Abstract
Background
About 13–25% of cerebral venous thrombosis (CVT) cases lack clear etiology, which may be associated with underlying genetic factors. This study aims to investigate genetic factors in CVT patients using whole exome sequencing (WES).
Methods
Thirty-eight CVT patients hospitalized underwent WES. 977 subjects with WES data from a community cohort study --the Shunyi cohort were as the control group. Using bioinformatics analysis, differential genes with rare damaging variants between two groups were filtered (P < 0.05). KEGG enrichment analysis was performed on the screened genes to identify pathways associated with CVT.
Results
Through analysis of medical history, routine tests, and imaging examinations, the etiology of 38 patients: 8 cases of antiphospholipid syndrome, 6 cases with hematologic diseases, 3 cases of protein C deficiency, and 2 cases of protein S deficiency. Five cases occurred during pregnancy or puerperium, and 3 cases had a history of oral contraceptive use, and so on. The etiology was unknown in 12 cases (31.6%), and the etiology of 4 patients were further clarified through WES: F9 c.838 + 1_838 + 16del, Hemizygote: F9 EX1-EX7 Dup; CBS c.430G > A, CBS c.949 A > G; F2 c.1787G > A; SERPINC1 c.409-11G > T. Comparing the WES data of two groups, a total of 179 different genes with rare damaging variants were screened (P < 0.05), with 5 genes of interest (JAK2, C3, PROC, PROZ, SERPIND1). Enrichment analysis of the 179 different genes revealed the complement and coagulation pathway and the mitogen activated protein kinases (MAPK) pathway were associated with CVT.
Conclusion
For CVT patients with unknown etiology, WES could help identify the cause of CVT early, which is of great significance for treatment decisions and prognosis. In addition to the complement and coagulation pathway, MAPK pathway is associated with CVT, potentially related to platelet regulation and inflammatory response.
Similar content being viewed by others
Introduction
Cerebral venous thrombosis (CVT) is a special type of cerebrovascular disease that results from impaired blood flow or cerebrospinal fluid circulation, leading to intracranial hypertension and focal brain damage. The incidence of CVT is approximately 5 per million, accounting for approximately 0.5-3% of cerebrovascular diseases [1, 2].
The pathogenesis of CVT remains incompletely elucidated, intricately linked with diverse risk factors categorized as transient or permanent. Transient risk factors including gender-specific factors like oral contraceptives, pregnancy, puerperium, and hormone replacement therapy, alongside procedural factors such as lumbar punctures and neurosurgical interventions. Additionally, cranial or cervical infections, anemia, and dehydration contribute to transient ones. On the other hand, permanent risk factors involve genetic predispositions to thrombosis, notably prothrombin G20210A mutation, Factor V Leiden mutation (FVL), deficiencies in proteins C (PC), protein S (PS), and antithrombin (AT), Janus Kinase-2 V617F mutation (JAK2 V617F), and MTHFR (C677T) polymorphism [3]. Furthermore, systemic diseases including autoimmune diseases, neoplasms, and myeloproliferative disorders, arteriovenous fistulas, and obesity constitute permanent ones. Hereditary thrombophilia notably contributes to CVT risk, accounting for approximately 34-41% of cases [1, 4]. CVT patients with hereditary thrombophilia may necessitate prolonged or lifelong anticoagulation post-acute phase management.
In addition to the well-established hereditary thrombophilia mentioned above, retrospective case-control investigations have revealed other genetic predispositions to thrombosis such as LDLR mutation, protein Z (G79A), plasma glutathione peroxidase (GPx-3) gene promoter, and XII factor (C46T) gene polymorphisms [5,6,7,8]. However, these studies, predominantly relied on candidate genes, which hindered the discovery of new risk genes. Moreover, 13–25% of CVT cases still lack clear risk factors or etiologies, possibly related to underlying undetermined genetic factors [9]. Addressing this gap, the International Stroke Genetics Consortium (ISGC) has been conducting global multicenter studies towards the genetic basis of CVT (the BEAST Consortium) [9]. Given the racial and regional disparities in hereditary factors associated with CVT [4, 10], it is necessary to investigate genetic risk factors among Chinese CVT patients.
Genome-Wide Association Studies (GWAS) focus on common variations. Compared to rare variations, common variations often have smaller effects and are difficult to map to causal genes. Protein-coding genes constitute only approximately 1% of the human genome but harbor 85% of the mutations with significant impacts on disease-related traits [11]. Therefore, selectively sequencing the complete coding regions (i.e., “whole exome”) may potentially contribute to understanding both rare and common human diseases. Whole exome sequencing (WES) enables the study of associations between rare pathogenic and susceptible genetic variations and complex diseases. This study aims to investigate genetic factors in CVT patients using WES in a comprehensive hospital in China.
Methods
Study design and patient selection
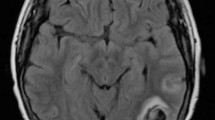
From June 2017 to June 2023, 38 inpatients diagnosed with CVT were prospectively enrolled consecutively at the Department of Neurology, Peking Union Medical College Hospital (PUMCH). In the study, CVT was diagnosed according to established criteria and confirmed by at least one of the following neuroradiological examinations: computed tomography venography (CTV), magnetic resonance imaging (MRI), magnetic resonance venography (MRV), or digital subtraction angiography (DSA) [12]. Demographic characteristics, medical history, clinical manifestations, laboratory tests, imaging data (CT, MRI, MRV, DSA), and treatment were collected. Laboratory results including thrombophilia tests such as PC, PS, ATIII and activated PC resistance (APC-R), antiphospholipid antibodies (aPL) such as anticardiolipin antibodies (aCL), anti-β2-glycoprotein I antibodies (aB2GPI), lupus anticoagulant, and antinuclear antibodies, and homocysteine. All 38 patients signed informed consent forms for enrollment, and whole blood samples were collected for WES. Severity of illness at admission and discharge was assessed by modified Rankin Scale (mRS) [13].
All controls were recruited from the Shunyi Study, an ongoing prospective population-based cohort aimed at exploring the risk factors and consequences of brain changes in Chinese community-dwelling adults. A detailed recruitment procedure has been previously published [14]. Briefly, all residents aged 35 and above, living independently in five villages in Shunyi, a suburb northeast of Beijing, were invited to participate between June 2013 and April 2016 and a total of 1586 individuals participated in the study. The control group consisted of 977 participants, who had no history of stroke or dementia, and their blood samples were collected for WES.
The study was approved by the local hospital Ethics Committee (JS-2420). Written and informed consent was obtained from all participants.
Whole exome sequencing
Patients: Blood samples of 38 patients were subjected to high depth WES performed at BGI Genomics Co., Ltd. Genomic DNA was extracted from the blood samples (MagPure Buffy Coat DNA Midi KF Kit, MAGEN). Firstly, the genomic DNA was broken into 100–500 bp fragments by enzyme kit (Shearing Enzyme premix reagent, ENZYMATICS), then the 200–300 bp fragments were collected by magnetic bead (Vahtstm DNA Clean Beads, VAZYME) and prepared into libraries. Subsequently, the KAPA Hyper Exome, ROCHE was employed to capture and enrich the DNA of target gene exons and adjacent splice regions. Finally, mutation detection was conducted using the MGISEQ-2000 sequencing platform. Quality control metrics for sequencing data included: average sequencing depth of the target region ≥ 180X, with over 95% of the sites in the target region having an average depth > 20X.
Data Analysis: The “clean reads” (with a length of 90 bp) derived from targeted sequencing and filtering were then aligned to the human genome reference (hg19) using the BWA (Burrows Wheeler Aligner) Multi-Vision software package [15]. After alignment, the output files were used to perform sequencing coverage and depth analysis of the target region, single-nucleotide variants (SNVs) and INDEL calling. We used GATK software [16] to detect SNVs and indels. All SNVs and indels were filtered and estimated via multiple databases, including NCBI dbSNP, HapMap, 1000 human genome dataset and database of 100 Chinese healthy adults. To predict the effect of missense variants, we used dbNSFP [17] which contains seven well-established in silico prediction programs (Scale-Invariant Feature Transform (SIFT), Polyphen2, LRT, Mutation Taster, and PhyloP). Pathogenic variants were assessed under the protocol issued by ACMG [18]. The Human Gene Mutation Database (HGMD) was used to screen mutations reported in published studies.
Controls: DNA samples of 977 participants were subjected to high depth WES performed at Novogene Corporation (Beijing, China). Detailed recruitment procedure has been previously published [14].
Variant annotation and definition of rare damaging variants
Variants were further annotated by Variant Effect Predictor (VEP, v105) and the LOFTEE plugin. LOFTEE applies a range of filters on variants annotated as stop-gained, splice site, and frameshift variants to remove those that are unlikely to be disruptive. Those variants labeled as “high-confidence” by LOFTEE were retained. Besides, variants annotated as missense variants were then filtered by (1) CADD score > = 20, or (2) SIFT4G score < 0.05, or (3) PolyPhen-2 score > 0.8. Variants were classified as probably deleterious if they were satisfied criteria in at least 2 software tools. Rare variants were defined using a minor allele frequency (MAF) threshold of 0.1% in all gnomAD database, gnomAD exome database and ExAC East Asian.
Screen out rare damaging variants in the WES data of the case and the control group from a total of 16,317 genes. The number of individuals with rare damaging variants in each gene in the case and control groups was obtained.
Statistical analysis
Descriptive analyses were conducted for the patients’ characteristics, represented as mean (standard deviation) for continuous variables and frequency (%) for categorical variables. The differences in rare damaging variants between CVT patients and the control group were compared using the Chi-square test. Statistical significance was defined as two-tailed P<0.05, unless otherwise specified. Statistical analyses described above were performed using SPSS, version 23.0. To explore the potential function of target genes, Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis was performed using GeneCodis (http://genecodis.genyo.es/?tdsourcetag=s_pcqq_aiomsg). The cut-off value for significance was P<0.05.
Results
Characteristics of the CVT patients
Table 1 presented the demographic, clinical, and imaging characteristics of 38 CVT patients. The average age was 39.61 ± 17.20 years, with 20 females and 18 males. Headache was the most common symptom (76.3%), followed by visual disturbances (34.2%), focal neurological deficits (34.2%), altered consciousness (31.6%), seizures (21.1%), and cognitive impairment (21.1%). Tinnitus and abnormal mental behavior were also reported by some patients. The most frequently involved venous sinus was the transverse sinus (57.9%), followed by the sigmoid sinus (55.3%) and the superior sagittal sinus (42.1%). Cortical vein thrombosis was observed in nine patients (23.7%). Additionally, 6 patients (18.4%) had cerebral deep venous thrombosis involving Gallen vein or internal cerebral veins. Approximately 70% of patients had multiple venous sinuses involvement. Eighteen patients presented with hemorrhage, and 21 patients presented with brain swelling and focal edema. Except for 2 patients who died and 1 patient whose condition remained poor, 92.1% of the patient’s showed improvement at discharge. The median mRS at admission was 2, whereas the median mRS at discharge was 1.
Summarized the classification of risk factors and etiology for 38 cases by analyzing medical history, routine clinical tests, and imaging examinations (Table 2). Among them, 8 patients were diagnosed with antiphospholipid antibody syndrome (APS) (21.1%). Six patients presented concomitant hematologic disorders (15.8%), including thrombocytosis, myelodysplastic syndrome, paroxysmal nocturnal hemoglobinuria (PNH), aplastic anemia, and iron deficiency anemia. Three patients had protein C deficiency, while two others had protein S deficiency. Among the 20 female patients, 5 suffered from CVT during pregnancy or puerperium (25.0%), and 3 had a history of oral contraceptive use (15.0%). In addition, one patient was diagnosed with cystathionine beta-synthase deficiency, another with hypertrophic duraitis, one with concomitant choriocarcinoma, and one with intracranial infection. Eleven patients were found to have hyperhomocysteinemia (hhcy) (30.6%). Nonetheless, the etiology remained unclear in 12 patients (31.6%).
Notably, all 8 patients suspected APS during hospitalization underwent follow-up and obtained repetition of serology at least 12 weeks apart, confirming the diagnosis of APS, with one patient being seronegative APS. Among the 5 patients with PC deficiency or PS deficiency, except for one patient who did not undergo follow-up examinations (Table 3, P1), the remaining 4 patients (Table 3, P 2–5) all underwent follow-up examinations during the non-acute phase, and the results remained abnormal.
The of etiology for 38 patients combined whole exome sequencing analysis
WES was performed on 38 patients. The primary focus was on gene mutations linked to well-established hereditary thrombophilia, including F2 (prothrombin G20210A mutation), F5 (FVL mutation), PROC mutation, PROS1 mutation, SERPINC1 mutation, JAK2 V617F, and MTHFR (C677T) polymorphism, along with gene mutations associated with the primary diseases or comorbidities. The specific conditions of each CVT patient were detailed in Table 3.
As shown in Table 3, two patients clinically presenting with protein S deficiency were found to have mutations in the PROS1 gene (P1, P5), and P5 suffered from CVT during puerperium. Three patients clinically presenting with protein C deficiency were found to have mutations in the PROC gene (P2, P3, P4). Among them, P3 also had a personal history of oral contraceptive use, and P4 suffered from CVT during pregnancy. For the five patients whose onset occurred during pregnancy or the puerperium, all had additional risk factors or causes. Among them, the two patients with low PS level or PC level both underwent follow-up examinations (P4, P5), and the results were still abnormal (PS 28%→47% (normal range 76–135%); PC 38%→35% (normal range 70–140%)), which were consistent with the gene mutations identified by WES. Except for the two combined hereditary protein S deficiency or hereditary protein C deficiency, the other three patients were diagnosed with APS (P6, P7, P8). P6 also carried a compound heterozygous mutation in the F8 gene. Two patients with combined thrombocytosis were found to have the JAK2 V617F mutation (P15, P16). One patient with PNH was identified with pathogenic mutations in the HBB and PIGA genes through WES (P17). P20 had significantly elevated F9 activity and WES revealed a duplication mutation in the exons of the F9 gene on the X chromosome. In P28, WES also identified a duplication mutation of the F9 gene, along with a deletion mutation; however, FIX activity was not detected in this patient. P35 had a family history of thrombosis (his father suffered from pulmonary embolism), and WES identified a mutation in F2 gene, which was assessed as pathogenic. A total of 12 patients were found to have hhcy, with one patient presenting markedly elevated level of homocysteine (> 250 umol/L) (P33). WES revealed compound heterozygous mutations in the CBS gene in this patient, which can lead to cystathionine beta-synthase deficiency, further predisposing to CVT. Among the remaining 11 patients with hhcy, 5 patients had the MTHFR (TT) polymorphism. Among 12 patients with unclear etiology, the causative etiology of 4 cases was further clarified through the mutation detected by WES. Thirteen patients had multiple risk factors (34.2%).
Differential genes and underlying pathways associated with CVT from case-control study
Drawing from published literature, and genes potentially associated with CVT, such as genes possibly related to APS, we assembled a list of genes of interest (see Supplementary Table 2). To further investigate genes potentially associated with CVT, rare damaging variants with differences between the case and control groups were filtered. A total of 179 genes were screened (see Supplementary Table 3), with 5 genes was in the list of genes of interest (JAK2, C3, PROC, PROZ, and SERPIND1 gene) (Table 4). Enrichment analysis of different 179 genes was conducted using KEGG. Some pathways were obtained and the results are shown in Fig. 1. Among them, the complement and coagulation cascades (involving genes C3, PROC, SERPIND1), and the mitogen activated protein kinases (MAPK) pathway (involving genes FLNB, CACNA1D, TAOK2, CACNB1, FLT4, NR4A) were associated with CVT. Further localization of the genes involved in the MAPK pathway revealed their primary impacts on the specific positions within the MAPK pathway (Fig. 2). Fifteen CVT patients (39.5%) were found to have rare damaging variants in six genes linked to the MAPK pathway, of which two patients lacked identifiable etiology for CVT, while the remaining thirteen patients had known causes or risk factors.
Discussion
We found that with only medical history, routine laboratory tests, and imaging data, the underlying cause of approximately 30% of CVT patients remained unknown. WES could help identify the cause of CVT early and timely, particularly for patients with unknown cause. By comparing WES data between CVT patients and controls, we identified five genes of interest (JAK2, C3, PROC, PROZ, and SERPIND1 gene) associated with CVT. Enrichment analysis revealed that beyond the complement and coagulation pathway, the MAPK pathway is related to CVT.
Through analyzing the medical history, routine laboratory tests, and imaging examinations of the CVT patients, we summarized the risk factors and etiology. Our findings revealed that autoimmune diseases constituted significant risk factors for CVT, accounting for approximately 21.1% of the CVT patients. A previous study at our hospital identified autoimmune diseases as the predominant cause of CVT cases among women of childbearing age, representing approximately 27.8% [19]. Studies indicated that autoimmune diseases, including Behçet’s syndrome, systemic lupus erythematosus, APS, and Sjögren’s syndrome, were important causes of CVT [20, 21]. In our study, all patients with autoimmune diseases were diagnosed with APS, and 75% of them were female. The mechanism of APS inducing CVT may be theorized that aPL instigate a prothrombotic state by activating endothelial cells, platelets, and monocytes. Furthermore, aB2GPI and complement activation play crucial roles in thrombosis [20, 21]. Additionally, hematologic disorders are important risk factors for CVT. Previous study has reported an association between anemia and CVT [22]. Furthermore, myeloproliferative neoplasms, thrombocytosis, and PNH could also lead to CVT [23,24,25]. Gender-specific risk factors such as pregnancy, puerperium and oral contraceptive use are important risk factors of CVT [4]. In our study, among 20 female patients, 5 patients suffered from CVT during pregnancy or puerperium, with 3 cases having a history of oral contraceptive use. It is noteworthy that all five pregnancy-related patients had additional risk factors and etiologies, such as APS, PS deficiency, and PC deficiency. This suggested that although pregnancy-induced hypercoagulability increases the risk of CVT, attributing the etiology of CVT solely to pregnancy is overly simplistic and screening for other risk factors should not be overlooked.
Although the etiology of the majority of CVT patients can be clarified through medical history, routine tests, and imaging data, approximately 30% of patients still have unknown causes. The causative etiology of 4 cases was further clarified by WES. WES revealed a duplication and deletion mutation in the F9 gene of patient 28. Patient 20 had similar F9 gene duplication mutation, yet had significantly elevated FIX activity, leading to CVT as detailed in a published article [26]. Additionally, a Turkish study emphasized that F9 gene duplication mutation and increased FIX activity can lead to unique thrombophilia, ultimately resulting in CVT [27]. Patient 33 displayed markedly elevated homocysteine level, and subsequent examinations showed elevated blood methionine levels (approximately double the upper limit of normal) alongside normal urinary methylmalonic acid level. This patient presented bilateral ectopia lentis and a Marfan syndrome-like appearance. Finally, WES identified compound heterozygous mutations in the CBS gene, confirming the diagnosis of cystathionine beta synthase deficiency caused by CBS mutations. The instance of CVT resulting from CBS mutations had been reported [28]. WES identified a mutation in F2 gene in patient 35 (F2 c.1787G > A, Prothrombin Belgrade mutation), which mutation had been confirmed as a pathogenic mutation causing antithrombin resistance [29]. In addition to acute-phase treatments like anticoagulation, dehydration, and life support, patients 33 also received various B-complex vitamins, especially pyridoxine for the primary disease [30]. All four patients underwent long-term anticoagulant therapy and subsequent follow-up showed stable conditions. This further emphasized that for patients with an unknown etiology, WES may assist in promptly identifying the causes of CVT, which could to some extent aid in treatment decision-making and improve patient prognosis. One point to note, in addition to PROC gene mutations, circulating levels of PC may be reduced in several conditions, such as DIC, infection, uremia, cancer or cancer therapy and some autoantibodies [31]. Therefore, in diagnosing hereditary PC deficiency, it is necessary to first rule out the acquired factors. Of course, functional assays of PC take precedence over WES. If several times of functional tests of PC consistently show significant abnormality, validation through WES could be pursued. PS deficiency is similar. Noteworthily, 34.2% patients had multiple risk factors, including genetic and clinical risk factors, and these factors synergistically contributed to the occurrence of CVT. The authors suggest that genetic risk factors may predispose to a potential prothrombotic state leading to CVT, and when combined with certain clinical triggers such as pregnancy or puerperium, oral contraceptives, dehydration, hyperhomocysteinemia, and so on, multiple factors can synergistically reach the threshold for thrombosis.
By screening for rare damaging variants in case and control groups, we identified that the genes JAK2, PROC, PROZ, SERPIND1, and C3 are associated with CVT in the gene of interest. The JAK2 gene, particularly JAK2 V617F mutation, was associated with myeloproliferative neoplasms [32]. Mutations in the PROC gene leading to protein C deficiency, as well as those in the JAK2 gene, had been shown to be specifically associated with CVT [3]. Protein Z is a plasma protein dependent on vitamin K, acting as a cofactor for the protein Z-dependent protease inhibitor to deactivate activated factor X, thereby playing a role in coagulation inhibition. Research on the relationship between the PROZ (G79A) polymorphism and CVT had yielded inconsistent results [5, 33]. Furthermore, the above-mentioned articles were limited to small-sample case-control studies, focusing solely on the polymorphism of the PROZ gene not rare damaging variants of PROZ. SERPIND1 (heparin cofactor II) is a serine protease inhibitor that selectively inactivates thrombin without affecting other proteases involved in the blood coagulation cascade. A previous study indicated an association between mutations in the SERPIND1 gene and venous thromboembolism [34], yet there is currently no study about SERPIND1 gene and CVT. Evidences had indicated interactions between the hemostatic system and innate immunity, and the coagulation and complement cascades. Complement factors make distinct contributions to platelet activation and fibrin deposition. Deficiency in C3 leads to prolonged bleeding time, with C3 playing a specific role in platelet activation [35]. However, there is currently very limited research on the complement and thrombosis, with no studies regarding the association between C3 with CVT. Our study confirmed the well-established genes such as PROC and JAK2, while also proposing the less-studied genes PROZ, SERPIND1, and C3, thus offering direction and insights for future research.
Enrichment analysis revealed that the complement and coagulation pathway was associated with CVT, which had been well-established. Notably, to the best of our knowledge, our study firstly reported a possible association between the MAPK pathway and CVT. In our study, fifteen CVT patients had rare damaging variants in six genes related to the MAPK pathway. Among them, two patients had no identified cause for CVT, while the other thirteen had known causes or risk factors. This indicated that changes in the MAPK pathway could serve as a potential etiology in certain patients with unexplained CVT, even after excluding known possible causes, and may synergistically contribute to the pathogenesis of CVT in patients with specific etiologies. MAPK is a part of the protein kinase cascade, with three identified families: C-Jun N-terminal kinase (JNK), p38 MAPK, and extracellular signal-regulated kinase (ERK). Each cascade requires at least three enzymes for activation: MAPKK kinase, MAPK kinase, and then to MAPK [36]. Dysregulation of MAPK signaling often leads to cancer, diabetes, and other diseases associated with immune response or inflammation. A few articles also emphasized the role of the MAPK pathway in regulating platelet function and thrombosis. Activation of ERK in platelets is crucial for collagen-induced platelet secretion and aggregation [37], and inhibition of its upstream MEK1/2 can suppress ERK activation and prolong occlusion time of arterial and venous thrombosis in mice [38]. Additionally, activation of p38 in collagen-stimulated platelets leads to increased platelet adhesion and spreading, as well as enhanced thromboxane A2 formation [39]. The absence of JNK in platelets also results in impaired platelet aggregation and granule release upon agonist stimulation, and inhibits vascular thrombosis in mouse cecum [40]. The MAPK-interacting kinase 1 regulate mRNA translation and cellular activation in platelets and megakaryocytes, endomitosis and thrombopoiesis, and thrombosis [41]. Furthermore, inflammation and thrombosis are closely linked processes. The p38 MAPK pathway plays a critical role in thrombin-induced endothelial proinflammatory activation [42]. In APS, a major mechanism of hypercoagulability is mediated by aPL, which upregulate tissue factor on monocytes through the p38 MAPK and NF-κB pathways [43]. A previous study found that MAPK signaling pathway was associated with deep venous thrombosis [44]. However, the MAPK signaling pathway is a vast and complex network, with limited research on its association with venous thrombosis. Further studies are needed to confirm the relationship between the MAPK pathway and CVT.
Our study has several limitations that should be acknowledged. The sample size of patients is small. The relationship between the MAPK pathway and CVT has not been experimentally validated. In addition, recruitment was limited to one hospital by Han Chinese people; therefore, caution is necessary when generalizing our findings to other ethnical groups.
Conclusion
This prospective case-control study of CVT patients enrolled from a comprehensive hospital in China, suggested that the role of genetic risk factors of CVT is indispensable and for patients with unknown etiology, WES could help identify the cause of CVT timely, which could to some extent aid in treatment decision-making and improve patient prognosis. In addition to the complement and coagulation pathways, we found that the MAPK pathway is associated with CVT, which is mainly related to platelet regulation and inflammation. The specific mechanism awaits further investigation through basic experiments.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Peking Union Medical College Hospital.
Abbreviations
- CVT:
-
Cerebral venous thrombosis
- WES:
-
Whole exome sequencing
- MAPK:
-
Mitogen activated protein kinases
- FVL:
-
Factor V Leiden
- PC:
-
Proteins C
- PS:
-
Protein S
- AT:
-
Antithrombin
- JAK2 V617F:
-
Janus Kinase-2 V617F
- ISGC:
-
International Stroke Genetics Consortium
- GWAS:
-
Genome-Wide Association Studies
- CTV:
-
Computed tomography venography
- MRI:
-
Magnetic resonance imaging
- MRV:
-
Magnetic resonance venography
- DSA:
-
Digital subtraction angiography
- APC-R:
-
Activated PC resistance
- aPL:
-
Antiphospholipid antibodies
- aCL:
-
Anticardiolipin antibodies
- aB2GPI:
-
Anti-β2-glycoprotein I antibodies
- SNVs:
-
Single-nucleotide variants
- HGMD:
-
Human Gene Mutation Database
- MAF:
-
Minor allele frequency
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- APS:
-
Antiphospholipid antibody syndrome
- hhcy:
-
Hyperhomocysteinemia
- PNH:
-
Paroxysmal nocturnal hemoglobinuria
- JNK:
-
C-Jun N-terminal kinase
- ERK:
-
Extracellular signal-regulated kinase
References
Saposnik G, Bushnell C, Coutinho JM, Field TS, Furie KL, Galadanci N, et al. Diagnosis and management of cerebral venous thrombosis: a Scientific Statement from the American Heart Association. Stroke. 2024. https://doi.org/10.1161/STR.0000000000000456.
Alet M, Ciardi C, Alemán A, Bandeo L, Bonardo P, Cea C, et al. Cerebral venous thrombosis in Argentina: clinical presentation, predisposing factors, outcomes and literature review. J Stroke Cerebrovasc Dis. 2020;29(10):105145. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105145.
Saposnik G, Bushnell C, Coutinho JM, Field TS, Furie KL, Galadanci N, et al. Diagnosis and management of cerebral venous thrombosis: a Scientific Statement from the American Heart Association. Stroke. 2024;55(3):e77–90. https://doi.org/10.1161/STR.0000000000000456.
Silvis SM, de Sousa DA, Ferro JM, Coutinho JM. Cerebral venous thrombosis. Nat Rev Neurol. 2017;13(9):555–65. https://doi.org/10.1038/nrneurol.2017.104.
Le Cam-Duchez V, Bagan-Triquenot A, Barbay V, Mihout B, Borg JY. The G79A polymorphism of protein Z gene is an independent risk factor for cerebral venous thrombosis. J Neurol. 2008;255(10):1521–5. https://doi.org/10.1007/s00415-008-0958-8.
Li Q-H, Xu L-Q, Dong Q, Chu H-L, Tang Y-P. Identification of LDLR mutation in cerebral venous sinus thrombosis co-existing with dural arteriovenous fistulas: a case report. BMC Neurol. 2023;23(1):423. https://doi.org/10.1186/s12883-023-03455-5.
Voetsch B, Jin RC, Bierl C, Deus-Silva L, Camargo ECS, Annichino-Bizacchi JM, et al. Role of promoter polymorphisms in the plasma glutathione peroxidase (GPx-3) gene as a risk factor for cerebral venous thrombosis. Stroke. 2008;39(2):303–7.
Reuner KH, Jenetzky E, Aleu A, Litfin F, Mellado P, Kloss M, et al. Factor XII C46T gene polymorphism and the risk of cerebral venous thrombosis. Neurology. 2008;70(2):129–32. https://doi.org/10.1212/01.wnl.0000296825.05176.da.
Cotlarciuc I, Marjot T, Khan MS, Hiltunen S, Haapaniemi E, Metso TM, et al. Towards the genetic basis of cerebral venous thrombosis-the BEAST Consortium: a study protocol. BMJ Open. 2016;6(11):e012351. https://doi.org/10.1136/bmjopen-2016-012351.
Li X, Cui L, Li Y, Zhu L, Wang C, Liu J, et al. Prevalence and geographical variation of Factor V Leiden in patients with cerebral venous thrombosis: a meta-analysis. PLoS ONE. 2018;13(8):e0203309. https://doi.org/10.1371/journal.pone.0203309.
Choi M, Scholl UI, Ji W, Liu T, Tikhonova IR, Zumbo P, et al. Genetic diagnosis by whole exome capture and massively parallel DNA sequencing. Proc Natl Acad Sci U S A. 2009;106(45):19096–101. https://doi.org/10.1073/pnas.0910672106.
Chinese Society of Neurology CSS. Chinese guidelines for diagnosis and treatment of cerebral venous thrombosis 2019. Chin J Neurol. 2020;53(09):648–63. (in Chinese).
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19(5):604–7.
Han F, Zhou L-X, Ni J, Yao M, Zhai F-F, Liu Y-T, et al. Design of the Shunyi study on cardiovascular disease and age-related brain changes: a community-based, prospective, cohort study. Ann Transl Med. 2020;8(23):1579. https://doi.org/10.21037/atm-20-4195.
Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25(14):1754–60. https://doi.org/10.1093/bioinformatics/btp324.
McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The genome analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20(9):1297–303. https://doi.org/10.1101/gr.107524.110.
San Lucas FA, Wang G, Scheet P, Peng B. Integrated annotation and analysis of genetic variants from next-generation sequencing studies with variant tools. Bioinformatics. 2012;28(3):421–2. https://doi.org/10.1093/bioinformatics/btr667.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24. https://doi.org/10.1038/gim.2015.30.
Wu Y-T, Zhou L-X, Yao M, Ni J, Zhu Y-C, Cui L-Y, et al. Clinical features of CVT in Women and Effect on subsequent pregnancy: a Follow-Up study in a Chinese National Comprehensive Hospital. J Stroke Cerebrovasc Dis. 2020;29(11):105274. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105274.
Zhang B, Lang Y, Zhang W, Cui L, Deng F. Characteristics and management of Autoimmune Disease-Associated cerebral venous sinus thrombosis. Front Immunol. 2021;12:671101. https://doi.org/10.3389/fimmu.2021.671101.
Leal Rato M, Bandeira M, Romão VC, Aguiar de Sousa D. Neurologic manifestations of the Antiphospholipid syndrome - an update. Curr Neurol Neurosci. 2021;21(8):41. https://doi.org/10.1007/s11910-021-01124-z.
Coutinho JM, Zuurbier SM, Gaartman AE, Dikstaal AA, Stam J, Middeldorp S, et al. Association between Anemia and cerebral venous thrombosis: case-control study. Stroke. 2015;46(10):2735–40. https://doi.org/10.1161/STROKEAHA.115.009843.
Meppiel E, Crassard I, de Latour RPd S, Terriou L, Chabriat H, et al. Cerebral venous thrombosis in paroxysmal nocturnal hemoglobinuria: a series of 15 cases and review of the literature. Med (Baltim). 2015;94(1):e362. https://doi.org/10.1097/MD.0000000000000362.
Finelli PF, Harrison RB, Uphoff DF. Myelodysplastic syndrome and sagittal sinus thrombosis. J Stroke Cerebrovasc Dis. 1998;7(3):211–2.
Zloto O, Lubetsky A, Ben-Bassat Mizrachi I, Kesler A, Quiros PA, Huna-Baron R. Prognostic value of JAK2V617F mutation in pseudotumor cerebri associated with cerebral venous sinus thrombosis. Acta Neurol Scand. 2019;139(2):166–71. https://doi.org/10.1111/ane.13032.
Guangsong H, Xinying H, Jun N, Weihai X, Ming Y. Hereditary hyperactivity of coagulation factor ix caused by a large fragment gene duplication as a rare etiology of cerebral venous sinus thrombosis. Hum Brain. 2023;2(2). https://doi.org/10.37819/hb.2.1769.
Turkut Tan T, Pariltay E, Avci Durmusaliogu E, Isik E, Cogulu O, Kavakli K, et al. A unique case of thrombophilia: the role of F9 gene duplication and increased factor IX activity in cerebral venous thrombosis. J Thromb Haemost. 2023;21(10):2913–6. https://doi.org/10.1016/j.jtha.2023.06.029.
Sarov M, Not A, de Baulny HO, Masnou P, Vahedi K, Bousser M-G, et al. A case of homocystinuria due to CBS gene mutations revealed by cerebral venous thrombosis. J Neurol Sci. 2014;336(1–2):257–9. https://doi.org/10.1016/j.jns.2013.10.009.
Dunjic Manevski S, Cumbo M, Pruner I, Gvozdenov M, Tomic B, Taxiarchis A, et al. Effect of prothrombin Belgrade mutation, causing antithrombin resistance, on fibrin clot properties. Int J Lab Hematol. 2023. https://doi.org/10.1111/ijlh.14195.
Morris AAM, Kožich V, Santra S, Andria G, Ben-Omran TIM, Chakrapani AB, et al. Guidelines for the diagnosis and management of cystathionine beta-synthase deficiency. J Inherit Metab Dis. 2017;40(1):49–74. https://doi.org/10.1007/s10545-016-9979-0.
Mannucci PM, Vigano S. Deficiencies of protein C, an inhibitor of blood coagulation. Lancet. 1982;2(8296):463–7.
Artoni A, Bucciarelli P, Martinelli I. Cerebral thrombosis and myeloproliferative neoplasms. Curr Neurol Neurosci. 2014;14(11):496. https://doi.org/10.1007/s11910-014-0496-y.
Lichy C, Dong-Si T, Reuner K, Genius J, Rickmann H, Hampe T, et al. Risk of cerebral venous thrombosis and novel gene polymorphisms of the coagulation and fibrinolytic systems. J Neurol. 2006;253(3):316–20.
Athar M, Ghita IS, Albagenny AA, Abduljaleel Z, Shadab G, Elsendiony A, et al. Targeted next-generation sequencing reveals novel and known variants of thrombophilia associated genes in Saudi patients with venous thromboembolism. Clin Chim Acta. 2021;519:247–54. https://doi.org/10.1016/j.cca.2021.05.012.
Subramaniam S, Jurk K, Hobohm L, Jäckel S, Saffarzadeh M, Schwierczek K, et al. Distinct contributions of complement factors to platelet activation and fibrin formation in venous thrombus development. Blood. 2017;129(16):2291–302. https://doi.org/10.1182/blood-2016-11-749879.
Patel P, Naik UP. Platelet MAPKs-a 20 + year history: what do we really know? J Thromb Haemost. 2020;18(9):2087–102. https://doi.org/10.1111/jth.14967.
Oury C, Toth-Zsamboki E, Vermylen J, Hoylaerts MF. P2X(1)-mediated activation of extracellular signal-regulated kinase 2 contributes to platelet secretion and aggregation induced by collagen. Blood. 2002;100(7):2499–505.
Dai Y, Zhou Q, Liu Y, Chen X, Li F, Yu B, et al. Ruscogenin alleviates deep venous thrombosis and Pulmonary Embolism Induced by Inferior Vena Cava Stenosis Inhibiting MEK/ERK/Egr-1/TF signaling pathway in mice. Curr Pharm Des. 2022;28(24):2001–9. https://doi.org/10.2174/1381612828666220526120515.
Saklatvala J, Rawlinson L, Waller RJ, Sarsfield S, Lee JC, Morton LF, et al. Role for p38 mitogen-activated protein kinase in platelet aggregation caused by collagen or a thromboxane analogue. J Biol Chem. 1996;271(12):6586–9.
Adam F, Kauskot A, Nurden P, Sulpice E, Hoylaerts MF, Davis RJ, et al. Platelet JNK1 is involved in secretion and thrombus formation. Blood. 2010;115(20):4083–92. https://doi.org/10.1182/blood-2009-07-233932.
Manne BK, Campbell RA, Bhatlekar S et al. MAPK-interacting kinase 1 regulates platelet production, activation, and thrombosis. Blood. 2022;140(23):2477–2489. Blood. 2023;141(24):3007. https://doi.org/10.1182/blood.2023020788.
Marin V, Farnarier C, Grès S, Kaplanski S, Su MS, Dinarello CA, et al. The p38 mitogen-activated protein kinase pathway plays a critical role in thrombin-induced endothelial chemokine production and leukocyte recruitment. Blood. 2001;98(3):667–73.
Lambrianides A, Carroll CJ, Pierangeli SS, Pericleous C, Branch W, Rice J, et al. Effects of polyclonal IgG derived from patients with different clinical types of the antiphospholipid syndrome on monocyte signaling pathways. J Immunol. 2010;184(12):6622–8. https://doi.org/10.4049/jimmunol.0902765.
Wang Q, Chang Y, Yang X, Han Z. Deep sequencing of circulating miRNAs and target mRNAs level in deep venous thrombosis patients. IET Syst Biol. 2023;17(4):212–27. https://doi.org/10.1049/syb2.12071.
Acknowledgements
Authors would like to thank all the authors of the original articles.
Funding
Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2022-I2M-1-001); Capital Medical Development Research funding of China (No. 2020-1-4012).
Author information
Authors and Affiliations
Contributions
Shaoying Wang: study design, data collection, analysis, and interpretation, drafting of the manuscript; Ming Yao: study design, data collection and interpretation; Xinzhuang Yang: bioinformatics analysis; Yicheng Zhu: data collection; Bin Peng: study design, study supervision and manuscript revision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors state that all methods were carried out in accordance with relevant guidelines and regulations and followed the principles outlined in the Declaration of Helsinki for human. The study was approved by the Ethics Committee of Peking Union Medical College Hospital (JS-2420). Written and informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
No conflict declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, S., Yao, M., Yang, X. et al. The genetic risk factors for cerebral venous thrombosis: a case-control study in a Chinese national comprehensive hospital. Thrombosis J 22, 50 (2024). https://doi.org/10.1186/s12959-024-00621-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-024-00621-8