthen resource capacity, academic leadership and research in the democratic republic of Congo. BMC Med Educ. 2021;21(1):136. https://doi.org/10.1186/s12909-021-02557-3.pdf.
Yamey G, Horváth H, Schmidt L, Myers J, Brindis CD. Reducing the global burden of Preterm Birth through knowledge transfer and exchange: a research agenda for engaging effectively with policymakers. Reprod Heal. 2016;13:26. https://doi.org/10.1186/s12978-016-0146-8.pdf.
Poursheikhali A, Alkhaldi M, Dehnavieh R, Haghdoost A, Masoud A, Noorihekmat S, et al. Identifying challenges and recommendations for advancing global mental health implementation research: a key informant study of the National Institute of Mental Health Scale-Up Hubs. Heal Res Policy Syst. 2021;57: 102557. https://doi.org/10.1186/s12961-022-00905-3.pdf.
Mijumbi RM, Oxman AD, Panisset U, Sewankambo NK. Feasibility of a rapid response mechanism to meet policymakers’ urgent needs for research evidence about health systems in a low income country: a case study. Implement Sci. 2014;9:114. https://doi.org/10.1186/s13012-014-0114-z.pdf.
Kumar MB, Taegtmeyer M, Madan J, Ndima S, Chikaphupha K, Kea A, et al. How do decision-makers use evidence in community health policy and financing decisions? A qualitative study and conceptual framework in four African countries. Heal Policy Plan. 2020;35(7):799–809.
Baatiema L, Otim ME, Mnatzaganian G, de-Graft Aikins A, Coombes J, Somerset S. Health professionals’ views on the barriers and enablers to evidence-based practice for acute stroke care: a systematic review. Implement Sci. 2017;12(1):1–15.
Price JA, Guinness L, Irava W, Khan I, Asante A, Wiseman V. How to do (or not to do) … translation of national health accounts data to evidence for policy making in a low resourced setting. Heal Policy Plan. 2016;31(4):472–81.
Biza A, Jille-Traas I, Colomar M, Belizan M, Requejo Harris J, Crahay B, et al. Challenges and opportunities for implementing evidence-based antenatal care in Mozambique: a qualitative study. BMC Pregnancy Childbirth. 2015;15(1):200.
Cooper D, Mantell JE, Moodley J, Mall S. The HIV epidemic and sexual and reproductive health policy integration: views of South African policymakers. BMC Public Health. 2015;15:217. https://doi.org/10.1186/s12889-015-1577-9.pdf.
Hedt-Gauthier BL, Chilengi R, Jackson E, Michel C, Napua M, Odhiambo J, et al. Research capacity building integrated into PHIT projects: leveraging research and research funding to build national capacity. BMC Heal Serv Res. 2017;17(Suppl 3):825. https://doi.org/10.1186/s12913-017-2657-6.pdf.
Feyissa YM, Hanlon C, Emyu S, Cornick RV, Fairall L, Gebremichael D, et al. Using a mentorship model to localise the Practical Approach to Care Kit (PACK): from South Africa to Ethiopia. Sex Reprod Heal Matters. 2018;3(Suppl 5): e001108.
Guleid FH, Njeru A, Kiptim J, Kamuya DM, Okiro E, Tsofa B. Experience of Kenyan researchers and policy-makers with knowledge translation during COVID-19: a qualitative interview study. BMJ Open. 2022;12(6): e059501.
Paci M, Faedda G, Ugolini A, Pellicciari L. Barriers to evidence-based practice implementation in physiotherapy: a systematic review and meta-analysis. Int J Qual Heal Care. 2021;33(2):1–13.
Walt G, Shiffman J, Schneider H, Murray SF, Brugha R, Gilson L. “Doing” health policy analysis: methodological and conceptual reflections and challenges. Health Policy Plan. 2008;23(5):308–17.
Zhou W, Yu Y, Yang M, Chen L, Xiao S. Policy development and challenges of global mental health: a systematic review of published studies of national-level mental health policies. BMC Psychiatry. 2018;18(1):1–9.
UN. Strengthening Policy Research Uptake in the Context of the 2030 Agenda for Sustainable Development. Geneva: United Nations; 2018. p. 1–82.
Baatiema L, de-Graft Aikins A, Sav A, Mnatzaganian G, Chan CKY, Somerset S. Barriers to evidence-based acute stroke care in Ghana: a qualitative study on the perspectives of stroke care professionals. BMJ Open. 2017;7(4): e015385.
Jenkins R, Mussa M, Haji SA, Haji MS, Salim A, Suleiman S, et al. Developing and implementing mental health policy in Zanzibar, a low income country off the coast of East Africa. Int J Ment Health Syst. 2011;5:1–11.
Bowsher G, Papamichail A, El Achi N, Ekzayez A, Roberts B, Sullivan R, Patel P. A narrative review of health research capacity strengthening in low and middle-income countries: lessons for conflict-affected areas. Glob Heal. 2019. https://doi.org/10.1186/s12992-019-0465-y.pdf.
Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–33.
Reed JE, Howe C, Doyle C, Bell D. Simple rules for evidence translation in complex systems: a qualitative study. BMC Med. 2018;16(1):1–20.
Kalibala S, Nutley T. Engaging stakeholders, from inception and throughout the study, is good research practice to promote use of findings. AIDS Behav. 2019;23:214–9.
El-Jardali F, Lavis J, Moat K, Pantoja T, Ataya N. Capturing lessons learned from evidence-to-policy initiatives through structured reflection. Heal Res Policy Syst. 2014;12(1):2.
Kapiriri L. Does the narrative about the use of evidence in Priority setting vary across health programs within the health sector: a case study of 6 Programs in a Low-Income National Healthcare System. Int J Heal Policy Manag. 2020;9(10):448–58.
Puchalski Ritchie LM, Debebe F, Azazh A. Barriers to and facilitators of the development and utilization of context appropriate evidence based clinical algorithms to optimize clinical care and patient outcomes in the Tikur Anbessa emergency department: a multi-component qualitative study. BMC Heal Serv Res. 2019;19(1):181. https://doi.org/10.1186/s12913-019-4008-2.pdf.
Verboom B, Baumann A. Mapping the qualitative evidence base on the use of research evidence in health policy-making: a systematic review. Int J Heal Policy Manag. 2022;11(7):883–98.
Ezeanolue EE, Menson WN, Patel D, Aarons G, Olutola A, Obiefune M, Dakum P, Okonkwo P, Gobir B, Akinmurele T, Nwandu A, et al. Gaps and strategies in developing health research capacity: experience from the Nigeria Implementation Science Alliance. Heal Res Policy Syst. 2018;16(10):125. https://doi.org/10.1186/s12961-018-0289-x.pdf.
Singh DR, Sah RK, Simkhada B, Darwin Z. Potentials and challenges of using co-design in health services research in low- and middle-income countries. Glob Heal Res Policy. 2023;8(1):5. https://doi.org/10.1186/s41256-023-00290-6.pdf.
Henriksson DK, Peterson SS, Waiswa P, Fredriksson M. Decision-making in district health planning in Uganda: does use of district-specific evidence matter? Heal Res Policy Syst. 2019;17(1):57. https://doi.org/10.1186/s12961-019-0458-6.pdf.
Witter S, Kardan A, Scott M, Moore L, Shaxson L. Generating demand for and use of evaluation evidence in government health ministries: lessons from a pilot programme in Uganda and Zambia. Heal Res Policy Syst. 2017;15(1):86. https://doi.org/10.1186/s12961-017-0250-4.pdf.
Abekah-Nkrumah G, Issiaka S, Virgil L, Ermel J. A review of the process of knowledge transfer and use of evidence in reproductive and child health in Ghana. Heal Res Policy Syst. 2018;16(1):75.
Demment MM, Peters K, Dykens JA, Dozier A, Nawaz H, McIntosh S, et al. Developing the evidence-base to inform best practice: a scoping study of breast and cervical cancer reviews in low- and middle-income countries. Matern Child Nutr. 2015;10(9): e0134618.
Koon AD, Rao KD, Tran NT, Ghaffar A. Embedding health policy and systems research into decision-making processes in low- and middle-income countries. Heal Res Policy Syst. 2013;11:30. https://doi.org/10.1186/1478-4505-11-30.pdf.
Liverani M, Chheng K, Parkhurst J. The making of evidence-informed health policy in Cambodia: knowledge, institutions and processes. BMJ Glob Health. 2018;3(3): e000652.
Gilson L, Hanson K, Sheikh K, Agyepong IA, Ssengooba F. Building the field of health policy and systems research: social science matters. PLoS Med. 2011;8(8):1–6.
Chan CK, Oldenburg B, Viswanath K. Advancing the science of dissemination and implementation in behavioral medicine: evidence and progress. Int J Behav Med. 2015;22(3):277–82. https://doi.org/10.1007/s12529-015-9490-2.pdf.
Tangcharoensathien V, Sudhakar M, Birhanu Z, Abraham G, Bawah A, Kyei P, et al. Health policy and systems research capacities in Ethiopia and Ghana: findings from a self-assessment. Glob Heal Sci Pr. 2022;10(Suppl 1): e2100715.
Naude CE, Zani B, Ongolo-Zogo P, Wiysonge CS, Dudley L, Kredo T, et al. Research evidence and policy: qualitative study in selected provinces in South Africa and Cameroon. Implement Sci. 2015;10:126. https://doi.org/10.1186/s13012-015-0315-0.pdf.
Al-Bader S, Masum H, Simiyu K, Daar AS, Singer PA. Science-based health innovation in sub-Saharan Africa. BMC Int Heal Hum Rights. 2010;10(Suppl 1):S1. https://doi.org/10.1186/1472-698X-10-S1-S1.pdf.
Beran D, Miranda JJ, Cardenas MK, Bigdeli M. Health systems research for policy change: lessons from the implementation of rapid assessment protocols for diabetes in low- and middle-income settings. Heal Res Policy Syst. 2015;13:41. https://doi.org/10.1186/s12961-015-0029-4.pdf.
Varallyay NI, Langlois EV, Tran N, Elias V, Reveiz L. Health system decision-makers at the helm of implementation research: development of a framework to evaluate the processes and effectiveness of embedded approaches. Heal Res Policy Syst. 2020;18(1):64. https://doi.org/10.1186/s12961-020-00579-9.pdf.
Vanyoro KP, Hawkins K, Greenall M, Parry H, Keeru L. Local ownership of health policy and systems research in low-income and middle-income countries: a missing element in the uptake debate. BMJ Glob Heal. 2019;4(4):2–4.
Murunga VI, Oronje RN, Bates I, Tagoe N, Pulford J. Review of published evidence on knowledge translation capacity, practice and support among researchers and research institutions in low- and middle-income countries. Heal Res Policy Syst. 2020;18(1):16. https://doi.org/10.1186/s12961-019-0524-0.pdf.
Brownson RC, Chriqui JF, Stamatakis KA. Understanding evidence-based public health policy. Am J Public Health. 2009;99(9):1576–83.
Gaym A. Health research in Ethiopia–past, present and suggestions on the way forward. Ethiop Med J. 2008;46(3):287–308.
Bazalgette L. A Practical Guide for Establishing an Evidence Centre. Alliance Useful Evid. 2020; www.alliance4usefulevidence.org/join%0A, https://media.nesta.org.uk/documents/Practical_Guide_Evidence_Centre_mjf4AUw.pdf.
Dizon JM, Grimmer K, Louw Q, Machingaidze S, Parker H, Pillen H. Barriers and enablers for the development and implementation of allied health clinical practice guidelines in South African primary healthcare settings: a qualitative study. Heal Res Policy Syst. 2017;15(1):79. https://doi.org/10.1186/s12961-017-0243-3.pdf.
FHI. Eight strategies for research to practice. 2012.
Elliott S, Zimmerman G. Trusted Evidence, Informed Decisions, Better Health. 2019. p. 3044323. http://www.cochrane.org/
Unadkat MB, Mbuba CK, Ngugi AK, Kamya D. Self-reported knowledge, attitudes, practices and barriers in use of evidence-based medicine among resident physicians in Kenya: a mixed methods study. BMC Med Educ. 2021;21(1):537. https://doi.org/10.1186/s12909-021-02974-4.pdf.
Akhlaq A, McKinstry B, Muhammad KB, Sheikh A. Barriers and facilitators to health information exchange in low- and middle-income country settings: a systematic review. Heal Policy Plan. 2016;31(9):1310–25.
Votruba N, Grant J, Thornicroft G. EVITA 2.0, an updated framework for understanding evidence-based mental health policy agenda-setting: tested and informed by key informant interviews in a multilevel comparative case study. Heal Res Policy Syst. 2021;19:35.
Norton TC, Rodriguez DC, Willems S. Applying the Theoretical Domains Framework to understand knowledge broker decisions in selecting evidence for knowledge translation in low- and middle-income countries. Heal Res Policy Syst. 2019;17(1):60.
Hyder AA, Bloom G, Leach M, Syed SB, Peters DH. Exploring health systems research and its influence on policy processes in low income countries. Glob Heal Action. 2007;7:309. https://doi.org/10.1186/1471-2458-7-309.pdf.
Yamey G. What are the barriers to scaling up health interventions in low and middle income countries? A qualitative study of academic leaders in implementation science. Glob Heal. 2012;8:11. https://doi.org/10.1186/1744-8603-8-11.pdf.
Jessani NS, Rohwer A, Schmidt BM, Delobelle P. Integrated knowledge translation to advance noncommunicable disease policy and practice in South Africa: application of the Exploration, Preparation, Implementation, and Sustainment (EPIS) framework. Heal Res Policy Syst. 2021;19(1):82.
Bigdeli M, Zafar S, Assad H, Ghaffar A. Health system barriers to access and use of magnesium sulfate for women with severe pre-eclampsia and eclampsia in Pakistan: evidence for policy and practice. PLoS ONE. 2013;8(3): e59158.
Aaserud M, Lewin S, Innvaer S, Paulsen EJ, Dahlgren AT, Trommald M, et al. Translating research into policy and practice in developing countries: a case study of magnesium sulphate for pre-eclampsia. BMC Heal Serv Res. 2005;5:68. https://doi.org/10.1186/1472-6963-5-68.pdf.
Abu-Odah H, Molassiotis A, Liu JYW. Gathering policymakers’ perspectives as an essential step in planning and implementing palliative care services at a national level: an example from a resource-limited country. BMC Palliat Care. 2022;21(1):43. https://doi.org/10.1186/s12904-022-00936-1.pdf.
Cambe MI, Botão C, Dulá J, Muamine E, Mahumane S, Alberto C, et al. The use of research for health systems policy development and implementation in mozambique: a descriptive study. Glob Heal Sci Pr. 2022;10(Suppl 1): e2100694.
Ager A, Zarowsky C. Balancing the personal, local, institutional, and global: multiple case study and multidimensional scaling analysis of African experiences in addressing complexity and political economy in health research capacity strengthening. Heal Res Policy Syst. 2015;13:5. https://doi.org/10.1186/1478-4505-13-5.pdf.
Rosenbaum SE, Glenton C, Wiysonge CS, Abalos E, Mignini L, Young T, et al. Evidence summaries tailored to health policy-makers in low- and middle-income countries. Bull World Heal Organ. 2011;89(1):54–61.
Nabyonga-Orem J, Ssengooba F, Mijumbi R, Kirunga Tashobya C, Marchal B, Criel B, et al. Uptake of evidence in policy development: the case of user fees for health care in public health facilities in Uganda. BMC Heal Serv Res. 2014;14(1):639.
Votruba N, Grant J, Thornicroft G. The EVITA framework for evidence-based mental health policy agenda setting in low- and middle-income countries. Hum Vaccin Immunother. 2020;35(4):424–39.
Hawkes S, Aulakh BK, Jadeja N, Jimenez M, Buse K, Anwar I, et al. Strengthening capacity to apply health research evidence in policy making: experience from four countries. Heal Policy Plan. 2016;31(2):161–70.
Afshari M, Teymourlouy AA, Maleki MA-L, Mohammadreza M. Global Health diplomacy for noncommunicable diseases prevention and control: a systematic review. Global Health. 2020;16(1):41. https://doi.org/10.1186/s12992-020-00572-5.pdf.
Abubakar I, Dalglish SL, Aliyu SH, Ihekweazu CA, Bolu O, Aliyu SH. Lessons from co-production of evidence and policy in Nigeria’s COVID-19 response. BMJ Glob Heal. 2021;6(3): e004793.
Bulthuis SE, Kok MC, Raven J, Dieleman MA. Factors influencing the scale-up of public health interventions in low- and middle-income countries: a qualitative systematic literature review. Heal Policy Plan. 2020;35(2):219–34.
Dalheim A, Harthug S, Nilsen RM, Nortvedt MW. Factors influencing the development of evidence-based practice among nurses: a self-report survey. BMC Heal Serv Res. 2012;12:367. https://doi.org/10.1186/1472-6963-12-367.pdf.
Nabyonga-Orem J, Dovlo D, Kwamie A, Nadege A, Guangya W, Kirigia JM. Policy dialogue to improve health outcomes in low income countries: What are the issues and way forward? BMC Health Serv Res. 2016. https://doi.org/10.1186/s12913-016-1450-2.
Buse K. Addressing the theoretical, practical and ethical challenges inherent in prospective health policy analysis. Health Policy Plan. 2008;23(5):351–60.
Campos PA, Reich MR. Political analysis for health policy implementation. Heal Syst Reform. 2019;5(3):224–35. https://doi.org/10.1080/23288604.2019.1625251.
Oliver TR. The politics of public health policy. Annu Rev Public Health. 2006;27(104):195–233.
Orem J, Mafigiri D, Marchal B, Ssengooba F, MacQ J, Criel B. Research, evidence and policymaking: the perspectives of policy actors on improving uptake of evidence in health policy development and implementation in Uganda. BMC Public Health. 2012;12(1):109.
Panisset U, Koehlmoos TP, Alkhatib AH, Pantoja T, Singh P, Kengey-Kayondo J, et al. Implementation research evidence uptake and use for policy-making. Heal Res Policy Syst. 2012;10:1–7.
Okedo-Alex IN, Akamike IC, Olisaekee GO, Okeke CC, Uneke CJ. Identifying advocacy strategies, challenges and opportunities for increasing domestic health policy and health systems research funding in Nigeria: perspectives of researchers and policymakers. Heal Res Policy Syst. 2021;19(1):41. https://doi.org/10.1186/s12961-021-00701-5.pdf.
Kredo T, Cooper S, Abrams A, Daniels K, Volmink J, Atkins S. National stakeholders’ perceptions of the processes that inform the development of national clinical practice guidelines for primary healthcare in South Africa. J Int AIDS Soc. 2018;16(1):68. https://doi.org/10.1186/s12961-018-0348-3.pdf.
Uneke CJ, Sombie I, Johnson E, Uneke BI, Okolo S. Promoting the use of evidence in health policymaking in the ECOWAS region: the development and contextualization of an evidence-based policymaking guidance. Global Health. 2020;16(1):1–12.
Wu S, Khan M, Legido-Quigley H, Legido-Quigley H. What steps can researchers take to increase research uptake by policymakers? A case study in China. Health Policy Plan. 2020;35(6):665–75.
Naghibi D, Mohammadzadeh S, Azami-Aghdash S. Barriers to evidence-based practice in health system: a systematic review. J Evidence-based Care. 2021;11(2):74–82.
Pucca GA, Gabriel M, De Araujo MED, De Almeida FCS. Ten years of a national oral health policy in Brazil: innovation, boldness, and numerous challenges. J Dent Res. 2015;94(10):1333–7.
Glandon D, Meghani A, Jessani N, Qiu M, Bennett S. Identifying health policy and systems research priorities on multisectoral collaboration for health in low-income and middle-income countries. BMJ Glob Heal. 2018;3:1–14.
Conalogue DM, Kinn S, Mulligan JA, McNeil M. International consultation on long-term global health research priorities, research capacity and research uptake in developing countries. Heal Res Policy Syst. 2017;15(1):1–6.
Mauti J, Gautier L, De Neve JW, Beiersmann C, Tosun J, Jahn A. Kenya’s health in all policies strategy: a policy analysis using Kingdon’s multiple streams. Heal Res Policy Syst. 2019;17(1):15. https://doi.org/10.1186/s12961-019-0416-3.pdf.
Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health. 2014;14(1):188.
Zhou W, Ouyang F, Nergui O-E, Bangura JB, Acheampong K, Massey IY, et al. Child and adolescent mental health policy in low- and middle-income countries: challenges and lessons for policy development and implementation. Front Psychiatry. 2020;11(March):1–8.
El-Jardali F, Lavis JN, Ataya N, Jamal D. Use of health systems and policy research evidence in the health policymaking in eastern Mediterranean countries: views and practices of researchers. Implement Sci. 2012;7(1):1–16.
Musango L, Orem JN, Elovainio R, Kirigia J. Moving from ideas to action - developing health financing systems towards universal coverage in Africa. BMC Int Heal Hum Rights. 2012;12:30. https://doi.org/10.1186/1472-698X-12-30.pdf.
Liverani M, Hawkins B, Parkhurst JO. Political and institutional influences on the use of evidence in public health policy A systematic review. PLoS ONE. 2013;8(10): e77404.
Sigudla J, Maritz J. A model to facilitate research uptake in health care practice and policy development for low- resource countries. 2020. p. 1–32.
Inguane C, Sawadogo-Lewis T, Chaquisse E, Roberton T, Ngale K, Fernandes Q, et al. Challenges and facilitators to evidence-based decision-making for maternal and child health in Mozambique: district, municipal and national case studies. BMC Heal Serv Res. 2020;20(1):598. https://doi.org/10.1186/s12913-020-05408-x.pdf.
Hyder AA, Corluka A, Winch PJ, El-Shinnawy A, Ghassany H, Malekafzali H, et al. National policy-makers speak out: are researchers giving them what they need? Health Policy Plan. 2011;26(1):73–82.
Vania DK, Randall GE. Can evidence-based health policy from high-income countries be applied to lower-income countries: considering barriers and facilitators to an organ donor registry in Mumbai, India. Heal Res Policy Syst. 2016;14:1–11.
Khalid AF, Lavis JN, El-Jardali F, Vanstone M. Supporting the use of research evidence in decision-making in crisis zones in low- and middle-income countries: a critical interpretive synthesis. Heal Res Policy Syst. 2020;18(1):1–12.
Erismann S, Pesantes MA, Beran D, Leuenberger A, Farnham A, Berger Gonzalez de White M, et al. How to bring research evidence into policy? Synthesizing strategies of five research projects in low-and middle-income countries. Heal Res Policy Syst. 2021;19(1):29. https://doi.org/10.1186/s12961-020-00646-1.pdf.
Mogueo A, Defo BK, Mbanya JC. Healthcare providers’ and policymakers’ experiences and perspectives on barriers and facilitators to chronic disease self-management for people living with hypertension and diabetes in Cameroon. BMC Prim Care. 2022;23(1):291. https://doi.org/10.1186/s12875-022-01892-8.pdf.
Malama A, Zulu JM, Nzala S, Kombe MM, Silumbwe A. Health research knowledge translation into policy in Zambia: policy-maker and researcher perspectives. Heal Res Policy Syst. 2021. https://doi.org/10.1186/s12961-020-00650-5.pdf.
Namisango E, Ramsey L, Dandadzi A, Okunade K, Ebenso B, Allsop MJ. Data and information needs of policymakers for palliative cancer care: a multi-country qualitative study. BMC Med Inf Decis Mak. 2021;21(1):189. https://doi.org/10.1186/s12911-021-01555-1.pdf.
Goyet S, Barennes H, Libourel T, van Griensven J, Frutos R, Tarantola A. Knowledge translation: a case study on pneumonia research and clinical guidelines in a low- income country. Int Nurs Rev. 2014;9:82. https://doi.org/10.1186/1748-5908-9-82.pdf.
Motani P, Van de Walle A, Aryeetey R, Verstraeten R. Lessons learned from evidence-informed decision-making in nutrition & health (EVIDENT) in Africa: a project evaluation. Heal Res Policy Syst. 2019;17(12):643–50. https://doi.org/10.1186/s12961-019-0413-6.pdf.
Bennett S, Paina L, Ssengooba F, Waswa D, M’Imunya JM. The impact of Fogarty International Center research training programs on public health policy and program development in Kenya and Uganda. BMC Public Health. 2013;13:770. https://doi.org/10.1186/1471-2458-13-770.pdf.
Langlois EV, Mancuso A, Elias V, Reveiz L. Embedding implementation research to enhance health policy and systems: a multi-country analysis from ten settings in Latin America and the Caribbean. Heal Res Policy Syst. 2019;17(1):85. https://doi.org/10.1186/s12961-019-0484-4.pdf.
Li R, Ruiz F, Culyer AJ, Chalkidou K, Hofman KJ. Evidence-informed capacity building for setting health priorities in low- and middle-income countries: a framework and recommendations for further research. Hum Reprod Updat. 2017;6:231.
Shroff ZC, Javadi D, Gilson L, Kang R, Ghaffar A. Institutional capacity to generate and use evidence in LMICs: current state and opportunities for HPSR. Heal Res Policy Syst. 2017;15(1):94. https://doi.org/10.1186/s12961-017-0261-1.pdf.
VanDevanter N, Vu M, Nguyen A, Nguyen T, Van Minh H, Nguyen NT, et al. A qualitative assessment of factors influencing implementation and sustainability of evidence-based tobacco use treatment in Vietnam health centers. Implement Sci. 2020;15(1):73. https://doi.org/10.1186/s13012-020-01035-6.pdf.
Jha A, Lin L, Short SM, Argentini G, Gamhewage G, Savoia E. Integrating emergency risk communication (ERC) into the public health system response: Systematic review of literature to aid formulation of the 2017 WHO Guideline for ERC policy and practice. PLoS ONE. 2018;13(10): e0205555.
Grobbelaar SS. Building institutional capacity for Research Uptake. Dev Res Uptake Sub-Saharan Africa. 2013; www.drussa.net/drussa.mobi
Lavis JN, Oxman AD, Moynihan R, Paulsen EJ. Evidence-informed health policy 1 - Synthesis of findings from a multi-method study of organizations that support the use of research evidence. Implement Sci. 2008;3(1):1–7.
Schleiff MJ, Kuan A, Ghaffar A. Comparative analysis of country-level enablers, barriers and recommendations to strengthen institutional capacity for evidence uptake in decision-making. Heal Res Policy Syst. 2020;18(1):1–12.
da Silva ATC, Hanlon C, Susser E, Rojas G, Claro HG, Quayle J, et al. Enhancing mental health research capacity: emerging voices from the National Institute of Mental Health (NIMH) global hubs. Int J Ment Heal Syst. 2019;13:21. https://doi.org/10.1186/s13033-019-0276-9.pdf.
Uzochukwu B, Onwujekwe O, Mbachu C, Okwuosa C, Etiaba E, Nyström ME, et al. The challenge of bridging the gap between researchers and policy makers: experiences of a Health Policy Research Group in engaging policy makers to support evidence informed policy making in Nigeria. Glob Health. 2016. https://doi.org/10.1186/s12992-016-0209-1.
Parkhurst J, Ettelt S, Peters G. Evidence use in health policy making: an international public policy perspective. 2018. 245 p. http://www.eprints.lse.ac.uk/90272/1/Parkhurst_Evidenceuse in healthpolicy_2018.pdf
Schmitz HP. The global health network on alcohol control: successes and limits of evidence-based advocacy. Heal Policy Plan. 2016;31(Suppl 1):i87-97.
Tilahun H, Flannery J, Berman P. Review of local and global practices on evidence- informed health policy: recommendations for Ethiopia. Massachusetts: Harvard TH Chan Sch Public Heal Boston; 2015.
Narasimhan M, Lucido B, Say L, Gholbzouri K, El-Adawy M, Al MA. Changing national health policies for introduction, uptake and scale-up of self-care interventions for sexual and reproductive health and rights in the Eastern Mediterranean Region. Heal Res Policy Syst. 2021;19(1):1–6.
Gilson L, Raphaely N. The terrain of health policy analysis in low and middle income countries: a review of published literature 1994–2007. Heal Policy Plan. 2008;23:294–307.
Dam JL, Nagorka-Smith P, Waddell A, Wright A, Bos JJ, Bragge P. Research evidence use in local government-led public health interventions: a systematic review. Heal Res Policy Syst [Internet]. 2023;21(1):1–15. https://doi.org/10.1186/s12961-023-01009-2.
De Freitas Lopes AC, Novaes HMD, De Soárez PC. Does patient and public involvement impact public health decision-making? A 10 year retrospective analysis of public consultation in Brazil. Heal Res policy Syst. 2023;21(1):72. https://doi.org/10.1186/s12961-023-01018-1.
Farris P, Crist R, Miller S, Shannon J. Rural research capacity: a co-created model for research success. Heal Res Policy Syst. 2023;21(1):1–13. https://doi.org/10.1186/s12961-023-01030-5.
van den Akker A, Fabbri A, Alardah DI, Gilmore AB, Rutter H. The use of participatory systems mapping as a research method in the context of non-communicable diseases and risk factors: a scoping review. Heal Res Policy Syst. 2023;21(1):1–14. https://doi.org/10.1186/s12961-023-01020-7.
Alley ZM, Chapman JE, Schaper H, Saldana L. The relative value of pre-implementation stages for successful implementation of evidence-based practice. Under Rev. 2022. https://doi.org/10.1186/s13012-023-01285-0.
Mahendradhata Y, Kalbarczyk A. Prioritizing knowledge translation in low- and middle-income countries to support pandemic response and preparedness. Heal Res Policy Syst. 2021;19(1):10–2. https://doi.org/10.1186/s12961-020-00670-1.
Malla C, Aylward P, Ward P. Knowledge translation for public health in low- and middle- income countries: a critical interpretive synthesis. Glob Heal Res Policy. 2018;3(1):1–12.
Emmons KM, Chambers D, Abazeed A. Embracing policy implementation science to ensure translation of evidence to cancer control policy. Transl Behav Med. 2021;11(11):1972–9.
Kim C, Wilcher R, Petruney T, Krueger K, Wynne L, Zan T. A research utilisation framework for informing global health and development policies and programmes. Heal Res Policy Syst. 2018;16(1):1–10.
Bennett S, Corluka A, Doherty J, Tangcharoensathien V. Approaches to developing the capacity of health policy analysis institutes: a comparative case study. Heal Res Policy Syst. 2012;10:1–9.
Wensing M, Sales A, Aarons GA, Xu D, Wilson P. Evidence for objects of implementation in healthcare: considerations for implementation science and implementation science communications. Implement Sci. 2022;17(1):1–5. https://doi.org/10.1186/s13012-022-01249-w.
Uberoi D, Ojo T, Sriharan A, Lau L. What can implementation science offer civil society in their efforts to drive rights-based health reform? Glob Heal Res Policy. 2023;8(1):4–10. https://doi.org/10.1186/s41256-023-00284-4.
Owusu-Manu D, Badu E, Agyekum K, Akom JB. Putting research into practice : Exploring the inherent challenges of research uptake in the built environment faculties in ... Procs 6th West Africa Built Environment Research (WABER) Conference. 2015.
Yazdizadeh B, Sajadi HS, Mohtasham F, Mohseni M, Majdzadeh R. Systematic review and policy dialogue to determine challenges in evidence-informed health policy-making: findings of the SASHA study. Heal Res Policy Syst. 2021;19(1):73.
Partridge ACR, Mansilla C, Randhawa H, Lavis JN, El-Jardali F, Sewankambo NK. Lessons learned from descriptions and evaluations of knowledge translation platforms supporting evidence-informed policy-making in low- and middle-income countries: a systematic review. Heal Res Policy Syst. 2020;18(1):1–22.
Penkunas MJ, Berdou E, Chong SY, Launois P, Rhule ELM, Allotey P. Increasing knowledge translation capacity in low- and middle-income countries: a model for implementation research training. Front Trop Dis. 2021;2(December):1–10.
Osanjo GO, Oyugi JO, Kibwage IO, Mwanda WO, Ngugi EN, Otieno FC, et al. Building capacity in implementation science research training at the University of Nairobi. Implement Sci. 2016;11(1):1–9. https://doi.org/10.1186/s13012-016-0395-5.
Riera R, de Oliveira Cruz Latorraca C, Padovez RCM, Pacheco RL, Romão DMM, Barreto JOM, et al. Strategies for communicating scientific evidence on healthcare to managers and the population: a scoping review. Heal Res Policy Syst. 2023;21(1):1–20. https://doi.org/10.1186/s12961-023-01017-2.
Squires JE, Graham ID, Santos WJ, Hutchinson AM, Team TI. The Implementation in Context ( ICON ) Framework : A meta ‑ framework of context domains , attributes and features in healthcare. 2023;1–19.
Acknowledgements
This work was financially supported by the Wellcome Trust [Grant ID 221576/Z/20/Z]. We would also like to thank the CDT-Africa, Addis Ababa University, University of Sussex and National Institute of Health Research (NIHR)-Wellcome Global Health Research Partnership, UK, for the overall support. AF receives a research grant from the NIHR-Wellcome Trust to the Unit for Health Evidence and Policy (UHEP) Ethiopia (Grant ID 221576/Z/20/Z) and NIHR Global Health Research Unit on Neglected Tropical Diseases-Phase 1 (G2153) & Phase 2 (G3417). CH receives support from the National Institute of Health and Care Research through the NIHR Global Health Research Group on Homelessness and Mental Health in Africa (NIHR134325) and the SPARK project (NIHR200842) using UK aid from the UK Government. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. CH receives support from the Wellcome Trust through grants 222154/Z20/Z and 223615/Z/21/Z.
Funding
This work was financially supported by the Wellcome Trust [Grant ID 221576/Z/20/Z]. The funder has no role on the technical work and interpretation of the finding which is responsibility of authors.
Author information
Authors and Affiliations
Contributions
AF, AS, TM, EG, and BF participated from conception to design of the proposed project implementation. AS drafted the manuscript. All authors review the manuscript and incorporate their scientific and intellectual inputs, provided feedback and approved for final submission.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
NA.
Consent for publication
NA.
Competing interest
Have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1.
Completed- Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2.
Literature search strategies.
Additional file 3.
Data charting.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Semahegn, A., Manyazewal, T., Hanlon, C. et al. Challenges for research uptake for health policymaking and practice in low- and middle-income countries: a scoping review. Health Res Policy Sys 21, 131 (2023). https://doi.org/10.1186/s12961-023-01084-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12961-023-01084-5