Abstract
Background
This study aimed to assess the predictive value of endometrial blood flow branches on pregnancy outcomes after hormone replacement therapy-frozen embryo transfer (HRT-FET).
Methods
This prospective observational study involved 292 reproductive-aged women who underwent endometrial receptivity assessment in a tertiary care academic medical center in southwest China using power Doppler ultrasonography during HRT-FET. Three-dimensional power Doppler ultrasound was performed on the day of endometrial transformation and the day before embryo transfer. The endometrial blood flow branches of the endometrial and subendometrial regions were compared in the non-pregnant and pregnant groups at the two time points mentioned above.
Results
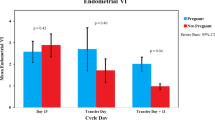
The endometrial blood flow branches were higher in pregnant patients than in non-pregnant patients on the day of endometrial transformation (P = 0.009) and the day before embryo transfer (P = 0.001). Changes in endometrial blood flow pattern and endometrial blood flow branches at the two time points did not differ among the pregnancy outcome samples. After adjusting for age, antral follicles, and embryos transferred, the endometrial blood flow branches on the day before embryo transfer was the independent factor influencing the chance of clinical pregnancy, with an odds ratio of 3.001 (95% confidence interval: 1.448 − 6.219, P = 0.003).
Conclusions
Endometrial blood flow perfusion during the peri-transplantation period of the HRT-FET cycle is a good indicator of pregnancy outcomes, suggesting that valuation of endometrial branches via power Doppler ultrasound is a simple and effective approach for achieving indicator measurements.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Accurate assessment of endometrial development and receptivity remains a challenge in reproductive medicine. None of the endometrial receptivity markers that can be evaluated by endometrial biopsy, endometrial fluid aspiration, or hysteroscopy have sufficient discriminatory value to act as a diagnostic measure for endometrial receptivity [1]. However, ultrasound remains the most non-invasive and reproducible method for evaluating endometrial receptivity compared to invasive procedures, such as histology and molecular research. Previous studies have focused on the effects of independent ultrasound parameters on embryo implantation, including endometrial patterns and thickness, which have been repeatedly tested and compared with pregnancy rates during in vitro fertilization (IVF) cycles with conflicting results [2, 3]. In recent years, some studies have focused on the comprehensive evaluation of ultrasound parameters for predicting endometrial receptivity, including conservative endometrial measurements, endometrial myometrial junction studies, and comprehensive scores of endometrial and subendometrial Doppler indices [4, 5], which are considered to represent better the actual ability of the endometrium to accept embryos.
Among the various ultrasound parameters, endometrial blood flow perfusion is typically considered necessary for embryo implantation. This factor can be non-invasively evaluated and roughly estimated using color Doppler ultrasound; however, power Doppler imaging is more sensitive for detecting low-speed flow, with stronger visibility of small blood vessels, increased accuracy in counting, and high operability [6, 7]. Therefore, power Doppler has the potential to become a daily detection tool for checking the blood supply to the entire endometrium and subendometrial area.
To the best of our knowledge, research on endometrial blood flow correlating power Doppler ultrasound (PD-US) data with hormone replacement therapy-frozen embryo transfer (HRT-FET) pregnancy outcomes remains rare, and the optimal measurement time for pregnancy outcome prediction remains unclear. Moreover, in most independent or comprehensive parameters used to evaluate endometrial receptivity, the evaluation is often limited to a specific time point, such as oocyte retrieval day and embryo transfer day. In this study, we evaluated the role of endometrial receptivity ultrasound parameters in predicting pregnancy on the day of endometrial transformation and the day before embryo transfer in HRT-FET cycles. At the same time, endometrial and subendometrial blood flow changes at two time points were added to evaluate the prediction performance. These results may be used to assess the value of incorporating appropriate endometrial receptivity indicators into routine monitoring during HRT-FET cycles.
Methods
Study subjects
This prospective observational study was conducted at a tertiary care academic medical center in southwestern China. Women who received their first HRT-FET between November 2021 and July 2023 were invited to participate in this study. Based on previous ultrasound, hysterosalpingography, magnetic resonance imaging, or surgical records, patients with stage III and IV endometriosis, adenomyosis, hydrosalpinx, uterine fibroids, history of severe uterine adhesions, endometrial polyps, scarred uterus, or uterine malformations were excluded. Furthermore, patients with a history of recurrent miscarriage or repeated implantation failure (more than three occurrences) were excluded from the study. This study was approved by the Scientific Ethics Committee of Chengdu Women’s and Children’s Central Hospital (reference: B2021-7), and all enrolled patients provided informed consent.
FET procedures
For hormonal replacement therapy cycles, all patients received estradiol (Femoston red tablets; Abbott Biologicals B.V., Olst, NL) treatment at 4 mg orally, with the dosage regulated on a 7-day basis according to endometrial thickness (EMT). If the EMT was < 8 mm, the estradiol dosage was increased. When the EMT reached ≥ 8 mm, and the oral estradiol dosage reached ≥ 14 days, or the clinicians and patients recognized EMT as having a relatively maximum thickness, progesterone was administered to initiate endometrial transformation. The secretory transformation was initiated using fematon-yellow tablets (containing estradiol 2 mg and dydrogesterone 10 mg; Abbott Biologicals B.V.) twice daily, and 40 mg oil-based intramuscular progesterone injection (Zhejiang Xianju Pharmaceutical) once daily was administered from the day of transformation to the day of the pregnancy test.
Power Doppler operation and data collection
Identity 3D power Doppler (3D PD-US, H60, Samsung, Seoul, South Korea) settings with a transvaginal probe of 4 − 9 MHz were used in patients for endometrial receptivity testing on the endometrial transformation day as well as on the day preceding embryo transfer at approximately 1 pm. The settings for this study were as follows: low frequency; signal magnifying, 50; pulse repetition frequency, 0.8 kHz; power Doppler map, 5; and power, 90%. The sector of interest was adjusted to cover the endometrial cavity in the longitudinal plane of the uterus. The color gain was adjusted to 80%±2% to optimize blood flow detection in the small vessels of endometrial and subendometrial areas.
The data produced by the PD-US measurement included EMT, endometrial patterns (classified as type A, trilinear endometrium; type Not-A, no trilinear endometrium), endometrial contraction, endometrial volume, blood flow patterns (type I, the vessels pass through the lateral hypo-echoic band of the endometrium but do not enter the hyper-echoic rim of the endometrium; type II, the vessels pass through the hyper-echoic rim of the endometrium but do not enter the endometrium; type III, the vessels enter the endometrium [8]), and endometrial blood flow branches (countable endometrial and subendometrial blood flow branches in a single plane) (Fig. 1). In this study, the subendometrial region was considered to be within 1 mm of the originally defined myometrial–endometrial contour [9]. The endometrial volume was drawn manually along the endometrial outline. Stored volumes were analyzed using VOCAL software of Three-dimensional (3D) Power Doppler. The results of the ultrasound evaluation did not affect the subsequent clinical procedures. The primary outcome measure was intrauterine clinical pregnancy (defined as the presence of a gestational sac in the uterus determined using ultrasonography).
Power Doppler ultrasound imaging of endometrial and subendometrial blood flow: type-branch. (A) type I - branch<5: the vessels pass through the lateral hypo-echoic band of the endometrium but do not enter the hyper-echoic rim of the endometrium, branch 1. (B) type II - branch<5: the vessels pass through the hyper-echoic rim of the endometrium but do not enter the endometrium, branch 4. (C) type III – branch <5: the vessels enter the endometrium, branch 4
The Kappa test was applied to evaluate the consistency of the endometrial blood flow pattern results, with a Kappa value of 0.778 (P = 0.001). The Kendall W test was used to evaluate the consistency of the endometrial blood flow branches, with the Kendall Wa being 0.979 (P = 0.001). An ROC curve was constructed to explore the cutoff value of EMBLB for Pregnancy outcome.
Statistical analyses
Statistical analyses were performed using the Statistical Program for Social Sciences (SPSS Version 26, IBM Corp, Armonk, NY, USA). Normal distribution was identified using the Shapiro-Wilk test. Data were statistically described in terms of mean ± standard deviation (± SD), median and range, or number of cases (frequencies) when appropriate normality of data was tested. A nonparametric Mann-Whitney U test was used to compare the non-normally distributed data. Other comparisons were performed using the chi-squared and Fisher’s Exact tests, where appropriate. Binary stepwise logistic regression was used to determine the independent predictive factor of clinical pregnancy, adjusting for patient age, antral follicles (AFC), number of embryos transferred, embryo transfer type, good quality embryos transfer, endometrial blood flow, and changes of blood flow at two time points. The results are presented as the odds ratio (OR) and 95% confidence interval (CI). The significance level for all analyses was set at P < 0.05.
Results
A total of 292 patients who underwent HRT-FET met the inclusion criteria and were processed for this study. They completed PD-US tests on the day of endometrial transformation and the day before embryo transfer. Among them, 176 patients achieved clinical pregnancy, including two who had a tubal pregnancy (2/176) and twelve who had spontaneous abortions (12/176). The remaining 116 patients were classified into the non-pregnant group, with an intrauterine pregnancy rate of 59.59% per HRT-FET. The demographic and clinical characteristics of the patients are presented in Table 1.
Discussion
The results of this study demonstrated that measuring the endometrial blood perfusion using PD-US was a simple and effective method for predicting pregnancy outcomes during the HRT-FET cycle. Embryos are estimated to account for one-third of implantation failures, whereas poor endometrial receptivity and altered embryo endometrial dialogue account for the remaining two-thirds [10]. Several studies have examined EMT, endometrial type, subendometrial contraction, and endometrial volume and have attempted to provide a clear overview of the implantation window. However, contradictory findings have been reported [11, 12]. The ultrasound endometrial indicators in our study were not the final factors affecting pregnancy outcomes.
This study evaluated the role of PD-US in predicting pregnancy during HRT-FET cycles by counting endometrial and subendometrial blood flow branches. The pregnant group was younger and had higher AFC values. However, after adjusting for these parameters, the branches of the spiral arteries on the day before transplantation were the only factors that affected pregnancy outcomes. While Wang et al. concluded that the coexistence of endometrial and subendometrial blood flow results in a higher embryo implantation rate [13], our results suggest that blood perfusion is more critical than the endometrial − subendometrial blood flow distribution pattern. Blood supply to the endometrium comes from the radial artery, which passes through the connection between the uterine muscle and endometrium, divides into basal arteries that supply the basal layer, and then forms a spiral artery to reach the surface of the endometrium. At the junction of the myometrium and endometrium, ultrasonography shows a low-echo area called the subendometrial area. Histological studies have confirmed that this area is the innermost layer of the myometrium, or the junction zone [14]. Compared to the outer muscular layer, our results showed that blood flow in the junction zone was more abundant in most cases. Thus, whether the branch enters the endometrium the day before embryo transfer may not be an absolute factor affecting pregnancy outcomes; instead, the richness of blood flow in the endometrium or junction zone is suggested as a predictive factor.
In this study, all eight patients with endometrial blood flow branches > 10 on the progesterone start day were pregnant, while 13 with blood flow branches > 10 on the day before transplantation had conceived. Therefore, we emphasize the possible positive relationship between the abundance of blood flow during the secretory phase and pregnancy; however, it should not be concluded that patients without endometrial or subendometrial blood flow branches have absolutely low implantation and pregnancy rates. In patients with blood flow branch counts of 0 − 1 on either the day of transformation or the day before transplantation, we did not find a linear correlation between no blood flow and pregnancy. These data indicate that there may be a certain threshold for endometrial vascularization that, when reached, has a significant positive impact on clinical pregnancy. Whether the research conclusions can become a reference option for selective embryo transfer or guide clinical medication requires further large-scale prospective cohort studies. For patients with poor blood flow on the day of embryo transfer, can we improve pregnancy outcomes through drugs that increase local endometrial blood flow? The related drug effects will be announced in the future.
Ng et al. [15] reported that the measurement of endometrial and subendometrial blood flow using 3D PD-US could not predict pregnancy well if measured at a time point during IVF treatment. Due to baseline differences between patients in the present study, we compared the changes in 3D PD-US parameters of the endometrium at the two time points. However, we failed to confirm that the changes on the day of endometrial transformation and the day before embryo transfer significantly differed between the pregnant and non-pregnant groups. It has not been confirmed whether this change has any role in predicting HRT-FET results, and the main variable determining pregnancy outcomes is endometrial blood flow during the peri-transplantation period.
This study had the advantage of being the first prospective cohort study to use PD-US to detect endometrial receptive ultrasound indicators at two time points after HRT-FET. Due to the inconsistent Doppler signal waveforms of these small spiral vessels, predicting pregnancy using the spiral artery Doppler flow index is highly controversial [16,17,18]; thus, our study did not measure the subendometrial vascularization flow index but instead chose a more intuitive indicator for assessing blood perfusion. Previous studies have reported that blood flow to the endometrium affects pregnancy outcomes after freeze-thawed embryo transfer; however, the detection methods needed to be more consistent. Jinno et al. [19] measured endometrial tissue blood flow (ETBF) using laser blood flowmetry and found that women with an endometrial microvascular blood flow of at least 29 mL/min per 100 g of tissue in the early luteal phase had a significantly higher pregnancy rate, with 85% of gestational sacs in normal uteri implanted in the uterine regions with the highest measured ETBF. Other studies have demonstrated that vascular endothelial growth factor levels and its receptors significantly increase during the peri-implantation period [20,21,22]. Additionally, 3D Doppler angiography has been shown to quantitatively evaluate the vascular density and blood flow in the endometrium and subendometrium [23]. However, none of these methods have the operability of real-time monitoring during endometrial preparation for FET, whereas 3D PD-US can achieve the convenience of bedside monitoring.
There was a limitation to the current study. Most patients refused to undergo transvaginal ultrasound on the day of embryo transfer. Therefore, after endometrial transformation, we performed a second endometrial receptivity test in the afternoon before transplantation, and there may have been some deviations from the actual values on the day of transplantation.
Conclusion
Measuring the endometrial and subendometrial blood flow branches on the day of the peri-transplantation period during the HRT-FET cycle using PD-US was shown to be a simple and effective method for predicting pregnancy outcomes. In the future, the development of ultrasound may improve the consistency of endometrial blood flow assessment and generate more accurate non-invasive blood flow assessment methods for daily clinical practice, such as microvascular flow ultrasound.
Comparison of characteristics between pregnant and non-pregnant patients
There was a significant difference in age distribution between the pregnancy and non-pregnancy groups (31.57 ± 4.41 years vs. 33.07 ± 4.24 years; P = 0.004) as well as a significant difference in bilateral AFC between the two groups (12.0 (8.0 − 17.0) vs. 10.0 (6.0 − 14.0); P = 0.004). However, both groups did not show significant differences in body mass index, anti-Müllerian hormone levels, the proportion of primary infertility, and the cause of infertility. The fallopian tube was the most common infertility factor in both groups. The proportion of blastocyst transfer cycles (61.49% vs. 51.72%) and good-quality embryo transfer cycles (79.31% vs. 74.14%) was higher in the pregnancy group than in the non-pregnancy group, but without significant difference (Table 1).
Endometrial receptivity indices on the day of endometrial transformation and the day before embryo transfer
Table 2 summarizes the endometrial PD-US indices on the days of endometrial transformation and before transplantation. An ROC curve was constructed to explore the predictive value of EMBLB for Pregnancy outcome, and to find the cut-off value [area under the curve (AUC)0.662, 95% CI 0.559–0.725, cutoff = 5].On the day of endometrial transformation, there were significant differences in blood flow branches among the different clinical pregnancy outcome samples (P = 0.009). On the day before transplantation, endometrial blood flow branches were higher in pregnant patients than in non-pregnant patients (P = 0.001). However, both groups were similar regarding EMT, frequency or direction of endometrial contraction, endometrial blood flow pattern, and endometrial volume at the two time points. All eight patients with endometrial blood flow branches ≥ 10 were pregnant on the day of secretory transformation. Meanwhile, there were 14 patients with endometrial blood flow branches > 10 on the day before transplantation, 13 were pregnant, and the remaining one who was not pregnant was transplanted with a D6 poor-quality blastocyst.
Changes in endometrial blood flow parameters
It was found that different pregnancy outcome samples did not show significant differences in the changes in endometrial blood flow pattern and blood flow branch between the day of progesterone initiation and the day before FET (Table 3).
Logistic regression and receiver operating characteristics curve analysis
Binary stepwise logistic regression analysis was performed to identify the covariates independently associated with the primary outcome of clinical pregnancy (Table 4). After adjusting for age, AFC, number of embryos transferred, embryo level, the proportion of good-quality embryo transfer, endometrial type, and endometrial blood flow branches, and changes of blood flow at two time points, only the endometrial blood flow branches on the day before embryo transfer significantly improved the chance of pregnancy, with ORs of 3.001 (95% CI: 1.448 − 6.219, P = 0.003).
Data Availability
Not applicable.
Abbreviations
- HRT-FET:
-
Hormone Replacement Therapy-Frozen Embryo Transfer
- IVF:
-
In Vitro Fertilization
- PD-US:
-
Power Doppler Ultrasound
- EMT:
-
Endometrial Thickness
- AFC:
-
Antral Follicles
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
- 3D:
-
Three-Dimensional
- ETBF:
-
Endometrial Tissue Blood Flow
- EMP:
-
Endometrial Pattern
- FEC:
-
Frequency of Endometrial Contraction
- DEC:
-
Direction of Endometrial Contraction
- EMBLP:
-
Endometrial Blood Flow Pattern
- EMBLB:
-
Endometrial Blood Flow Branches
- EV:
-
Endometrial Volume
References
Craciunas L, Gallos I, Chu J, Bourne T, Quenby S, Brosens JJ, et al. Conventional and modern markers of endometrial receptivity: a systematic review and meta-analysis. Hum Reprod Update. 2019;25:202–23.
Liu WJ, Nong YQ, Ruan JX, Chen Y, Fan L, Huang QW, et al. Impact of endometrial thickness during menstruation and endometrial scratching on the pregnancy in frozen-thawed embryo transfer. J Obstet Gynaecol Res. 2019;45:619–25.
Oluborode B, Burks H, Craig LB, Peck JD. Does the ultrasound appearance of the endometrium during treatment with assisted reproductive technologies influence pregnancy outcomes? Hum Fertil (Camb). 2022;25:166–75.
Martins RS, Oliani AH, Oliani DV, de Oliveira JM. Continuous endometrial volumetric analysis for endometrial receptivity assessment on assisted reproductive technology cycles. BMC Pregnancy Childbirth. 2020;20:663.
Zhang CH, Chen C, Wang JR, Wang Y, Wen SX, Cao YP, et al. An endometrial receptivity scoring system basing on the endometrial thickness, volume, echo, peristalsis, and blood flow evaluated by ultrasonography. Front Endocrinol (Lausanne). 2022;13:907874.
Ng EH, Chan CC, Tang OS, Yeung WS, Ho PC. The role of endometrial and subendometrial blood flows measured by three-dimensional power doppler ultrasound in the prediction of pregnancy during IVF treatment. Hum Reprod. 2006;21:164–70.
Choi YJ, Lee HK, Kim SK. Doppler ultrasound investigation of female infertility. Obstet Gynecol Sci. 2023;66:58–68.
Applebaum M. The uterine biophysical profile. Ultrasound Obstet Gynecol. 1995;5:67–8.
Ng EH, Chan CC, Tang OS, Yeung WS, Ho PC. Factors affecting endometrial and subendometrial blood flow measured by three-dimensional power doppler ultrasound during IVF treatment. Hum Reprod. 2006;21:1062–9.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101:656–63.
Haas J, Casper RF. Observations on clinical assessment of endometrial receptivity. Fertil Steril. 2022;118:828–31.
Son JB, Jeong JE, Joo JK, Na YJ, Kim CW, Lee KS. Measurement of endometrial and uterine vascularity by transvaginal ultrasonography in predicting pregnancy outcome during frozen-thawed embryo transfer cycles. J Obstet Gynaecol Res. 2014;40:1661–7.
Wang L, Qiao J, Li R, Zhen X, Liu Z. Role of endometrial blood flow assessment with color Doppler energy in predicting pregnancy outcome of IVF-ET cycles. Reprod Biol Endocrinol. 2010;18:122.
Chien LW, Au HK, Chen PL, Xiao J, Tzeng CR. Assessment of uterine receptivity by the endometrial-subendometrial blood flow distribution pattern in women undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2002;78:245–51.
Ng EH, Chan CC, Tang OS, Yeung WS, Ho PC. Changes in endometrial and subendometrial blood flow in IVF. Reprod Biomed Online. 2009;18:269–75.
Sadek S, Matitashvili T, Kovac A, Ramadan H, Stadtmauer L. Assessment of uterine receptivity by endometrial and sub-endometrial blood flow using SlowflowHD in hormone prepared frozen embryo transfer cycles: a pilot study. J Assist Reprod Genet. 2022;39:1069–79.
Tong R, Zhou Y, He Q, Zhuang Y, Zhou W, Xia F. Analysis of the guidance value of 3D ultrasound in evaluating endometrial receptivity for frozen-thawed embryo transfer in patients with repeated implantation failure. Ann Transl Med. 2020;8:944.
Wu HM, Chiang CH, Huang HY, Chao AS, Wang HS, Soong YK. Detection of the subendometrial vascularization flow index by three-dimensional ultrasound may be useful for predicting the pregnancy rate for patients undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2003;79:507–11.
Jinno M, Ozaki T, Iwashita M, Nakamura Y, Kudo A, Hirano H. Measurement of endometrial tissue blood flow: a novel way to assess uterine receptivity for implantation. Fertil Steril. 2001;76:1168–74.
Licht P, Russu V, Lehmeyer S, Wissentheit T, Siebzehnrübl E, Wildt L. Cycle dependency of intrauterine vascular endothelial growth factor levels is correlated with decidualization and corpus luteum function. Fertil Steril. 2003;80:1228–33.
Malamitsi-Puchner A, Sarandakou A, Tziotis J, Stavreus-Evers A, Tzonou A, Landgren BM. Circulating angiogenic factors during periovulation and the luteal phase of normal menstrual cycles. Fertil Steril. 2004;81:1322–7.
Nayak NR, Brenner RM. Vascular proliferation and vascular endothelial growth factor expression in the rhesus macaque endometrium. J Clin Endocrinol Metab. 2002;87:1845–55.
Chen L, Quan S, Li H, Chen C, Xing F, Yu Y. A comparison of endometrial and subendometrial vascularity assessed by three-dimensional ultrasonography and power doppler angiography between healthy fertile women and women with unexplained primary recurrent miscarriage. Fertil Steril. 2011;95:1127–9.
Acknowledgements
We would like to thank the staff of the Department of Assisted Reproduction at Chengdu Women’s and Children’s Central Hospital for their cooperation and support.
Funding
Chengdu Medical Research Project. Project number: 2022 − 171.
Author information
Authors and Affiliations
Contributions
Xue Ke conducted the data analyses and manuscript drafting. XF Liang contributed to the data collection. YH Lin and Fang Wang were responsible for the interpretation of the data and revision of the article. All authors critically reviewed and approved the final version of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Scientific Ethics Committee of Chengdu Women’s and Children’s Central Hospital (reference: B2021-7), and all enrolled patients provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors report no conflict of interest for this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ke, X., Liang, Xf., Lin, Yh. et al. Pregnancy prediction via ultrasound-detected endometrial blood for hormone replacement therapy-frozen embryo transfer: a prospective observational study. Reprod Biol Endocrinol 21, 112 (2023). https://doi.org/10.1186/s12958-023-01164-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-023-01164-9