Abstract
Background
Thromboembolism was a chief cause of mortality in 70% of patients with COVID-19. Our objective was to see if serum interleukins 1 beta (IL-1β) and soluble platelets selectin (sP-selectin) could serve as novel markers of thromboembolism in COVID-19 patients.
Methods
This cross sectional study involved 89 COVID-19 patients who were recruited from 1st of February to 1st of May 2021. Clinical and laboratory data were collected, and chest imaging was performed. The levels of IL-1β and sP-selectin were assessed in all cases through ELISA kits. Comparisons between groups were done using an unpaired t-test in normally distributed quantitative variables. In contrast, a non-parametric Mann-Whitney test was used for non-normally distributed quantitative variables.
Results
Severe COVID-19 infection was associated with higher serum levels of CRP, Ferritin, LDH, D dimer, IL-1β and sP-selectin (P < 0.001) with significant correlation between levels of IL-1β and sP-selectin (r 0.37, P < 0.001), D-dimer (r 0.29, P 0.006) and Ferritin (r 0.5, p < 0.001).
Likewise, a positive correlation was also found between levels of sP-selectin, D-dimer and Ferritin (r 0.52, P < 0.001) (r 0.59, P < 0.001). Imaging studies revealed that 9 (10.1%) patients developed venous and 14 (15.7%) developed arterial thrombosis despite receiving anticoagulant therapy. Patients with thrombotic events had significantly higher levels of IL-1β, sP-selectin and LDH serum levels. Meanwhile, there was no statistical significance between CRP, D-dimer or Ferritin levels and the development of thrombotic events.
Conclusion
IL-1β and sP-selectin levels can be promising predictors for severe COVID-19 infection and predictable thrombosis.
Similar content being viewed by others
Background
In 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a member of Coronaviridae family, resulted in a distinctive infection characterized by acute severe respiratory syndrome (ARDS) which was declared as coronavirus disease of 2019 (COVID-19) pandemic [1].
SARS-CoV-2 infection is frequently linked to coagulopathy and venous thromboembolism (VTE) which promotes tissue injury and multiorgan dysfunction. Venous thrombosis followed by pulmonary embolism (PE) is commonly seen in severe COVID-19 and is found to be associated with increased severity and mortality rate [2].
Although mild flu-like symptoms were reported in most infected cases, viral replication resulted in a severe disease course in 20% of individuals. The reported mortality rate in hospitalized patients with COVID-19 ranges from 4.3 to 15% [3]. Thromboembolism was addressed as a chief cause of mortality in 70% of affected patients [4].
Pathogenesis of COVID-19 infection involves a complex interplay between coagulopathy and endotheliopathy due to viral infection and replication in the target cells with consequent immune and coagulation systems dysregulation [5], leading to uncontrolled inflammatory responses and eventually resulting in the cytokine storm [6]. The fibrinogen level in COVID-19 patients increases by 2–3 folds due to cytokine storm, causing thrombus formation, particularly in severe cases [7]. Moreover, the cytokine storm can damage both epithelial cells and endothelial cells, vascular leakage and finally result in ARDS and death [8].
Many cytokines have been implicated as possible players in a subset of severe patients, such as interlukin-1beta (IL-1β), IL-6, IL-18 and interferon [9]. In response to IL-6 and IL-1ß, the tissue factor is expressed by monocytes, activating the extrinsic pathway of coagulation cascade and suppressing fibrinolysis through the increased release of plasminogen activator inhibitor-1 and decreased activity of urokinase plasminogen activator [10].
In severe COVID-19 infection, pro-coagulant status is mediated through platelet activation and aggregation [11, 12]. Platelets are activated directly by the SARS-CoV-2 spike protein and indirectly through mediators released secondary to endothelial damage [13].
Soluble platelet selectin (sP-selectin) is stored in platelets’ α-granules and in endothelial cells. It acts as an adhesion receptor that initiates the recruitment of leukocytes to the sites of inflammation, tissue injury and immune control [14]. When the extracellular domain is spliced, it is released into circulation and referred to as soluble P-selectin,which mediates the interaction of stimulated endothelial cells or platelets with the white blood cells on the vascular surface [15]. When combined with its ligand P-selectin glycoprotein ligand-1 (PSGL-1), it triggers platelet release and aggregation and mediates the adhesion of platelets to vascular endothelial cells [16].
In the current work, we aim to correlate abnormalities in inflammatory and coagulation pathways which offers opportunities for identifying biomarkers for severe disease and the occurrence of thromboebolism. Combined with clinical risk factors, this will help promptly identify patients at risk of the severe disease requiring early and targeted intervention.
Methods
Study design
This prospective cross-sectional study was carried out on 89 COVID-19 infected patients between the 1st and 30th of April, 2021. They were admitted to two government-authorized hospitals to treat COVID-19 patients (Insurance hospital and Beni-Suef University hospital).
Inclusion criteria
Adult Egyptian patients > 18 years who tested positive by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of the nasopharyngeal sample were enrolled.
Both sexes are included for the mild, moderate and severe cases
Exclusion criteria included patients whose age was < 18 years, COVID 19 Patients with negative real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasopharyngeal sample.
According to the interim guidelines of the World Health Organization (WHO) classification [17], COVID-19 infection was categorized into a mild, moderate or severe infection. Typical symptoms without pneumonia or hypoxia were defined as a mild cases, while moderate or severe cases were diagnosed if there were clinical and radiological signs of pneumonia. In moderate infection, patients had to have a saturation of peripheral oxygen (SpO2) ≥ 90% on room air, while one of the following was required to define the severe cases: respiratory rate > 30 breaths/min; severe respiratory distress; or SpO2 < 90% on room air. The treatment protocol followed by the two centers was according to the report of the national institute of health treatment guidelines [18].
Data collection
Clinical data were obtained, including patient demographics (age, gender, body mass index (BMI)), comorbid conditions (diabetes mellitus, hypertension, chronic pulmonary disease, chronic kidney disease, chronic liver disease, cardiovascular disease) and entire drug history especially anticoagulation and antiplatelets.
Clinical symptoms were reported by asking patients about the presence of constitutional symptoms (fever, bony aches and fatigue), respiratory symptoms (chest pain, cough and dyspnea), gastrointestinal symptoms (diarrhea and abdominal pain) and neurological symptoms (headache and anosmia). The severity of COVID-19 infection was determined based on initial computed tomography of the chest (CT-chest) results and clinical symptoms.
Laboratory assessment included complete blood picture, liver transaminases, serum urea, creatinine, C-reactive protein (CRP), D-dimer, and ferritin were collected within 24 hours of symptoms onset then on deterioration if occurred with documenting a day of deterioration. IL-1β and sP-selectin were assessed in all cases and were sampled at day of diagnosis before initiation of treatment.
Five ml of blood was withdrawn from patients and control groups under complete aseptic condition and added to ethylenediaminetetraacetic acid (EDTA) tubes. Plasma was separated within 30 minutes of collection by centrifugation at 3000 хg. Samples were stored at − 80 °C until assayed for IL-1β and sP-selectin.
Measurement of plasma IL-1β and plasma sP-selectin
This was done using human IL-1β enzyme-linked immunosorbent assay (ELISA) Kit for quantitatively detecting human IL-1β, catalog numbers BMS224–2 Pub. No. MAN0016591. Rev. C.0, 32 and human sP-selectin Kit for quantitative detection of human sP-selectin, catalog Numbers BMS219–4. This sandwich kit is for the accurate in vitro quantitative detection of human IL-1β and plasma sP-selectin [19].
Ethical consideration
Ethical approval was obtained from the ethical committee, Faculty of Medicine, Beni-Suef University. Approval NO. FMBSUREC/07032021. Written informed consents were taken from the participants. The study was performed in accordance with the principles of the Declaration of Helsinki.
Statistical analysis
Data were coded using the statistical package for the Social Sciences (SPSS) version 26 (IBM Corp., Armonk, NY, USA). Data were summarized using mean, standard deviation, median, minimum and maximum for quantitative variables and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between groups were made using an unpaired t-test in normally distributed quantitative variables, while a non-parametric Mann-Whitney test was u sed for non-normally distributed quantitative variables [20]. The Chi-square (χ2) test was performed to compare categorical data. The exact test was used when the expected frequency was less than 5 [21]. The Spearman correlation coefficient [22] revealed correlation between quantitative variables. P-values less than 0.05 were considered statistically significant.
Results
Demographics and clinical characteristics of the study population
The study population included 89 patients who had non-severe and severe COVID-19 infection. They were 44(49.4%) non-severe and 45(50.6%) severe according to WHO classification. 41.6% were males, and 52% were females, with a mean age of 61 ± 10 years. 55 (61.8%) patients received anticoagulation, according to the report of the national institute of health treatment guidelines. However, 23(41.8%) patients had thrombotic events despite anticoagulation, whereas 9 (10.1%) patients developed venous thrombosis (DVT), and 14 (15.7%) patients developed arterial thrombosis (pulmonary embolism) as documented by bilateral lower limb duplex or CTPA (CT pulmonary angiography). Other clinical characteristics of the study population were summarized in (Table 1).
Clinical characteristics of patients with non-severe versus severe COVID-19 infection
The mean age of patients with non-severe COVID-19 infection was 54.7 ± 8.3 years, while in severe was 68 ± 6.5, with statistical significance between the two groups (P = < 0.001).
28(63.6%) patients with diabetes and 32(72.7%) patients with hypertension experienced severe COVID-19 infection (P < 0.001). In contrast, no significant association was found with other comorbidities such as chronic pulmonary disease, chronic liver and kidney disease, ischemic heart disease, thyroid disease and cancer (Table 1).
Characteristics of patients with severe COVID-19 infection in relation to laboratory data
Patients with severe COVID-19 infection had significantly lower levels of total leucocyte count, lymphocyte %, neutrophil % and higher levels of CRP, ferritin, D-dimer, LDH, IL-1β and sP-selectin as demonstrated in (Table 1).
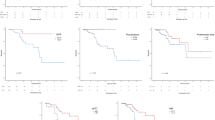
There was a statistically significant positive correlation between CRP, D-dimer, ferritin, LDH, IL-1β, and sP-selectin serum levels and the severity of COVID-19 infection (Table 2) (Fig. 1).
Clinical characteristics of patients without versus with thrombotic events
The mean age of patients without thrombotic events was 64 ± 10, while in patients with thrombotic events was 67 ± 7 years, with no statistically significant difference between the two groups (P = 0.18). Also, there was no statistically significant difference between the two groups in terms of gender or preexisting medical comorbidities, as demonstrated in (Table 3).
Characteristics of patients with thrombotic events concerning the severity of COVID-19 infection
There was no statistical significance in COVID-19 infection severity and the development of thrombotic events (P = 0.09) (Table 3).
Characteristics of patients with thrombotic events in relation to laboratory data
Patients with thrombotic events had significantly higher levels of IL-1β, sP-selectin, and LDH serum levels. Meanwhile, there was no statistical significance between serum levels of CRP, D-dimer or ferritin and the development of thrombotic events (Table 3) (Fig. 2).
Discussion
This study aims to assess the levels of IL-1β as an inflammatory cytokine and sP-selectin as a novel plasma marker for thromboembolism in COVID-19 patients and correlate abnormalities in inflammatory and coagulation pathways (IL-1β and sP-selectin) to the severity of the disease and the occurrence of venous thromboembolism (VTE) even on anticoagulation therapy. This, combined with clinical risk factors, will help promptly identify patients at risk of the severe disease who require early and targeted intervention.
SARS-CoV-2-Induced endothelial damage releases a variety of soluble markers of endothelial dysfunction, including von Willebrand factor (VWF), soluble E-selectin, P-selectin and thrombomodulin. Such biologically active molecules ultimatepromote platelet activation, which eventually contributes to inflammatory response and thrombotic complications, increasing the severity of COVID-19 [23].
On the assessment of IL-1β and sP-selectin levels and their relation to disease severity, we found a statistically significant increase in their level in the severe group compared to the non-severe group. Also, there is a statistically significant difference in D-dimer, CRP, Ferritin and LDH serum levels between non-severe and severe COVID-19 patients. Huang et al., studied Prothrombin time and D-dimer levels on admission which were higher in ICU patients (median prothrombin time 12·2 s [IQR 11·2–13·4]; median D-dimer level 2·4 mg/L [0·6–14·4]) than non-ICU patients (median prothrombin time 10·7 s [9·8–12·1], p = 0·012; median D-dimer level 0·5 mg/L [0·3–0·8], p = 0·0042) [24].
Tang et al. did not report on VTE incidence but noted derangement in coagulation and clotting markers PT, aPTT, D-dimer, fibrin degradation products which were higher in non-survivors [25].
Chiara Agrati et al. investigated sP-selectin plasma concentration as a biomarker of endothelial dysfunction and platelet activation in 46 severe COVID-19 hospitalized patients and found a higher sP-selectin plasma concentration in patients with Covid-19, regardless of intensive care unit (ICU) admission compared to the typical reference values and compared to ten contextually sampled healthy donors [26].
Emre Karsli et al. assessed the relationship between sP-selectin level and the clinical severity of COVID-19 infections in 80 patients, and similar to our study, they divided them into two groups, mild to the moderate group containing 50 patients and the severe group 30 patients, they compared results to 60 non-symptomatic healthy volunteers.
They found that serum sP-Selectin levels in both mild-to-moderate pneumonia and severe pneumonia groups were higher than in the control group, with a statistical significance difference.
They also found that the serum sP-Selectin level was found to be 76.9% sensitive and 51.9% specific to predict the need for intensive care treatment and concluded that sP-selectin can be used as a valuable biomarker in both diagnosing and predicting the need for intensive care treatment of COVID-19 infection [27].
Evolving datasets indicate that cytokines like IL-1β, IL-6, IL-17A, IL-9, transforming growth factor-β (TGF-β) and C-C chemokine ligand 2 (CCL-2) promote thrombosis, and other cytokines such as IL-8, IL-10 and TNF-α help in thrombus resolution [28].
In studying the relationship between the incidence of thrombosis and the levels of IL-1β and sP-selectin, there was a statistically significant correlation between serum levels IL-1β and sP-selectin concerning the occurrence of thrombosis in COVID-19 patients.
Mona M. Watany et al. studied 103 hospitalized COVID-19 patients and 50 healthy volunteer controls. COVID-19 patients were categorized into two groups; group 1, which developed thrombosis during hospitalization and group 2, which did not. Soluble selectins were quantitated using the ELISA technique. Higher levels of sP-selectin, sE-selectin and sL-selectin were detected in COVID-19 patients compared to controls. Significantly, higher levels were found in group 1 compared to group 2 [29].
In addition, we found 21 patients who developed thrombosis among the severe group despite receiving anticoagulation, compared to 2 patients only in the mild group, with a statistically significant difference between both groups, which also intensifies this idea.
So, we suggest evaluating the potential role of IL-1β as a therapeutic target in COVID management. Lorenza Landi et al. studied blockage of interleukin-1β with canakinumab in 88 patients hospitalized for Covid-19 pneumonia. Oxygen-support requirements improved, and overall mortality was 13.6% [30].
Conclusions
We concluded that IL-1β and sP-selectin levels could be promising predictors for severe COVID-19 infection and predictable thrombosis in the case of higher levels.
We suggest evaluating the potential role of IL-1β as a therapeutic target in COVID management.
Further studies should be directed toward this topic among a more significant number of patients and different ethnic groups. Also case control studies including healthy controls to compare the differences between controls, non severe and severe COVID-19 patients should be performed, which is considered a limitation of our study.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute severe respiratory distress syndrome
- BMI:
-
Body mass index
- COVID-19:
-
Coronavirus disease of 2019
- CCL-2:
-
C-C chemokine ligand 2
- CRP:
-
C-reactive protein
- CT-chest:
-
Computed tomography of the chest
- CTPA:
-
Computed tomography pulmonary angiography
- EDTA:
-
Ethylenediaminetetraacetic acid
- ELISA:
-
Enzyme-linked immunosorbent assay
- ICU:
-
Intensive care unit
- IL-1β:
-
Interlukin-1beta
- LDH:
-
Lactate dehydrogenase
- PSGL-1:
-
P-selectin glycoprotein ligand-1
- PE:
-
Pulmonary embolism
- RT-PCR:
-
Real-time reverse transcriptase-polymerase chain reaction
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SpO2:
-
Saturation of peripheral oxygen
- sP-selectin:
-
Soluble platelet selectin
- SPSS:
-
Statistical package for the Social Sciences
- TGF-β:
-
Transforming growth factor-β
- TNF:
-
Tumor necrozing factor
- VTE:
-
Venous thromboembolism
- VWF:
-
Von willebrand factor
- WHO:
-
World Health Organization
References
Coronaviridae Study Group of the International Committee on Taxonomy of V. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–44. https://doi.org/10.1038/s41564-020-0695-z.
Gupta A, Al-Tamimi AO, Halwani R, Alsaidi H, Kannan M, Ahmad F. Lipocalin-2, S100A8/A9, and cystatin C: Potential predictive biomarkers of cardiovascular complications in COVID-19. Exp Biol Med. 2022;247(14):1205–13.
Shang W, Dong J, Ren Y, et al. The value of clinical parameters in predicting the severity of COVID-19. J Med Virol. 2020;92:2188–92. https://doi.org/10.1002/jmv.26031.
Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel corona- virus pneumonia. J Thromb Haemost. 2020;18(7):844. https://doi.org/10.1111/jth.14768.
Schulte-Schrepping J, Reusch N, Paclik D, et al. Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell. 2020;182(6):1419–1440 e1423. https://doi.org/10.1016/j.cell.2020.08.001.
Cao, Xuetao. "COVID-19: immunopathology and its implications for therapy." Nat Rev Immunol. 2020;20(5):269–70.
Gupta A, Marzook H, Ahmad F. Comorbidities and clinical complications associated with SARS-CoV-2 infection: an overview. Clin Exp Med. 2022. https://doi.org/10.1007/s10238-022-00821-4.
Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–39. https://doi.org/10.1007/s00281-017-0629-x.
Mehta P, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. https://doi.org/10.1016/S0140-6736(20)30628-0.
Iba T, Levy JH, Levi M, Connors JM, Thachil J. Coagulopathy of coronavirus disease 2019. Crit Care Med. 2020;9:1358–64. https://doi.org/10.1097/CCM.0000000000004458.
Hottz ED, Azevedo-Quintanilha IG, Palhinha L, Teixeira L, Barreto EA, Pão CRR, et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020;136:1330–41.
Salamanna F, Maglio M, Landini MP, Fini M. Platelet functions and activities as potential hematologic parameters related to Coronavirus Disease 2019 (Covid-19). Platelets. 2020;31:627–32.
Zhang S, Liu Y, Wang X, et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol. 2020;13:1–22. https://doi.org/10.1186/s13045-020-00954-7.
McEver RP. Selectins: initiators of leucocyte adhesion and signal- ling at the vascular wall. Cardiovasc Res. 2015;107:331–9. https://doi.org/10.1093/cvr/cvv154.
Pasquali A, Trabetti E, Romanelli MG, et al. Detection of a large deletion in the P-selectin (SELP) gene. Mol Cell Probes. 2010;24:161–5.
Mayadas TN, Johnson RC, Rayburn H, Hynes RO, Wagner DD. Leukocyte rolling and extravasation are severely compromised in P selectin-deficient mice. Cell. 1993;74:541–54.
World Health Organization. Clinical management of COVID-19: interim guidance, 27 May 2020. No. WHO/2019-nCoV/clinical/2020.5. World Health Organization; 2020.
COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Available at https://www.covid19treatmentguidelines.nih.gov.
eBioscience, thermo fisher scientific, Bender MedSystems GmbH | Campus Vienna Biocenter 2 | 1030 Vienna, Austria for descriptions of symbols on product labels or product documents, thermofisher.com/symbols-definition.
Chan YH. Biostatistics102: Quantitative data – Parametric & non-parametric Tests. Singap Med J. 2003a;44(8):391–6.
Chan YH. Biostatistics 103: Qualitative data –tests of Independence. Singap Med J. 2003b;44(10):498–503.
Chan YH. Biostatistics 104: Correlational analysis. Singap Med J. 2003c;44(12):614–9.
Al-Tamimi AO, Yusuf AM, Jayakumar MN, Ansari AW, Elhassan M, AbdulKarim F, Kannan M, Halwani R, Ahmad F. SARS-CoV-2 infection induces soluble platelet activation markers and PAI-1 in the early moderate stage of COVID-19. Int J Lab Hematol. 2022;44(4):712–21. https://doi.org/10.1111/ijlh.13829. Epub 2022 Mar 9.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The lancet. 2020 Feb 15;395(10223):497-506. Tang N, Li D, Wang X, Sun Z. abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–7.
Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–7.
Chiara A, Veronica B, Alessandra S, et al. Elevated P-Selectin in Severe Covid-19: Considerations for Therapeutic Options. Mediterr J Hematol Infect Dis. 2021;13(1).
Emre K, Ramazan S, Emel A, et al. Soluble P-selectin as a potential diagnostic and prognostic biomarker for COVID-19 disease: a case-control study. Life Sci. 2021;277.
Ahmad F, Kannan M, Ansari AW. Role of SARS-CoV-2 -induced cytokines and growth factors in coagulopathy and thromboembolism. Cytokine Growth Factor Rev. 2022;63:58–68. https://doi.org/10.1016/j.cytogfr.2021.10.007. Epub 2021 Oct 24.
Watany MM, Abdou S, Elkolaly R, Elgharbawy N, Hodeib H. Correction to: Evaluation of admission levels of P, E and L selectins as predictors for thrombosis in hospitalized COVID-19 patients [published online ahead of print, 2022 Feb 16]. Clin Exp Med. 2022;1. https://doi.org/10.1007/s10238-022-00802-7.
Lorenza L, Claudia R, Emanuele R, et al. Blockage of interleukin-1β with canakinumab in patients with Covid-19. Sci Rep. 2020;10.
Acknowledgements
Not applicable.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research did not receive any specific grant from public, commercial or not-for-profit funding agencies.
Author information
Authors and Affiliations
Contributions
SA: Designed the study idea and the data collection plan, wrote the study protocol, shared in writing the manuscript and submission and being the corresponding author. RR: Did the laboratory and practical work and shared in writing the manuscript RE: Participated in patient assessment and data collection. AY: Participated in patient assessment and data collection. HA: Shared data organization, analysis, and manuscript writing. WS: Took part in writing the manuscript. RI: Participated in data entry and writing of the manuscript. MA: Participated in data entry and writing of the manuscript. MM: Participated in data analysis and writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the ethical committee, Faculty of Medicine, Beni-Suef University. Approval NO. FMBSUREC/07032021. Written informed consents were taken from the participants. The study was performed following the principles of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abd El-Ghani, S.ES., Hamed, R.M.R., Eid, R.A. et al. Serum interleukin 1β and sP-selectin as biomarkers of inflammation and thrombosis, could they be predictors of disease severity in COVID 19 Egyptian patients? (a cross-sectional study). Thrombosis J 20, 77 (2022). https://doi.org/10.1186/s12959-022-00428-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-022-00428-5