Abstract
Background
Hypocalcemia has been shown to be involved in the adverse outcomes of acute pulmonary embolism (APE). We aimed to determine the incremental value of adding hypocalcemia, defined as serum calcium level ≤ 2.12 mmol/L, on top of the European Society of Cardiology (ESC) prognostic algorithm, for the prediction of in-hospital mortality in APE patients, which in turn could lead to the optimization of APE management.
Methods
This study was conducted at West China Hospital of Sichuan University from January 2016 to December 2019. Patients with APE were retrospectively analyzed and divided into 2 groups based on serum calcium levels. Associations between hypocalcemia and adverse outcomes were assessed by Cox analysis. The accuracy of risk stratification for in-hospital mortality was assessed with the addition of serum calcium to the current ESC prognostic algorithm.
Results
Among 803 patients diagnosed with APE, 338 (42.1%) patients had serum calcium levels ≤ 2.12 mmol/L. Hypocalcemia was significantly associated with higher in-hospital and 2-year all-cause mortality compared to the control group. The addition of serum calcium to ESC risk stratification enhanced net reclassification improvement. Low-risk group with serum calcium level > 2.12 mmol/L had a 0% mortality rate, improving the negative predictive value up to 100%, while high-risk group with serum calcium level ≤ 2.12 mmol/L indicated a higher mortality of 25%.
Conclusion
Our study identified serum calcium as a novel predictor of mortality in patients with APE. In the future, serum calcium may be added to the commonly used ESC prognostic algorithm for better risk stratification of patients suffering from APE.
Similar content being viewed by others
Introduction
Acute pulmonary embolism (APE) is a common cause of hospital and mortality, which results in a heavy disease burden on both families and countries [1]. The clinical severity of APE is variable and ranges from minor symptoms to right ventricular dysfunction and cardiogenic shock [2, 3]. The early detection of high-risk patients represents an important step in prudent therapeutic decision making and reducing the risk of mortality. The European Society of Cardiology (ESC) prognostic algorithm is currently used in the risk assessment in patients with APE [4,5,6]. Patients were classified into low, intermediate-low, intermediate-high and high mortality risk groups based on the assessment of hemodynamic instability, clinical status, and laboratory indicators of APE severity, mostly related to the presence of right ventricular (RV) dysfunction [6, 7]. Low-and intermediate–low-risk APE patients can be candidates for home anticoagulant treatment or short hospital stays, intermediate–high-risk APE patients need additional close monitoring, and high-risk PE patients require urgent systemic thrombolysis or surgical embolectomy therapy to improve RV function [8].
Calcium is an important coagulation factor that participates in different cellular processes [9]. Hypocalcemia is a common biochemical abnormality and has been recognized as a prognostic marker of coronary heart disease, chronic kidney disease, acute myocardial infarction and gastrointestinal bleeding [10,11,12,13]. Furthermore, evidence is mounting that hypocalcemia is associated with short-term mortality after APE [14, 15]. A study of 4196 consecutive subjects revealed that serum calcium improved the simplified Pulmonary Embolism Severity Index (sPESI) score for risk stratification in patients with APE [16]. However, whether the assessment of serum calcium adds to the ESC risk stratification to produce greater power for predicting in-hospital and long-term mortality is unclear.
The aim of this study was to investigate the incremental value of adding serum calcium on top of the ESC-defined prognostic algorithm for the prediction of in-hospital and long-term mortality in patients with APE. We particularly sought to determine whether it permits the identification of high-risk patients with an even higher degree of safety.
Methods
Study design
This study was retrospectively conducted at West China Hospital of Sichuan University, China. The study enrolled consecutive adult inpatients diagnosed with APE from January 2016 to December 2019. The diagnosis of APE was based on the following criteria: (1) CTPA showing a segmental or proximal filling defect; or (2) the V/Q scan yielding high probability.
for pulmonary embolism. We excluded patients with incomplete initial clinical data. Patients with a diagnosis of hyperparathyroidism were also excluded for the impact on serum calcium. This study was approved by the Institutional Review Board of West China Hospital of Sichuan University, which waived the requirement for written informed consent because of the retrospective study design.
Data collection
Data were obtained from the hospital’s computerized medical records, including demographic data, symptoms, vital signs, comorbidities and laboratory and radiographic findings. The presence of comorbidities was defined according to clinical diagnosis. Laboratory and radiographic data, including N-terminal-pro-B-type natriuretic peptide (NT-proBNP), troponin T, RV dilation (defined as the diameter ratio of right ventricle and left ventricle qualed or exceeded 1 by computed tomography (CT) or ultrasound), and pleural effusion were reviewed. The use of anticoagulant agents (low-molecular weight heparin (LMWH), fondaparinux, unfractionated heparin, vitamin K antagonists, or nonvitamin K antagonist oral anticoagulants), thrombolytic, interventional or surgical treatment was directed by the attending physician in accordance with clinical protocols based on ESC guidelines [6].
Laboratory assessment of serum calcium
The assessment of serum calcium was routinely conducted for all of the enrolled patients within 24 h after admission. Levels of serum calcium were measured by Arsenazo III colorimetry (Beckman Coulter, Brea, America) using fresh samples, which had a functional sensitivity of 0.01 mmol/L. It was unadjusted for serum albumin and the reference interval of serum calcium for our laboratory ranged from 2.11 to 2.52 mmol/L. Hypocalcemia was defined as a serum calcium level ≤ 2.12 mmol/L [17].
ESC risk stratification
The ESC prognostic algorithm for patients with APE was calculated using the following criteria: (i) signs of hemodynamic instability, RV overload and plasma troponin concentrations; and (ii) presence of comorbidity and any other clinical symptoms [6]. Patients were divided into three groups based on the ESC guidelines: low risk, intermediate risk (intermediate–low and intermediate–high risk), and high risk.
Follow-up and outcomes
Each patient was followed up with a telephone conversation after admission until 2 years. The primary outcomes of the study was in-hospital and 2-year all-cause mortality, while the secondary outcomes were in-hospital APE-related mortality, intensive care unit (ICU) admission, respiratory failure, mechanical ventilation and length of stay.
Statistical analysis
Continuous variables are reported as the means with standard deviations or medians with interquartile ranges and were compared using Student’s t test or the Mann–Whitney U test, while categorical variables are presented as percentages and were compared using the chi-square test. All parameters were compared between the hypocalcemia group and the control group. Univariable and multivariable Cox regression analyses were conducted to confirm the risk factors for mortality, which are presented as hazard ratios (HRs) with 95% confidence intervals (CIs). For survival analysis, Kaplan–Meier analysis and log-rank test were used to describe and compare mortality between the patients with serum calcium level ≤ 2.12 mmol/L and serum calcium level > 2.12 mmol/L in the population with APE. The changes in predicted risk reclassification were calculated for the evaluation of the improvement in prediction performance gained by adding the serum calcium to the ESC prognostic algorithm. A P value of less than 0.05 was considered to be statistically significant, and analyses were performed with SPSS software (IBM Corporation, Armonk, New York, United States).
Results
Baseline information
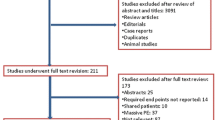
During the study period, a total of 813 patients were identified as having APE. Patients were excluded from the analyses: 7 patients did not have serum calcium measurements, and 3 patients had hyperparathyroidism. The final analysis included 803 patients, of whom 61 died and 742 survived (Fig. 1).
Clinical characteristics of patients with APE and hypocalcemia
There were 338 patients with serum calcium levels ≤ 2.12 mmol/L (hypocalcemia group) and 465 with serum calcium levels > 2.12 mmol/L (control group). The demographic and clinical characteristics of patients with and without hypocalcemia are presented in Table 1. Compared with the control group, the hypocalcemia group showed a significantly higher percentage of males (222[65.7%] vs. 255[54.8%], P = 0.002) and smokers (110[32.5%] vs. 121[26.0%], P = 0.044). Additionally, dyspnea, hemoptysis, and leg pain or swelling were more frequently observed in the hypocalcemia group than in the control group, but the difference was not statistically significant. Patients admitted with hypocalcemia had lower systolic blood pressure, higher body temperature, and faster pulse rate and respiratory rate (both P < 0.05). According to the PESI and sPESI, high-risk patients comprised a significantly greater percentage of the hypocalcemia group than of the control group (P < 0.001 and P = 0.017). Except for active cancer and coronary heart disease, the data of comorbid conditions did not significantly differ between the 2 groups.
Laboratory and computed tomography findings in patients with APE and hypocalcemia
Patients with hypocalcemia had higher levels of NT-proBNP (P = 0.006), and there were no significant differences between groups in terms of troponin T. RV dilation was significantly more common (110 [48.5%] vs. 132 [38.8%], P = 0.023), and pleural effusion tended to be more common (244 [72.6%] vs. 257 [55.4%], P < 0.001) in the hypocalcemia group than in the control group.
Hypocalcemia and clinical outcome
A total of 61 (7.6%) patients died during hospitalization, and 25 (3.1%) deaths were adjudicated as APE-related. The in-hospital and 2-year all-cause mortality was significantly higher in the hypocalcemia group than in the control group (both P < 0.05) (Table 1). The presence of hypocalcemia was associated with a higher rate of respiratory failure (25.1% vs. 15.1%, P < 0.001) and mechanical ventilation (7.1% vs. 3.9%, P = 0.042). However, there were no significant differences between groups in terms of APE-related mortality, ICU admission, systemic thrombolysis, or length of hospital stay (all P > 0.05).
Predictors of mortality and survival analysis
All patients included in the study were divided into a death group (n = 61) and a survival group (n = 742). The results of univariable hazard risk analysis for the prediction of in-hospital all-cause mortality are presented in Table 2. The multivariable hazard risk analysis showed that independent predictors of fatal outcome were age, male sex, systolic blood pressure < 100 mmHg, pulse rate ≥ 110 beats/min, active cancer, chronic renal insufficiency, and serum calcium level ≤ 2.12 mmol/L(Table 3).
The log-rank test was used to compare the difference in survival between the hypocalcemia and control groups, while the Kaplan–Meier method was used to draw a survival curve. The results revealed a significant difference in 2-year all-cause mortality between the two groups (P = 0.005) (Fig. 2).
Combining ESC Risk Stratification and Serum Calcium for Prognostic Assessment
Forty-six (5.7%) patients presented with hemodynamic instability and formed a high-risk group, whereas the remaining 757 patients were normotensive on admission. Eleven deaths occurred in the high-risk APE group (mortality 23.9%), and a serum calcium level ≤ 2.12 mmol/L on admission indicated 28 patients with 25.0% mortality, while a serum calcium level > 2.12 mmol/L indicated 22.2% mortality. In the intermediate-risk group, the in-hospital mortality was 7.8%. Patients with hypocalcemia had a higher observed mortality rate than patients with normal serum calcium (10.4% vs. 5.8%). One (0.8) death was reported in the low-risk group, and a serum calcium level > 2.12 mmol/L on admission was present in a group of 126 APE patients with a mortality rate of 0% (Fig. 3).
Discussion
This study investigated the prognostic significance of hypocalcemia, defined as a serum calcium level ≤ 2.12 mmol/L, for APE. Our results showed that lower serum calcium was associated with worse in-hospital and long-term mortality. Importantly, the present study might be the first to reveal that the combined use of serum calcium and the ESC prognostic algorithm was better able to predict in-hospital death compared with ESC risk stratification alone. Furthermore, early assessment of serum calcium might accurately identify high-risk patients with APE.
The ESC prognostic algorithm was developed for the early risk assessment of patients with APE, which represented an important step in therapeutic decision making [8]. Moor et al. reported that the area under the receiver operating characteristic curve (AUC) predictive value of the 2019 ESC algorithm for 30-day mortality was 0.636 [18]. In a prospective cohort study, the risk of death in patients at “intermediate-high” and “intermediate-low” risk according to the ESC model was similar, and risk stratification in patients at intermediate risk requires further improvement [19]. Therefore, the categorization of patients with APE based on RV dysfunction, elevated troponins and sPESI seems not sufficiently efficient.
Hypocalcemia is one of the most common electrolyte disturbances and may potentially impact virtually any organ and system [17]. There is evidence that serum calcium independently predicts mortality in acute PE. In a study including 2017 nationwide inpatients with APE, Murthi et al. found that patients with hypocalcemia had higher in‑hospital mortality and complications than those without hypocalcemia, along with a longer length of stay [15]. Wang et al. reported that hypocalcemia was an independent predictor of 30-day mortality following APE [14]. In the present study, the existence of hypocalcemia was an independent predictor of all-cause in-hospital and long-term mortality of APE, which reported that hypocalcemia showed better prognostic predictive performance and could be a novel marker for predicting poor prognosis of APE. These studies encouraged us to add serum calcium to the ESC prognostic algorithm, with the aim of improving its prognostic value.
This study showed that serum calcium assessment improved the accuracy of the current ESC risk stratification strategy in identifying patients with APE at increased risk of death. Our results strengthen those described by Yang et al., who proposed a new prognostic assessment model combining the sPESI risk score with serum calcium, which had higher performance than the PESI and sPESI [16]. In this study, a serum calcium level ≤ 2.12 mmol/L in patients with low risk identified a group with a mortality of 2.5%, improving the negative predictive value up to 100%, while in high-risk patients, it indicated a high early mortality of 25%. Some ESC-defined intermediate-risk APE patients were accurately stratified as high and low risk after adding serum calcium to the model. Compared with the ESC prognostic algorithm alone, serum calcium assessment significantly improved the current risk stratification according to the ESC guidelines.
Our study clarified that hypocalcemia was significantly associated with a higher PESI and sPESI score, higher blood levels of NT-proBNP, and higher rates of RV dilation and pleural effusion compared to those without hypocalcemia. All of these clinical prediction rules are known strong predictors of short-term and long-term prognosis after APE [20,21,22,23,24]. Based on these findings, we assumed that hypocalcemia influences the short-term and long-term prognosis of APE. Mechanisms by which hypocalcemia has been hypothesized to be associated with mortality include APE with a high risk of causing proinflammatory cytokine release, inhibiting parathyroid hormone release, causing cellular redistribution of calcium, and consequently precipitating hypocalcemia [15]; hypocalcemia is associated with cardiac dysfunction and hypotension [25]; and vitamin D deficiency is considered to be one of the most common causes of hypocalcemia and contributes to poor prognosis in patients with cardiopulmonary disease [26, 27].
Based on the findings of this study, some suggestions for management and treatment were given about APE. The presence of hypocalcemia has an important prognostic impact for APE and might help predict short-term and long-term mortality, which should be closely monitored for the benefits of patients with APE in the hospital and after discharge. On the other hand, serum calcium assessment may be added to the ESC prognostic algorithm to acquire higher predictive power for in-hospital mortality.
Several limitations of the present study require consideration. Firstly, these findings come from a single-center, retrospective study and cannot be extrapolated to other APE patients. Validation with a prospective population in a well-designed multicenter study is needed. Secondly, we also did not collect data on the use of blood products, which may affect serum calcium levels. Therefore, we could not determine the correlation between these factors and mortality. Thirdly, it is unclear if hypocalcemia in itself affects the prognosis, or if it is a surrogate marker for another factor (e.g. vitamin D deficiency). Fourthly, the prevalence of hypocalcemia in our study was much higher than that reported in previous studies, in which it reported prevalence rates of 0.8% [15]. However, this was in accordance with the findings by PUMCH cohort study conducted in China recently, which reported that the prevalence of hypocalcemia was 49.48% in acute pulmonary embolism [14]. In addition to the possible effect of the different patient populations investigated, we believed that this large difference in the cutoff value of serum calcium levels among the studies can mainly be attributed to differences in the prevalence of hypocalcemia in patients with APE. Fifthly, we only explored the relationship between serum calcium levels on admission and mortality in patients with APE. Serum calcium levels change as the disease progresses, and we did not report the relationship between dynamic changes in serum calcium levels and prognosis in patients with APE.
Conclusion
Hypocalcemia present on admission in 42.1% of patients with acute PE indicated worse prognosis. Serum calcium ≤ 2.12 mmol/L not only independently predicted higher in-hospital and long-term all-cause mortality but also, when added to the current ESC risk stratification algorithm, improved the identification of both low- and high-risk patients. Therefore, serum calcium assessment may be implemented in the risk assessment of APE.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- APE:
-
Acute pulmonary embolism
- ESC:
-
European society of cardiology
- RV:
-
Right ventricular
- PESI:
-
Pulmonary embolism severity index
- sPESI:
-
Simplified pulmonary embolism severity index
- NT-pro BNP:
-
N-terminal pro-B–type natriuretic peptide
- CT:
-
Computed tomography
- LMWH:
-
Low-molecular weight heparin
- ICU:
-
Intensive care unit
- HR:
-
Hazard ratios
- CI:
-
Confidence interval
- AUC:
-
Area under the receiver operating characteristic curve
References
Konstantinides SV, Barco S, Lankeit M, Meyer G. Management of Pulmonary Embolism: An Update. J Am Coll Cardiol. 2016;67:976–90.
Meyer G, Planquette B, Sanchez O. Pulmonary embolism: whom to discharge and whom to thrombolyze? J Thromb Haemost. 2015;13(Suppl 1):S252-258.
Huisman MV, Barco S, Cannegieter SC, Le Gal G, Konstantinides SV, Reitsma PH, Rodger M, Vonk Noordegraaf A, Klok FA. Pulmonary embolism Nat Rev Dis Primers. 2018;4:18028.
Vanni S, Nazerian P, Pepe G, Baioni M, Risso M, Grifoni G, Viviani G, Grifoni S. Comparison of two prognostic models for acute pulmonary embolism: clinical vs. right ventricular dysfunction-guided approach. J Thromb Haemost. 2011;9:1916–23.
Jimenez D, Lobo JL, Fernandez-Golfin C, Portillo AK, Nieto R, Lankeit M, Konstantinides S, Prandoni P, Muriel A, Yusen RD. Effectiveness of prognosticating pulmonary embolism using the ESC algorithm and the Bova score. Thromb Haemost. 2016;115:827–34.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings CS, Jiménez D, et al. ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J. 2019;2019:54.
Kostrubiec M, Pływaczewska M, Jiménez D, Lankeit M, Ciurzynski M, Konstantinides S, Pruszczyk P. The Prognostic Value of Renal Function in Acute Pulmonary Embolism-A Multi-Centre Cohort Study. Thromb Haemost. 2019;119:140–8.
Chopard R, Jimenez D, Serzian G, Ecarnot F, Falvo N, Kalbacher E, Bonnet B, Capellier G, Schiele F, Bertoletti L, et al. Renal dysfunction improves risk stratification and may call for a change in the management of intermediate- and high-risk acute pulmonary embolism: results from a multicenter cohort study with external validation. Crit Care. 2021;25:57.
Torres B, Alcubilla P, González-Cordón A, Inciarte A, Chumbita M, Cardozo C, Meira F, Giménez M, de Hollanda A, Soriano A. Impact of low serum calcium at hospital admission on SARS-CoV-2 infection outcome. Int J Infect Dis. 2021;104:164–8.
Chen Q, Zhang Y, Ding D, Li D, Yang Y, Li Q, Chen X, Hu G, Ling W. Associations between serum calcium, phosphorus and mortality among patients with coronary heart disease. Eur J Nutr. 2018;57:2457–67.
Lim LM, Kuo HT, Kuo MC, Chiu YW, Lee JJ, Hwang SJ, Tsai JC, Hung CC, Chen HC. Low serum calcium is associated with poor renal outcomes in chronic kidney disease stages 3–4 patients. BMC Nephrol. 2014;15:183.
Shiyovich A, Plakht Y, Gilutz H. Serum calcium levels independently predict in-hospital mortality in patients with acute myocardial infarction. Nutr Metab Cardiovasc Dis. 2018;28:510–6.
Korytny A, Klein A, Marcusohn E, Freund Y, Neuberger A, Raz A, Miller A, Epstein D. Hypocalcemia is associated with adverse clinical course in patients with upper gastrointestinal bleeding. Intern Emerg Med. 2021;16:1813–22.
Wang X, Xiang Y, Zhang T, Yang Y, Sun X, Shi J. Association between serum calcium and prognosis in patients with acute pulmonary embolism and the optimization of pulmonary embolism severity index. Respir Res. 2020;21:298.
Murthi M, Shaka H, El-Amir Z, Velagapudi S, Jamil A, Wani F, Atluri R, Kumar A, Kichloo A. Association of hypocalcemia with in-hospital mortality and complications in patients with acute pulmonary embolism: results from the 2017 Nationwide Inpatient Sample. BMC Pulm Med. 2021;21:410.
Yang YQ, Wang X, Zhang YJ, Chen YF, Wang L, Hu XW, Niu L, Pu HM, Zhang X, Zhang Z, et al. Prognosis assessment model based on low serum calcium in patients with acute pulmonary thromboembolism. Respirology. 2022;27:645–52.
Pepe J, Colangelo L, Biamonte F, Sonato C, Danese VC, Cecchetti V, Occhiuto M, Piazzolla V, De Martino V, Ferrone F, et al. Diagnosis and management of hypocalcemia. Endocrine. 2020;69:485–95.
Moor J, Baumgartner C, Méan M, Stalder O, Limacher A, Rodondi N, Aujesky D. Validation of the 2019 European Society of Cardiology Risk Stratification Algorithm for Pulmonary Embolism in Normotensive Elderly Patients. Thromb Haemost. 2021;121:1660–7.
Becattini C, Agnelli G, Lankeit M, Masotti L, Pruszczyk P, Casazza F, Vanni S, Nitti C, Kamphuisen P, Vedovati MC, et al. Acute pulmonary embolism: mortality prediction by the 2014 European Society of Cardiology risk stratification model. Eur Respir J. 2016;48:780–6.
Moores L, Zamarro C, Gómez V, Aujesky D, García L, Nieto R, Yusen R, Jiménez D. Changes in PESI scores predict mortality in intermediate-risk patients with acute pulmonary embolism. Eur Respir J. 2013;41:354–9.
Mizuno A, Yamamoto T, Tanabe Y, Obayashi T, Takayama M, Nagao K. Pulmonary embolism severity index and simplified pulmonary embolism severity index risk scores are useful to predict mortality in Japanese patients with pulmonary embolism. Circ J. 2015;79:889–91.
Vuilleumier N, Le Gal G, Verschuren F, Perrier A, Bounameaux H, Turck N, Sanchez JC, Mensi N, Perneger T, Hochstrasser D, Righini M. Cardiac biomarkers for risk stratification in non-massive pulmonary embolism: a multicenter prospective study. J Thromb Haemost. 2009;7:391–8.
Barco S, Mahmoudpour SH, Planquette B, Sanchez O, Konstantinides SV, Meyer G. Prognostic value of right ventricular dysfunction or elevated cardiac biomarkers in patients with low-risk pulmonary embolism: a systematic review and meta-analysis. Eur Heart J. 2019;40:902–10.
Choi KJ, Cha SI, Shin KM, Lim J, Yoo SS, Lee J, Lee SY, Kim CH, Park JY, Lee WK. Prognostic implications of computed tomographic right ventricular dilation in patients with acute pulmonary embolism. Thromb Res. 2014;133:182–6.
Kelly A, Levine MA. Hypocalcemia in the critically ill patient. J Intensive Care Med. 2013;28:166–77.
Akbar MR, Wibowo A, Pranata R, Setiabudiawan B. Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated With Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis. Front Nutr. 2021;8: 660420.
Kusunose K, Okushi Y, Okayama Y, Zheng R, Abe M, Nakai M, Sumita Y, Ise T, Tobiume T, Yamaguchi K, et al. Association between Vitamin D and Heart Failure Mortality in 10,974 Hospitalized Individuals. Nutrients. 2021;13(2):335.
Acknowledgements
The authors would like to give great thanks to Xiaoqian Li and Yuehong Hu for helping to search the patients in the database. This study was supported by the National Natural Science Foundation of China (82170013), the Sichuan Science and Technology Program (2022YFS0262) and the National Key Research Program of China (2016YFC1304202).
Author information
Authors and Affiliations
Contributions
JZ contributed to the analysis and interpretation of the data and drafted the manuscript. QY and HZ contributed to the design of the study and final approval of the version to be published. All other authors contributed to the acquisition and interpretation of the data and reviewed the manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of West China Hospital of Sichuan University, which waived the requirement for written informed consent because of the retrospective study design.
Consent for publication
The participant has consented to the submission of this article to the journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, J., Ali, A., Liu, Y. et al. Additive prognostic value of serum calcium to the ESC risk stratification in patients with acute pulmonary embolism. Thrombosis J 21, 20 (2023). https://doi.org/10.1186/s12959-023-00461-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-023-00461-y