Abstract
Background
This study aimed to assess the outcomes of thrombectomy with/without iliac vein stenting for young and transiently provoked DVT patients with iliac vein stenosis.
Methods
This is a retrospective analysis of a prospectively collected multicenter database. Acute, transiently provoked DVT patients between 18 and 45 years old with iliac vein stenosis were included. All patients underwent thrombectomy. Outcomes including the Villalta score, the VEINES-QOL score, and adverse events were evaluated.
Results
The data of 522 patients were collected of whom 75 were included, 58 underwent thrombectomy alone (nonstenting group) and 17 underwent thrombectomy and stenting (stenting group). Within 6 months, the Villalta score of patients in stenting group is lower than that of patients in nonstenting group (6 mo: 0.73 ± 0.77 vs. 1.41 ± 0.56, p = .0004), and the VEINES-QOL score of stenting group is higher than that of nonstenting group (6 mo: 89.00 ± 2.94 vs. 87.47 ± 3.72, p = .2141). At the following follow-ups, the Villalta score (12 mo: 0.56 ± 0.49 vs. 0.60 ± 0.58, p = .8266) and VEINES-QOL score (12 mo: 88.36 ± 2.29 vs. 88.31 ± 3.36, p = .9604) between the two groups are similar.
Conclusion
The stenting group had better efficacy within 6 months after intervention, while there was no significant difference in the symptom, signs, and quality of life between two groups after 6 months within a 2-year follow-up.
Trial registration
This study was registered in the Chinese Clinical Trial Registry (Registration Number: ChiCTR2200056073).
Similar content being viewed by others
Introduction
Deep venous thrombosis (DVT) is the abnormal coagulation of blood in the deep venous system, with an annual incidence of approximately 1–2‰ [1,2,3]. Approximately 50% of DVT patients gradually develop a series of signs and symptoms called postthromobtic syndrome (PTS), which may reduce the quality of life of patients severely [1].
Venous thrombosis in the lower extremities may be associated with iliac vein stenosis. Previous studies noted that more than 75% of patients suffering from left lower extremity DVTs have iliac stenosis, such as iliac vein compression syndrome [4, 5]. The treatment strategy for acute DVT patients with iliac vein stenosis remains controversial, since interventional therapies appear to be no more effective than anticoagulant therapy alone [6, 7]. Stent implantation may be effective for acute DVT patients with iliac vein occlusion or stenosis greater than 50% after thrombectomy [8, 9]. However, the average age in existing studies were mostly over 50 years [5, 10, 11], and there have been fewer studies on younger patients [12]. Stenting is proved important in preventing venous fibrotic stenosis and maintaining venous outflow tract patency [8, 13], but evidence for stenting was lacking in young and acute DVT patients with sufficient venous return function.
In this study, we investigated whether stenting can be avoided in young and transiently provoked DVT patients with iliac stenosis more than 50% and good venous return (defined as the contrast agent stasis time of fewer than 6 s). The symptom remission, quality of life of the patients, and incidences of thrombosis and stent occlusion were compared between stenting and nonstenting groups. The results might provide data for the development of interventional strategies for young patients with provoked DVT.
Methods
This study is reported with guidance of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [14].
Study design and patient population
The data was prospectively collected from four medical alliance hospitals (Shanghai Ninth People’s Hospital, Fengcheng Hospital, Zhoupu Hospital, and Putuo Hospital). between January 2016 and December 2021. Acute, transiently provoked DVT patients between 18 and 45 years old with iliac stenosis who underwent AngioJet rheolytic thrombectomy (ART) and met the criteria were included. This study was approved by the Ethics Committee of Shanghai JiaoTong University School of Medicine.
The inclusion criteria were as follows: [1] age 18–45 years; [2] acute-phase DVT (within 2 weeks of symptoms onset) with iliac vein stenosis and received ART; [3] a clear provoking factor of DVT; [4] iliac-femoral DVT diagnosed for the first time, with or without femoropopliteal DVT and pulmonary embolism, and no history of superficial varicose veins or leg swelling. The exclusion criteria were as follows: [1] congenital diseases, such as Klippel-Trenaunay syndrome; [2] contraindications to anticoagulation or abnormal coagulation function; [3] incomplete treatment or missing data, and [4] iliac vein stenosis less than 50%, or contrast agent stasis time more than 6 s after ART and possible balloon dilation or catheter-directed thrombolysis (CDT).
Procedures
The ART procedures have been described previously [5]. Briefly, patients received 200 U/kg low-molecular-weight heparin or 1.0 mg/kg enoxaparin following diagnosis. During the procedure, after the guidewire and the AngioJet catheter (Solent/Zelante, Boston Scientific, USA) were successfully advanced through the thrombosed vein segment, a power pulse lytic model was used with 0.25 × 106 units of urokinase in 100 mL of saline. Fifteen minutes later, the AngioJet catheter was placed in standard rheolytic thrombectomy mode. This sequence was repeated if significant residual thrombi remained on subsequent venograms.
Some patients underwent balloon dilation and CDT after ART. The balloon dilation was performed using balloon catheters (Mustang, Boston Scientific, USA) with a diameter of 8–16 mm for serial dilation from the femoral vein to the common iliac vein. The procedure of CDT was inserting a multiple-side-hole infusion catheter (Angiodynamics, Queensbury, USA) into the thrombotic segment, and injecting urokinase (30,000–50,000 U/100 mL/h). When the fibrinogen level reached 1.5 g/L, the urokinase dosage was halved, and CDT would be finished when the fibrinogen level was decreased to 1.0 g/L. After ART and possible balloon dilation or CDT, venogram was performed to exam the iliac vein stenosis rate and contrast agent stasis time. The representative DSA sequence of contrast agent stasis time examination is shown in Supplemental file 1. The contrast agent stasis time is defined as the interval from the arrival of contrast agent in the iliac vein to the disappearance of contrast at the same level.
As described before [15], for patients underwent stenting, self-expanding stents Wallstent (Boston Scientific, USA) or a Lifestar (Bard Medical, USA) were implanted after balloon dilation. The stent diameters ranged from 12 to 14 mm for the iliac-femoral vein and from 14 to 16 mm for the common iliac.
After the procedure, patients of both groups received the same anti-coagulation therapy. Low molecular weight heparin was used during hospitalization. After discharge, warfarin or rivaroxaban were prescribed for at least 6 months since patients underwent endovascular intervention according to CIRSE standards of practice guidelines [8]. For patients taking warfarin, the international normalized ratio was maintained between 2 and 3. Patients received no postoperative anti-platelet treatment. All the patients used compression stockings (class II, 30 mmHg) as a standard adjunct treatment.
Follow-up and outcomes
The outcomes included severity of lower limb symptoms, quality of life, free from re-thrombosis rate and complications. The severity of lower limb symptoms was evaluated using the Villalta score. The VEINES-QOL questionnaire was translated into local language from the appendix of Kahn 2006 [16]. Clinical follow-up visits were scheduled at 1, 3, 6, and 12 months after the procedure, and then yearly. A duplex scan or venography was performed to assess patency, and questionnaire follow-up was used to record the Villalta score and the VEINES-QOL score. Adverse events were continuously monitored during follow-up.
Statistical analysis
Binary data are expressed as absolute or relative frequencies and were compared by the chi-square or Fisher exact tests. Ranked data are expressed as absolute values and were compared by the Cochran-Armitage trend test. Continuous data are expressed as the mean ± standard deviation and were compared using Student’s t-test. The free from re-thrombosis rate was assessed by the Kaplan–Meier estimator. For all tests, p < .05 was defined as significant. All analysis was performed using SAS 9.2 (Stat, SAS Institute, Cary, NC, USA).
Results
Patient demographics and procedure characteristics
The prospective database contained 522 patients, of whom 75 (14.37%) patients met the criteria and involved in the analysis. All involved patients were admitted to hospital and underwent the procedure during the acute phase of DVT. The baseline characteristics of the patients are reported in Table 1. The average age of patients who underwent stenting was 36.65 ± 4.61 years (range: 25–45) and that of patients without stenting was 32.52 ± 8.77 years (range: 19–45). All patients had transient provoking factors for DVT, including surgery, trauma, immobilization (≥ 72 h), pregnancy/puerperium and hormone therapy (such as oral contraceptive). In both groups, most of the thrombi occurred in the left extremity. A total of 58.82% of patients in the stenting group and 25.86% of patients in the nonstenting group underwent CDT (p = .0183). Except for the rate of CDT use, no other significant differences were observed in the baseline characteristics between the stenting and nonstenting groups. No vessel perforation, hemorrhage, severe pain, or rapid heart rate or blood pressure drop occurred during the procedure. All patients received therapeutic oral anticoagulation for at least 6 months after discharge, and there was no significant difference in the use of anticoagulants (p = .8268). Three patients in the stenting group and twelve patients in the nonstenting group requested switch from warfarin to rivaroxaban for ease of administration, and no adverse event was reported before and during the drug switch. No patient received anti-platelet therapy.
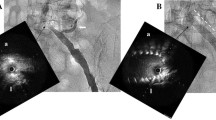
DSA images. (A) DSA image showed the presence of iliofemoral vein thrombosis before intervention. (B-C) Intraoperative imaging of ART and balloon dilation of iliofemoral veins. (D) After intervention, the proximal iliac vein was still stenosed. (E-F) Six-month follow-up angiography showed the proximal iliac vein occlusion and well-developed collateral vessels. DSA: digital subtraction angiography; DVT: deep vein thrombosis.
The representative digital subtraction angiography (DSA) images of a patient underwent ART without stent are presented. The patient was a 23-years-old female, diagnosed as DVT provoked by pregnancy (Fig. 1A). ART and balloon dilation were performed as described above (Fig. 1B-C). After intervention, the proximal iliac vein stenosis was still more than 50% and the stasis time of the contrast agent in the left iliac vein was 5 s (Fig. 1D). Iliac vein stent was not implanted. Six-month follow-up DSA showed that well-developed collateral vessels were visualized while the proximal iliac vein stenosis presented (Fig. 1E-F). The patient had no symptoms or signs of heaviness, cramps, edema, and varicose veins.
Representative DSA images of a patient underwent ART without stent. DSA images. (A) DSA image showed the presence of iliofemoral vein thrombosis before intervention. (B-C) Intraoperative imaging of ART and balloon dilation of iliofemoral veins. (D) After intervention, the proximal iliac vein was still stenosed. (E-F) Six-month follow-up angiography showed the proximal iliac vein occlusion and well-developed collateral vessels. DSA: digital subtraction angiography; DVT: deep vein thrombosis
Outcomes
The Villalta score and VEINES-QOL score of young DVT patients with iliac stenosis received stent implantation or not after thrombus removal before intervention and during follow-up.
The preoperative and follow-up outcomes are summarized in Table 2; Fig. 2. The Villalta score was used to quantify the severity of symptoms and signs. Before intervention, the Villalta scores of the stenting and nonstenting groups were similar (p = .5266). After intervention, the Villalta scores of both groups decreased. The Villalta scores of patients with stenting were significantly lower than those of patients without stenting at 1 month (p = .0005) and 6 months (p = .0004) after intervention. At month 12, the Villalta scores of the stenting group and nonstenting group had decreased further, and there was no significant difference between the two groups (p = .8266). At the 18- and 24-month follow-ups, the scores in both groups remained low, and there was also no significant difference between the two groups. During the follow-up, no patient was diagnosed with PTS in either group. The VEINES-QOL questionnaires were used to assess patients’ quality of life. Before intervention, there was no significant difference in the VEINES-QOL scores between stenting group and nonstenting group (p = .0576). The VEINES-QOL score of the nonstenting group was significantly lower than that of the stenting group at 1 month after intervention (p = .0094), and there was no significant difference between the two groups at the subsequent 6- (p = .2141), 12- (p = .9604), 18- (p = .8101) and 24- (0.0571) month follow-ups.
The Kaplan-Meier curves represent the occurrence of recurrent DVT within the follow-up duration. CI: confidence interval.
The proportion of patients free from recurrent DVT was represented by Kaplan–Meier survival curves (Fig. 3). For the stenting group, stent occlusion was also included among the events. According to the Kaplan–Meier curves, there was no significant difference in the rate of or recurrent DVT between the nonstenting group and the stenting group after 12 months (p = .0596). In the stenting group, 1 case of thrombosis was diagnosed by the 3-month follow-up, and another case was reported 6 months after intervention. The rethrombosis-free rate was 88.24% after 12 months. In the nonstenting group, one rethrombosis was reported in the 12 months after intervention, and the rethrombosis-free rate was 97.92%. No serious adverse events (defined as vessel perforation, iatrogenic embolization, other hospitalizations or death) occurred after the intervention.
Discussion
Existing intervention strategies inadequately target the young secondary DVT population with iliac vein stenosis due to the low morbidity, small number of studies, and low sample size [17]. Although venous stenting has become a more commonly used treatment for iliac vein obstruction [18], the evidence supporting the use of stenting to prevent PTS and rethrombosis is insufficient. More targeted stent implantation was also conducive to reducing medical costs and improving the medical experience of young patients. In the real world, a considerable number of young people were reluctant to undergo stent implantation for the risk of rethrombosis, stent fatigue and instent stenosis. To meet the needs, more detailed strategy was supposed to be refined.
This study was conducted specially for young patients under 45 years old. Within 6 months after endovascular treatment, the degree of improvement in limb symptoms and quality of life in patients who underwent stenting was higher than that in patients who did not. At the 12-month and later follow-ups, there was no significant difference in clinical outcomes between the stenting and nonstenting groups. This result suggested that nonstenting was feasible for young patients with transiently provoked DVT, in cases of iliac vein stenosis more than 50% with proper collateral circulation after thrombus removal.
In patients with DVT provoked by a major transient risk factor, the risk of recurrent venous thromboembolism was low [19, 20]. The patients involved in this study had no previous symptoms of chronic venous insufficiency, and their DVT was triggered by obvious causes. In addition, the risk was also considered low in patients with an unprovoked isolated distal deep vein thrombosis [21]. For these patients, the venous return may recover if the thrombosis was cleared and the pelvic venous collateral circulation was re-established; 3–6 months of treatment after thrombosis was considered adequate [9, 19, 22]. In this study, the results indicated that within 6 months after the procedure, the Villalta score and quality of life of patients without stenting were lower than those of patients who underwent stent implantation. At subsequent follow-ups, the Villalta score and quality of life of the two groups converged and showed no significant difference.
Stenting may be beneficial and necessary for patients with severe iliac vein obstruction. In this study, only young DVT patients with clear provoking factor were included. For these patients, iliac vein stenosis may not be the direct factor provoking DVT. Therefore, it is notable that the result cannot be generalized to the whole population. For patients with DVT provoked by iliac vein stenosis, stent implantation might be the etiological treatment. Besides, only patients with good venous return underwent ART without stenting. Venous return function of iliac-femoral vein was assessed by the stasis time of the contrast agent whether exceeded 6 s during angiography. Six seconds was referred to the final stage of the femoral vein valvar reflux time phase in venous insufficiency, which was considered persistent reflux [23]. It was used for the first time as an index to evaluate the reflow efficiency of the iliac vein and collateral veins in DVT. Although the most appropriate time is not known, this is a relatively conservative attempt to minimize human-made thrombotic factors in clinical observation.
The limitations of the study should also be mentioned. The relatively small sample size resulted in wider confidence intervals regarding the estimates of the Villalta score and quality of life, and may obscure the differences between two groups. In other words, although current research indicates no significant difference between two groups after 6 months, potential differences may be revealed with the increase in sample size. Therefore, the findings should be interpreted with caution. Besides, during the procedure, we prescribed that the young patients had to undergo stenting when the stenosis of the femoral-iliac vein remained more than 50% and the stasis time of the contrast agent exceeded 6 s after CDT. However, the stricter and more detailed criteria were unknown, which required us to explore steadily and safely. Another limitation was the relatively short follow-up period of this study. The occurrence and development of PTS was a long-term process, and long-term follow-up was important for research on PTS. This study was ongoing, and future results may provide more evidence on this topic. Additionally, this study was subjected to uncontrolled confounding due to the heterogeneous nature of the cohort and the incomplete incorporation of variables, such as the lack of the grade of thrombus clearance. The presence of these confounding may potentially contribute to reduced confidence. Overall, this study was a pilot study, and further randomized controlled studies were needed to verify the conclusions and define more detailed treatment criteria.
Conclusion
Young DVT patients with iliac vein stenosis needed to be treated with caution. Our study indicated that for acute DVT patient with iliac vein stenosis and good venous return, patients underwent thrombectomy combined with stenting had better efficacy compared with patients underwent thrombectomy alone with 6 months, while there was no significant difference in the symptom, signs, and quality of life between two groups after 6 months within a 2-year follow-up. This study provided meaningful guidance for the use of stents in this clinical setting. It was expected that through our and future research, more detailed intervention strategies for young DVT patients with iliac vein stenosis could be developed.
Data Availability
Data are now available from the corresponding author (Xinwu Lu) on reasonable request.
Abbreviations
- ART:
-
AngioJet rheolytic thrombectomy
- CDT:
-
Catheter-directed thrombolysis
- DSA:
-
Digital subtraction angiography
- DVT:
-
Deep-venous thrombosis
- PTS:
-
Postthromobtic syndrome
References
Kahn SR, Comerota AJ, Cushman M, Evans NS, Ginsberg JS, Goldenberg NA, et al. The postthrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2014;130(18):1636–61. https://doi.org/10.1161/CIR.0000000000000130.
Rogers MA, Levine DA, Blumberg N, Flanders SA, Chopra V, Langa KM. Triggers of hospitalization for venous thromboembolism. Circulation. 2012;125(17):2092–9. https://doi.org/10.1161/CIRCULATIONAHA.111.084467.
Zhang Z, Lei J, Shao X, Dong F, Wang J, Wang D, et al. Trends in hospitalization and In-Hospital mortality from VTE, 2007 to 2016, in China. Chest. 2019;155(2):342–53. https://doi.org/10.1016/j.chest.2018.10.040.
Liu G, Liu X, Wang R, Ye K, Yin M, Huang X, et al. Catheter-Directed Thrombolysis of Acute entire limb deep vein thrombosis from below the knee Access: a retrospective analysis of a single-center experience. Catheter Cardiovasc Interv. 2018;91(2):310–7. https://doi.org/10.1002/ccd.27118.
Liu G, Qin J, Cui C, Ye K, Shi H, Liu X, et al. Comparison of direct Iliofemoral Stenting following AngioJet Rheolytic Thrombectomy vs staged Stenting after AngioJet Rheolytic Thrombectomy Plus Catheter-Directed Thrombolysis in patients with Acute Deep vein thrombosis. J Endovasc Ther. 2018;25(1):133–9. https://doi.org/10.1177/1526602817714570.
Stevens SM, Woller SC, Kreuziger LB, Bounameaux H, Doerschug K, Geersing GJ, et al. Antithrombotic therapy for VTE Disease: second update of the CHEST Guideline and Expert Panel Report. Chest. 2021;160(6):e545–e608. https://doi.org/10.1016/j.chest.2021.07.055.
Vedantham S, Goldhaber SZ, Julian JA, Kahn SR, Jaff MR, Cohen DJ, et al. Pharmacomechanical Catheter-Directed Thrombolysis for Deep-Vein thrombosis. N Engl J Med. 2017;377(23):2240–52. https://doi.org/10.1056/NEJMoa1615066.
Mahnken AH, Thomson K, de Haan M, O’Sullivan GJ. CIRSE standards of practice guidelines on iliocaval stenting. Cardiovasc Intervent Radiol. 2014;37(4):889–97. https://doi.org/10.1007/s00270-014-0875-4.
Mazzolai L, Aboyans V, Ageno W, Agnelli G, Alatri A, Bauersachs R, et al. Diagnosis and management of acute deep vein thrombosis: a joint consensus document from the European Society of Cardiology working groups of aorta and peripheral vascular diseases and pulmonary circulation and right ventricular function. Eur Heart J. 2018;39(47):4208–18. https://doi.org/10.1093/eurheartj/ehx003.
Enden T, Haig Y, Klow NE, Slagsvold CE, Sandvik L, Ghanima W, et al. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. Lancet. 2012;379(9810):31–8. https://doi.org/10.1016/S0140-6736(11)61753-4.
Pouncey AL, Gwozdz AM, Johnson OW, Silickas J, Saha P, Thulasidasan N, et al. AngioJet Pharmacomechanical Thrombectomy and Catheter Directed Thrombolysis vs. Catheter Directed Thrombolysis alone for the treatment of Iliofemoral Deep Vein thrombosis: a single Centre Retrospective Cohort Study. Eur J Vasc Endovasc Surg. 2020;60(4):578–85. https://doi.org/10.1016/j.ejvs.2020.05.006.
Foegh P, Jensen LP, Klitfod L, Broholm R, Baekgaard N, editors. ‘s Choice - Factors Associated with Long-Term Outcome in 191 Patients with Ilio-Femoral DVT Treated With Catheter-Directed Thrombolysis. Eur J Vasc Endovasc Surg. 2017;53(3):419 – 24. https://doi.org/10.1016/j.ejvs.2016.12.023.
Taha MAH, Busuttil A, Bootun R, Thabet BAH, Badawy AEH, Hassan HA, et al. A clinical guide to deep venous stenting for chronic iliofemoral venous obstruction. J Vasc Surg Venous Lymphat Disord. 2022;10(1):258–66e1. https://doi.org/10.1016/j.jvsv.2020.12.087.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X.
Ye K, Lu X, Jiang M, Yang X, Li W, Huang Y, et al. Technical details and clinical outcomes of transpopliteal venous stent placement for postthrombotic chronic total occlusion of the iliofemoral vein. J Vasc Interv Radiol. 2014;25(6):925–32. https://doi.org/10.1016/j.jvir.2014.02.031.
Kahn SR, Lamping DL, Ducruet T, Arsenault L, Miron MJ, Roussin A, et al. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol. 2006;59(10):1049–56. https://doi.org/10.1016/j.jclinepi.2005.10.016.
Naess IA, Christiansen SC, Romundstad P, Cannegieter SC, Rosendaal FR, Hammerstrom J. Incidence and mortality of venous thrombosis: a population-based study. J Thromb Haemost. 2007;5(4):692–9. https://doi.org/10.1111/j.1538-7836.2007.02450.x.
Notten P, Ten Cate H, Ten Cate-Hoek AJ. Postinterventional antithrombotic management after venous stenting of the iliofemoral tract in acute and chronic thrombosis: a systematic review. J Thromb Haemost. 2021;19(3):753–96. https://doi.org/10.1111/jth.15197.
Khan F, Tritschler T, Kahn SR, Rodger MA. Venous thromboembolism. Lancet. 2021;398(10294):64–77. https://doi.org/10.1016/S0140-6736(20)32658-1.
Iorio A, Kearon C, Filippucci E, Marcucci M, Macura A, Pengo V, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010;170(19):1710–6. https://doi.org/10.1001/archinternmed.2010.367.
Khan F, Rahman A, Carrier M, Kearon C, Weitz JI, Schulman S, et al. Long term risk of symptomatic recurrent venous thromboembolism after discontinuation of anticoagulant treatment for first unprovoked venous thromboembolism event: systematic review and meta-analysis. BMJ. 2019;366:l4363. https://doi.org/10.1136/bmj.l4363.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the european respiratory society (ERS). Eur Heart J. 2020;41(4):543–603. https://doi.org/10.1093/eurheartj/ehz405.
Liu X, Zheng G, Ye B, Chen W, Xie H, Zhang T. Factors related to the size of venous leg ulcers: a cross-sectional study. Med (Baltim). 2019;98(5):e14389. https://doi.org/10.1097/MD.0000000000014389.
Acknowledgements
Not applicable.
Funding
This study is funded by Clinical Research Program of Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine (JYLJ201810), Shanghai Municipal Health Commission Clinical Research Project (202240145), and the National Natural Science Foundation of China (82170488, and 82170509).
Author information
Authors and Affiliations
Contributions
Xiaobing Liu, Xinwu Lu, Guang Liu contributed to the study concept and research design. Hongji Pu, Jumin Song, Zhijun He; Fuyin Wang, Sheng Huang, Minyi Yin, Weimin Li contributes to performing the research. Hongji Pu, Xinwu Lu, Guang Liu participated in statistical analysis and interpretation of data. Hongji Pu and Guang Liu drafted the manuscript. All authors revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the participating hospitals and registered in the Chinese Clinical Trial Registry (Registration Number: ChiCTR2200056073).
Consent for publication
Written informed consent was obtained from all the participants prior to the data collection of this study.
Competing interests
The authors declare that there is no conflict of interest regarding the publication of this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pu, H., Song, J., He, Z. et al. Assessing outcomes after thrombectomy with or without iliac vein stenting for young provoked DVT patients with iliac vein stenosis. Thrombosis J 21, 96 (2023). https://doi.org/10.1186/s12959-023-00537-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-023-00537-9