Abstract
Background
In recent years, neoadjuvant immunotherapy with chemotherapy has shown increasing promise for locally advanced non-small cell lung cancer (NSCLC). However, to establish its clinical efficacy and safety, it is imperative to amass more real-world clinical data. This retrospective study aims to assess the safety and effectiveness of combing sintilimab, a PD-1 inhibitor, with chemotherapy as a neoadjuvant treatment modality in patients diagnosed with potentially resectable NSCLC.
Methods
We retrospectively reviewed patients with stage II-III NSCLC receiving neoadjuvant chemoimmunotherapy in Sichuan Cancer Hospital between February 2021 and February 2023. Sintilimab injection (intravenously,200 mg, iv, d1, q3w) and platinum-based chemotherapy were administered intravenously every 3 weeks, with radical lung cancer resection planned approximately 4–11 weeks after the last dose. The primary endpoint of the study was pathologic complete response (pCR). The secondary endpoints were objective response rate (ORR), and safety.
Result
Thirteen patients were enrolled, they were mostly diagnosed with stage III NSCLC (IIB 15.4% IIIA 38.5%; IIIB 46.2%). Most of them had pathologically confirmed squamous cell carcinoma (69.2%).
All patients received sintilimab combined with platinum-based chemotherapy for 2 to 4 cycles. Notably, none of the patients necessitated a reduction in initial dosages or treatment postponement due to intolerable adverse events. Then, all of them underwent surgical operation. Impressively, nine patients (69.2%) achieved a pathologic complete response. The objective response rate (ORR) stood at 46.15%. Nine patients experienced neoadjuvant treatment-related adverse events (TRAEs), with only one patient (7.6%) encountering a grade 4 neoadjuvant TRAE.
Conclusion
Therefore, the current study suggested that neoadjuvant sintilimab plus platinum-based chemotherapy can be a safe approach in increasing the efficiency of treatment and hopefully improving the prognosis of patients with potentially resectable locally advanced NSCLC.
Similar content being viewed by others
Introduction
The global cancer statistics report of 2022 revealed lung cancer’s sustained status as the leading cause of cancer-related mortality, claiming an estimated 0.6 million lives (27.2%) [1]. Notably, non-small-cell lung cancer (NSCLC) comprised 80% of all newly diagnosed cases of lung cancer. For stage III patients, the overarching therapeutic objective is curative surgical resection. However, patients with sizable or invasive tumors, as well as those with inoperable conditions, have historically been treated with neoadjuvant chemotherapy and chemoradiotherapy. Nevertheless, a meta-analysis of preoperative chemotherapy demonstrated a marginal 5% increase in the 5-year overall survival rate, rising from 40 to 45% [2]. Furthermore, a phase 3 randomized trial unveiled superior objective response, pathologic complete response (pCR), and R0 resection rates in patients who underwent chemoradiotherapy prior to surgery, as compared to those treated with chemotherapy alone. In spite of all of these, the incorporation of radiotherapy yielded no enhancements in event-free survival (the primary endpoint) or overall survival, and the pCR rate remained a modest 16% [3]. This predicament calls for novel therapeutic approaches.
At present, from ICIs (immune checkpoint inhibitors) alone to combination with chemotherapy, ICIs as neoadjuvant immunotherapy for NSCLC are evolving at a rapid pace and have acquired a certain effect [4]. The primary tumor can be used to be an antigen source, and neoadjuvant can facilitate the early development of memory T cells and induce a strong adaptive antitumor response. This mechanism was first explored by J Liu et al. in preclinical mouse models of triple-negative breast cancer [5]. Their investigation involved the inoculation of 4T1.2 tumors into BALB/c FOXP3-GFP-DTR mice (FOXP3-DTR), where all regulatory T cells (Tregs), characterized by CD4 + FOXP3 + expression, were marked with green fluorescent protein (GFP) and carried the human diphtheria toxin (DT) receptor, enabling conditional depletion via DT treatment. The findings underscored the superiority of neoadjuvant Treg depletion in eradicating metastatic disease when compared to adjuvant Treg depletion immunotherapy.
The present study aimed to describe the efficacy and safety of sintilimab plus platinum-based chemotherapy as neoadjuvant chemoimmunotherapy in patients with locally advanced NSCLC.
Materials and methods
Patients
The study was a retrospective study conducted at the Sichuan Cancer Hospital. The comprehensive analysis of medical records from consecutive patients who underwent therapy within the timeframe spanning February 2021 to February 2023 was undertaken. Inclusion criteria for participant selection were defined as follows: (1) verification of non-small cell lung cancer (NSCLC) at stages II–III through imaging and histological assessment prior to surgery, (2) Suitability for neoadjuvant chemoimmunotherapy (involving Sintilimab along with platinum-based chemotherapy), with subsequent capability to undergo radical lung cancer surgery post-evaluation, (3) Adherence to the Eastern Cooperative Oncology Group (ECOG) performance status criterion: ECOG ≤ 1. Conversely, the exclusion criteria were enumerated as follows: (1) NSCLC, stages II–III confirmed by imaging and histologically examination before surgery, (2) feasible neoadjuvant chemoimmunotherapy (Sintilimab plus platinum-based chemotherapy) and were able to undergo radical surgery for lung cancer after assessment, (3) ECOG score standard: ECOG ≤ 1. The exclusion criteria were as follows: (1) received chemotherapy, radiotherapy, or immunotherapy previously, (2) PD-1 inhibitors or chemotherapy intolerance, (3) complicated with other malignant tumors, (4) liver, kidney, or other organ dysfunction, (5) serious uncontrolled repeated infection or other serious uncontrolled concomitant diseases.
Drug treatment and surgical methods
Thirteen patients were enrolled and all of them received sintilimab as neoadjuvant immunotherapy. The specific cycles and concomitant neoadjuvant chemotherapy regimen were determined by the physician in charge. Surgery was planned 4–11 weeks after the last dose. All patients received radical lung cancer resection that refers to the complete resection of tumors and regional lymph nodes in strict accordance with surgical specifications. The specific surgical method and adjuvant treatment were adopted according to the individual clinical condition of the patient.
Study endpoints
The primary endpoint of the study was pathologic complete response (pCR). The secondary endpoints were objective response rate (ORR), and safety. ORR was evaluated according to RECIST 1.1 criteria before surgery. The safety of the neoadjuvant chemoimmunotherapy was evaluated by the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 5.0 [6].
Evaluation of efficacy
Before treatment, patients had chest computed tomography (CT), positron emission tomography-computed tomography (PET/CT), and brain magnetic resonance imaging (MRI) as baseline tumor evaluation. The radiological response of the tumor was assessed after 2 cycles of neoadjuvant and before the operation according to the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1. The indicators included complete response (CR), partial response (PR), stable disease (SD), and disease progression (PD). The pathologic responses to neoadjuvant therapy were obtained from pathological specimens after surgery. Pathological complete response (pCR) was defined as tumor regression with no residual tumor on pathology.
Statistical analysis
All statistical analyses were performed using SPSS version 27.0 (IBM, New York, USA). All the statistical tests were two-sided with a significance level of p < 0.05.
Result
Patient characteristics
In total, 13 patients were eligible and enrolled in the present study. A comprehensive depiction of their demographic and clinical attributes is presented in Table 1. The participant composition included 12 males and 1 female, with a predominant diagnosis of stage III NSCLC (IIB 15.4% IIIA 38.5%; IIIB 46.2%). Most of them had pathologically confirmed squamous cell carcinoma (69.2%). Three patients received 2 cycles, five patients received 3 cycles, and five patients received 4 cycles. The median interval time between the last neoadjuvant treatment and operation was 37 days (IQR 28–77).
Efficacy and safety
The median follow-up time was 6 months (2–15 months), and there were no deaths among these participants. After neoadjuvant treatment, six patients achieved a partial response (PR) while seven achieved stable disease (SD) according to RECIST 1.1 criteria. Specially, the radiological assessment of patient 3 showed over 50% tumor shrinkage (Fig. 1). The objective response rate (ORR) was 46.15%. All of them underwent surgical operation (Table 2) and nine patients (69.23%) achieved pCR (Table 3 and Fig. 2 Outcomes of neoadjuvant treatment).
All adverse events (AEs) were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 5.0. The recorded AEs were mainly grade 1, and only one patient experienced severe AEs (SAEs, grade ≥ 3). The majority of grade 1 AEs included decreased Hb count (62%), and increased alanine aminotransferase (46%) (Table 4). With symptomatic treatment, all patients with AEs were normalized and no AEs resulted in the discontinuation of neoadjuvant therapy.
Discussion
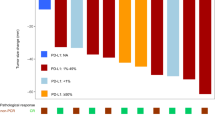
Numerous lines of evidence underscore the value of neoadjuvant therapy in lung cancer, as it affords the opportunity to uncover latent metastases, address comorbidities, and implement strategies such as preoperative smoking cessation and pulmonary “pre-habilitation” techniques [7]. Nevertheless, as mentioned earlier, the improvement of overall survival with neoadjuvant chemotherapy is less than satisfactory. The data of pathologic responses with neoadjuvant chemotherapy is relatively low for NSCLC (MPR < 20% and pCR ≤ 4%) [8]. The emergence of neoadjuvant immunotherapy and neoadjuvant chemoimmunotherapy has shown promise in circumventing this predicament. Notably, a meta-analysis encompassing seven studies on neoadjuvant immunotherapy indicated MPR rates spanning 18–45%, with corresponding pCR rates ranging from 4.9 to 27.3% [9]. A pivotal milestone in this field was Checkmate 159 clinical trial, which introduced neoadjuvant immunotherapy in limited-stage NSCLC patients. In this study, patients who were surgically resectable early (stage I, II, or IIIA) NSCLC received nivolumab every 2 weeks (at a dose of 3 mg per kilogram of body weight), and surgery was planned approximately 4 weeks after the first dose. This regimen induced a major pathological response in 45% (9 of 20) of resected tumors [10]. LCMC3 trial administered atezolizumab as neoadjuvant therapy, resulting in a major pathological response for 45% of the resected tumors (29 out of 143) [11]. NEOSTAR study, a phase 2, open-label, single-institution, randomized trial, evaluated Nivolumab or Nivolumab plus ipilimumab, administered intravenously. The MPR rate was 22% (5 of 23) and 38% (8 of 21) respectively [12]. And one study about neoadjuvant sintilimab was set by Li N et al., a total of 40 patients with NSCLC were enrolled. They received 2 doses of sintilimab and 37 patients underwent radical resection. Among 37 patients, 15(40.5%) patients achieved MPR, and 6 (16.2%) patients had complete pathologic response (pCR) [13].
Immunotherapy does not have a direct cytotoxic effect targeting tumor cells to reduce tumor volume, however, chemotherapy dose [14]. However, an interesting trend has emerged in recent years regarding the shifting landscape of immunotherapy trials. The average planned enrollment for immunotherapy trials has experienced a substantial decline of more than 500% over the past 7 years, plummeting from 854 participants in 2014 to 131 participants in 2020 [15]. This shift has seen combination therapies take center stage in clinical trials involving PD1/PDL1 inhibitors, gradually becoming the focus of research endeavors. This trend has also paved the way for the rise of neoadjuvant chemoimmunotherapy as a potential treatment. Several studies reported the effectiveness of neoadjuvant chemoimmunotherapy for NSCLC which seemed better than neoadjuvant immunotherapy alone, because of higher MPR and pCR rate. The most encouraging is the NADIM study [16]. Patients received nivolumab combined with paclitaxel and carboplatin for 3 cycles before surgical resection. Forty-one patients underwent surgery, the rate of MPR was 83% (34 of 41), and the rate of pCR was 63.4% (26 of 41).
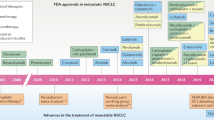
Checkmate 816 trial, an open-label, phase III clinical study focusing on patients with stage IB–IIIA NSCLC, compared neoadjuvant nivolumab plus platinum-based chemotherapy with chemotherapy alone. In this study, the pCR rate was 24.0% versus 2.2%, and the MPR rate was 36.9% versus 8.9% [17]. NCT02716038 was an open-label, phase III trial, and patients received atezolizumab with carboplatin plus nab-paclitaxel [18]. Eleven patients were successfully operated upon, and 7/14 (50%) patients achieved MPR, including 3 patients (21%) with pCR. In SAKK16/14 trail, neoadjuvant treatment consisted of 3 cycles of cisplatin plus docetaxel followed by 2 cycles of durvalumab [19]. Finally, 55 patients underwent resection. Thirty-four patients (62%) achieved MPR, including 10 patients (18%) with pCR. We listed all studies in Fig. 3 and Table 5. Furthermore, a number of neoadjuvant chemoimmunotherapy studies were ongoing: Keynote-671 (NCT03425643), IMpower-030 (NCT03456063), and AEGEAN study (NCT03800134), and all above were randomized, double-blind, phase III clinical studies. These studies involve the administration of pembrolizumab, atezolizumab, and durvalumab in combination with platinum chemotherapy, with the objective of comparing the efficacy of neoadjuvant chemoimmunotherapy to chemotherapy alone in patients with resectable NSCLC.
Sintilimab can bind to PD-1, blocking the interaction of PD-1 with its ligands, and then it can help to recover the anti-tumor response of T cells. Wang J et al. conducted a surface plasmon resonance (SPR) analysis to assess the binding of sintilimab, nivolumab, and pembrolizumab to human PD-1. Their findings indicated that sintilimab exhibited the highest affinity among the three anti-PD-1 monoclonal antibodies [20]. Furthermore, an evaluation of the anti-tumor efficacy of these anti-PD-1 monoclonal antibodies in NOG mice reconstituted with human immune cells demonstrated that sintilimab treatment yielded a superior anti-tumor effect against NCI-H292 tumors when compared to nivolumab and pembrolizumab. This effect correlated with an increased number of CD8 + T cells and tumor-specific effector T cells. These results suggested that the observed higher objective response rate (ORR) and pathologic complete response (pCR) rates in our study could potentially be attributed to these mechanisms. However, it is important to acknowledge that these conclusions should be approached with caution, considering our study’s limited sample size.
In our study, patients received 2–4 cycles sintilimab plus platinum-based chemotherapy, and we performed an evaluation to update the treatment plan after every 2 cycles, which followed the expert consensus [21]. In neoSCORE trial, they found that increasing the number of cycles of neoadjuvant treatment from two to three led to a numerical improvement in MPR with good tolerability [22]. Most participants in our study received 3 cycles of treatment, while a subset underwent 4 cycles of neoadjuvant therapy after comprehensive multidisciplinary treatment (MDT) discussions, primarily driven by the requirement for adequate surgical margins. Furthermore, the consensus also recommended surgery can be performed 4–6 weeks after the last cycle of neoadjuvant immunotherapy, our study was more or less the same as it (only one participant had surgery after 11 weeks due to COVID-19). More importantly, it did encourage that the ORR was 46.15% and pCR rate was 69.23% in our study.
Our study has several limitations. It is a descriptive study conducted at a single institution which only has a few cases, and it may limit the generalizability of results because the majority of participants are male. The existing research fail to provide the relevant data of the overall survival due to the median follow-up time is short. Furthermore, our study is kind of a descriptive one, some selected participants may refuse to receive ICIs as adjuvant therapy, and it is also recommended by some other experts [15]. Meanwhile, some patients did not test for PD-L1 because the amount of samples from the preoperative biopsy is not enough to detect PD-L1, although biomarker-based selection is not essential [21]. But our study presents a promising efficacy of sintilimab plus platinum-based chemotherapy as neoadjuvant chemoimmunotherapy, and the study also makes a contribution to provide more evidence of this kind of treatment for Asian patients. All of these above-mentioned are worthy of further investigation. In future research, we will focus on studying the effects of different combination chemotherapy regimens and PD-L1 expression on patient efficacy.
Conclusion
In conclusion, sintilimab plus platinum-based chemotherapy as neoadjuvant chemoimmunotherapy showed promising efficacy for resectable locally advanced NSCLC and adverse drug effects were acceptable. More cases, longer follow-up time, and more evaluation index are needed to confirm the long-term outcomes of this novel treatment.
Availability of data and materials
Data available on request from the authors.
References
Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Center. 2022;2(1):1–9.
NSCLC Meta-analysis Collaborative Group. Preoperative chemotherapy for non-small-cell lung cancer: a systematic review and meta-analysis of individual participant data. Lancet. 2014;383(9928):1561-1571.
Pless M, Stupp R, Ris HB, Stahel RA, Weder W, Thierstein S, Gerard MA, Xyrafas A, Früh M, Cathomas R, Zippelius A, Roth A, Bijelovic M, Ochsenbein A, Meier UR, Mamot C, Rauch D, Gautschi O, Betticher DC, Mirimanoff RO, Peters S; SAKK Lung Cancer Project Group. Induction chemoradiation in stage IIIA/N2 non-small-cell lung cancer: a phase 3 randomised trial. Lancet. 2015;386(9998):1049–56.
Uprety D, Mandrekar SJ, Wigle D, Roden AC, Adjei AA. Neoadjuvant Immunotherapy for NSCLC: Current Concepts and Future Approaches. J Thorac Oncol. 2020;15(8):1281–97.
Liu J, Blake SJ, Yong MCR, Harjunpää H, Ngiow SF, Takeda K, Young A, O'Donnell JS, Allen S, Smyth MJ, Teng MWL. Improved efficacy of neoadjuvant compared to adjuvant immunotherapy to eradicate metastatic disease. Cancer Discov. 2016;6(12):1382–1399.
National institute of health. National cancer institute Common Terminology Criteria for Adverse Events (CTCAE) version 5.0. NIH Publ. 2017
Blumenthal GM, Bunn PA Jr, Chaft JE, et al. Current status and future perspectives on neoadjuvant therapy in lung cancer. J Thorac Oncol. 2018;13(12):1818–31.
Hellmann MD, Chaft JE, William WN Jr, et al. Pathological response after neoadjuvant chemotherapy in resectable non-small-cell lung cancers: proposal for the use of major pathological response as a surrogate endpoint. Lancet Oncol. 2014;15(1):e42–50.
Jia XH, Xu H, Geng LY, et al. Efficacy and safety of neoadjuvant immunotherapy in resectable nonsmall cell lung cancer: a meta-analysis. Lung Cancer. 2020;147:143–53.
Forde PM, Chaft JE, Smith KN, Anagnostou V, Cottrell TR, Hellmann MD, Zahurak M, Yang SC, Jones DR, Broderick S, Battafarano RJ, Velez MJ, Rekhtman N, Olah Z, Naidoo J, Marrone KA, Verde F, Guo H, Zhang J, Caushi JX, Chan HY, Sidhom JW, Scharpf RB, White J, Gabrielson E, Wang H, Rosner GL, Rusch V, Wolchok JD, Merghoub T, Taube JM, Velculescu VE, Topalian SL, Brahmer JR, Pardoll DM. Neoadjuvant PD-1 Blockade in Resectable Lung Cancer. N Engl J Med. 2018;378(21):1976–86.
Chaft JE, Oezkan F, Kris MG, Bunn PA, Wistuba II, Kwiatkowski DJ, Owen DH, Tang Y, Johnson BE, Lee JM, Lozanski G, Pietrzak M, Seweryn M, Byun WY, Schulze K, Nicholas A, Johnson A, Grindheim J, Hilz S, Shames DS, Rivard C, Toloza E, Haura EB, McNamee CJ, Patterson GA, Waqar SN, Rusch VW, Carbone DP; LCMC study investigators. Neoadjuvant atezolizumab for resectable non-small cell lung cancer: an open-label, single-arm phase II trial. Nat Med. 2022;28(10):2155–2161.
Cascone T, William WN Jr, Weissferdt A, Leung CH, Lin HY, Pataer A, Godoy MCB, Carter BW, Federico L, Reuben A, Khan MAW, Dejima H, Francisco-Cruz A, Parra ER, Solis LM, Fujimoto J, Tran HT, Kalhor N, Fossella FV, Mott FE, Tsao AS, Blumenschein G Jr, Le X, Zhang J, Skoulidis F, Kurie JM, Altan M, Lu C, Glisson BS, Byers LA, Elamin YY, Mehran RJ, Rice DC, Walsh GL, Hofstetter WL, Roth JA, Antonoff MB, Kadara H, Haymaker C, Bernatchez C, Ajami NJ, Jenq RR, Sharma P, Allison JP, Futreal A, Wargo JA, Wistuba II, Swisher SG, Lee JJ, Gibbons DL, Vaporciyan AA, Heymach JV, Sepesi B. Neoadjuvant nivolumab or nivolumab plus ipilimumab in operable non-small cell lung cancer: the phase 2 randomized NEOSTAR trial. Nat Med. 2021;27(3):504–14.
Li N, Ying J, Tao X, et al. P1.18–06 efficacy and safety of neoadjuvant PD-1 blockade with sintilimab in resectable non-small cell lung Cancer, J. Thorac. Oncol. 2019;14(10):S627–S628.
Zhu J, Armstrong AJ, Friedlander TW, Kim W, Pal SK, George DJ, Zhang T. Biomarkers of immunotherapy in urothelial and renal cell carcinoma: PD-L1, tumor mutational burden, and beyond. J Immunother Cancer. 2018;6(1):4.
Upadhaya S, Neftelino ST, Hodge JP, Oliva C, Campbell JR, Yu JX. Combinations take centre stage in PD1/PDL1 inhibitor clinical trials. Nat Rev Drug Discov. 2021;20(3):168–9. https://doi.org/10.1038/d41573-020-00204-y.
Provencio M, Nadal E, Insa A, et al. Neoadjuvant chemotherapy and nivolumab in resectable non-small-cell lung cancer (NADIM): an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020;21(11):1413–1422.
Forde PM, Spicer J, Lu S, Provencio M, Mitsudomi T, Awad MM, Felip E, Broderick S, Brahmer J, Swanson SJ, Kerr K, Wang C, Saylors GB, Tanaka F, Ito H, Chen K-N, Dorange C, Cai J, Fiore J, Girard N. Abstract CT003: Nivolumab (NIVO) + platinum-doublet chemotherapy (chemo) vs chemo as neoadjuvant treatment (tx) for resectable (IB-IIIA) non-small cell lung cancer (NSCLC) in the phase 3 CheckMate 816 trial. Cancer Res. 2021;81(13_Supplement): CT003.
Shu CA, Gainor JF, Awad MM, Chiuzan C, Grigg CM, Pabani A, Garofano RF, Stoopler MB, Cheng SK, White A, Lanuti M, D’Ovidio F, Bacchetta M, Sonett JR, Saqi A, Rizvi NA. Neoadjuvant atezolizumab and chemotherapy in patients with resectable non-small-cell lung cancer: an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020;21(6):786–95.
Rothschild SI, Zippelius A, Eboulet EI, Savic Prince S, Betticher D, Bettini A, Früh M, Joerger M, Lardinois D, Gelpke H, Mauti LA, Britschgi C, Weder W, Peters S, Mark M, Cathomas R, Ochsenbein AF, Janthur WD, Waibel C, Mach N, Froesch P, Buess M, Bohanes P, Godar G, Rusterholz C, Gonzalez M, Pless M; Swiss Group for Clinical Cancer Research (SAKK). SAKK 16/14: Durvalumab in Addition to Neoadjuvant Chemotherapy in Patients With Stage IIIA(N2) Non-small-cell lung cancer-a multicenter single-arm phase II trial. J Clin Oncol. 2021;39(26):2872–2880.
Wang J, Fei K, Jing H, Wu Z, Wu W, Zhou S, Ni H, Chen B, Xiong Y, Liu Y, Peng B, Yu D, Jiang H, Liu J. Durable blockade of PD-1 signaling links preclinical efficacy of sintilimab to its clinical benefit. MAbs. 2019;11(8):1443–51.
Liang W, Cai K, Chen C, et al. Expert consensus on neoadjuvant immunotherapy for non-small cell lung cancer. Transl Lung Cancer Res. 2020;9(6):2696–715.
Shao M, Yao J, Wang Y, Zhao L, Li B, Li L, Wu Z, Chen Z, Fan J, Qiu F. Two vs three cycles of neoadjuvant sintilimab plus chemotherapy for resectable non-small-cell lung cancer: neoSCORE trial. Signal Transduct Target Ther. 2023;8(1):146.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Cunli Yin and Bin Hu wrote the main manuscript text. Cunli Yin and Jun Ge processed the data. Xi Yang and Lingna Kou prepared the ethical approval. Bo Tian and Chenghao Wang prepared all figures. Siru Li and Bin Liu made all tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study followed the Declaration of Helsinki and ethical approval was obtained from the Research Ethics Committee of Sichuan Cancer Hospital.
Consent for publication
Written informed consent was obtained from the patients for their anonymized information to be published in this article.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yin, C., Hu, B., Yang, X. et al. Neoadjuvant sintilimab combined with chemotherapy in resectable locally advanced non-small cell lung cancer: case series and literature review. World J Surg Onc 21, 304 (2023). https://doi.org/10.1186/s12957-023-03194-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03194-4