Abstract
Background
Although the atherogenic index of plasma (AIP) based on a single measurement is a known risk factor for cardiovascular disease (CVD), little is known about whether changes in AIP over time are related to incident CVD. We aimed to determine whether AIP trajectory, which reflects homogenous AIP trends for a particular period, is associated with CVD risk.
Methods
Data from 5,843 participants of the Korean Genome and Epidemiology Study (KoGES) were analyzed. The KoGES had been conducted biennially from the baseline survey (2001–2002) to the eighth follow-up survey (2017–2018). The research design specifies the exposure period from baseline to the third follow-up, designates the latent period at the fourth follow-up, and establishes the event accrual period from the fifth to the eighth follow-up. During the exposure period, we identified two trajectories: a decreasing (n = 3,036) and an increasing group (n = 2,807) using latent variable mixture modeling. Information on CVD was collected initially through the self-reporting, followed by in depth person-to-person interview conducted by a well-trained examiner. During the event accrual period, the cumulative incidence rates of CVD between the two AIP trajectory groups were estimated using Kaplan–Meier analysis with the log-rank test. Multiple Cox proportional hazard models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs).
Results
The increasing AIP trajectory group had a significantly higher cumulative incidence rate of CVD than the decreasing AIP trajectory group. Compared to the decreasing AIP trajectory group, the increasing AIP trajectory group had a higher risk of incident CVD (HR: 1.31, 95% CI: 1.02–1.69) after adjusting for confounders.
Conclusions
The risk of incident CVD increased when the AIP level showed an increasing trend and remained high over a long period. This suggests that checking and managing the trajectory of the AIP can be a preventive strategy for incident CVD.
Similar content being viewed by others
Background
Cardiovascular disease (CVD) is a global leading cause of mortality [1]. From 1980 to 2017, the global trend for CVD mortality showed an increase by about 21% [2]. In South Korea, CVD has been ranked second among the causes of death between 2009 and 2019, and ischemic heart disease and ischemic stroke ranked sixth and seventh among the top 10 causes of death and disability, respectively [3]. Moreover, there is an increasing trend in the prevalence of CVD as the society ages [1, 4]. As in Europe, the United States, and most developing countries, the socioeconomic cost due to CVD in South Korea is rising and reached 820 million US dollars in 2015 [5, 6].
Risk factors of CVD include modifiable factors such as obesity, hypertension (HTN), diabetes mellitus (DM), dyslipidemia, and cigarette smoking, as well as non-modifiable factors such as sex, age, ethnicity, and heredity [7]. According to the Korean Heart Study that evaluated data from 1997 to 2011, the attributable risk of dyslipidemia for CVD was 8.7% in men and 4.1% in women among modifiable risk factors [8]. As the prevalence of dyslipidemia in Korea increased from 9.0% to 2007 to 20.7% in 2018, the contribution of dyslipidemia to CVD may have increased over time [9]. Among serum lipid profile parameters such as triglyceride (TG), high-density lipoprotein (HDL) cholesterol, and low-density lipoprotein (LDL) cholesterol, serum LDL cholesterol, especially small-dense LDL (sdLDL) cholesterol which is very vulnerable to oxidative damage, has been identified as an atherogenic lipoprotein parameter [10]. However, direct measurements of sdLDL cholesterol levels are limited in clinical practice because of lacking cost-effectiveness and a complicated detection method [11].
The atherogenic index of plasma (AIP) is a simple index based on TG and HDL cholesterol levels [12]. It associates with the lipoprotein particle size and cholesterol esterification rates in apoB-lipoprotein-depleted plasma, and this correlation suggests that the AIP could be an independent biomarker of atherosclerotic diseases [13]. In addition, previous findings have shown that the AIP is inversely proportional to the diameter of LDL cholesterol particles and, thus, reflects the sdLDL cholesterol level [14, 15]. Studies have confirmed the cross-sectional correlation between AIP and CVD risk [16, 17]. However, lipid profiles change continuously throughout a lifetime, as does the AIP, and so far, little is known about the cumulative and serial relationships between AIP trends and cardiovascular outcomes. Thus, it is necessary to determine whether the AIP trend over time is related to the incidence of CVD.
Therefore, this study aimed to determine whether the AIP trajectory, which reflects homogenous AIP trends for a certain period, is associated with CVD incidence using a large-scale community-based cohort dataset.
Methods
Study population
The Korean Genome and Epidemiology Study (KoGES) Ansan and Ansung is a community-based cohort study including randomly recruited residents from Ansan, an urbanized city located southwest of Gyeonggi-do, and from Ansung, a rural community south of Gyeonggi-do. For statistical reliability, participants were randomly contacted via home visits, telephone, or mail to recruit representative samples. The baseline survey was performed in 2001–2002, and follow-up examinations were conducted at 2-year intervals until the eighth follow-up (2017–2018). In the present study, we defined the median 5.8 years of baseline to the third follow-up period of the survey as the exposure period (2001–2008), the median 2.1 years of fourth follow-up as the latent period (2009–2010) and the median 7.8 years of fifth to the eighth follow-up period as the event accrual period (2011–2018).
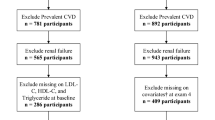
Figure 1 shows the flowchart depicting the study population selection process. Among the participants in the baseline survey (n = 10,030), we selected participants without CVD during the exposure period taking the following exclusion criteria into account: (1) missing AIP data at baseline (n = 3); (2) missing follow-up AIP data during the exposure period (n = 1,205); (3) lack of information about a history of CVD at baseline (n = 4); (4) prevalent CVD at baseline (n = 274); (5) participants who newly developed CVD during the exposure period (n = 224); (6) participants who newly developed CVD during the latent period (n = 86), and (7) missing data on the event accrual period (n = 2,391). Finally, 5,843 participants were included in the analysis. This study was approved by the institutional review board (IRB) of Nowon Eulji Medical Center (IRB number: EMCS 2022-12-010).
Assessment of the AIP trajectory groups
The AIP is defined by the following equation [14]:
AIP = log (TG (mg/dL) / HDL cholesterol (mg/dL)).
Using the baseline and follow-up AIP measurements during the exposure period, we performed latent variable mixture modeling to identify trends of changes in AIP. Latent variable mixture modeling and group-based trajectory modeling are representative statistical methods used for trajectory analysis [18]. In our study, we used latent variable mixture modeling to identify AIP trajectories; this approach has the ability to capture potential heterogeneity in AIP trends over time, which might not be fully captured by a predefined set of groups in group-based trajectory modeling [19].
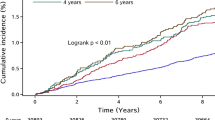
Groups of the study population that maintained relatively homogeneous AIP trends during the study period were classified as AIP trajectories [20,21,22]. The optimal number of AIP trajectories was identified by applying the minimum Bayesian information criterion (Table S1). Finally, we identified two trajectories: a group with decreasing trend of AIP trajectory (n = 3036) and a group with increasing trend of AIP trajectory (n = 2807), as shown in Fig. 2, considering the random effect using individual AIP data (Table S2). The AIP ranged between 0.20 and 0.40 in the decreasing AIP trajectory group and between 0.55 and 0.70 in the increasing AIP trajectory group during the exposure period.
Assessment of CVD
CVD was defined as cerebrovascular accident, peripheral arterial occlusive disease, myocardial infarction, or angina pectoris. CVD history was assessed based on self-reported medical history at each follow-up. If a participant reported an incident CVD event, a well-trained examiner confirmed the case after an in-depth personal interview. In a previous study that utilized data from the same cohort, the concordance between self-reported diagnoses and those ascertained by physician reviews of medical records was 93% [23]. Person-time for each participant was calculated from the start point of the event accrual period (2009–2010) until one of the following were observed: occurrence of CVD, loss to follow-up, or the end of the event accrual period (2017–2018). For individuals who did not experience CVD or were still under follow-up at the end of the event accrual period, person-time was censored at that point.
Covariates
With reference to the Korean Society for the Study of Obesity, obesity was defined as a body mass index (BMI) ≥ 25 kg/m2, which was calculated by dividing weight by the square of height (kg/m2) [24]. We measured systolic blood pressure (SBP, mmHg) and diastolic blood pressure (DBP, mmHg) in the sitting position after at least 30 min of rest. The smoking status of participants was classified as never, ex-, intermittent, or daily smoker. The drinking status of participants was classified as non-drinker or current drinker. Regarding the measurement of physical activity, we utilized the International Physical Activity Questionnaire to assess the metabolic equivalents of task (METs)-hours per day (METs-h/day). This was based on participants’ self-reported hours spent in various activities, including sleeping, sedentary behavior (0 METs), very light (1.5 METs), light (3 METs), moderate (5 METs), and heavy (7 METs) physical activities [25]. Participants were subsequently divided into three groups based on their weekly hours of physical activity: low (< 7.5 METs-h/day), moderate (7.5–30 METs-h/day), and high (> 30 METs-h/day) [26]. We calculated the total energy intake (kcal/day) based on a 103-item food frequency questionnaire. Blood samples were collected after at least 8 h of fasting. Fasting plasma glucose (FPG), total cholesterol, TG, HDL cholesterol, C-reactive protein (CRP), and white blood cell counts were analyzed. Serum LDL cholesterol levels were calculated using the Friedewald formula in case of serum TG levels < 400 mg/dL.
DM was defined as glycosylated hemoglobin ≥ 6.5%, FPG ≥ 126 mg/dL, plasma glucose ≥ 200 mg/dL at 2 h in the oral glucose tolerance test, or treatment with anti-diabetic medications or insulin therapy [27]. HTN was defined as SBP ≥ 140 mm Hg, DBP ≥ 90 mm Hg, or treatment with antihypertensive agents according to the 7th Joint National Committee [28]. Dyslipidemia was defined based on any one of the following criteria: (1) serum total cholesterol ≥ 240 mg/dL, (2) serum TG ≥ 200 mg/dL, (3) serum LDL cholesterol ≥ 160 mg/dL, (4) serum HDL cholesterol < 40 mg/dL for men or < 50 mg/dL for women, or (5) treatment with lipid-lowering medications [29].
Statistical analysis
Continuous variables, including age, BMI, waist circumference (WC), MBP, FPG, serum total cholesterol, TG, HDL cholesterol, LDL cholesterol, CRP, and total energy intake, were expressed as mean ± standard deviation. Categorical variables, including sex, smoking status, current drinking, physical activity, HTN, DM, and dyslipidemia, were expressed as numbers (percentages). Significant differences between continuous variables were assessed using Student’s t-test, whereas the chi-square test was used to analyze differences between categorical variables.
The cumulative incidence rates of CVD between the two AIP trajectory groups were estimated using Kaplan–Meier analysis and compared using the log-rank test. Multiple Cox proportional hazard regression analyses were performed to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) for incident CVD in the two AIP trajectory groups.
All statistical analyses were conducted using the SPSS software version 23 for Windows (IBM Corp., Armonk, NY, USA) and R software (version 4.1.3; R Foundation for Statistical Computing, Vienna, Austria). We used the R package ‘lcmm’ for latent variable mixture modeling. Statistical significance was set at P < 0.05.
Results
Baseline characteristics of the study population
The baseline characteristics of the study population are summarized in Table 1. The proportion of men was 46.4%, and the average age was 51.5 years in the total study population. The mean values of BMI, WC, MBP, FPG, total cholesterol level, LDL level and TG level, as well as the proportions of daily smokers, current drinkers, participants with low intensity of physical activity, patients with HTN, patients with DM, and patients with dyslipidemia, were higher in the increasing AIP trajectory group than in the decreasing group. By contrast, the mean values of serum HDL levels were lower in the increasing AIP trajectory group than in the decreasing group.
Incidence of CVD by AIP trajectory group
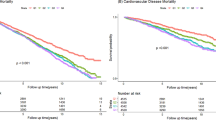
During the median 7.8 years of event accrual period, 278 (4.8%) newly developed CVD cases were registered in total. The incidence rate per 2 years ranged from 1.22 to 1.53 (Table 2). Figure 3 presents the Kaplan–Meier estimates of the cumulative incidence rate of CVD by AIP trajectory group. The increasing AIP trajectory group had a higher cumulative incidence rate of CVD than the decreasing AIP trajectory group (P for log-rank test < 0.001).
Associations of AIP trajectories and incident CVD
Table 3 presents the HRs with 95% CIs for incident CVD in participants with an increasing trajectory of AIP versus those with a decreasing trajectory of AIP. Compared to the decreasing AIP trajectory group, the increasing AIP trajectory group had a higher risk of incident CVD (HR: 1.57, 95% CI: 1.47–2.00). Similar trends were observed in the adjusted models. The adjusted HRs (95% CIs) for incident CVD of the increasing AIP trajectory group were 1.43 (1.12–1.83) in model 1, 1.34 (1.04–1.73) in model 2, and 1.31 (1.02–1.69) in model 3, respectively, compared to those of the decreasing AIP trajectory group.
Discussion
This study aimed to explore the possible relationship between the AIP trajectory and CVD using a large-scale community-based cohort dataset. While a single measurement of AIP can provide valuable information about an individual’s current CVD risk, tracking AIP trajectories over time allows for the identification of individuals who consistently exhibit high AIP levels. Two patterns of AIP trajectories were identified during the exposure period: increasing values and decreasing values. The incident CVD rate in the increasing AIP trajectory group was significantly higher than that in the decreasing AIP trajectory group. Moreover, the increasing AIP trajectory group had a higher risk of incident CVD than the decreasing AIP trajectory group in both crude and adjusted models. Additional analysis by CVD subtypes further indicated their individual significance in relation to AIP trajectories (Fig. S2). This supports the argument that maintaining a high AIP for a long period significantly increases the probability of CVD occurrence.
Considering the contribution of dyslipidemia to the development of atherosclerosis, it is very important to monitor the changes in lipid profiles, especially serum sdLDL levels, since sdLDL induces atherosclerotic lesions [30]. Several studies indicate that through the AIP, considerable information about the lipoprotein spectrum can be inferred, especially about the LDL cholesterol particle size [14,15,16, 31]. The formula for calculating the AIP incorporates the serum TG and HDL cholesterol levels, and using the AIP as a substitute marker for sdLDL has the advantages of cost-effectiveness and simplicity of its measurement.
While previous studies only determined the correlation between AIP at baseline and incident CVD [32,33,34], we verified the association of AIP trajectories with incident CVD. Considering that trajectory modeling is a useful statistical method for predicting different outcomes between subgroups of individuals exhibiting similar patterns over time [35], our results, obtained using AIP trajectory modeling, provide valuable insights into the long-term effects of lipid profiles on CVD risk. This analysis also supports the importance of monitoring lipid changes over time and subsequently extends evidence from previous studies [32,33,34].
Although the mechanisms for the relation of AIP trajectories with CVD risk remain unclear, several possible explanations may account for this relationship. First, increasing AIP trajectory could reflect the increasing trend of insulin resistance. Many studies have investigated the association between insulin resistance and CVD [36,37,38], and it has been found that hypertriglyceridemia and decreased levels of HDL cholesterol affect insulin resistance [39]. Hypertriglyceridemia inhibits glucose entry into cells and negatively affects glucose oxidation, resulting in insulin resistance [40]. In addition, as the TG level increases, the number and activity of insulin receptors in fat cells decrease [40]. The effect of HDL cholesterol on insulin sensitivity is due to its capability to facilitate glucose uptake into target cells such as hepatocytes, myocytes, and adipocytes [41]. Due to this dyslipidemia-insulin resistance interaction, the TG/HDL cholesterol ratio has been used as an insulin resistance marker [42]. Second, AIP is significantly correlated with the number of very LDL and sdLDL particles, which can upregulate the expression of adherence molecules on endothelial cells [43]. Direct associations between AIP and atherosclerosis have been identified in several studies, including arterial stiffness [44], carotid artery intima-media thickness, and overall state of atherosclerosis [45, 46]. Several studies have demonstrated that the AIP has potential efficacy in predicting CVD risks [13, 16, 31]. In line with these studies, the prevalence of DM, HTN, and incidence of CVD was significantly higher in the increasing AIP group than in the decreasing AIP group. Finally, systemic inflammation is considered a key factor in the development of CVD [47], and inflammatory responses may have mediated the association between AIP and CVD [31, 48]. Zhan et al. [49] suggested that the AIP is a reliable biomarker of ischemic heart disease and reported the relationship between AIP increases and the high incidence of ischemic heart disease mediated by lipid-driven inflammation. Thus, we performed a mediation analysis to determine the effect of serum CRP levels as mediators of CVD development (Table S3). Although CRP is the most commonly used biomarkers of systemic inflammation [50,51,52], contrary to our expectations, the mediation effect of CRP was not significant. Possible explanations for these results are that pro-inflammatory cytokines other than CRP, such as tumor necrosis factor alpha, interleukin (IL)-1, or IL-6, may act as mediators, and other effects that may cause chronic inflammation could not be completely ruled out in this study. Moreover, genetic differences such as single nucleotide polymorphisms between increasing and decreasing AIP trajectory groups need to be further analyzed. Therefore, further research is needed to identify possible mediators between AIP trajectories and CVD.
This study has several strengths compared to previous studies. First, unlike previous studies, our study confirmed the trend based on trajectories, not spot-checks, which means the study period is the result of data for up to 16 years, including 6 years of exposure, 2 years of latent period and 8 years of event accrual period. To the best of our knowledge, this study is the first to verify that identifying the trend of time-varying variables using trajectory modeling is an important part of CVD prevention. Second, it also has the strength of research using a large population cohort, which demonstrated a robust association between AIP and future CVD risk.
In addition, our research has some limitations. First, selection bias may have occurred because CVD that occurred during the exposure period was not included in the analysis. Second, the prevalence of CVD in the study participants was not directly assessed using the 10th revision of the International Statistical Classification of Diseases code; instead, it was determined through interviews. In this process, recall bias or incomplete reporting may have occurred. Nevertheless, we believe the reliability of this study considering the high concordance rate (93%) of diagnoses of disease between self-reported diagnoses and those ascertained by physician review of medical records [23]. Third, information on mortality was not available. Therefore, the possibility of under-diagnosis of CVD in this study exists. Moreover, it is possible that only healthier people were selected, and the selection bias had rather increased. Fourth, we assumed that changes in AIP during the latent period did not affect CVD events. Fifth, only Korean individuals were included in the current analysis. Considering that the mean value of AIP varies depending on ethnicity [53], our results cannot be generalized to other ethnic populations. Nonetheless, the results of this study still have clinical significance in that AIP trajectories can be a reliable predictor of CVD risk in Asian ethnicities.
Conclusions
In conclusion, the risk of incident CVD increased when an increasing trend of AIP was maintained for a long time. This suggests that serial monitoring of AIP can be a preventive strategy for incident CVD. Further laboratory research and large-scale clinical studies should be conducted to explain the exact mechanism of the relationship between trajectories of AIP and CVD risk.
Data Availability
The dataset used in this study can be provided after a KCDA review and evaluation of the research plan (https://www.nih.go.kr/ko/main/contents.do?menuNo=300563).
Abbreviations
- CVD:
-
Cardiovascular Disease
- AIP:
-
Atherogenic Index of Plasma
- KoGES:
-
Korean Genome and Epidemiology Study
- TG:
-
Triglycerides
- HDL-C:
-
High-Density Lipoprotein Cholesterol
- LDL-C:
-
Low-Density Lipoprotein Cholesterol
- BMI:
-
Body Mass Index
- WC:
-
Waist Circumference
- MBP:
-
Mean Blood Pressure
- FPG:
-
Fasting Plasma Glucose
- CRP:
-
C-Reactive Protein
- WBC:
-
White Blood Cell
- DM:
-
Diabetes Mellitus
- HTN:
-
Hypertension
- METs:
-
Metabolic Equivalents of Task
- HR:
-
Hazard Ratio
- CI:
-
Confidence Interval
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk factors, 1990–2019: Update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010.
Global regional. National age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88. https://doi.org/10.1016/s0140-6736(18)32203-7.
Kim HC. Epidemiology of cardiovascular disease and its risk factors in Korea. Glob Health Med. 2021;3(3):134–41. https://doi.org/10.35772/ghm.2021.01008.
Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–47. https://doi.org/10.1016/s0140-6736(11)60393-0.
Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: a systematic review. BMC Public Health. 2018;18(1):975. https://doi.org/10.1186/s12889-018-5806-x.
Pereira E, Pereira H. Socioeconomic impact of cardiovascular disease. Revista Portuguesa de Cardiologia (English edition). 2020;39(5):253–4. https://doi.org/10.1016/j.repce.2020.10.006.
Magnus P, Beaglehole R. The real contribution of the major risk factors to the coronary epidemics: time to end the only-50% myth. Arch Intern Med. 2001;161(22):2657–60. https://doi.org/10.1001/archinte.161.22.2657.
Jee SH, Jang Y, Oh DJ, Oh BH, Lee SH, Park SW, et al. A coronary heart disease prediction model: the Korean Heart Study. BMJ Open. 2014;4(5):e005025. https://doi.org/10.1136/bmjopen-2014-005025.
Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Joo HJ, et al. Dyslipidemia Fact Sheets in Korea 2020: an analysis of Nationwide Population-based data. J Lipid Atheroscler. 2021;10(2):202–9. https://doi.org/10.12997/jla.2021.10.2.202.
Ikezaki H, Lim E, Cupples LA, Liu CT, Asztalos BF, Schaefer EJ. Small dense low-density lipoprotein cholesterol is the most atherogenic lipoprotein parameter in the prospective Framingham offspring study. J Am Heart Assoc. 2021;10(5):e019140. https://doi.org/10.1161/jaha.120.019140.
Kanonidou C. Small dense low-density lipoprotein: Analytical review. Clin Chim Acta. 2021;520:172–8. https://doi.org/10.1016/j.cca.2021.06.012.
Dobiásová M, Frohlich J. [The new atherogenic plasma index reflects the triglyceride and HDL-cholesterol ratio, the lipoprotein particle size and the cholesterol esterification rate: changes during lipanor therapy]. Vnitr Lek. 2000;46(3):152–6.
Choudhary MK, Eräranta A, Koskela J, Tikkakoski AJ, Nevalainen PI, Kähönen M, et al. Atherogenic index of plasma is related to arterial stiffness but not to blood pressure in normotensive and never-treated hypertensive subjects. Blood Press. 2019;28(3):157–67. https://doi.org/10.1080/08037051.2019.1583060.
Dobiásová M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apob-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem. 2001;34(7):583–8. https://doi.org/10.1016/s0009-9120(01)00263-6.
Burns SF, Lee SJ, Arslanian SA. Surrogate lipid markers for small dense low-density lipoprotein particles in overweight youth. J Pediatr. 2012;161(6):991–6. https://doi.org/10.1016/j.jpeds.2012.06.013.
Dobiásová M, Frohlich J, Sedová M, Cheung MC, Brown BG. Cholesterol esterification and atherogenic index of plasma correlate with lipoprotein size and findings on coronary angiography. J Lipid Res. 2011;52(3):566–71. https://doi.org/10.1194/jlr.P011668.
Dobiásová M. [AIP–atherogenic index of plasma as a significant predictor of cardiovascular risk: from research to practice]. Vnitr Lek. 2006;52(1):64–71.
Hetherington E, Plamondon A, Williamson T. Trajectory modeling with latent groups: potentials and pitfalls. Curr Epidemiol Rep. 2020;7(4):171–8. https://doi.org/10.1007/s40471-020-00242-5.
Kwon J-Y, Sawatzky R, Baumbusch J, Lauck S, Ratner PA. Growth mixture models: a case example of the longitudinal analysis of patient-reported outcomes data captured by a clinical registry. BMC Med Res Methodol. 2021;21(1):79. https://doi.org/10.1186/s12874-021-01276-z.
Song M, Hu FB, Wu K, Must A, Chan AT, Willett WC, et al. Trajectory of body shape in early and middle life and all cause and cause specific mortality: results from two prospective US cohort studies. BMJ. 2016;353:i2195. https://doi.org/10.1136/bmj.i2195.
Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, et al. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA. 2014;311(5):490–7. https://doi.org/10.1001/jama.2013.285122.
Yang S, Kwak S, Song Y-H, Han SS, Lee HS, Kang S, et al. Association of longitudinal trajectories of insulin resistance with adverse renal outcomes. Diabetes Care. 2022;45(5):1268–75. https://doi.org/10.2337/dc21-2521.
Baik I, Cho NH, Kim SH, Shin C. Dietary information improves cardiovascular disease risk prediction models. Eur J Clin Nutr. 2013;67(1):25–30. https://doi.org/10.1038/ejcn.2012.175.
Seo MH, Lee WY, Kim SS, Kang JH, Kang JH, Kim KK, et al. 2018 korean Society for the study of obesity Guideline for the management of obesity in Korea. J Obes Metab Syndr. 2019;28(1):40–5. https://doi.org/10.7570/jomes.2019.28.1.40.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):498–504. https://doi.org/10.1097/00005768-200009001-00009.
Jang M, Won C, Choi H, Kim S, Park W, Kim D, et al. Effects of physical activity on fractures in adults: A Community-Based korean Cohort Study. Korean J Sports Med. 2017;35(2):97–102. https://doi.org/10.5763/kjsm.2017.35.2.97.
2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):14–s31. https://doi.org/10.2337/dc20-S002.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–52. https://doi.org/10.1161/01.HYP.0000107251.49515.c2.
Joint committee for guideline r. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol. 2018;15(1):1–29. https://doi.org/10.11909/j.issn.1671-5411.2018.01.011.
Cure MC, Tufekci A, Cure E, Kirbas S, Ogullar S, Kirbas A, et al. Low-density lipoprotein subfraction, carotid artery intima-media thickness, nitric oxide, and tumor necrosis factor alpha are associated with newly diagnosed ischemic stroke. Ann Indian Acad Neurol. 2013;16(4):498–503. https://doi.org/10.4103/0972-2327.120438.
Onat A, Can G, Kaya H, Hergenç G. Atherogenic index of plasma (log10 triglyceride/high-density lipoprotein-cholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol. 2010;4(2):89–98. https://doi.org/10.1016/j.jacl.2010.02.005.
Fernández-Macías JC, Ochoa-Martínez AC, Varela-Silva JA, Pérez-Maldonado IN. Atherogenic index of plasma: Novel Predictive Biomarker for Cardiovascular Illnesses. Arch Med Res. 2019;50(5):285–94. https://doi.org/10.1016/j.arcmed.2019.08.009.
Kim JJ, Yoon J, Lee YJ, Park B, Jung DH. Predictive value of the Atherogenic Index of plasma (AIP) for the risk of Incident Ischemic Heart Disease among non-diabetic Koreans. Nutrients. 2021;13(9). https://doi.org/10.3390/nu13093231.
Sadeghi M, Heshmat-Ghahdarijani K, Talaei M, Safaei A, Sarrafzadegan N, Roohafza H. The predictive value of atherogenic index of plasma in the prediction of cardiovascular events; a fifteen-year cohort study. Adv Med Sci. 2021;66(2):418–23. https://doi.org/10.1016/j.advms.2021.09.003.
Nagin DS. Group-based trajectory modeling: an overview. Ann Nutr Metab. 2014;65(2–3):205–10. https://doi.org/10.1159/000360229.
McFarlane SI, Banerji M, Sowers JR. Insulin resistance and cardiovascular disease. J Clin Endocrinol Metab. 2001;86(2):713–8. https://doi.org/10.1210/jcem.86.2.7202.
Hill MA, Yang Y, Zhang L, Sun Z, Jia G, Parrish AR, et al. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism. 2021;119:154766. https://doi.org/10.1016/j.metabol.2021.154766.
Muniyappa R, Chen H, Montagnani M, Sherman A, Quon MJ. Endothelial dysfunction due to selective insulin resistance in vascular endothelium: insights from mechanistic modeling. Am J Physiol Endocrinol Metab. 2020;319(3):E629–e46. https://doi.org/10.1152/ajpendo.00247.2020.
Li N, Fu J, Koonen DP, Kuivenhoven JA, Snieder H, Hofker MH. Are hypertriglyceridemia and low HDL causal factors in the development of insulin resistance? Atherosclerosis. 2014;233(1):130–8. https://doi.org/10.1016/j.atherosclerosis.2013.12.013.
Goodpaster BH, Kelley DE. Skeletal muscle triglyceride: marker or mediator of obesity-induced insulin resistance in type 2 diabetes mellitus? Curr Diab Rep. 2002;2(3):216–22. https://doi.org/10.1007/s11892-002-0086-2.
Drew BG, Rye KA, Duffy SJ, Barter P, Kingwell BA. The emerging role of HDL in glucose metabolism. Nat Rev Endocrinol. 2012;8(4):237–45. https://doi.org/10.1038/nrendo.2011.235.
Steiner G, Vranic M. Hyperinsulinemia and hypertriglyceridemia, a vicious cycle with atherogenic potential. Int J Obes. 1982;6(Suppl 1):117–24.
Kawakami A, Aikawa M, Alcaide P, Luscinskas FW, Libby P, Sacks FM. Apolipoprotein CIII induces expression of vascular cell adhesion molecule-1 in vascular endothelial cells and increases adhesion of monocytic cells. Circulation. 2006;114(7):681–7. https://doi.org/10.1161/circulationaha.106.622514.
Nam JS, Kim MK, Park K, Choi A, Kang S, Ahn CW, et al. The plasma atherogenic index is an independent predictor of arterial stiffness in healthy Koreans. Angiology. 2022;73(6):514–9. https://doi.org/10.1177/00033197211054242.
Yildiz G, Duman A, Aydin H, Yilmaz A, Hür E, Mağden K, et al. Evaluation of association between atherogenic index of plasma and intima-media thickness of the carotid artery for subclinic atherosclerosis in patients on maintenance hemodialysis. Hemodial Int. 2013;17(3):397–405. https://doi.org/10.1111/hdi.12041.
Fu L, Zhou Y, Sun J, Zhu Z, Xing Z, Zhou S, et al. Atherogenic index of plasma is associated with major adverse cardiovascular events in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2021;20(1):201. https://doi.org/10.1186/s12933-021-01393-5.
Libby P. Inflammation in atherosclerosis. Nature. 2002;420(6917):868–74. https://doi.org/10.1038/nature01323.
Mazidi M, Katsiki N, Mikhailidis DP, Banach M. Association of ideal cardiovascular health metrics with serum uric acid, inflammation and atherogenic index of plasma: a population-based survey. Atherosclerosis. 2019;284:44–9. https://doi.org/10.1016/j.atherosclerosis.2018.09.016.
Zhan Y, Xu T, Tan X. Two parameters reflect lipid-driven inflammatory state in acute coronary syndrome: atherogenic index of plasma, neutrophil-lymphocyte ratio. BMC Cardiovasc Disord. 2016;16:96. https://doi.org/10.1186/s12872-016-0274-7.
Kushner I. C-reactive protein and the acute-phase response. Hosp Pract (off Ed). 1990;25(3a):13. 6, 21 – 8.
Pepys MB, Baltz ML. Acute phase proteins with special reference to C-reactive protein and related proteins (pentaxins) and serum amyloid A protein. Adv Immunol. 1983;34:141–212. https://doi.org/10.1016/s0065-2776(08)60379-x.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644-55. https://doi.org/10.1378/chest.101.6.1644.
Cheah WL, Chang CT, Hazmi H, Wan Muda WM. Gender and racial differences in the Cardiovascular Risk factors among overweight and obese rural adults, Kuching and Samarahan Division, Sarawak, Malaysia. J Nutr Metab. 2016;2016:4536753. https://doi.org/10.1155/2016/4536753.
Acknowledgements
Data in this study were from the Korean Genome and Epidemiology Study (KoGES; 6635 − 302), National Institute of Health, Korea Disease Control and Prevention Agency, Republic of Korea.
Funding
This research was supported by the Korea Institute of Planning and Evaluation for Technology in Food, Agriculture, and Forestry (IPET) through the High Value-added Food Technology Development Program, funded by the Ministry of Agriculture, Food, and Rural Affairs (MAFRA), grant number 321030051HD030.
Author information
Authors and Affiliations
Contributions
Dong-Wook Chun, Jun-Hyuk Lee and Ji-Won Lee wrote the main manuscript text.Dong-Wook Chun, Jun-Hyuk Lee and Yae-Ji Lee prepared Tables 1, 2 and 3.Dong-Wook Chun and Jun-Hyuk Lee prepared Figs. 1, 2 and 3. As corresponding authors, Ji-Won Lee and Jun-Hyuk Lee contributed equally to this work.All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The present study involving human subjects has received ethical approval from the Institutional Review Board (IRB) of Nowon Eulji Medical Center (IRB number: EMCS 2022-12-010). Informed consent was obtained from all human participants included in this study. Participants were provided with a detailed explanation of the study’s purpose, procedures, potential risks and benefits, confidentiality measures, and their right to withdraw at any time without consequence. Written consent forms were signed by participants prior to their participation, indication their voluntary agreement to take part in the study.
Consent for publication
Separate consent for publication was obtained from all human participants who agreed to have their data and findings shared in scientific publications. Participants were informed about the possibility of their anonymized data being used for academic and research purposes, while ensuring their confidentiality and privacy. Written consent for publication was obtained to ensure compliance with ethical guidelines.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chun, DW., Lee, YJ., Lee, JH. et al. Longitudinal trajectories of atherogenic index of plasma and risks of cardiovascular diseases: results from the Korean genome and epidemiology study. Thrombosis J 21, 99 (2023). https://doi.org/10.1186/s12959-023-00542-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-023-00542-y