Abstract
Background
The epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) is still under investigation as adjuvant treatment for early-stage disease. Here, we performed a meta-analysis to evaluate the efficacy of adjuvant EGFR-TKI versus non-EGFR-TKI treatment in patients with completely resected non-small cell lung cancer (NSCLC) harboring EGFR mutation.
Methods
Two investigators independently extracted data from databases. A meta-analysis was performed following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The protocol was registered in PROSPERO (ID: CRD42022316481). The primary outcome was disease-free survival (DFS) in patients with EGFR mutation, measured as the hazard ratio (HR). Other outcomes (of subgroup analyses) included overall survival (OS) and DFS.
Results
After the systematic screening, eight studies with a total of 3098 patients with stage IB–IIIA NSCLC were included. The results show that in patients with EGFR mutation, the DFS in the adjuvant EGFR-TKI group was significantly superior to that in the control group, with a HR of 0.47 (95% confidence interval [CI]: 0.30–0.74; P = 0.001). In subgroup analyses of DFS, the benefit was observed in the EGFR-TKI group versus the chemotherapy group (HR 0.50, 95% CI 0.30–0.84; P = 0.009), the EGFR-TKI combined with chemotherapy group versus the chemotherapy group (HR 0.37, 95% CI 0.16–0.85; P = 0.02), and in stage IIA–IIIA NSCLC (HR 0.45, 95% CI 0.27–0.74; P = 0.002). However, the benefit of DFS did not translate into improved OS in the whole population (HR 0.79, 95% CI 0.54–1.14; P = 0.20).
Conclusion
EGFR-TKIs prolonged DFS but not OS in patients with completely resected stage II–IIIA NSCLC harboring EGFR mutation. Longer follow-ups and new clinical trials that can result in changes in clinical practice are needed.
Similar content being viewed by others
Introduction
Lung cancer is a leading cause of cancer-related deaths worldwide. Only 20–25% of patients with non-small cell lung cancer (NSCLC) receive surgery [1]. Postoperative cisplatin-based adjuvant chemotherapy is recommended for patients with completely resected stage II–IIIA disease [2]. Pooled analysis by the Lung Adjuvant Cisplatin Evaluation (LACE) Collaborative Group showed that cisplatin-based adjuvant chemotherapy significantly improved survival in patients with NSCLC, but at 5 years the absolute benefit was only about 5% [3]. Compared with chemotherapy alone, the addition of bevacizumab to adjuvant chemotherapy has failed to improve overall survival (OS) or disease-free survival (DFS) in patients with stage IB–IIIA disease [4]. Thus, the efficacy of adjuvant chemotherapy is not satisfactory.
EGFR mutations were identified in 40–60% of lung adenocarcinomas in East Asians, and exon19 and exon 21 accounted for 87% [5, 6]. Epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs) have revolutionized the treatment of advanced NSCLC, leading to the investigation of adjuvant EGFR-TKI treatment for early-stage disease. The BR19 study demonstrated that gefitinib as an adjuvant treatment did not improve OS or progression-free survival compared with a placebo [7]. The RADIANT study failed to show that erlotinib as an adjuvant treatment prolonged DFS in EGFR-expressing NSCLC patients, but a benefit trend was observed in an EGFR-mutant subgroup [8]. The single-arm SELECT study demonstrated that adjuvant erlotinib improved the 2-year DFS rate (88%) in stage IA–IIIA patients with EGFR mutation compared to that of historic genotype-matched controls 76% [9].
The ADJUVANT and EVAN studies confirmed that in stage II–IIIA patients with EGFR mutation, adjuvant gefitinib or erlotinib significantly prolonged DFS compared with chemotherapy [10, 11]. However, the WJOG6410L study showed that adjuvant gefitinib did not significantly prolong DFS or OS in patients with completely resected stage II–III EGFR-mutated NSCLC [12]. In 2020, the ADAURA study showed the overwhelming efficacy of osimertinib for adjuvant treatment of patients with stage IB–IIIA NSCLC harboring EGFR mutation [13]. More recently, the EVIDENCE study showed encouraging results of adjuvant icotinib treatment of EGFR-mutant patients [14].
Several meta-analyses have been performed to assess the role of adjuvant EGFR-TKIs in resected patients [15, 16]; however, those studies did not include the ADAURA, WJOG6410L, or EVIDENCE studies. Moreover, the ADJUVANT and EVAN studies recently updated their OS data [17, 18]. Thus, we performed a meta-analysis of randomized controlled trials to evaluate the efficacy of EGFR-TKIs as adjuvant treatment for completely resected NSCLC.
Methods
Search strategy
We carried out this meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The protocol was registered in PROSPERO (ID: CRD42022316481).
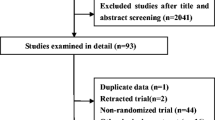
Two experienced investigators (Zhao and Wu) independently conducted a literature search and screening. They systematically searched the PubMed, EMBASE, Chinese Biomedical Literature Database, and Cochrane Library databases as the primary literature sources. The following conferences in the last 3 years were also searched manually: the European Society for Medical Oncology, the American Society of Clinical Oncology (ASCO), and the World Conference on Lung Cancer. The publishing deadline was July 1, 2021. Search keywords included non-small cell lung cancer, NSCLC, osimertinib, icotinib, gefitinib, erlotinib, afatinib, dacomitinib, and EGFR-TKI. The reference lists of studies and previous meta-analyses were also further investigated. Figure 1 presents the screening process.
Eligibility criteria
The inclusion criteria were (1) phase II or III prospective randomized controlled clinical studies, (2) patients with histologically confirmed stage IB–IIIA NSCLC who had completed resection, and (3) patients who received EGFR-TKIs as adjuvant therapy. The exclusion criteria were (1) retrospective or non-randomized controlled clinical studies; (2) studies on the use of EGFR-TKIs as the first-line treatment for advanced lung cancer or the inclusion of immunotherapy in adjuvant therapy; (3) studies on wild-type EGFR (for EGFR-unselected patients, EGFR mutation data should be available); (4) case reports, reviews, and studies not written in English; and (5) articles with low quality or with small sample sizes (< 10 cases).
Data extraction and quality assessment
The following data were extracted from included studies: authors, publication year, number of patients, patient characteristics, stage, EGFR status, treatments, DFS, OS, hazard ratio (HR), and 95% confidence interval (95% CI). The characteristics and outcomes of the included trials as well as the data extracted from the trials were entered into RevMan version 5.3 (Cochrane Collaboration, Oxford, UK). Two experienced investigators (Zhao and Wu) evaluated the quality of the studies independently using the Cochrane Risk of Bias tool. Sequence generation, allocation concealment, blinding, incomplete data, selective reporting, and other bias sources were assessed. Items were scored as having a low, high, or unclear risk of bias. Any discrepancies were determined by a third researcher (Yang).
Statistical analyses
Statistical analyses were performed in Review Manager (Revman) Version 5.3. HRs were calculated for DFS and OS using the inverse variance method. P < 0.05 was considered statistically significant. All P values and 95% CIs were two-sided. Heterogeneity was assessed using the chi-squared test. If significant heterogeneity was high (P ≤ 0.05 or I2 > 50%), a random-effects model was used to reduce the impact of heterogeneity on the results; otherwise, a fixed-effect model was used. HRs were calculated as an effect measure for OS and DFS using the inverse variance method. Publication bias was tested using a funnel plot.
Endpoints
The primary endpoint was DFS in EGFR-mutant patients, and other endpoints included DFS in subgroup analysis and OS.
Results
Eligible studies
Eight studies with a total of 3098 patients were included [7, 8, 10,11,12,13,14, 19]. Among these studies, six were phase III clinical trials and two were phase II clinical trials. Another study was excluded because it was of low quality, and the HRs were not available [20]. The characteristics of the studies included in the meta-analysis are shown in Table 1. We evaluated the quality of the studies using the Cochrane Risk of Bias tool, as shown in Fig. 2.
DFS
Data on median DFS and HRs were available in all eight trials. As shown in Fig. 3, in EGFR-mutant patients, the DFS of the adjuvant EGFR-TKI group was significantly superior to that of the control group, with a HR of 0.47 (95% CI 0.30–0.74; P = 0.001). Compared with chemotherapy, DFS was significantly improved in the EGFR-TKI subgroup (HR 0.50, 95% CI 0.30–0.84; P = 0.009), whereas DFS did not differ significantly between the placebo and EGFR-TKI subgroups (HR 0.68, 95% CI 0.21–2.17; P = 0.51). Only one study compared EGFR-TKI combined with chemotherapy to chemotherapy alone, showing significant improvement in DFS with a HR of 0.37 (95% CI 0.16–0.85; P = 0.02).
Subgroup analysis of DFS
We performed a subgroup analysis of DFS. As shown in the forest plot (Fig. 4), in patients with stage IIA–IIIA NSCLC, DFS was significantly prolonged in the EGFR-TKI group compared with the control group (HR 0.45, 95% CI 0.27–0.74; P = 0.002). However, in stage IB patients, the difference in DFS between the EGFR-TKI and control groups was not significant (HR 0.66, 95% CI 0.27–1.61; P = 0.36). Seven studies used the first-generation EGFR-TKIs; the overall HR for DFS in this subgroup was 0.54 (95% CI 0.37–0.79; P = 0.001). Only the ADAURA study used the third-generation EGFR-TKI osimertinib, with a superior HR of 0.20 (95% CI 0.14–0.30; P < 0.001).
OS
The forest plot of OS implied that the difference between the adjuvant EGFR-TKI group and the control group was not statistically significant (HR 0.79, 95% CI 0.54–1.14, P = 0.20). No significant differences were found among all subgroups. In the subgroup of EGFR-TKI compared with chemotherapy, the HR was 0.77 (95% CI 0.49–1.20, P = 0.25). In the EGFR-TKI versus placebo subgroup, the overall HR was 1.07 (95% CI 0.44–2.63; P = 0.88) (Fig. 5).
Discussion
In this study, we performed a meta-analysis to assess the efficacy of EGFR-TKIs as adjuvant treatment for completely resected NSCLC. The results reached the first endpoint. The DFS of the adjuvant EGFR-TKI group was significantly superior to that of the control group in EGFR-mutant patients, with a HR of 0.47 (P = 0.001), showing that adjuvant EGFR-TKIs decreased the risk of disease recurrence or death by 53% compared with the non-EGFR-TKI group. However, the benefit did not result in a significant improvement in OS (HR 0.79, P = 0.20), possibly due to the crossover effect of subsequent therapies. Moreover, the OS data of ADAURA and EVIDENCE were immature.
In patients with advanced NSCLC, the first-generation EGFR-TKIs have been shown to be superior to chemotherapy with respect to progression-free survival in untreated patients [21,22,23]. Adjuvant EGFR-TKI treatment is still being explored for the treatment of early-stage NSCLC, but it has been a challenging process. Initial studies, including BR19 and RADIANT, produced negative results because the patients enrolled in these two studies were unselected. Patients with wild-type EGFR did not benefit from EGFR-TKIs compared with chemotherapy [24]; thus, EGFR mutation status should be detected before the use of EGFR-TKIs. It is not recommended that patients with unknown EGFR mutation status use EGFR-TKIs in the adjuvant treatment setting.
Several questions remain about adjuvant EGFR-TKI treatment. First, it is unclear whether EGFR-TKIs should be used in stage IB EGFR-mutant patients after complete resection. In the ADJUVANT, EVAN, and EVIDENCE studies, all enrolled patients had stage II–IIIA disease with EGFR mutation, and the results showed improved DFS with EGFR-TKIs compared to chemotherapy. Only the WJOG6410L study showed that adjuvant gefitinib did not significantly prolong DFS or OS in patients with stage II–III NSCLC with EGFR mutation [12]. In this meta-analysis, the overall DFS of stage IIA–IIIA NSCLC was significantly prolonged in the EGFR-TKI group, with a HR of 0.45 (P = 0.002), showing that the risk of disease recurrence or death decreased by 55% in the adjuvant EGFR-TKI group compared with the non-EGFR-TKI-treated group. Two studies (ADAURA, RADIANT) enrolled stage IB patients with available data, and their overall DFS was not significantly different (HR 0.66; P = 0.36). Only the ADAURA study found that EGFR-mutant patients with stage IB could also benefit from osimertinib, with a HR of 0.39 (95% CI 0.18–0.76), though the degree of benefit was smaller than that in stage II (HR 0.17; 95% CI 0.08–0.31) and stage IIIA (HR 0.12; 95% CI 0.07–0.20). Therefore, EGFR-mutant patients with stage II–IIIA disease, especially those with lymph node metastases, can benefit from adjuvant EGFR-TKI treatment after resection. Stage IB patients may benefit from third-generation TKIs rather than first-generation TKIs.
Second, it is unknown whether first-generation or third-generation TKIs should be used as adjuvant treatment in EGFR-mutant patients post-surgery. The efficacy of the third-generation EGFR-TKI osimertinib has been shown to be superior to that of first-generation TKIs for the first-line treatment of EGFR-mutant advanced NSCLC [25, 26]. In this meta-analysis, six studies used first-generation EGFR-TKIs and only one study used the third-generation EGFR-TKIs; however, the HR for DFS in the third-generation subgroup was superior, providing the best HR to date (HR 0.20; P < 0.001). Moreover, adjuvant osimertinib reduces the risk of central nervous system recurrence by 82% in patients with resected EGFR-mutant NSCLC [13]. The overwhelming efficacy of osimertinib has made it the priority adjuvant treatment for EGFR-mutant patients. However, subsequent treatment should be considered if third-generation TKIs are used in the adjuvant setting; the final OS results of the ADAURA study will be relevant and should elucidate this issue.
Third, what role of adjuvant chemotherapy play in EGFR-mutant patients after complete resection? Chemotherapy improves survival rates by about 5% in patients with NSCLC, and adjuvant chemotherapy is the standard treatment in patients with completely resected stage II–IIIA disease [27]. In patients harboring EGFR mutation, three head-to-head studies (including ADJUVANT, EVAN, and EVIDENCE) demonstrated that EGFR-TKIs were superior to chemotherapy as adjuvant therapy. However, the WJOG6410L study presented at the 2021 ASCO meeting found that adjuvant gefitinib did not significantly prolong DFS or OS compared with chemotherapy. In this meta-analysis, the overall HR for EGFR-TKIs compared with chemotherapy was 0.50 (P = 0.009), while in the EGFR-TKI combined with chemotherapy versus the chemotherapy-alone subgroup, the difference in DFS was not significant (HR 0.38; P = 0.11). In the ADAURA study, the majority of patients with stage II–IIIA disease and approximately one-quarter of stage IB patients received adjuvant chemotherapy. The HRs for DFS were 0.16 (0.10–0.26) and 0.23 (0.13–0.40) in patients who did and did not receive adjuvant chemotherapy, respectively. The subsequent analysis of the ADAURA study showed adjuvant osimertinib as an effective treatment for patients with stage IB–IIIA EGFR mutation NSCLC after resection, with or without prior adjuvant chemotherapy [28]. Adjuvant chemotherapy appeared to have a limited effect on EGFR-mutant patients after resection. In a multicenter retrospective study, researchers found adjuvant EGFT-TKIs might be a beneficial choice compared with EGFR-TKIs plus chemotherapy in EGFR-mutant stage III-pN2 lung adenocarcinoma [29]. These results do not indicate that adjuvant chemotherapy should be abandoned. To date, adjuvant chemotherapy is one of the only treatments that has shown an OS benefit in resected NSCLC. Therefore, further prospective studies designed to understand the role of adjuvant chemotherapy in EGFR-mutant NSCLC patients are needed.
Fourth, the optimal exposure duration of adjuvant EGFR-TKI treatment is uncertain. For advanced patients, EGFR-TKIs are recommended until disease progression, but in the adjuvant setting, the situation is somewhat different. Patients can have long tumor-free survival after complete resection. Currently, most clinical trials are designed with 2 years of adjuvant drug treatment, but these studies have been empirical without definitive evidence. However, Lyu et al. found that 2 years of treatment with icotinib resulted in a significantly lower risk of recurrence compared to 1 year of treatment in EGFR-mutant patients with stage II–IIIA NSCLC after R0 resection [30]. The 3-year treatment duration in the ADAURA study led to great benefits. Whether a longer treatment duration might lead to improved survival remains unknown. A head-to-head clinical trial is needed for further analysis.
Finally, the benefit of DFS did not translate into improved OS, possibly due to the crossover effect of subsequent therapies. After disease recurrence, patients may receive many lines of treatment, which may contribute to improved OS. In the final OS analysis of the ADJUVANT study, the median OS times were 75.5 months and 62.8 months with gefitinib and chemotherapy, respectively (HR 0.92, P = 0 0.674) [17]. At the 2021 ASCO meeting, the OS of the EVAN study was updated; the median OS was 84.2 months with adjuvant erlotinib versus 61.1 months with adjuvant chemotherapy (HR 0.318; 95% CI 0.151–0.670) [18]. This was the first randomized study of adjuvant EGFR-TKI treatment to demonstrate a clinically meaningful improvement in OS versus chemotherapy alone in patients with stage IIIA EGFR-mutant NSCLC.
This meta-analysis had several limitations. First, the meta-analysis was not based on individual data, and some data were from subgroup analyses; moreover, the OS data of several studies were immature, which may have led to bias. Second, some studies compared EGFR-TKI treatment to chemotherapy while others compared it to a placebo, which made them not completely comparable. In addition, due to the limitations of the included studies, the optimal adjuvant treatment for patients with resected NSCLC harboring EGFR mutation is still unclear. The treatment model used in the ADAURA study was accepted by doctors, but longer follow-ups are needed. And new clinical trials that can result in changes in clinical practice merit further exploration.
In conclusion, EGFR-TKIs prolonged DFS but not OS in completely resected stage II–IIIA NSCLC patients harboring EGFR mutation. Longer follow-ups and new clinical trials that can result in changes in clinical practice are needed.
Availability of data and materials
Not applicable.
References
Arriagada R, Auperin A, Burdett S, et al. Adjuvant chemotherapy, with or without postoperative radiotherapy, in operable non-small-cell lung cancer: two meta-analyses of individual patient data. Lancet. 2010;375(9722):1267–77.
Ettinger DS, Wood DE, Aggarwal C, et al. NCCN guidelines insights: non-small cell lung cancer, Version 1.2020. J Natl Compr Canc Netw. 2019;17(12):1464–72.
Burdett S, Pignon JP, Tierney J, et al. Adjuvant chemotherapy for resected early-stage non-small cell lung cancer. Cochrane Database Syst Rev. 2015;3:D11430.
Wakelee HA, Dahlberg SE, Keller SM, et al. Adjuvant chemotherapy with or without bevacizumab in patients with resected non-small-cell lung cancer (E1505): an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2017;18(12):1610–23.
Zhang X, Jiang Y, Yu H, et al. A comprehensive study on the oncogenic mutation and molecular pathology in Chinese lung adenocarcinoma patients. World J Surg Oncol. 2020;18(1):172.
Li S, Li X. Analysis of EGFR, KRAS, and PIK3CA gene mutation rates and clinical distribution in patients with different types of lung cancer. World J Surg Oncol. 2021;19(1):197.
Goss GD, O’Callaghan C, Lorimer I, et al. Gefitinib versus placebo in completely resected non-small-cell lung cancer: results of the NCIC CTG BR19 study. J Clin Oncol. 2013;31(27):3320–6.
Kelly K, Altorki NK, Eberhardt WE, et al. Adjuvant erlotinib versus placebo in patients with stage IB-IIIA non-small-cell lung cancer (RADIANT): a randomized, double-blind, phase III trial. J Clin Oncol. 2015;33(34):4007–14.
Pennell NA, Neal JW, Chaft JE, et al. SELECT: a phase II trial of adjuvant erlotinib in patients with resected epidermal growth factor receptor-mutant non-small-cell lung cancer. J Clin Oncol. 2019;37(2):97–104.
Zhong WZ, Wang Q, Mao WM, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II-IIIA (N1–N2) EGFR-mutant NSCLC (ADJUVANT/CTONG1104): a randomised, open-label, phase 3 study. Lancet Oncol. 2018;19(1):139–48.
Yue D, Xu S, Wang Q, et al. Erlotinib versus vinorelbine plus cisplatin as adjuvant therapy in Chinese patients with stage IIIA EGFR mutation-positive non-small-cell lung cancer (EVAN): a randomised, open-label, phase 2 trial. Lancet Respir Med. 2018;6(11):863–73.
Tada H, Mitsudomi T, Misumi T, et al. Randomized phase III study of gefitinib versus cisplatin plus vinorelbine for patients with resected stage II-IIIA non-small-cell lung cancer with EGFR mutation (IMPACT). J Clin Oncol. 2022;40(3):231-41.
Wu YL, Tsuboi M, He J, et al. Osimertinib in resected EGFR-mutated non–small-cell lung cancer. N Engl J Med. 2020;383(18):1711–23.
He J, Su C, Liang W, et al. Icotinib versus chemotherapy as adjuvant treatment for stage II-IIIA EGFR-mutant non-small-cell lung cancer (EVIDENCE): a randomised, open-label, phase 3 trial. Lancet Respir Med. 2021;9(9):1021-9.
Cheng H, Li XJ, Wang XJ, et al. A meta-analysis of adjuvant EGFR-TKIs for patients with resected non-small cell lung cancer. Lung Cancer. 2019;137:7–13.
Tang W, Li X, Xie X, et al. EGFR inhibitors as adjuvant therapy for resected non-small cell lung cancer harboring EGFR mutations. Lung Cancer. 2019;136:6–14.
Zhong W Z, Wang Q, Mao W M, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II-IIIA (N1-N2) EGFR-mutant NSCLC: final overall survival analysis of CTONG1104 phase III trial. J Clin Oncol. 2021;39(7):713-22.
Yue DS, Xu SD, Wang Q. Updated overall survival (OS) and exploratory analysis from the randomized, phase II EVAN study of erlotinib (E) versus vinorelbine plus cisplatin (NP) as adjuvant therapy in Chinese patients with stage IIIA EGFR+ NSCLC. J Clin Oncol. 2021;39(suppl 15; abstr 8520):2021.
Li N, Ou W, Ye X, et al. Pemetrexed-carboplatin adjuvant chemotherapy with or without gefitinib in resected stage IIIA-N2 non-small cell lung cancer harbouring EGFR mutations: a randomized, phase II study. Ann Surg Oncol. 2014;21(6):2091–6.
Feng SY, Wang YY, Cai KC, et al. Randomized adjuvant chemotherapy of EGFR-mutated non-small cell lung cancer patients with or without icotinib consolidation therapy. PLoS One. 2015;10(10):e140794.
Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57.
Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–46.
Shi YK, Wang L, Han BH, et al. First-line icotinib versus cisplatin/pemetrexed plus pemetrexed maintenance therapy for patients with advanced EGFR mutation-positive lung adenocarcinoma (CONVINCE): a phase 3, open-label, randomized study. Ann Oncol. 2017;28(10):2443–50.
Zhou Q, Cheng Y, Yang JJ, et al. Pemetrexed versus gefitinib as a second-line treatment in advanced non-squamous non-small-cell lung cancer patients harbouring wild-type EGFR (CTONG0806): a multicenter randomized trial. Ann Oncol. 2014;25(12):2385-91.
Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25.
Ramalingam SS, Vansteenkiste J, Planchard D, et al. Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N Engl J Med. 2020;382(1):41–50.
Takashima S, Imai K, Atari M, et al. Clinical benefits of adjuvant chemotherapy with carboplatin and gemcitabine in patients with non-small cell lung cancer: a single-center retrospective study. World J Surg Oncol. 2020;18(1):263.
Wu YL, John T, Grohe C, et al. Postoperative chemotherapy use and outcomes from ADAURA: osimertinib as adjuvant therapy for resected EGFR-mutated NSCLC. J Thorac Oncol. 2022;17(3):423–33.
Li Q, Ma L, Qiu B, et al. Benefit from adjuvant TKIs versus TKIs plus chemotherapy in EGFR-mutant stage III-pN2 lung adenocarcinoma. Curr Oncol. 2021;28(2):1424–36.
Lyu C, Wang R, Li SL. Different exposure duration of adjuvant icotinib in stage II-IIIA non-small cell lung cancer patients with positive EGFR mutation (ICOMPARE study): a randomized, open-label phase 2 study. J Clin Oncol. 2021;39(suppl 15; abstr 8521):2021.
Acknowledgements
Not applicable.
Funding
This work was supported by the medical research project of Foshan Health Bureau, No. 20220336.
Author information
Authors and Affiliations
Contributions
Ning Zhao and Zhuo-peng Wu contributed equally to this work, contributed to all aspects of this study, and were major contributors to the writing of this manuscript. Jie Yang and Wei-quan Gu contributed to the study conception and design, and critical revision of the article. Wei-neng Feng and Sheng-li Yang contributed to the data collection and extraction. The other authors contributed to the quality assessment of the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Search Strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, N., Wu, Zp., Yang, J. et al. Epidermal growth factor receptor inhibitors as adjuvant treatment for patients with resected non-small cell lung cancer harboring EGFR mutation: a meta-analysis of randomized controlled clinical trials. World J Surg Onc 21, 45 (2023). https://doi.org/10.1186/s12957-023-02925-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-02925-x