Abstract
Background
Health workforce projection models are integral components of a robust healthcare system. This research aims to review recent advancements in methodology and approaches for health workforce projection models and proposes a set of good practice reporting guidelines.
Methods
We conducted a systematic review by searching medical and social science databases, including PubMed, EMBASE, Scopus, and EconLit, covering the period from 2010 to 2023. The inclusion criteria encompassed studies projecting the demand for and supply of the health workforce. PROSPERO registration: CRD 42023407858.
Results
Our review identified 40 relevant studies, including 39 single countries analysis (in Australia, Canada, Germany, Ghana, Guinea, Ireland, Jamaica, Japan, Kazakhstan, Korea, Lesotho, Malawi, New Zealand, Portugal, Saudi Arabia, Serbia, Singapore, Spain, Thailand, UK, United States), and one multiple country analysis (in 32 OECD countries). Recent studies have increasingly embraced a complex systems approach in health workforce modelling, incorporating demand, supply, and demand–supply gap analyses. The review identified at least eight distinct types of health workforce projection models commonly used in recent literature: population-to-provider ratio models (n = 7), utilization models (n = 10), needs-based models (n = 25), skill-mixed models (n = 5), stock-and-flow models (n = 40), agent-based simulation models (n = 3), system dynamic models (n = 7), and budgetary models (n = 5). Each model has unique assumptions, strengths, and limitations, with practitioners often combining these models. Furthermore, we found seven statistical approaches used in health workforce projection models: arithmetic calculation, optimization, time-series analysis, econometrics regression modelling, microsimulation, cohort-based simulation, and feedback causal loop analysis. Workforce projection often relies on imperfect data with limited granularity at the local level. Existing studies lack standardization in reporting their methods. In response, we propose a good practice reporting guideline for health workforce projection models designed to accommodate various model types, emerging methodologies, and increased utilization of advanced statistical techniques to address uncertainties and data requirements.
Conclusions
This study underscores the significance of dynamic, multi-professional, team-based, refined demand, supply, and budget impact analyses supported by robust health workforce data intelligence. The suggested best-practice reporting guidelines aim to assist researchers who publish health workforce studies in peer-reviewed journals. Nevertheless, it is expected that these reporting standards will prove valuable for analysts when designing their own analysis, encouraging a more comprehensive and transparent approach to health workforce projection modelling.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Effective health workforce planning is a key instrument for a resilient and sustainable health system that achieves its key objectives, including enhancing access, health outcomes, responsiveness, and reducing disparities [1]. Health workforce projection model is an integral element of health workforce planning, a crucial quantitative tool to attain the so-called ‘6 rights’ in the health workforce, e.g. ensuring the right number of professionals with the right skills, delivering the right services at the right time and place, all with right financial resources to address health workforce gap [2, 3]. Inaccurate health workforce projection and forecasting can result in workforce shortages or surpluses, leading to inadequate care, increased costs, and restricted access [1].
It is important to recognize that, in many health systems, health workforce challenges are not simply about the total number of healthcare professionals, but also a distributional one [4, 5]. In high-income countries, despite universal health coverage, it is not uncommon for the health system to suffer from severe shortages of healthcare professionals in specific specialties or regions [6, 7]. In low- and middle-income countries, where resource constraints often present significant challenges, achieving effective health workforce planning is further complicated by limited financial resources and the need to balance healthcare delivery with workforce sustainability, highlighted by the Sustainable Development Goals Target 3c [8, 9].
The analysis of the health workforce, though fundamentally a labour market study, exhibits attributes that distinguish it from other sectors. Notably, one of the significant challenges lies in the lengthy training period for health professionals, which can exceed a decade. The regulatory framework governing the health workforce introduces complexities, constraining its adaptability and response to short-term provider needs [10, 11]. The health workforce, itself operating as a complex system, is linked with many other sectors or systems in society, such as education, immigration, and public finance. Hence, achieving labour market equilibrium through the ‘invisible hand’ of demand and supply can be challenging, leading to both acute and chronic shortages or surpluses in the health workforce.
Over the past decade, the methodologies and techniques of health workforce projection and forecasting models have evolved more complex, particularly in methods aligning health workforce projection with underlying population health needs and health workforce requirements of various health service delivery models [12, 13]. However, there is a notable gap in the systematic review summarizing the development of these methodologies. While there may be numerous studies on health workforce projection and forecasting, there is a lack of systematic guidelines on how these studies should be conducted and reported. This lack of transparency has led to the misperception that health workforce models operate as ‘black boxes’, without a clear explanation of statistical approaches, assumptions and data sources, and model validity.
The aim of this paper is to conduct a systematic review of recent literature on health workforce projection and forecasting, with the dual purpose of summarizing key findings and proposing comprehensive good practice reporting guidelines. Specifically, we aim to: (1) systematically review and synthesize the existing literature on methods used in health workforce projection models to identify key findings, trends, and methodological approaches; (2) critically assess the methodological quality, strengths, and weaknesses of the existing literature, with a focus on its relevance in answering policy and scenario analysis; (3) develop good practice reporting guidelines that encompass essential elements of study design, data, methodology, and reporting specific to health workforce projection models.
Methods
This systematic review adhered to a pre-established protocol and was registered with PROSPERO (registration number CRD 42023407858).
Systematic review of peer-reviewed papers
We conducted a systematic review of recent academic papers focused on health workforce projection and forecasting models published since 2010.
Database
In August 2023, we systematically searched electronic databases, including Ovid Medline, EMBASE, and Scopus. The search encompassed articles published from January 1, 2010, to June 2023. The time frame was limited to recent studies to focus on the most relevant and up-to-date information. Additionally, the bibliographies of included articles were screened to identify additional studies meeting the inclusion criteria.
Search strategy
Our search strategy involved the utilization of relevant keywords and Medical Subject Headings (MeSH) terms. The keywords for health workforce were ‘health workforce’, ‘health professionals’, and ‘human resources’. The keywords for projection and forecasting models were ‘planning’, ‘model’, ‘forecast’, and ‘projection’.
Inclusion and exclusion criteria
Population, Intervention, Comparison, Outcome, Study Design (PICOS) inclusion and exclusion criteria are outlined in Table 1.
Data extraction
A standardized data extraction form was developed to systematically extract relevant information from the included studies. Key data elements included study characteristics (e.g. author, publication year, study design), methodology, data sources, variables utilized in the models, and the models’ application in addressing specific health policy issues.
The process of developing the reporting guideline engaged a panel of experts with diverse backgrounds in health workforce planning. This included specialists in health workforce modelling (IC, JTL, MT, JL), health workforce data (DM), and health workforce implementation (MC). Furthermore, experts experienced in journal editing (JTL) and decision-making (MC, FX, TS) participated in the discussions. This collaborative approach leveraged their collective expertise to ensure the academic rigour of the reporting guideline and its relevance in policymaking.
Results
We retrieved 4070 citations from bibliographic databases, supplemented by 73 citations from other sources. After removing duplicates, we screened 2657 unique citations by title and abstract, resulting in 336 full-text articles for further evaluation. Out of these, 292 studies were excluded based on predefined criteria, and ultimately, 40 studies met the final inclusion criteria. The PRISMA flowchart of the study identification process is presented in Fig. 1.
Characteristics of included articles
The systematic review covered 40 articles from various countries, including 39 single-country studies and one multiple-country study. Over 70 percent of studies concentrated in high-income countries. Single-country studies represented a range of countries, including Australia (n = 3) [14,15,16], Canada (n = 6) [17,18,19,20,21,22], Germany (n = 1) [23], Ghana (n = 2) [24, 25], Guinea (n = 1) [26], Ireland (n = 1) [27], Jamaica (n = 1) [28], Japan (n = 1) [29], Kazakhstan (n = 1) [30], Korea (n = 1) [31], Lesotho (n = 1) [32], Malawi (n = 1) [33], New Zealand (n = 2) [34, 35], Portugal (n = 1) [36], Saudi Arabia (n = 1) [37], Serbia (n = 1) [38], Singapore (n = 2) [39, 40], Spain (n = 1) [41], Thailand (n = 3) [42,43,44], the United Kingdom (n = 2) [45, 46], and the United States (n = 6) [47,48,49,50,51,52]. The multiple-country study focused on 32 OECD countries [53].
Among the included studies, 30 focused on national analysis, and only ten focused on sub-national analyses, examining specific regions or areas within a country. The most considered health professionals in the models were physicians and general practitioners (GPs) (n = 17), nurses (n = 12), and dental professionals (n = 4). The mean and median projected duration in the models reviewed were 15.7 and 15.0 years, respectively. A detailed description of each article can be found in Additional file 1: Table S1.
Components of the health workforce projection model
Nearly all the included studies describe the overarching analytical framework for the health workforce planning model. Figure 2 summarizes the analytical framework, consisting of three components: demand-side analysis, supply-side analysis, and gap analysis (including training and financial resources needs). It is worth noting that very few studies also incorporate budgetary analysis (n = 5) into the gap analysis to examine the financial feasibility of closing the supply–demand gap. The primary tool employed in building these models is Excel spreadsheets.
Supply and demand analytical framework
We identified eight common supply and demand projection frameworks: population-to-provider ratios (n = 7), utilization-based (n = 10), needs-based (n = 25), skill-mixed (n = 5), stock-and-flow (n = 40), agent-based simulation (n = 3), system dynamic (n = 7) and budgetary model (n = 5). Studies often combine these models to project the demand and supply of the health workforce. We further summarize the relative strengths and limitations of each model in Additional file 1: Table S2.
It is worth noting that included studies often combine these models for demand, supply, and gap analysis. Additionally, we identified seven statistical approaches commonly used for estimation: arithmetic calculation, optimization, time series analysis, econometric regression, microsimulation, cohort-based simulation, and feedback causal loops (see Table 2 for model and approach details).
Demand-side analysis
The Provider-to-Population model estimates health workforce requirements as a proportion of the population. A common statistical approach used for this model is arithmetic calculation. For example, Lupu et al. [47] adopted this model to calculate the workforce requirements for hospice and palliative care as a fraction of the 65+ population in the US. More sophisticated approaches like time series analysis have also been applied. Milicevic et al. [38] estimated a polynomial least squares model to project the population requiring public health specialists in Serbia. The provider-to-population model is simple and easy to use. However, it disregards skills, distribution, and specific healthcare needs. Another limitation arises from the challenge of determining the “ideal” ratio of providers to the population, which is subjective and influenced by healthcare needs, geography, and cultural context.
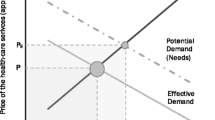
Utilization (or demand-based) models can overcome the above limitation by estimating health service needs based on historical utilization. Since historical data are used, the most common statistical approaches used for this model are econometrics and time series analysis. For instance, Jager et al. [23] projected dental services using least-square estimation, accounting for factors like age, gender, and socioeconomic status. This straightforward approach enables policymakers to incorporate demographic factors into the demand projection. However, it is important to note that utilization-based models also have limitations. They heavily rely on past or current utilization patterns, which may overlook unmet needs or instances of overutilization within the population. This can be mitigated by adjusting for unmet needs, as done by Landry et al. [52].
To address over-utilization in the demand projection, an alternative solution to model demand is to use needs instead of utilization. The schema of the conceptual framework of the needs-based model is illustrated in Additional file 1: Fig. S1. The needs-based model, found in most included studies, explicitly considers population health needs, particularly epidemiological factors like health conditions and health status. For example, Tomblin Murphy et al. [53] estimated the needs for general practitioners to deliver primary care in Canada. Time series analysis is also used for predicting demographic and epidemiological trends in this model. An example is Al-Senani et al. [37], who predicted stroke incidence using epidemiological modelling to determine workforce requirements. Since the model relies heavily on disease prevalence data, these studies focus more on a single health condition than a broader range of health conditions. Moreover, the model also does not account for changes in the delivery of health care due to the missing utilization data.
The skill-mix model, applied in several studies, uses optimization models to optimize the allocation of healthcare professionals, considering skills, capacity, scope of practice, and capability. An advantage of this model is the ability to account for substitution between providers of the same levels (horizontal substitutions) and between providers of different levels (vertical substitutions). For example, Gallagher et al. [45, 46] used an optimization model to identify the optimal healthcare workforce mix for dental services in the UK. Both papers used linear programming, which assumes workforce requirements as a linear function of dental care demand estimates, staff competency, cost, and volume of activity. Then, an optimal staff mix can be numerically computed. Despite its uses in decision-making, the skill mix model relies heavily on skill data, which is sometimes unavailable. Incomplete or inaccurate data can affect the accuracy of the model's reflection of the actual distribution of skills within the healthcare workforce. Additionally, the model may not sufficiently consider factors such as patient preferences or cultural aspects that can influence the distribution of healthcare providers. Lastly, the skill-mix model can be difficult for non-mathematicians to use since it builds on the optimization process, which can be computationally complex [54].
Supply-side analysis
Supply-side analysis typically begins with a stock-and-flow model, which examines workforce variables such as size, education, migration, and attrition. The input variables can be estimated using either simple mathematical formulas or more advanced time series analysis. The model also estimates clinical Full-Time Equivalents (FTE) based on participation rates and direct clinical time. The stock-and-flow model provides a simplified yet effective framework for analysing the supply side of the health workforce. However, it may not capture the heterogeneity in the workforce (e.g. age) and its interaction with the system (e.g. changes in minimum wages).
Agent-Based Simulation (ABS) and System Dynamic (SD) models can address these limitations. The ABS adopts the microsimulations approach to simulate the behaviour and interactions of individual agents, such as healthcare workers, within a given system, considering their interactions with the broader policy and social-environmental context. For example, Lopes [36] built an ABS model using Portuguese administrative data to predict the healthcare workers’ decision to work, providing a more detailed prediction of the anticipated supply. They built the model in AnyLogic, a free software tool for simulation. Another free software that can be used for microsimulation is R. The software has been used by the US. Health Resources and Services Administration to produce their health workforce model and dashboard [55].
Unlike ABS models, SD models operate at the cohort or group levels, accounting for feedback loops and delays. Thus, it enables the interconnectivity of different model components. For example, Dill et al. [49] utilized this model to estimate the supply of physicians in the US. The model builds on the stock-and-flow model but allows it to respond to demand changes and vice versus. For example, when supply exceeds demand, immigration may slow down. The model is built in free simulation software, Vensim. Another SD software is Stella, which is a web-based modelling tool. However, the software is free for only limited functions. Although these two models are helpful in predicting changes in the labour supply because of system changes, both methods are time-consuming and resource-intensive, requiring detailed unit-level data and specific software knowledge.
Gap analysis and budgetary analysis
Gap analysis is a common element in all studies, presenting demand–supply gaps in absolute numbers and sometimes relative gaps. Additionally, some studies incorporate budgetary analysis, as seen in Asamani et al. [32], which assesses the financial implications of filling supply–demand gaps and evaluates affordability within public health budgets.
Data prerequisites, variables, and sources
Most included studies described data and variables for their models. Table 3 summarizes data prerequisites for various models.
Demand-side analyses increase data complexity from the Provider-to-Population Model to the Utilization and Needs-Based Models. The Provider-to-Population Model requires basic demographic data, while the Utilization Model adds age and gender-based health service utilization rates. The Needs-Based Model extends this to epidemiological data, health interventions, and service delivery recommendations. Skill-mix models need comprehensive data for optimizing the workforce. Except for the Provider-to-Population Model, all demand-side models require productivity and workload data to estimate health workforce needs based on service requirements.
Supply-side models have specific data needs. The Stock and Flow Model needs current health workforce, education, mobility, and migration data. Agent-Based Simulation Models use individual behaviour data. System Dynamic Models focus on feedback loops, while Budgetary Analysis requires staff costs, education expenses, intervention costs, and government health budget data.
Our findings indicate a prevalent use of assumptions in the models, with many parameters derived from prior literature or expert opinions. Notably, sub-national analyses often suffer from a lack of local-specific data, while even national analyses often have challenges with data availability and accessibility. For instance, in a needs-based analysis of physicians, midwives, and nurses in 32 OECD countries, Tomblin-Murphy et al. [53] found that only 35% of the data elements required to implement the projection model were available. The most common available variables were population size, general health status of the population, head count of current supply, new graduates per year, health workforce participation rate, salary. Other variables have minimal availability.
Methods for model validation and uncertainty
We found limited number of the studies, incorporating model validation and uncertainty analysis (see Additional file 1: Table S4). These analyses comprise three key aspects: external model validation of the model structure (n = 4), internal validation of prediction accuracy (n = 8), and sensitivity analysis to assess parameter uncertainty (n = 13).
External model validation is used to confirm the accuracy of the high-level model structure in the system dynamic model and evaluate the behavioural assumptions in the agent-based simulation models. To achieve this, researchers often engage in panel discussions with groups of experts in healthcare services, systems research, and government agencies. The aim is to reach a consensus that the model structure accurately reflects real-world situations [43].
On the other hand, internal validation primarily focuses on demonstrating that the model's predictions closely align with actual values. All included papers conduct internal validation by comparing model estimates with historical data. The statistical analysis method used in this validation process often involves calculating the normalized measure of error or root-mean-square percentage error (RMPSE). A commonly accepted rule of thumb is that an RMPSE of less than 10% is considered reasonable [40, 56].
Regarding uncertainty stemming from parameters in the model, two types of sensitivity analysis are normally conducted in the included studies: probabilistic and deterministic analysis. The first approach utilized in Lopes et al. [36], is the Markov Chain Monte Carlo (MCMC) analysis. This involves generating replicated samples of parameters and running simulations multiple times to estimate the probability distribution of model values, allowing for the generation of confidence intervals in the estimates. The second approach commonly used to address parameter uncertainty involves comparing estimates derived from high and low parameter values. For example, Anash et al. [56] assessed model uncertainty by comparing optimistic and pessimistic scenarios.
Policy and scenario analysis
Most studies (32 out of 40) conducted policy and scenario analysis, as detailed in Additional file 1: Table S4. This analysis changes one or some parameters in the model and identifies changes in the outputs compared to a status quo. The common parameter changes include changes in population size (n = 7), epidemiological characteristics (n = 5), alternative care delivery models (n = 11), levels of health insurance use (n = 6), intervention affects labour participation of health workforce (n = 12), increases in education and training placements (n = 14), the number of overseas immigrants (n = 3), and changes in working hours and productivity levels (n = 14).
Most studies model multiple scenarios simultaneously rather than a single intervention alone. For example, Tomblin-Murphy [17] models the following policies in isolation, as well as the combined effect of the following policies: increased education places, reduced attrition in education programmes, improved retention in workforce, reduced absenteeism, reduced in-migration of foreign-trained workforce, increase productivity level.
Recommended health workforce projection model reporting guideline
One of the key findings of our study is the lack of standardization in reporting methods within existing studies. In response, we have proposed a “Good Practice Reporting Guideline for Health Workforce Models” (Table 4). The “Good Practice Guideline for Health Workforce Reporting” comprises 30 items that provide a structured framework for clear and comprehensive reporting in health workforce projection studies. These items cover critical aspects, including study identification, population characteristics, geographical considerations, analytical methods, results presentation, demand–supply gap analysis, and financial assessments. Furthermore, the guideline emphasizes the significance of addressing uncertainty, assumptions, and model validation.
Discussion
Principal findings
Our study provides a comprehensive review of recent advancements in the methods for health workforce projection and forecasting models. In our study, we have identified eight different model types covering supply, demand, and budgetary components of the health workforce projection model. It is important to acknowledge that no model can be considered flawless, as each one operates under its unique set of assumptions, strengths, and limitations. Health workforce modelers frequently used these eight models in combination. Our findings suggest that best practices incorporate considerations of both the drivers of supply and demand for healthcare services, in addition to epidemiological needs, shifts in productivity, skill mix dynamics, policy alternatives, and budgetary requirements.
Regarding statistical techniques, we have identified seven common statistical approaches used in health workforce projection models, and the use of these approaches is highly contingent on data availability. These techniques are commonly used and have their roots in the fields of health economics, operational, epidemiological, and health service research. It is also noteworthy that workforce projection often relies on imperfect data with limited granularity at the local level.
Furthermore, it is important to acknowledge the diversity of health workforce projection models and statistical approaches in the literature, where existing studies often lack uniformity in reporting their methodologies. While some health workforce modelers consider health workforce modelling a blend of science and art [57, 58], our best-practice reporting guidelines aim to provide a comprehensive framework for future research in this field. To tackle this diversity, our recommended guidelines are designed to accommodate various model types, emerging methodologies, and the growing utilization of advanced statistical techniques to address uncertainties and the urgent need for model validation.
Research recommendations
Based on these findings, several research recommendations emerge. First, as the size of the health workforce continues to grow and health workforce projection and forecasting models become increasingly complex, there is a strong need to adopt standardized reporting criteria for health workforce projection models. A common reporting framework can be a catalyst for transparency and model quality.
Secondly, our findings reveal a growing trend in aligning health workforce projection models with underlying health needs and considering the implications of different health service delivery models. It is essential to continue developing methodologies for needs-based, multi-professional, skill-mixed models, particularly considering recent trends such as an aging population, an increased prevalence of chronic diseases, and patients with multiple conditions. As patients increasingly require patient-centred care delivered by a multi-professional team, there is a methodological challenge in effectively modelling team-based care [59, 60]. This shift away from profession-specific approaches in favour of a more team-oriented approach is necessary to address the evolving workforce requirements in healthcare.
Our study revealed a need for more research that addresses the mal-distribution of the health workforce across different geographical areas. To address this issue, it is crucial to develop methodologies for assessing geographical distribution and examining the relative over-service or under-service of health professionals [61]. While financial resources are crucial for health workforce planning implementation, existing literature suggests that many current models neglect budgetary analyses. Among the few studies that include budgetary analysis, none considered the potential cost offsets resulting from improved health outcomes [62]. Explicitly integrating financial and budgetary analysis into health workforce projection models, rather than treating it as an add-on, is highly desirable.
Our study focuses on specific professions like GPs, nurses, and dentists in health workforce planning. This narrow focus on only a few health professionals may be attributed to the lack of data on other professionals, such as allied health and aged care workers. To enhance workforce planning, it is crucial to improve data collection for these occupations. Data collection should also consider contemporary work patterns, where health professionals may work part-time and allocate varying proportions of their time to clinical practice. Additionally, data on the mobility and behaviour of health professionals, including their movement across geographical areas, will significantly enhance the accuracy of simulation models.
Finally, our study revealed that existing research predominantly relies on static system frameworks rather than dynamic analyses of the interconnected ‘systems’ inherent in health workforce planning. Existing models have been largely linear, instead of systems-based, regarding their methodologies [49]. It is imperative for researchers to shift towards a complex system-thinking approach within health workforce projection models, departing from static models. This shift involves comprehending the dynamic and interrelated nature of healthcare systems and considering the potential existence of feedback loops under different scenarios. This holistic perspective is essential for a more comprehensive understanding of workforce planning dynamics.
Limitations
This paper has a few caveats. Firstly, it focuses on studies that project both health workforce demand and supply while calculating the demand–supply gap. This exclusion applies to research that exclusively addresses either the demand or supply of the health workforce, as well as cross-sectional studies. Secondly, the review only includes studies published after 2010, potentially missing older studies. Nevertheless, this approach was chosen to encompass the representation of recent developments in the field and highlight their significance and innovation.
Conclusion
Health workforce projection models are complex analyses of various interconnected systems of demand for and supply of health workforce, as well as the resources required to meet the demand–supply gap. Our study underscores the importance of dynamic, multi-professional, and fine-tuned demand, supply, and budget impact analyses, supported by robust health workforce data intelligence. The suggested best-practice reporting guidelines aim to promote transparency in health workforce projection models and provide valuable support to healthcare practitioners and researchers.
Availability of data and materials
Not applicable.
References
World Health Organization. Working together for health: the World Health Report. Geneva: WHO; 2006.
Crettenden I, Poz MD, Buchan J. Right time, right place: improving access to health service through effective retention and distribution of health workers. Hum Resour Health. 2013;11:60.
Lopes MA, Almeida ÁS, Almada-Lobo B. Handling healthcare workforce planning with care: where do we stand? Hum Resour Health. 2015;13(1):38.
Ahmed SM, Hossain MA, RajaChowdhury AM, Bhuiya AU. The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health. 2011;9(1):3.
Dussault G, Franceschini MC. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health. 2006;4(1):12.
Kroezen M, Van Hoegaerden M, Batenburg R. The joint action on health workforce planning and forecasting: results of a European programme to improve health workforce policies. Health Policy. 2018;122(2):87–93.
Organization WH. Health workforce and labor market dynamics in OECD high-income countries: a synthesis of recent analyses and simulations of future supply and requirements. 2017.
Liu JX, Goryakin Y, Maeda A, Bruckner T, Scheffler R. Global health workforce labor market projections for 2030. Hum Resour Health. 2017;15(1):11.
Nation U. The sustainable development goals report 2023: special edition, towards a rescue plan for people and planet; 2023.
Dower C, Moore J, Langelier M. It is time to restructure health professions scope-of-practice regulations to remove barriers to care. Health Aff. 2013;32(11):1971–6.
Dubois C-A, Singh D. From staff-mix to skill-mix and beyond: towards a systemic approach to health workforce management. Hum Resour Health. 2009;7(1):87.
Asamani JA, Christmals CD, Reitsma GM. The needs-based health workforce planning method: a systematic scoping review of analytical applications. Health Policy Plan. 2021;36(8):1325–43.
Birch S, Ahern S, Brocklehurst P, et al. Planning the oral health workforce: time for innovation. Community Dent Oral Epidemiol. 2021;49(1):17–22.
Schofield D, Callander E, Kimman M, Scuteri J, Fodero L. Projecting the radiation oncology workforce in Australia. Asian Pac J Cancer Prev. 2012;13(4):1159–66.
Laurence CO, Karnon J. Improving the planning of the GP workforce in Australia: a simulation model incorporating work transitions, health need and service usage. Hum Resour Health. 2016;14:13.
Laurence CO, Heywood T, Bell J, Atkinson K, Karnon J. The never ending road: improving, adapting and refining a needs-based model to estimate future general practitioner requirements in two Australian states. Fam Pract. 2018;35(2):193–8.
Tomblin Murphy G, Birch S, MacKenzie A, Alder R, Lethbridge L, Little L. Eliminating the shortage of registered nurses in Canada: an exercise in applied needs-based planning. Health Policy. 2012;105(2–3):192–202.
Vanderby SA, Carter MW, Latham T, Feindel C. Modelling the future of the Canadian cardiac surgery workforce using system dynamics. J Oper Res Soc. 2014;65(9):1325–35.
Yip SM, Loewen SK, Li H, Hao D, Easaw JC. Management of medical oncology services in Canada: redefined workload with a novel supply-and-demand workforce projection model. J Oncol Pract. 2018;14(7):e438–45.
MacKenzie A, Tomblin Murphy G, Audas R. A dynamic, multi-professional, needs-based simulation model to inform human resources for health planning. Hum Resour Health. 2019;17(1):42.
Taghavi M, Johnston G, Urquhart R, Henderson D, Tschupruk C, Tupala B. Workforce planning for community-based palliative care specialist teams using operations research. J Pain Symptom Manag. 2021;61(5):1012-22.e4.
Dass AR, Deber R, Laporte A. Forecasting staffing needs for Ontario’s long-term care sector. Healthc Policy. 2022;17(Sp):91–106.
Jäger R, van den Berg N, Hoffmann W, Jordan RA, Schwendicke F. Estimating future dental services’ demand and supply: a model for Northern Germany. Community Dent Oral Epidemiol. 2016;44(2):169–79.
Asamani JA, Christmals CD, Reitsma GM. Advancing the population needs-based health workforce planning methodology: a simulation tool for country application. Int J Environ Res Public Health. 2021;18(4):2113.
Asamani JA, Christmals CD, Reitsma GM. Modelling the supply and need for health professionals for primary health care in Ghana: implications for health professions education and employment planning. PLoS ONE. 2021;16(9): e0257957.
Jansen C, Codjia L, Cometto G, Yansané ML, Dieleman M. Realizing universal health coverage for maternal health services in the Republic of Guinea: the use of workforce projections to design health labor market interventions. Risk Manag Healthc Policy. 2014;7:219–32.
Ahern S, Woods N, Kalmus O, Birch S, Listl S. Needs-based planning for the oral health workforce—development and application of a simulation model. Hum Resour Health. 2019;17(1):55.
Murphy GT, MacKenzie A, Guy-Walker J, Walker C. Needs-based human resources for health planning in Jamaica: using simulation modelling to inform policy options for pharmacists in the public sector. Hum Resour Health. 2014;12(1):1–11.
Ishikawa T, Ohba H, Yokooka Y, Nakamura K, Ogasawara K. Forecasting the absolute and relative shortage of physicians in Japan using a system dynamics model approach. Hum Resour Health. 2013;11(1):41.
Koichubekov B, Kharin A, Sorokina M, Korshukov I, Omarkulov B. System dynamics modeling for general practitioner workforce forecasting in Kazakhstan. Ann Ig. 2021;33(3):242–53.
Oh Y. The future prospects of supply and demand for urologists in Korea. Investig Clin Urol. 2017;58(6):400–8.
Asamani JA, Zurn P, Pitso P, et al. Health workforce supply, needs and financial feasibility in Lesotho: a labour market analysis. BMJ Glob Health. 2022;7(Suppl 1): e008420.
Berman L, Prust ML, Maungena Mononga A, et al. Using modeling and scenario analysis to support evidence-based health workforce strategic planning in Malawi. Hum Resour Health. 2022;20(1):34.
Ranta A, Tiwari P, Mottershead J, et al. New Zealand’s neurologist workforce: a pragmatic analysis of demand, supply and future projections. N Z Med J. 2015;128(1419):35–44.
Dunn A, Costello S, Imlach F, et al. Using national data to model the New Zealand radiation oncology workforce. J Med Imaging Radiat Oncol. 2022;66(5):708–16.
Lopes MA, Almeida ÁS, Almada-Lobo B. Forecasting the medical workforce: a stochastic agent-based simulation approach. Health Care Manag Sci. 2018;21(1):52–75.
Al-Senani F, Salawati M, AlJohani M, Cuche M, Seguel Ravest V, Eggington S. Workforce requirements for comprehensive ischaemic stroke care in a developing country: the case of Saudi Arabia. Hum Resour Health. 2019;17(1):90.
Santric Milicevic M, Vasic M, Edwards M, Sanchez C, Fellows J. Strengthening the public health workforce: an estimation of the long-term requirements for public health specialists in Serbia. Health Policy. 2018;122(6):674–80.
Ansah JP, De Korne D, Bayer S, et al. Future requirements for and supply of ophthalmologists for an aging population in Singapore. Hum Resour Health. 2015;13:86.
Ansah JP, Koh V, De Korne D, Jayabaskar T, Matchar DB, Quek D. Modeling manpower requirement for a changing population health needs: the case of ophthalmic nurses and allied health ophthalmic professionals. Health Policy Technol. 2019;8(3):282–95.
Barber P, López-Valcárcel BG. Forecasting the need for medical specialists in Spain: application of a system dynamics model. Hum Resour Health. 2010;8(1):24.
Thongsukdee P, Weerawat W. Physician workforce planning and allocation model using agent-based modeling: a case study in Thailand. Int J Health Plan Manag. 2020;35(6):1384–97.
Leerapan B, Teekasap P, Urwannachotima N, et al. System dynamics modelling of health workforce planning to address future challenges of Thailand’s universal health coverage. Hum Resour Health. 2021;19(1):31.
Pagaiya N, Phanthunane P, Bamrung A, Noree T, Kongweerakul K. Forecasting imbalances of human resources for health in the Thailand health service system: application of a health demand method. Hum Resour Health. 2019;17(1):4.
Gallagher JE, Kleinman ER, Harper PR. Modelling workforce skill-mix: how can dental professionals meet the needs and demands of older people in England? Br Dent J. 2010;208(3):E6.
Gallagher JE, Lim Z, Harper PR. Workforce skill mix: modelling the potential for dental therapists in state-funded primary dental care. Int Dent J. 2013;63(2):57–64.
Lupu D, Quigley L, Mehfoud N, Salsberg ES. The growing demand for hospice and palliative medicine physicians: will the supply keep up? J Pain Symptom Manag. 2018;55(4):1216–23.
Chen C, Luo Q, Chong N, et al. Coronavirus disease 2019 planning and response: a tale of 2 health workforce estimator tools. Med Care. 2021;59(Suppl 5):S420–7.
Dill MJ, Hirsch GB. The Association of American Medical Colleges’ local area physician workforce modeling project. Acad Med. 2021;96(10):1393–400.
Correll CK, Ditmyer MM, Mehta J, et al. 2015 American college of rheumatology workforce study and demand projections of pediatric rheumatology workforce, 2015–2030. Arthritis Care Res. 2022;74(3):340–8.
Russo MW, Fix OK, Koteish AA, et al. Modeling the hepatology workforce in the United States: a predicted critical shortage. Hepatology. 2020;72(4):1444–54.
Landry MD, Hack LM, Coulson E, et al. Workforce projections 2010–2020: annual supply and demand forecasting models for physical therapists across the United States. Phys Ther. 2016;96(1):71–80.
Tomblin Murphy G, Birch S, MacKenzie A, Rigby J. Simulating future supply of and requirements for human resources for health in high-income OECD countries. Hum Resour Health. 2016;14(1):77.
Safarishahrbijari A. Workforce forecasting models: a systematic review. J Forecast. 2018;37(7):739–53.
Health Resources & Services Administration. Technical documentation for HRSA’s health workforce simulation model. 2023.
Ansah JP, De Korne D, Bayer S, et al. Future requirements for and supply of ophthalmologists for an aging population in Singapore. Hum Resour Health. 2015;13(1):86.
Parsons D. Medical-workforce planning: an art or science? Hum Resour Manag Int Dig. 2010;18(5):36–8.
Ono T, Lafortune G, Schoenstein M. Health workforce planning in OECD countries. 2013.
Segal L, Guy S, Leach M, Groves A, Turnbull C, Furber G. A needs-based workforce model to deliver tertiary-level community mental health care for distressed infants, children, and adolescents in South Australia: a mixed-methods study. Lancet Public Health. 2018;3(6):e296–303.
Segal L, Leach MJ, May E, Turnbull C. Regional primary care team to deliver best-practice diabetes care: a needs-driven health workforce model reflecting a biopsychosocial construct of health. Diabetes Care. 2013;36(7):1898–907.
Birch S, Tomblin Murphy G, MacKenzie A, Whittaker W, Mason T. Will the need-based planning of health human resources currently undertaken in several countries lead to excess supply and inefficiency? A comment on Basu and Pak. Health Econ. 2017;26(6):818–21.
Moretti C. Financial and cost benefit implications of the recommendations of the national aged care staffing and skills mix final report. Adelaide: Australian Industrial Transformation Institute, Flinders University of South Australia; 2017.
Ishikawa T, Ohba H, Yokooka Y, Nakamura K, Ogasawara K. Forecasting the absolute and relative shortage of physicians in Japan using a system dynamics model approach. Hum Resour Health. 2013;11:41.
Vanderby SA, Carter MW, Latham T, et al. Modeling the cardiac surgery workforce in Canada. Ann Thorac Surg. 2010;90(2):467–73.
Tomblin Murphy G, MacKenzie A, Guy-Walker J, Walker C. Needs-based human resources for health planning in Jamaica: using simulation modelling to inform policy options for pharmacists in the public sector. Hum Resour Health. 2014;12:67.
Laurence CO, Karnon J. Improving the planning of the GP workforce in Australia: a simulation model incorporating work transitions, health need and service usage. Hum Resour Health. 2016;14:1–14.
Pagaiya N, Phanthunane P, Bamrung A, Noree T, Kongweerakul K. Forecasting imbalances of human resources for health in the Thailand health service system: application of a health demand method. Hum Resour Health. 2019;17(1):1–12.
Funding
The National Centre for Health Workforce Studies and the Health Data Analytics Team at the Australian National University are supported by the Transform funding initiative at the College of Health and Medicine, Australian National University. John Tayu Lee is supported by the Yushan Fellow Program by the Ministry of Education in Taiwan.
Author information
Authors and Affiliations
Contributions
Conception and design: JTL. Analysis: JTL, MT. Interpretation of the data: JTL, IC. Manuscript writing: JTL, MT. All authors contributed to the development of the checklist, and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Characteristics of the included studies. Table S2. Strength and limitation of health workforce analytical framework. Table S3. Model validation and uncertainty. Table S4. Policy and scenario analysis of the included studies. Figure S1. Schematic diagram of a needs-based health workforce planning model.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, J.T., Crettenden, I., Tran, M. et al. Methods for health workforce projection model: systematic review and recommended good practice reporting guideline. Hum Resour Health 22, 25 (2024). https://doi.org/10.1186/s12960-024-00895-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-024-00895-z