Abstract
Background
Extraperitoneal and transperitoneal approaches are two common modalities in single-port (SP) robot-assisted radical prostatectomy (RARP), but differences in safety and efficacy between the two remain controversial. This study aimed to compare the perioperative, function, and positive surgical margin of extraperitoneal with transperitoneal approaches SP-RARP.
Methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, this study is registered with PROSPERO (CRD 42023409667). We systematically searched databases including PubMed, Embase, Web of Science, and Cochrane Library to identify relevant studies published up to February 2023. Stata 15.1 software was used to analyze and calculate the risk ratio (RR) and weighted mean difference (WMD).
Results
A total of five studies, including 833 participants, were included in this study. The SP-TPRP group is superior to the SP-EPRP group in intraoperative blood loss (WMD: − 43.92, 95% CI − 69.81, − 18.04; p = 0.001), the incidence of postoperative Clavien-Dindo grade II and above complications (RR: 0.55, 95% CI − 0.31, 0.99; p = 0.04), and postoperative continence recovery (RR: 1.23, 95% CI 1.05, 1.45; p = 0.04). Conversely, the hospitalization stays (WMD: 7.88, 95% confidence interval: 0.65, 15.1; p = 0.03) for the SP-EPRP group was shorter than that of the SP-TPRP group. However, there was no significant difference in operation time, postoperative pain score, total incidence of postoperative complications, and positive surgical margin (PSM) rates between the two groups (p > 0.05).
Conclusions
This study demonstrates that both extraperitoneal and extraperitoneal SP-RARP approaches are safe and effective. SP-TPRP is superior to SP-EPRP in postoperative blood loss, the incidence of postoperative Clavien-Dindo grade II and above complications, and postoperative continence recovery, but it is accompanied by longer hospital stays.
Similar content being viewed by others
Introduction
Minimally invasive surgery has gained widespread popularity globally, and robot-assisted radical prostatectomy (RARP) has emerged as a prominent surgical approach for localized prostate cancer treatment [1,2,3]. In recent years, with the rise of extraperitoneal radical prostatectomy (EPRP), it has become a common surgical approach like transperitoneal radical prostatectomy (TPRP) [4, 5]. Some scholars advocate that EPRP can reduce operation time, blood loss, and postoperative hospital stay while reducing positive surgical margin (PSM) and the incidence of postoperative complications. Conversely, other scholars assert that TPRP provides an improved surgical field of vision, heightened surgical precision, and better safeguarding of the urethra and nerve tissue. In addition, many researchers compared the two surgical approaches. Previous meta-analyses have indicated that EPRP has faster operation time, shorter postoperative hospital stay, and lower postoperative complication rates compared with TPRP [6, 7].
The single-port (SP) RARP was approved by the USA for the treatment of radical prostatectomy in 2018. It has the characteristics of a compact body, minimal trauma, and dual cameras, and it has attracted more and more attention. The SP-RARP can reduce surgical invasiveness and complication rate and can be used as an alternative to traditional multiport RARP [8,9,10]. The SP-RARP can also achieve both extraperitoneal and transperitoneal surgical approaches, yet the disparities in safety and efficacy between these approaches remain unclear, leaving the debate over the optimal surgical technique unresolved. Therefore, it is necessary to summarize and analyze the current studies comparing the two surgical approaches of SP-RARP to fill in the gaps in this field.
This study endeavors to compare the perioperative, function, and positive surgical margin of extraperitoneal with transperitoneal approaches SP-RARP and provide valuable insights to clinicians in their selection of the most suitable surgical method.
Methods
Our meta-analysis adheres to the Cochrane Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11] and was registered with PROSPERO (CRD42023409667) before the study started.
Search strategy
Up to February 2023, we have searched the databases of PubMed, Embase, Web of Science, and Cochrane Library to compare the studies of SP-TPRP and SP-EPRP in the treatment of prostate cancer. We construct the keywords according to the principles of PICOS and use the combination of subject words and free words to search: (((((transperitoneal radical prostatectomy) OR (TPRP)) OR (extraperitoneal radical prostatectomy)) OR (EPRP)) AND (((Robotic Surgical Procedures) OR (Robotics)) OR (Robot-assisted))) AND ((SP) OR (single port)). Additionally, we manually retrieved and reviewed the relevant references of the papers to ensure comprehensiveness and minimize potential omissions.
Study selection
We defined inclusion criteria according to PICOS principles. P(patients): Patients diagnosed with localized prostate cancer; I (intervention): the patient underwent extraperitoneal single-hole robot-assisted radical prostatectomy; C (comparator): the patient underwent SP-EPRP or SP TPRP; O (outcome): The included studies include one or more outcome indicators: perioperative outcome, functional outcome, and oncological outcome; S (study type): a case–control study, cohort study, or randomized controlled trial. Exclusion criteria: (1) conference reports, editorial comments, and conference abstracts; (2) non-comparative research; and (3) no data analysis available.
Data collection
The two observers independently extracted the following data from the research we included (1) general information: first author, publication years, and country; (2) population characteristics: patient age, body mass index (BMI), prostate-specific antigen (PSA) level, prostate size, and tumor stage; (3) perioperative outcomes: operation time, hospital stay, intraoperative blood loss, and postoperative pain score; (4) postoperative total complications; (5) postoperative complications of II grade or above (defined as Clavien-Dindo grade ≥ II); (6) continence recovery (defined as the using no pad or one safety pad/day); and (7) positive surgical margins (PSM). Discrepancies were resolved by a third reviewer.
Bias risk assessment
We used the Newcastle–Ottawa Scale (NOS) (https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp) to evaluate the quality of included non-randomized controlled trials and excluded those with scores < 5, including bias due to (1) case selection, (2) comparability, and (3) outcome reporting. Two reviewers assessed the quality and evidence of the study and resolved the differences through discussion.
Statistical analysis
A meta-analysis was carried out using the Stata15.1 software (StataSE, USA). The results of the dichotomous variables are reported by the risk ratio (RR) and its 95% confidence interval (CI), and the results of the continuous variables are reported by the weighted mean difference (WMD) and its 95%CI. Statistical heterogeneity was evaluated based on I2 statistics. The I2 ≥ 50% indicates significant heterogeneity, using a random effect model, and when I2 < 50%, a fixed effect model is used. We use the leave-one-out method for sensitivity analysis to ensure the stability of the results, that is, delete each study in turn and observe the changes in the results. However, we cannot conduct a sensitivity analysis of three or fewer studies. P ≤ 0.05 means the difference is statistically significant [12].
Results
Baseline characteristics
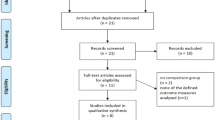
We searched 318 studies from 4 databases, excluded repeated studies, then screened them according to PICOS principles, and finally obtained five studies [10, 13,14,15,16]. The five studies (sample sizes ranging from 34 to 476) were prospective or retrospective cohort studies conducted in the USA, with a total of 833 patients (425 SP-TPRP and 408 SP-EPRP). For more information on the screening process, please see (Fig. 1).
Table 1 summarizes the baseline characteristics and preoperative variables (including prostate volume, pathological stage, age, body weight, etc.). In addition, the two groups were balanced in age (p = 0.957), BMI (p = 0.054), preoperative PSA (p = 0.139), previous abdominal surgery (p = 0.394), biopsy grade (p = 0.995), and prostate volume (p = 0.458) (Supplementary File 1). Table 2 summarizes the perioperative period, function, and positive surgical margin of various studies.
Assessment of quality
The NOS scale was used to score the included literature. All studies had a score of ≥ 5 with a median of 7, with one study [16] scoring 7 and two studies [10, 15] scoring 8. See Table 3 for details.
Outcome analysis
Perioperative outcomes
A total of 5 studies [10, 13,14,15,16] reported the operative time for both SP-EPRP and SP-TPRP surgical approaches, and the meta-analysis results showed no significant difference in operative time (WMD: 3.02 min, 95% CI − 32.49, 38.52; p = 0.868) between the two groups (Fig. 2A).
The meta-analysis of 4 studies [10, 14,15,16] showed that SP-TPRP was associated with a longer hospital stay than SP-EPRP (WMD: 7.88, 95% CI 0.65, 15.10; p = 0.03) (Fig. 2B).
The meta-analysis of 3 studies [10, 14, 15] showed no significant difference between the two groups in postoperative pain scores (WMD − 0.08, 95% CI − 0.40, 0.23; p = 0.6) (Fig. 3A).
The meta-analysis of 5 studies [10, 13,14,15,16] showed that SP-TPRP was associated with a lower intraoperative blood loss than SP-EPRP (WMD − 43.92, 95% CI − 69.81, − 18.04; p = 0.001) (Fig. 3B).
The meta-analysis of 4 studies [10, 14,15,16] showed that SP-TPRP was associated with a lower incidence of postoperative Clavien-Dindo II and above complications than SP-EPRP (RR 0.55, 95% CI 0.31, 0.99; p = 0.04) (Fig. 4A), but there was no significant difference in the incidence of total postoperative complications between the two groups (RR 0.92, 95% CI 0.64, 1.31; p = 0.74) (Fig. 4B).
Furthermore, sensitivity analysis results demonstrated no change in the results for the above perioperative outcomes when we removed each study in turn, suggesting that our results were not influenced by any one study.
Functional outcomes
The meta-analysis of 4 studies [10, 14,15,16] showed that the continence recovery in the SP-TPRP group was better than that in the SP-EPRP group 90 days after the operation (RR 1.23, 95% CI 1.05, 1.45; p = 0.04) (Fig. 5A). Moreover, the results of the sensitivity analysis showed no change in the functional outcomes when we removed each study in turn, suggesting that our results were not influenced by any one study.
Positive surgical margin
The meta-analysis of 4 studies [10, 14,15,16] showed no significant difference between the two groups in PSM (RR 1.03, 95% CI 0.80, 1.32; p = 0.8) (Fig. 5B). Furthermore, the sensitivity analysis reiterated no change in the PSM when we removed each study in turn, suggesting that our results were not influenced by any one study.
Heterogeneity
Among the seven outcome indicators analyzed in this study, four indicators had moderate or low heterogeneity. However, the hospital stays (I2 = 94.0%, p = 0.03), operation time (I2 = 96.2%, p = 0.868), and blood loss (I2 = 75.4%, p = 0.001) were highly heterogeneous. Given the limited number of included studies, we conducted a meta-regression based on publication year and sample size, as outlined. In accordance with the outcomes of the meta-regression analysis, the potential origins of heterogeneity appear to stem from disparities in publication year and the variations in the size of incorporated research cohorts (P > 0.05), as shown in Supplementary File 2.
In light of the constrained inclusivity of the available studies, further subdivision analyses at a sub-group level were regrettably deferred.
Sensitivity analysis and publication bias
Given the considerable heterogeneity observed in certain outcomes (EBL, LOS, and OT), we conducted sensitivity analyses on the target parameters. Through leave-one-out re-calculation of effect sizes, the results demonstrate the robustness of the findings. Assessment using funnel plots revealed no evidence of publication bias (OT, EBL, LOS), further supported by Begg’s regression tests (P > 0.05) (Supplementary File 3), ensuring the integrity of our conclusions in light of potential biases.
Discussion
To our knowledge, this is the first systematic review and meta-analysis comparing extraperitoneal with transperitoneal surgical approaches in SP-RARP for prostate cancer. We found that both extraperitoneal and transperitoneal SP-RARP are safe and effective. SP-TPRP is superior to SP-EPRP in blood loss, the incidence of postoperative Clavien-Dindo grade II and above complications, and continence recovery, but it is accompanied by a longer hospital stay, which is worthy of our in-depth discussion.
In this study, we extracted the perioperative outcome indicators of SP-EPRP and SP-TPRP surgical approaches for prostate cancer, including operation time, hospital stay, postoperative pain score, blood loss, and the incidence of postoperative complications. The results of the meta-analysis showed that there was no significant difference in operation time between SP-EPRP and SP-TPRP. This is different from the results of previous studies. Uy et al. [6] compared the outcomes of extraperitoneal with transperitoneal surgical approaches in multiport RARP and found that EPRP had a shorter operation time than TPRP. Since EPRP can directly reach the prostate tissue without going through the peritoneum and abdominal cavity during the operation, it has an advantage over TPRP in terms of operation time [7, 17, 18]. The following reasons may lead to this difference: First of all, SP-RARP is a relatively new and complicated surgical method, and the surgical experience of doctors may affect the operation time. Among the studies we included, two studies reported that most surgeons were more proficient in SP-TPRP but less experienced in SP-EPRP, which resulted in the surgery time of SP-EPRP being longer than SP-TPRP [10, 13]. In addition, the patient’s BMI is also an important factor affecting the time of operation [13, 16]. Obesity exerts a discernible impact on the surgical duration and physiological parameters during robot-assisted laparoscopic prostatectomy (RALP). Notably, within the context of transperitoneal robot-assisted laparoscopic prostatectomy (TP RALP), individuals presenting with elevated BMI and assuming the Trendelenburg position tend to exhibit appreciably prolonged operative durations, a pattern that manifests conspicuously [19, 20]. The thicker the abdominal wall fat of the patient, the longer it takes the surgeon doctor to separate the abdominal fat and the longer the operation time [21]. If these biases can be controlled, we expect that the operation time for SP-EPRP will be shorter. In this study, our meta-analysis found that SP-TPRP had a longer hospital stay than SP-EPRP. This may be related to the possibility of peritoneal irritation and intestinal obstruction caused by TPRP [22, 23]. During the operation, since EPRP bypasses the intestine, contact with the intestine is greatly reduced, and intestinal recovery is faster, so the patient’s hospital stay is shortened [24, 25]. While the postoperative pain differential remains inconspicuous between the two approaches, recent investigations have unveiled a superior analgesic efficacy of percutaneous transversus abdominis plane (TAP) block for patients undergoing RARP compared to conventional local anesthetic port infiltration [26, 27]. Employing a robotic-assisted transperitoneal route, this innovative technique specifically targets the anterior branches of the intercostal nerves T7–T11, subcostal nerve T12, ilioinguinal nerve, and iliohypogastric nerve at the TAP plane, intricately interwoven within the sensory neural supply of the skin, musculature, and abdominal wall peritoneal dome [28]. This promising advancement holds the potential to confer a heightened postoperative experience for individuals opting for the SP-TPRP approach.
It should be noted that studies [29, 30] have shown that the patient’s previous abdominal surgery history does not usually affect the incidence of complications after RARP. There was no statistically significant difference in the incidence of total complications between SP-TPRP and SP-EPRP, as was also the case in multiport RARP [31]. However, we found that SP-TPRP has a lower incidence of postoperative Clavien-Dindo II and above complications compared to SP-EPRP. Balasubranian et al. [16] and Zeinab et al. [10] pointed out that SP-EPRP has a higher incidence of lymphoid cysts than SP-TPRP. This may be due to the fact that although SP-EPRP does not destroy the intraperitoneal structure, its operating space is limited, and it lacks lymphatic channels to absorb fluid. Keeping the peritoneal space open during operation or during lymph node dissection may help to reduce such complications. In addition, Reddy et al. [32] pointed out that SP-RARP can provide deterministic treatment of lymphoid cysts and reduce the number of days of abdominal drainage while reducing surgical invasion, but the drainage of lymphocele is also related to the experience of the operator. Therefore, SP-RARP has the advantage of being less invasive, and its postoperative complications, if acceptable, will not affect its rising status in the treatment of prostate cancer.
Our meta-analysis showed that the continence recovery in the SP-TPRP group was better than that in the SP-EPRP group 90 days after the operation. This may be due to the fact that SP-TPRP can better protect the urethral sphincter and external urethral sphincter and reduce the incidence of postoperative continence recovery. It should be noted that intraoperative procedures may affect patients’ continence recovery, such as nerve preservation techniques [33, 34]. In addition, the experience of the surgeon (such as inexperience in SP-RARP or EPRP) and the specific conditions of the patient (such as external urethral sphincter or tissue infiltration around the sphincter) may affect the results. The results of the meta-analysis showed that there was no significant difference in PSM between SP-EPRP and SP-TPRP. The results indicate that the SP-RARP of the two surgical approaches is safe and effective. It should be noted that due to the narrow surgical field of view during SP-RARP, the capsule may be accidentally cut open when surgical instruments are used to remove the prostate through the pelvic levator anal muscle, resulting in occasional false-positive edges [35]. In addition, Freedland et al. [36] found that prostate weight was significantly correlated with postoperative PSM. Consequently, future studies can provide further interpretation by better control of relevant variables.
In recent years, the literature has featured reports examining the feasibility and safety of the SP RARP technique [37]. In comparison to the conventional MP RARP, SP RARP has demonstrated a reduction in superfluous surgical incisions, potentially affording patients an improved postoperative experience with fewer complications [38]. Consequently, a comparative analysis between these two surgical modalities has become indispensably warranted.
In 2021, Fahmy et al. [39] undertook a comprehensive meta-analysis, revealing that SP RARP may potentially lead to shortened hospitalization periods and diminished postoperative pain. However, there were no discernible differences between the two approaches concerning operative time, blood loss, and similar indicators. The validity of these findings was, however, constrained by uncontrollable biases inherent in the included studies. Therefore, for a more conclusive assessment of the comparison between SP RARP and MP RARP techniques in the future, a well-designed randomized controlled trial and long-term follow-up will remain imperative.
At present, SP-RARP is a developing technology, but there are still some problems, such as technical difficulties, lack of experience, and limited available data [40]. The choice of SP-EPRP and SP-TPRP should take into account the experience of the surgeon and the specific conditions of the patient. For experienced surgeons, there is no absolute difference between the two methods. For patients, for patients with low BMI, medium, or small prostate tumors, Moschovas et al. [41] recommend SP-RARP. This is because the patient’s BMI and prostate volume will affect the grasping strength and range of motion of the robotic arm during SP.
Limitations
Several limitations warrant acknowledgment. First of all, the studies we included are medium-quality retrospective studies with a small sample size, which may lead to the risk of selection bias and reduce the credibility of the results. While the entirety of the investigations was conducted within the ambit of the USA, several of our study metrics yet attain noteworthy levels. Adhering to plausible confounding variables, we conducted a meta-regression analysis; however, due to the constraints imposed by the number of studies included, our capacity to undertake further granularity through sub-group analyses remains circumscribed. We hope that more researchers will pay attention to this topic in the future. Second, even if we use modern statistical methods, some problems still cannot be solved, such as the experience of the surgeons that may interfere with surgical outcomes, nerve-preserving procedures, selection of patient surgical approaches, and other immeasurable confounding factors. Third, most of the studies we included have insufficient median follow-up time, which may lead to a one-sided analysis and lack of comparison of long-term postoperative results between the two groups.
Conclusions
This study demonstrates that both extraperitoneal and extraperitoneal SP-RARP approaches are safe and effective. Notably, SP-TPRP is superior to SP-EPRP in postoperative blood loss, the incidence of postoperative Clavien-Dindo grade II and above complications, and postoperative continence recovery, but it is accompanied by longer hospital stays. Our findings supplement the comparative data of the two surgical methods, but there are few high-quality studies at present, and this result needs to be further verified by follow-up studies.
Availability of data and materials
The data that supports the findings of this study is available from the corresponding authors upon reasonable requests.
References
Lowrance WT, Eastham JA, Savage C, Maschino AC, Laudone VP, Dechet CB, Stephenson RA, Scardino PT, Sandhu JS. Contemporary open and robotic radical prostatectomy practice patterns among urologists in the United States. J Urol. 2012;187:2087–92.
Oberlin DT, Flum AS, Lai JD, Meeks JJ. The effect of minimally invasive prostatectomy on practice patterns of American urologists. Urol Oncol. 2016;34(255):e251-255.
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, Freedland SJ, Greene K, Klotz LH, Makarov DV, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options. J Urol. 2018;199:683–90.
Martini A, Falagario UG, Villers A, Dell’Oglio P, Mazzone E, Autorino R, Moschovas MC, Buscarini M, Bravi CA, Briganti A, et al. Contemporary techniques of prostate dissection for robot-assisted prostatectomy. Eur Urol. 2020;78:583–91.
Semerjian A, Pavlovich CP. Extraperitoneal robot-assisted radical prostatectomy: indications, technique and outcomes. Curr Urol Rep. 2017;18:42.
Uy M, Cassim R, Kim J, Hoogenes J, Shayegan B, Matsumoto ED. Extraperitoneal versus transperitoneal approach for robot-assisted radical prostatectomy: a contemporary systematic review and meta-analysis. J Robot Surg. 2022;16:257–64.
Lee JY, Diaz RR, Cho KS, Choi YD. Meta-analysis of transperitoneal versus extraperitoneal robot-assisted radical prostatectomy for prostate cancer. J Laparoendosc Adv Surg Tech A. 2013;23:919–25.
Bertolo R, Garisto J, Gettman M, Kaouk J. Novel system for robotic single-port surgery: feasibility and state of the art in urology. Eur Urol Focus. 2018;4:669–73.
Dobbs RW, Halgrimson WR, Talamini S, Vigneswaran HT, Wilson JO, Crivellaro S. Single-port robotic surgery: the next generation of minimally invasive urology. World J Urol. 2020;38:897–905.
Abou Zeinab M, Beksac AT, Ferguson E, Kaviani A, Moschovas MC, Joseph J, Kim M, Crivellaro S, Nix J, Patel V, Kaouk J. Single-port extraperitoneal and transperitoneal radical prostatectomy: a multi-institutional propensity-score matched study. Urology. 2023;171:140–5.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Abaza R, Martinez O, Murphy C, Urkmez A, Davis J. Adoption of single-port robotic prostatectomy: two alternative strategies. J Endourol. 2020;34:1230–4.
Kaouk J, Aminsharifi A, Wilson CA, Sawczyn G, Garisto J, Francavilla S, Abern M, Crivellaro S. Extraperitoneal versus transperitoneal single port robotic radical prostatectomy: a comparative analysis of perioperative outcomes. J Urol. 2020;203:1135–40.
Abou Zeinab M, Beksac AT, Ferguson E, Kaviani A, Kaouk J. Transvesical versus extraperitoneal single-port robotic radical prostatectomy: a matched-pair analysis. World J Urol. 2022;40:2001–8.
Balasubramanian S, Shiang A, Vetter JM, Henning GM, Figenshau RS, Kim EH. Comparison of three approaches to single-port robot-assisted radical prostatectomy: our institution’s initial experience. J Endourol. 2022;36:1551–8.
Davis JW, Achim M, Munsell M, Matin S. Effectiveness of postgraduate training for learning extraperitoneal access for robot-assisted radical prostatectomy. J Endourol. 2011;25:1363–9.
Ragavan N, Dholakia K, Ramesh M, Stolzenburg JU. Extraperitoneal vs. transperitoneal robot-assisted laparoscopic radical prostatectomy-analysis of perioperative outcomes, a single surgeon’s experience. J Robot Surg. 2019;13:275–81.
Blecha S, Harth M, Zeman F, Seyfried T, Lubnow M, Burger M, Denzinger S, Pawlik MT. The impact of obesity on pulmonary deterioration in patients undergoing robotic-assisted laparoscopic prostatectomy. J Clin Monit Comput. 2019;33:133–43.
Gu X, Araki M, Wong C. Does elevated body mass index (BMI) affect the clinical outcomes of robot-assisted laparoscopic prostatectomy (RALP): a prospective cohort study. Int J Surg. 2014;12:1055–60.
Sundi D, Reese AC, Mettee LZ, Trock BJ, Pavlovich CP. Laparoscopic and robotic radical prostatectomy outcomes in obese and extremely obese men. Urology. 2013;82:600–5.
Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992;77:162–84.
Yonekura H, Hirate H, Sobue K. Comparison of anesthetic management and outcomes of robot-assisted vs pure laparoscopic radical prostatectomy. J Clin Anesth. 2016;35:281–6.
Chung JS, Kim WT, Ham WS, Yu HS, Chae Y, Chung SH, Choi YD. Comparison of oncological results, functional outcomes, and complications for transperitoneal versus extraperitoneal robot-assisted radical prostatectomy: a single surgeon’s experience. J Endourol. 2011;25:787–92.
Jacobs BL, Montgomery JS, Dunn RL, Weizer AZ, Miller DC, Wood DP, Wolf JS Jr, Zhang Y, Wei JT, Hollenbeck BK. A comparison of extraperitoneal and intraperitoneal approaches for robotic prostatectomy. Surg Innov. 2012;19:268–74.
Shahait M, Yezdani M, Katz B, Lee A, Yu SJ, Lee DI. Robot-assisted transversus abdominis plane block: description of the technique and comparative analysis. J Endourol. 2019;33:207–10.
Taha T, Sionov BV, Rosenberg P, Stein A, Tsivian M, Sidi A, Tsivian A. Pain control after laparoscopic radical prostatectomy: comparison between unilateral transversus abdominis plane block and wound infiltration. Urol Int. 2019;103:19–24.
McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193–7.
Ginzburg S, Hu F, Staff I, Tortora J, Champagne A, Salner A, Shichman SJ, Kesler SS, Wagner JR, Laudone VP. Does prior abdominal surgery influence outcomes or complications of robotic-assisted laparoscopic radical prostatectomy? Urology. 2010;76:1125–9.
Weldon VE, Tavel FR, Neuwirth H, Cohen R. Patterns of positive specimen margins and detectable prostate specific antigen after radical perineal prostatectomy. J Urol. 1995;153:1565–9.
Tholomier C, Couture F, Ajib K, Preisser F, Bondarenko HD, Negrean C, Karakiewicz P, El-Hakim A, Zorn KC. Oncological and functional outcomes of a large Canadian robotic-assisted radical prostatectomy database with 10 years of surgical experience. Can J Urol. 2019;26:9843–51.
Reddy S, Moschovas MC, Bhat S, Noel J, Helman T, Perera R, Rogers T, Patel V. Minimally invasive lymphocele drainage using the Da Vinci® single port platform: step-by- step technique. Int Braz J Urol. 2022;48:363–4.
Wagaskar VG, Mittal A, Sobotka S, Ratnani P, Lantz A, Falagario UG, Martini A, Dovey Z, Treacy PJ, Pathak P, et al. Hood technique for robotic radical prostatectomy-preserving periurethral anatomical structures in the space of retzius and sparing the pouch of Douglas, enabling early return of continence without compromising surgical margin rates. Eur Urol. 2021;80:213–21.
Holze S, Mende M, Healy KV, Koehler N, Gansera L, Truss MC, Rebmann U, Degener S, Stolzenburg JU. Comparison of various continence definitions in a large group of patients undergoing radical prostatectomy: a multicentre, prospective study. BMC Urol. 2019;19:70.
Lenfant L, Garisto J, Sawczyn G, Wilson CA, Aminsharifi A, Kim S, Schwen Z, Bertolo R, Kaouk J. Robot-assisted radical prostatectomy using single-port perineal approach: technique and single-surgeon matched-paired comparative outcomes. Eur Urol. 2021;79:384–92.
Freedland SJ, Isaacs WB, Platz EA, Terris MK, Aronson WJ, Amling CL, Presti JC Jr, Kane CJ. Prostate size and risk of high-grade, advanced prostate cancer and biochemical progression after radical prostatectomy: a search database study. J Clin Oncol. 2005;23:7546–54.
Kaouk J, Garisto J, Bertolo R. Robotic urologic surgical interventions performed with the single port dedicated platform: first clinical investigation. Eur Urol. 2019;75:684–91.
Ju GQ, Wang ZJ, Shi JZ, Zhang ZQ, Wu ZJ, Yin L, Liu B, Wang LH, Xu DL. A comparison of perioperative outcomes between extraperitoneal robotic single-port and multiport radical prostatectomy with the da Vinci Si Surgical System. Asian J Androl. 2021;23:640–7.
Fahmy O, Fahmy UA, Alhakamy NA, Khairul-Asri MG. Single-port versus multiple-port robot-assisted radical prostatectomy: a systematic review and meta-analysis. J Clin Med. 2021;10(24):5723.
Kim KH, Song W, Yoon H, Lee DH. Single-port robot-assisted radical prostatectomy with the da Vinci SP system: a single surgeon’s experience. Investig Clin Urol. 2020;61:173–9.
Covas Moschovas M, Bhat S, Onol F, Rogers T, Patel V. Early outcomes of single-port robot-assisted radical prostatectomy: lessons learned from the learning-curve experience. BJU Int. 2021;127:114–21.
Acknowledgements
Thanks to Mr. Liu Yang for his encouragement and support.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by YJ and XH. The first draft of the manuscript was written by YJ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. The demographics of the studies.
Additional file 2.
The potential origins of heterogeneity appear to stem from disparities in publication year and the variations in the size.
Additional file 3.
Assessment using funnel plots revealed no evidence of publication bias.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, Y., Liu, Y., Qin, S. et al. Perioperative, function, and positive surgical margin in extraperitoneal versus transperitoneal single port robot-assisted radical prostatectomy: a systematic review and meta-analysis. World J Surg Onc 21, 383 (2023). https://doi.org/10.1186/s12957-023-03272-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03272-7