Abstract
Cardiocerebrovascular diseases (CVDs) are the leading cause of death worldwide, consuming huge healthcare budget. For CVD patients, the prompt assessment and appropriate administration is the crux to save life and improve prognosis. Thrombolytic therapy, as a non-invasive approach to achieve recanalization, is the basic component of CVD treatment. Still, there are risks that limits its application. The objective of this review is to give an introduction on the utilization of thrombolytic therapy in cardiocerebrovascular blockage diseases, including coronary heart disease and ischemic stroke, and to review the development in risk assessment of thrombolytic therapy, comparing the performance of traditional scales and novel artificial intelligence-based risk assessment models.
Similar content being viewed by others
Introduction
Cardiocerebrovascular diseases (CVDs) are pathological conditions involving the cardiovascular system, which are the leading cause of death worldwide, and more than 80% CVD-caused deaths are due to CHD and stroke [1]. According to data from WHO, in 2019, about 17.9 million people died from CVDs, accounting for 32% of the global total. In the United States, the main type of CVDs was CHD, with a proportion of 41.3%, followed by stroke (17.2%) [2]. CHDs are the stenosis or obstruction of the coronary artery, leading to myocardial ischemia, hypoxia and even necrosis. One of the most important characteristics of CHD is atherosclerosis. (The pathogenesis of atherosclerosis is shown in Additional file 1). According to their stability, atheromatous plaques are divided into stable plaques and unstable plaques. When the unstable plaque ruptures or erodes, subendothelial collagen, lipid core, and procoagulants like tissue factor and von Willebrand factor are exposed to the blood circulation, which rapidly promotes platelets to adhere to the vessel wall and subsequently aggregate, contributing to acute thrombosis. Then the coronary artery is completely blocked, and later the ischemia and hypoxia of the myocardium in the corresponding area emerge, resulting in myocardial infarction characterized by ST-segment elevation (STEMI), which is a serious type of acute coronary syndrome (ACS).
Another fatal type of CVD, stroke, is divided into hemorrhagic stroke and ischemic stroke based on its pathogenesis. Ischemic stroke is the main type of stroke, accounting for 85% of strokes. It is defined as a result of thrombosis or embolism that blocks cerebral vessels in a specific area of the brain, causing a sudden loss of blood flow to the corresponding area of the brain and leading to neurological dysfunction [3]. Unlike in situ thrombosis in ACS, plaque ruptures in extracranial cervical arteries mostly result in distal embolization of the thrombus to the brain (arterial embolism), while the consequences of intracranial atherosclerotic plaque rupture are similar to those of ACS, namely bringing about in situ vessel occlusion [4]. Atherosclerosis and the build-up of plaque constrict blood vessels and reduce blood flow to the brain region, leading to severe stress and cell death due to hypoxia in the ischemic region.
In conclusion, thrombosis is the common pathogenetic process of myocardial infarction and ischemic stroke. Thus, thrombolysis plays a significant role in the treatment of these two diseases.
Thrombolytic therapy
The application of thrombolytic therapy in CVDs
Thrombolytic therapy, or thrombolysis, is to use the thrombolytic agents (TAs) to destroy or dissolve the thrombi in vessels. It is applied in various thrombotic or embolic CVDs, ranging from venous thromboembolism (VTE), acute ischemic stroke (AIS), acute myocardial infarction (AMI), to prosthetic valve thrombosis (PVT) [5].
As the mechanism of AMI and AIS is the acute artery occlusion which leads to ischemic necrosis of the tissue in its supplying area, to achieve recanalization and reperfusion as soon as possible is vital for avoiding irreversible damage and improving outcomes. Thrombolysis and interventional therapy, such as thrombectomy and stent implantation, are the two major approaches. For STEMI, though primary percutaneous coronary intervention (PCI) is a prior strategy [6, 7], it is hard to achieve, especially in regions with limited medical resources and emergency services, while it requires equipment for angiographic guidance and the evidence-based timeframe is restricted. When early PCI is not feasible, the application of thrombolysis before being transferred to facilities where catheterization is available provides an opportunity for early reperfusion at the symptom onset. The TRANSFER-AMI study has shown that, among the 1059 high-risk STEMI patients those who were treated with tenecteplase and then transferred for PCI within 6 h have a lower occurrence of endpoint composited of death, reinfarction, recurrent ischemia, new or worsening congestive heart failure, or cardiogenic shock within 30 days [8].
If PCI cannot be performed within the guideline-recommended timeframe, which is approximately 120 min, fibrinolytic drugs should be administered at full dose for patients under 75 years old, with the exclusion of contraindications [9]. The contraindications to thrombolytic therapy include uncontrolled hypertension, prior intracranial hemorrhage, history of head trauma within 3 months, intracranial surgery within 2 months, brain malignancy, cerebrovascular malformation, aortic dissection, active or recent bleeding, bleeding diatheses [5].
Thrombolytic agents
Thrombolytic agents are natural or artificial substances that contribute to the fibrinolytic process, catalyzing the conversion of plasminogen to plasmin, which can degrade the essential component of thrombus, fibrin, into fibrin degradation products (FDPs). Features of several commonly used TAs are compared in Additional file 2 [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25].
According to the time of discovery and characteristics, TAs are divided into 3 generations. In addition, TAs can be categorized as either “fibrin specific” or “non-fibrin specific”. The fibrin-specific TAs, including the second-and third-generation TAs, selectively activate the plasminogen that are bound to fibrin. Therefore, they pose a lower risk of complications attributed to systemic fibrinolytic activation. The first-generation TAs are streptokinase (SK) and urokinase (UK). The second-generation TAs, represented by recombinant tissue plasminogen activator (rt-PA) and single-chain urokinase (scu-PA), share common characteristics: They are to a certain extent fibrin specific but require large therapeutic dose and continuous intravenous infusion due to the short half-life. Among the new candidates of third-generation TAs, tenecteplase and reteplase are the two TAs approved by FDA for clinical treatment. They have a prolonged half-life, which allows them to be administered as a bolus dose rather than an infusion. Several clinical trials including RAPID II [18], PAPID II [19] and INJECT [25] have demonstrated that compared with other TAs such as rt-PA and SK, reteplase achieved a higher coronary artery patency rate without increasing the risk of bleeding or other adverse events.
The way of delivering TAs includes systematic delivery, Intracoronary (IC) thrombolysis, nanocarriers and so on. As a traditional way to deliver TAs, systematic delivery has the advantages of being convenient and affordable, while its limitations are non-specific bio-distribution and the risk of bleeding complications. IC thrombolysis is developed in 1990s as an adjunctive treatment to angioplasty, aimed at decreasing the risk of distal thromboembolism [26]. Through the direct administration of TAs in coronary artery, site-specific TA concentrations can be reached at high levels with fewer doses, and therefore posing less danger of systematic hemorrhage. Nanocarrier is a novel approach of drug delivery, which is still under clinical investigation [27, 28]. It conjugates with TAs, then under the trigger of an internal or external stimulus the conjugation disassembles at the thrombus site, thereby the concentration of TAs is increased.
Risk prediction
Clinical risks
As illustrated above, prompt treatment with fibrinolytic agents, such as alteplase, is an effective therapy for AIS [29] and STEMI [30], reducing mortality and improving recovery [30, 31]. However, it is associated with risks, which generally include in-hospital death (from any causes), recurrent occlusion, reperfusion injury, and immunologic and hemorrhagic complications.
Unsurprisingly, hemorrhage is the most common complication, since TAs may not only dissolve the protective blood clots, but lead to secondary hyperfibrinolysis, hypofibrinogenemia, platelet dysfunction, and other hemostatic defects [32] as well. Depending on site and severity, hemorrhagic complications can be further divided into several categories, among which intracranial hemorrhage (ICH) and major bleeding are most life-threatening and require specific treatment. The reported rates of post-thrombolysis ICH in AIS patients ranged from 0.2% to 1.0%, while the rate of major bleeding could reach 15% [33]. Since the diagnosis criteria might vary in different studies, these absolute rates are for reference only.
The allergic reactions are more often seen in patients given streptokinase as it is a heterologous protein. Acute anaphylaxis is severe but unusual, which may manifest as itching and redness of the skin, vasogenic edema, bronchospasm, dyspnea, hypotension, arrhythmia and shock.
Before applying thrombolytic therapy, in order to select the appropriate patient, reduce the risks of death or serious complications, and to get prepared in advance, it is necessary to carry out risk assessments and take the risk–benefit ratio into consideration.
Risk scores
Clinical prediction scores for risk stratification and outcomes estimation of CVD patients have been developed in the past few decades. The regularly used risk scores are listed in Additional file 3 [34,35,36,37,38,39,40,41,42,43]. Though the scales for different CVDs vary, they have multiple indicators in common. Undoubtedly, the incidence of complications is correlated with the dose and type of TA applied. Besides, a variety of factors may play a role, including patient characteristics (age, gender, CVD history), symptom severity, comorbidities (hypertension on admission, diabetes mellitus, atrial fibrillation, coagulation defects), other treatments, etc. [29, 44].
Regarding ACS, the TIMI risk score and the GRACE score are regarded as the most universally used scales for ischemic risk stratification and prognosis prediction. Their prominent advantage is the easy bedside application attributed to the simple calculation method. There are two main versions of TIMI risk scores [34, 38] for STEMI and UA/NSTEMI respectively. They both have reliable identification of high-risk patients and excellent discriminatory power but are weak at generalization. Eagle KA et al. [37] designed the GRACE model, which has higher accuracy (c statistics 0.81) and is enabled to predict the in-hospital and 6-month mortality of the entire spectrum of ACS patients, including those with ST elevation or depression [45]. Hence GRACE can be easier generalized. Nevertheless, according to the original study, it is not applicable to patients being observed in an emergency department [37]. In contrast to the massive bleeding risk scores for PCI and antithrombotic therapy, those scores for thrombolysis are currently few.
When it comes to AIS, the NIHSS score [46], developed and validated by Thomas et al. in 1989, is used to determine stroke severity, treatment and prognosis [47]. This concise scale can be completed in 6.6 min, providing a quantitative measure of critical ingredients of a standard neurological examination [46, 48], and has become one of the predictors of post-thrombolysis ICH. The MSS score [40] is a simple clinical four-point risk score that combines age, NIHSS score, glucose and platelet count together. However, the original study only included 481 patients, compromising its validity. M Lou et al. [41] constructed the HAT score, a quick and easy-to-perform five-point scale considering the pretreatment NIHSS score, CT findings, DM history and blood glucose. Its limitations are that this score was developed in retrospective studies, the sample size was also inadequate. Consequently, the HAT score should be examined in larger cohorts and prospective studies before utilized in clinical decision making [41]. Compared with the HAT score, the SITS-ICH risk score [42] was based on a larger data set of 31,627 patients, and requires neither the measurement of blood platelet count (needed in the MSS score), nor the manifest infarct size on initial imaging (needed in the HAT score). Therefore, it can be more easily and immediately calculated. The DRAGON score [49] has a scoring similar to HAT score and uses the prestroke modified Rankin Scale (mRS) as one of the predicators, was originally developed to assess the short-term functional outcome, but has since been used to assess intracranial hemorrhagic risk. The initial study of GRASPS score [43] was the first to report that male sex and Asian race were independent risk factors. This well-validated score is an excellent clinical tool to assess the risk of intravenous tPA-related symptomatic ICH in patients treated with tPA within 3 h of stroke onset, but it cannot provide an indication on how much benefit patients would gain from this strategy. Likewise, none of these risk scores should be used as a justification of withholding thrombolytic therapy, because they are incapable of demonstrating the harm is greater than the benefit [40,41,42,43].
Application of risk prediction in post-thrombolysis patients
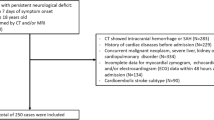
Clinical studies are carried out to evaluate whether the scores or prediction models are reliable in risk prediction, here we sorted the studies conducted in recent years to give a clear and objective comparison on them (Table 1 [50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66] was shown at the end of the text). Studies which did not give an explicit statement that patients had received thrombolytic therapy were excluded.
As for AMI, very few research discussed the performance of different risk scores in post-thrombolysis patients. Steyerberg EW et al. [54] compared the accuracy of Belgium model, GISS-II, TIMI and GUSTO-I risk score for the prediction of the all-cause mortality at 30-day in 40,830 patients, GUSTO-I nomogram reached the highest AUC of 0.827. Besides, researchers have made attempts to discover new risk factors. Brewster LM et al. [50] applied a new multivariant model, with CK and age as predictors, to evaluate the risk of major bleeding and composite endpoint in 1473 patients, and the AUC reached 0.80 and 0.75, respectively, which was higher than other current scales. In addition, Hassan AKM et al. [53] combined GRACE and 6-min walk test in the evaluation of major adverse cardiovascular events (MACE), which gained a satisfying result with the OR of 8.14, higher than that of GRACE (OR = 7.03) and TIMI (OR = 3.08) alone. In general, GUSTO-I and GRACE risk scores performed better in the prediction of post-thrombolysis MACE. However, considering the lack of relevant studies and the potential bias between studies, a credible conclusion yet cannot be drawn. Compared with TIMI score, the scoring criteria of GUSTO-I and GRACE scores are more detailed, especially in the segmentation of age and heart rate. Despite the vital signs, the history of CVDs and some laboratory indicators are included as well. GUSTO-I score particularly takes ventricular function into consideration, by adding EF into the metrics. To further improve the accuracy of risk assessment, introducing more indicators seems to be a reasonable approach. Nevertheless, this is very likely to make the calculation more complicated, and the laboratory examination is time consuming, which is not feasible when an immediate risk assessment is in demand.
For post-thrombolysis AIS patients, one of the most life-threatening situations is hemorrhagic transformation (HT), which was often defined as symptomatic intracerebral hemorrhage (SICH). Traditional risk scores, including SEDAN, HAT, SITS-ICH, GRAPS, MSS, SPAN-100, and DRAGON, were utilized in HT prediction and their efficacy were validated by multiple clinical retrospective studies. Since each risk score was developed using different definitions to classify SICH, the variation of definitions across studies may have an impact on the accuracy. According to the initial study, the SEDAN and HAT scores used European Cooperative Acute Stroke Study II (ECASS II) definition, the GRASPS, MSS and SPAN-100 scores used the National Institute of Neurological Disorder and Stroke (NINDS) definition, while the SITS score used the SITS-MOST definition. Overall, the DRAGON score has a relatively higher predictive value, as its AUCs in different studies were all above 0.7 [55, 56, 64], with a median of 0.77. The HAT score also shows high reliability, whose AUC fluctuated between 0.64 and 0.78 [55,56,57,58,59, 62, 64]. In the research of Chang X et al. [64], which included 298 patients, the ASPECTS, DRAGON, HAT, and SEDAN scores achieved an AUC of 0.895, 0.877, 0.777, and 0.764, respectively. These scores all use the signs on admission CT scan as one of the scoring metrics, which may explain their better predictability. The SEDAN, MSS, SITS-ICH, and GRASPS scores had similar risk assessment capabilities, with the median AUC of 0.67, 0.68, 0.68, and 0.67, respectively. Among all the mentioned scores, SPAN-100 had the least satisfactory result. Sung SF et al. [59] applied SPAN-100 index in 548 patients and the AUC to predict SICH per NINDS, ECASS-II and SITS-MOST was only 0.56, 0.55 and 0.57, respectively.
Above all, thrombolysis risk scores or prediction models for AMI and AIS varied from each other in feature and accuracy. It is still hard to determine which one is the best in the complicated clinical conditions, especially with the inputs of multi-dimensional datatype and increasing data. Thus, more efficient and accurate approaches to make risk assessment is in need.
Artificial Intelligence (AI) in risk prediction
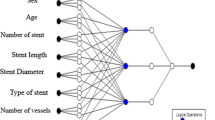
Artificial intelligence (AI) refers to a branch of computer science that is developed to perform tasks that normally require human intelligence, perceiving environment and mimicking human cognitive behavior [70, 71]. Machine learning is one of the technical foundations of AI, which involves the automatic development of algorithms to identify patterns or groups in data [71]. When dealing with complex or massive data, higher accuracy can be achieved through machine learning over the traditional statistical methods. Deep learning, as a novel technique, uses multilayer neural networks to learn datasets with multiple levels of abstraction [72]. The representation of the input signal is learned by the network itself through training [73], and some deep learning models do not require manual supervision [74]. In this way, risks of systematic or random errors introduced by human factors are minimized. Deep convolutional neural networks (CNNs) and deep recurrent neural networks (RNNs) are two typical deep neural networks, specialized for specific learnings and can accomplish more complicated tasks through adequate combination [75]. With its high efficiency and accuracy, machine learning is nowadays increasingly applied in clinical processes, including diagnosis, treatment, prognosis and management of multiple diseases [76]. Good application prospect was also seen in the field of cardiocerebrovascular. Ambale V et al. [77] utilized random forest technique in the prediction of 6 cardiovascular events and reached higher prediction accuracy than other established risk scores. Johnson KM et al. [78] used 5 machine learning methods to build models of vessel features, which better discriminated patients with subsequent adverse outcomes compared with conventional scores.
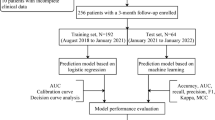
A number of researchers were devoted to the application of machine learning algorithms in post-thrombolysis risk prediction, identifying the potential predictors from various patient characteristics and developing new models (Table 2 [79,80,81,82,83,84,85,86,87,88,89,90,91,92] was shown at the end of the text).
The effectiveness of these models was validated through the comparison with traditional scores. In several studies, new nomograms were generated through logistic regression analysis, among which that developed by Zhang K et al. [83] reached a high AUC of 0.889 when predicting the risk of HT in 178 patients. Aziz F et al. [79] applied random forest, support vector machine and logistic regression models to predict short- and long-term mortality among heterogenous Asian STEMI patients. AUCs from 0.73 to 0.90 are achieved, with the highest AUCs of 0.89, 0.90 and 0.84 for hospitalization, 30 days, and 1 year respectively, outperforming TIMI risk score whose AUCs are 0.81,0.80 and 0.76. When it comes to AIS, in most studies AI models showed better prediction ability of hemorrhagic complications than traditional risk scores or statistically based models. Some researchers extracted radiomic features and utilized machine learning to build radiomics models. Meng Y et al. [81] extracted 5,400 radiomic features from 20 normal and abnormal regions of interest (ROIs) of MRI images among 71 patients, used the least absolute shrinkage and selection operator (LASSO) regression for feature selection, and constructed a radiomics model through RF, which was combined with 16 screened clinical factors with better support. The AUC with All-ROIs reached 0.871 and was further promoted to 0.91 when combined with other clinical factors. In addition to HT prediction after thrombolysis, radiomics-based models can also evaluate hemorrhage expansion well. Liu J et al. [87] applied LASSO regression to identify five optimal radiomic image features on non-contrast-enhanced CT (NECT) as predictors, and developed a quantitative radiological score with a maximum AUC of 0.91. Besides, some researchers have also utilized deep learning to construct thrombolytic risk assessment models for AIS patients. To predict 24-h and 90-day functional outcomes better, Bacchi S et al. [90] constructed a new prediction model among 204 stroke patients, using CNN and artificial neural networks (ANN), and found that a combination of CNN and ANN based on CT image and clinical data had the best performance, with the highest AUC of 0.70 and 0.75, respectively. Wang F et al. [89] have used logistic regression (LR), neutral network, support-vector machine (SVM), random forest (RF) and adaptive boosting (AdaBoost) to develop five machine learning models in 2237 cases for post-thrombolysis sICH prediction, screening out the five most valuable input factors (age, AF, glucose, NIHSS score and door-to-need time). The three-layer neural network model performed best and its AUC was 0.82. Among 40 patients, Chen Z et al. [88] have proposed a new prediction model named AUNet, which combined the features of an adaptive linear ensemble model (ALEM) and a deep U-Net network with an accelerated non-local module (U-NL-Net), to predict infarct volumes for AIS patients with or without recanalization, and the AUCs were 0.898 and 0.875, respectively.
AI models have obvious advantages in post-thrombolysis risk prediction, including high efficiency, higher accuracy when dealing with massive and multi-dimensional data, the capacity of comparing different methodologies on the same database, suitability for multi-ethnic population and so on. Undeniably, there are certain shortcomings, such as poor interpretability, weak generalization, and the unsatisfactory accuracy of some models. To solve these problems, efforts should be made in the improvement of algorithms, the enhancement of interpretability analysis, and the establish of multi-centered and normalized databases.
Conclusion
Among CVDs, blockage diseases such as CHD and stroke are the leading cause of death, imposing a huge burden to the public health. The key treatment is to recanalize the embolized vascular and restore blood supply in the ischemic area. Thrombolytic therapy is a basic therapy in the recanalization strategy, whose advantages lays in rapidity, economy and non-invasiveness. However, the thrombolysis-related clinical risks such as hemorrhagic complications, futile recanalization and reocclusion, restrict the use of thrombolysis, yet make the pretreatment risk assessment necessary. New risk scores and AI-based prediction models are therefore continually developed and modified. It is still hard to say which risk score can achieve the highest accuracy, but with the continuous improvement of risk prediction, the application of thrombolysis will be relatively safer, which definitely brings great benefits to patients.
Availability of data and materials
Not applicable.
References
World Health Organization. Cardiovascular diseases (CVDs). Published June 3, 2022. Accessed 3 Jun 2022. https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1.
Cardiovascular diseases (CVDs). World Health Organization. 2022. https://www.who.int/news-room/factsheets/detail/cardiovascular-diseases-(cvds).
Phipps MS, Cronin CA. Management of acute ischemic stroke. BMJ. 2020;368. https://doi.org/10.1136/bmj.l6983.
Musuka TD, Wilton SB, Traboulsi M, Hill MD. Diagnosis and management of acute ischemic stroke: Speed is critical. CMAJ. 2015;187(12):887–93. https://doi.org/10.1503/cmaj.140355.
Proctor P, Leesar MA, Chatterjee A. Thrombolytic Therapy in the Current ERA: Myocardial Infarction and Beyond. Curr Pharm Des. 2017;24(4). https://doi.org/10.2174/1381612824666171227211623.
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review of 23 randomised trials. Lancet. 2003;361(9351). https://doi.org/10.1016/S0140-6736(03)12113-7.
Thrane PG, Kristensen SD, Olesen KKW, et al. 16-year follow-up of the Danish Acute Myocardial Infarction 2 (DANAMI-2) trial: primary percutaneous coronary intervention vs. fibrinolysis in ST-segment elevation myocardial infarction. Eur Heart J. 2020;41(7):847–54. https://doi.org/10.1093/eurheartj/ehz595.
Cantor WJ, Fitchett D, Borgundvaag B, et al. Routine Early Angioplasty after Fibrinolysis for Acute Myocardial Infarction. N Engl J Med. 2009;360(26). https://doi.org/10.1056/nejmoa0808276.
Armstrong PW, Gershlick AH, Goldstein P, et al. Fibrinolysis or Primary PCI in ST-Segment Elevation Myocardial Infarction. N Engl J Med. 2013;368(15). https://doi.org/10.1056/nejmoa1301092.
Verstraete M, Collen D. Pharmacology of thrombolytic drugs. J Am Coll Cardiol. 1986;8(6). https://doi.org/10.1016/S0735-1097(86)80005-5.
Cannon CP, McCabe CH, Michael Gibson C, et al. TNK-tissue plasminogen activator in acute myocardial infarction: Results of the thrombolysis in myocardial infarction (TIMI) 10a dose-ranging trial. Circulation. 1997;95(2). https://doi.org/10.1161/01.CIR.95.2.351.
Seifried E, Müller MM, Martin U, König R, Hombach V. Bolus Application of a Novel Recombinant Plasminogen Activator in Acute Myocardial Infarction Patients: Pharmacokinetics and Effects on the Hemostatic System. Ann N Y Acad Sci. 1992;667(1). https://doi.org/10.1111/j.1749-6632.1992.tb51641.x.
The GUSTO Angiographic Investigators. The Effects of Tissue Plasminogen Activator, Streptokinase, or Both on Coronary-Artery Patency, Ventricular Function, and Survival after Acute Myocardial Infarction. N Engl J Med. 1993;329(22):1615–22. https://doi.org/10.1056/nejm199311253292204.
Neuhaus KL, Tebbe U, Gottwik M, et al. Intravenous Recombinant Tissue Plasminogen Activator (rt-PA) and Urokinase in Acute Myocardial Infarction: Results of the German Activator Urokinase Study (GAUS). J Am Coll Cardiol. 1988;12(3). https://doi.org/10.1016/S0735-1097(88)80040-8.
Califf RM, Topol EJ, Stack RS, et al. Evaluation of combination thrombolytic therapy and timing of cardiac catheterization in acute myocardial infarction: Results of thrombolysis and angioplasty in myocardial infarction - Phase 5 randomized trial. Circulation. 1991;83(5). https://doi.org/10.1161/01.CIR.83.5.1543.
Chesebro JH, Knatterud G, Roberts R, et al. Thrombolysis in myocardial infarction (TIMI) trial, phase I: A comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987;76(1). https://doi.org/10.1161/01.CIR.76.1.142.
Cannon CP, Gibson CM, McCabe CH, et al. TNK-tissue plasminogen activator compared with front-loaded alteplase in acute myocardial infarction: Results of the TIMI 10B trial. Circulation. 1998;98(25). https://doi.org/10.1161/01.CIR.98.25.2805.
Smalling RW, Bode C, Kalbfleisch J, et al. More rapid, complete, and stable coronary thrombolysis with bolus administration of reteplase compared with alteplase infusion in acute myocardial infarction. Circulation. 1995;91(11). https://doi.org/10.1161/01.CIR.91.11.2725.
Bode C, Smalling RW, Berg G, et al. Randomized comparison of coronary thrombolysis achieved with double- bolus reteplase (recombinant plasminogen activator) and front-loaded, accelerated alteplase (recombinant tissue plasminogen activator) in patients with acute myocardial infarction. Circulation. 1996;94(5). https://doi.org/10.1161/01.CIR.94.5.891.
Bar FW, Meyer J, Vermeer F, et al. Comparison of saruplase and alteplase in acute myocardial infarction. SESAM Study Group. The Study in Europe with Saruplase and Alteplase in Myocardial Infarction. Am J Cardiol. 1997;79(6).
Vermeer F, Bösl I, Meyer J, et al. Saruplase is a safe and effective thrombolytic agent; Observations in 1698 patients: Results of the PASS study. J Thromb Thrombolysis. 1999;8(2). https://doi.org/10.1023/A:1008967219698.
Tebbe U, Michels R, Adgey J, et al. Randomized, double-blind study comparing saruplase with streptokinase therapy in acute myocardial infarction: the COMPASS Equivalence Trial. Comparison Trial of Saruplase and Streptokinase (COMASS) Investigators. J Am Coll Cardiol. 1998;31(3).
Wall TC, Phillips HR, Stack RS, et al. Results of high dose intravenous urokinase for acute myocardial infarction. Am J Cardiol. 1990;65(3). https://doi.org/10.1016/0002-9149(90)90072-9.
GUSTO III Investigators. A Comparison of Reteplase with Alteplase for Acute Myocardial Infarction. N Engl J Med. 1997;337(16):1118–23. https://doi.org/10.1056/nejm199710163371603.
Wilcox RG. Randomised, double-blind comparison of reteplase double-bolus administration with streptokinase in acute myocardial infarction (INJECT): trial to investigate equivalence. International Joint Efficacy Comparison of Thrombolytics. Lancet. 1995;346(8971). https://doi.org/10.1016/S0140-6736(95)92224-5.
Tiefenbrunn AJ. Intracoronary thrombolysis. Chest. 1992;101(6). https://doi.org/10.1378/chest.101.6.1484.
Pawlowski CL, Li W, Sun M, et al. Platelet microparticle-inspired clot-responsive nanomedicine for targeted fibrinolysis. Biomaterials. 2017;128. https://doi.org/10.1016/j.biomaterials.2017.03.012.
Zhong Y, Gong WJ, Gao XH, et al. Synthesis and evaluation of a novel nanoparticle carrying urokinase used in targeted thrombolysis. J Biomed Mater Res A. 2020;108(2). https://doi.org/10.1002/jbm.a.36803.
Tanne D, Kasner SE, Demchuk AM, et al. Markers of increased risk of intracerebral hemorrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice: The multicenter rt-PA acute stroke survey. Circulation. 2002;105(14). https://doi.org/10.1161/01.CIR.0000012747.53592.6A.
Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14). https://doi.org/10.1093/eurheartj/ehaa575.
Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2014;2014(7). https://doi.org/10.1002/14651858.CD000213.pub3.
Sane DC, Califf RM, Topol EJ, Stump DC, Mark DB, Greenberg CS. Bleeding during thrombolytic therapy for acute myocardial infarction: mechanisms and management. Ann Intern Med. 1989;111(12). https://doi.org/10.7326/0003-4819-111-12-1010.
Califf RM, Fortin DF, Tenaglia AN, Sane DC. Clinical risks of thrombolytic therapy. Am J Cardiol. 1992;69(2). https://doi.org/10.1016/0002-9149(92)91168-4.
Morrow DA, Antman EM, Charlesworth A, et al. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An Intravenous nPA for Treatment of Infarcting Myocardium Early II trial substudy. Circulation. 2000;102(17). https://doi.org/10.1161/01.CIR.102.17.2031.
Amin ST, Morrow DA, Braunwald E, et al. Dynamic TIMI risk score for STEMI. J Am Heart Assoc. 2013;2(1). https://doi.org/10.1161/JAHA.112.003269.
Califf RM, Pieper KS, Kerry LL, et al. Prediction of 1-year survival after thrombolysis for acute myocardial infarction in the global utilization of streptokinase and TPA for occluded coronary arteries trial. Circulation. 2000;101(19). https://doi.org/10.1161/01.CIR.101.19.2231.
Eagle KA, Lim MJ, Dabbous OH, et al. A validated prediction model for all forms of acute coronary syndrome estimating the risk of 6-month postdischarge death in an international registry. J Am Med Assoc. 2004;291(22). https://doi.org/10.1001/jama.291.22.2727.
Antman EM, Cohen M, Bernink PJLM, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. J Am Med Assoc. 2000;284(7). https://doi.org/10.1001/jama.284.7.835.
Subherwal S, Bach RG, Chen AY, et al. Baseline Risk of Major Bleeding in Non–ST-Segment–Elevation Myocardial Infarction. Circulation. 2009;119(14). https://doi.org/10.1161/circulationaha.108.828541.
Cucchiara B, Tanne D, Levine SR, Demchuk AM, Kasner S. A Risk Score to Predict Intracranial Hemorrhage After Recombinant Tissue Plasminogen Activator for Acute Ischemic Stroke. J Stroke Cerebrovasc Dis. 2008;17(6). https://doi.org/10.1016/j.jstrokecerebrovasdis.2008.03.012.
Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: A simple grading scale for predicting hemorrhage after thrombolysis. Neurology. 2008;71(18). https://doi.org/10.1212/01.wnl.0000330297.58334.dd.
Mazya M, Egido JA, Ford GA, et al. Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase: Safe Implementation of Treatments in Stroke (SITS) symptomatic intracerebral hemorrhage risk score. Stroke. 2012;43(6). https://doi.org/10.1161/STROKEAHA.111.644815.
Menon BK, Saver JL, Prabhakaran S, et al. Risk score for intracranial hemorrhage in patients with acute ischemic stroke treated with intravenous tissue-type plasminogen activator. Stroke. 2012;43(9). https://doi.org/10.1161/STROKEAHA.112.660415.
van de Werf F, Barron H v., Armstrong PW, et al. Incidence and predictors of bleeding events after fibrinolytic therapy with fibrin-specific agents: A comparison of TNK-tPA and rt-PA. Eur Heart J. 2001;22(24). https://doi.org/10.1053/euhj.2001.2686.
Anderson JL. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;127(4). https://doi.org/10.1161/CIR.0b013e3182742cf6.
Brott T, Adams HP, Olinger CP, et al. Measurements of acute cerebral infarction: A clinical examination scale. Stroke. 1989;20(7). https://doi.org/10.1161/01.STR.20.7.864.
Garavelli F, Ghelfi AM, Kilstein JG. Usefulness of NIHSS score as a predictor of non-neurological in-hospital complications in stroke. Med Clin (Barc). 2021;157(9). https://doi.org/10.1016/j.medcli.2020.07.034.
Appelros P, Terént A. Characteristics of the National Institute of Health Stroke Scale: Results from a population-based stroke cohort at baseline and after one year. Cerebrovasc Dis. 2004;17(1). https://doi.org/10.1159/000073894.
Strbian D, Meretoja A, Ahlhelm FJ, et al. Predicting outcome of IV thrombolysis-treated ischemic stroke patients: The DRAGON score. Neurology. 2012;78(6):427–32. https://doi.org/10.1212/WNL.0b013e318245d2a9.
Brewster LM, Fernand J. Creatine kinase during non-ST-segment elevation acute coronary syndromes is associated with major bleeding. Open Heart. 2020;7(2). https://doi.org/10.1136/openhrt-2020-001281.
Chotechuang Y, Phrommintikul A, Kuanprasert S, et al. GRACE score and cardiovascular outcomes prediction among the delayed coronary intervention after post-fibrinolytic STEMI patients in a limited PCI-capable hospital. Open Heart. 2020;7(1). https://doi.org/10.1136/openhrt-2019-001133.
Chotechuang Y, Phrommintikul A, Muenpa R, et al. The prognostic utility of GRACE risk score in predictive cardiovascular event rate in STEMI patients with successful fibrinolysis and delay intervention in non PCI-capable hospital: A retrospective cohort study. BMC Cardiovasc Disord. 2016;16(1). https://doi.org/10.1186/s12872-016-0383-3.
Hassan AKM, Dimitry SR, Agban GW. Can exercise capacity assessed by the 6 minute walk test predict the development of major adverse cardiac events in patients with STEMI after fibrinolysis? PLoS One. 2014;9(6). https://doi.org/10.1371/journal.pone.0099035.
Steyerberg EW, Eijkemans MJC, Boersma E, Habbema JDF. Equally valid models gave divergent predictions for mortality in acute myocardial infarction patients in a comparison of logical regression models. J Clin Epidemiol. 2005;58(4). https://doi.org/10.1016/j.jclinepi.2004.07.008.
Nisar T, Hanumanthu R, Khandelwal P. Symptomatic Intracerebral Hemorrhage after Intravenous Thrombolysis: Predictive Factors and Validation of Prediction Models. J Stroke Cerebrovasc Dis. 2019;28(11). https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104360.
Asuzu D, Nystrom K, Amin H, et al. Comparison of 8 Scores for predicting Symptomatic Intracerebral Hemorrhage after IV Thrombolysis. Neurocrit Care. 2015;22(2). https://doi.org/10.1007/s12028-014-0060-2.
Watson-Fargie T, Dai D, MacLeod MJ, Reid JM. Comparison of predictive scores of symptomatic intracerebral haemorrhage after stroke thrombolysis in a single centre. J Royal College Phys Edinburgh. 2015;45(2). https://doi.org/10.4997/JRCPE.2015.208.
Van Hooff RJ, Nieboer K, De Smedt A, et al. Validation assessment of risk tools to predict outcome after thrombolytic therapy for acute ischemic stroke. Clin Neurol Neurosurg. 2014;125. https://doi.org/10.1016/j.clineuro.2014.08.011.
Sung SF, Chen SCC, Lin HJ, Chen YW, Tseng MC, Chen CH. Comparison of risk-scoring systems in predicting symptomatic intracerebral hemorrhage after intravenous thrombolysis. Stroke. 2013;44(6). https://doi.org/10.1161/STROKEAHA.111.000651.
Sung SF, Chen CH, Chen YW, Tseng MC, Shen HC, Lin HJ. Predicting symptomatic intracerebral hemorrhage after intravenous thrombolysis: Stroke territory as a potential pitfall. J Neurol Sci. 2013;335(1–2). https://doi.org/10.1016/j.jns.2013.08.036.
Mazya M V, Bovi P, Castillo J, et al. External validation of the SEDAN score for prediction of intracerebral hemorrhage in stroke thrombolysis. Stroke. 2013;44(6). https://doi.org/10.1161/STROKEAHA.113.000794.
Strbian D, Michel P, Seiffge DJ, et al. Symptomatic intracranial hemorrhage after stroke thrombolysis: Comparison of prediction scores. Stroke. 2014;45(3). https://doi.org/10.1161/STROKEAHA.113.003806.
Li M, Wang-Qin RQ, Wang YL, et al. Symptomatic intracerebral hemorrhage after intravenous thrombolysis in chinese patients: Comparison of prediction models. Journal of Stroke and Cerebrovascular Diseases. 2015;24(6). https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.01.026.
Chang X, Zhang X, Zhang G. Different Scores Predict the Value of Hemorrhagic Transformation after Intravenous Thrombolysis in Patients with Acute Ischemic Stroke. Evidence-based Complement Altern Med. 2021;2021. https://doi.org/10.1155/2021/2468052.
Orbán-Kálmándi R, Szegedi I, Sarkady F, et al. A modified in vitro clot lysis assay predicts outcomes and safety in acute ischemic stroke patients undergoing intravenous thrombolysis. Sci Rep. 2021;11(1). https://doi.org/10.1038/s41598-021-92041-1.
Turcato G, Cappellari M, Follador L, et al. Red Blood Cell Distribution Width Is an Independent Predictor of Outcome in Patients Undergoing Thrombolysis for Ischemic Stroke. Semin Thromb Hemost. 2017;43(1). https://doi.org/10.1055/s-0036-1592165.
Steiner S. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. Zeitschrift fur Gefassmedizin. 2016;13(1). https://doi.org/10.1056/nejmoa1504720.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377(7). https://doi.org/10.1056/nejmoa1611925.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2019;380(4). https://doi.org/10.1056/nejmoa1812389.
He J, Baxter SL, Xu J, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25(1). https://doi.org/10.1038/s41591-018-0307-0.
Bivard A, Churilov L, Parsons M. Artificial intelligence for decision support in acute stroke — current roles and potential. Nat Rev Neurol. 2020;16(10). https://doi.org/10.1038/s41582-020-0390-y.
LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521(7553):436–44. https://doi.org/10.1038/nature14539.
Siontis KC, Noseworthy PA, Attia ZI, Friedman PA. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat Rev Cardiol. 2021;18(7):465–78. https://doi.org/10.1038/s41569-020-00503-2.
Hinton GE, Dayan P, Frey BJ, Neal RM. The “Wake-Sleep” Algorithm for Unsupervised Neural Networks. Science (1979). 1995;268(5214):1158–61. https://doi.org/10.1126/science.7761831.
Jang HJ, Cho KO. Applications of deep learning for the analysis of medical data. Arch Pharm Res. 2019;42(6):492–504. https://doi.org/10.1007/s12272-019-01162-9.
Obermeyer Z, Emanuel EJ. Predicting the Future — Big Data, Machine Learning, and Clinical Medicine. N Engl J Med. 2016;375(13). https://doi.org/10.1056/nejmp1606181.
Ambale-Venkatesh B, Yang X, Wu CO, et al. Cardiovascular Event Prediction by Machine Learning: The Multi-Ethnic Study of Atherosclerosis. Circ Res. 2017;121(9). https://doi.org/10.1161/CIRCRESAHA.117.311312.
Johnson KM, Johnson HE, Zhao Y, Dowe DA, Staib LH. Scoring of coronary artery disease characteristics on coronary CT angiograms by using machine learning. Radiology. 2019;292(2).https://doi.org/10.1148/radiol.2019182061.
Aziz F, Malek S, Ibrahim KS, et al. Short- And long-term mortality prediction after an acute ST-elevation myocardial infarction (STEMI) in Asians: A machine learning approach. PLoS One. 2021;16(8 August). https://doi.org/10.1371/journal.pone.0254894.
Xu Y, Li X, Wu D, Zhang Z, Jiang A. Machine Learning-Based Model for Prediction of Hemorrhage Transformation in Acute Ischemic Stroke After Alteplase. Front Neurol. 2022;13. https://doi.org/10.3389/fneur.2022.897903.
Meng Y, Wang H, Wu C, Liu X, Qu L, Shi Y. Prediction Model of Hemorrhage Transformation in Patient with Acute Ischemic Stroke Based on Multiparametric MRI Radiomics and Machine Learning. Brain Sci. 2022;12(7):858. https://doi.org/10.3390/brainsci12070858.
Weng ZA, Huang XX, Deng D, et al. A New Nomogram for Predicting the Risk of Intracranial Hemorrhage in Acute Ischemic Stroke Patients After Intravenous Thrombolysis. Front Neurol. 2022;13. https://doi.org/10.3389/fneur.2022.774654.
Zhang K, Luan J, Li C, Chen M. Nomogram to predict hemorrhagic transformation for acute ischemic stroke in Western China: a retrospective analysis. BMC Neurol. 2022;22(1):156. https://doi.org/10.1186/s12883-022-02678-2.
Zhang KJ, Jin H, Xu R, Zhang P, Guo ZN, Yang Y. N-Terminal Pro-brain Natriuretic Peptide Is Associated With Hemorrhagic Transformation and Poor Outcomes in Patients With Stroke Treated With Intravenous Thrombolysis. Front Mol Neurosci. 2021;14. https://doi.org/10.3389/fnmol.2021.758915.
Guo H, Xu W, Zhang X, et al. A nomogram to predict symptomatic intracranial hemorrhage after intravenous thrombolysis in chinese patients. Neuropsychiatr Dis Treat. 2021;17. https://doi.org/10.2147/NDT.S320574.
Soni M, Wijeratne T, Ackland DC. A risk score for prediction of symptomatic intracerebral haemorrhage following thrombolysis. Int J Med Inform. 2021;156. https://doi.org/10.1016/j.ijmedinf.2021.104586.
Liu J, Tao W, Wang Z, Chen X, Wu B, Liu M. Radiomics-based prediction of hemorrhage expansion among patients with thrombolysis/thrombectomy related-hemorrhagic transformation using machine learning. Ther Adv Neurol Disord. 2021;14. https://doi.org/10.1177/17562864211060029.
Chen Z, Li Q, Li R, et al. Ensemble learning accurately predicts the potential benefits of thrombolytic therapy in acute ischemic stroke. Quant Imaging Med Surg. 2021;11(9). https://doi.org/10.21037/qims-21-33.
Wang F, Huang Y, Xia Y, et al. Personalized risk prediction of symptomatic intracerebral hemorrhage after stroke thrombolysis using a machine-learning model. Ther Adv Neurol Disord. 2020;13. https://doi.org/10.1177/1756286420902358.
Bacchi S, Zerner T, Oakden-Rayner L, Kleinig T, Patel S, Jannes J. Deep Learning in the Prediction of Ischaemic Stroke Thrombolysis Functional Outcomes: A Pilot Study. Acad Radiol. 2020;27(2). https://doi.org/10.1016/j.acra.2019.03.015.
Chung CC, Hong CT, Huang YH, et al. Predicting major neurologic improvement and long-term outcome after thrombolysis using artificial neural networks. J Neurol Sci. 2020;410. https://doi.org/10.1016/j.jns.2020.116667.
Bentley P, Ganesalingam J, Carlton Jones AL, et al. Prediction of stroke thrombolysis outcome using CT brain machine learning. Neuroimage Clin. 2014;4. https://doi.org/10.1016/j.nicl.2014.02.003.
Funding
This work is supported by National Natural Science Foundation of China (Grant No. 82100531).
Author information
Authors and Affiliations
Contributions
Kexin Zhang and Yao Jiang searched the literature, analyzed data and drafted the manuscript. Dr. Zhu and Professor Zeng developed the idea and revised the manuscript. All authors agreed to submit the paper to the journal.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The Pathogenic Mechanism of Atherosclerosis.
Additional file 2.
Features of Different TAs.
Additional file 3.
Traditional Risk Scores for ACS and AIS.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, K., Jiang, Y., Zeng, H. et al. Application and risk prediction of thrombolytic therapy in cardio-cerebrovascular diseases: a review. Thrombosis J 21, 90 (2023). https://doi.org/10.1186/s12959-023-00532-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-023-00532-0