Abstract
Introduction
Contralateral axillary lymph node metastasis (CALNM) in breast cancer (BC) is considered a distant metastasis, marking stage 4cancer. Therefore, it is generally treated as an incurable disease. However, in clinical practice, staging and treatment remain controversial due to a paucity of data, and the St. Gallen 2021 consensus panel recommended a curative approach in patients with oligometastatic disease. Aberrant lymph node (LN) drainage following previous surgery or radiotherapy is common. Therefore, CALNM may be considered a regional event rather than systemic disease, and a re-sentinel procedure aided by lymphoscintigraphy permits adequate regional staging.
Case report
Here, we report a 37-year-old patient with Lynch syndrome who presented with CALNM in an ipsilateral relapse of a moderately differentiated invasive ductal BC (ER 90%, PR 30%, HER2 negative, Ki-67 25%, microsatellite stable), 3 years after the initial diagnosis. Lymphoscintigraphy detected a positive sentinel LN in the contralateral axilla despite no sign of LN involvement or distant metastases on FDG PET/CT or MRI. The patient underwent bilateral mastectomy with sentinel node dissection, surgical reconstruction with histological confirmation of the CALNM, left axillary dissection, adjuvant chemotherapy, and anti-hormone therapy. In addition to her regular BC follow-up visits, the patient will undergo annual colonoscopy, gastroscopy, abdominal, and vaginal ultrasound screening. In January 2023, the patient was free of progression for 23 months after initiation of treatment for recurrent BC and CALNM.
Conclusion
This case highlights the value of delayed lymphoscintigraphy and the contribution of sentinel procedure for local control in the setting of recurrent BC. Aberrant lymph node drainage following previous surgery may be the underlying cause of CALNM. We propose that CALNM without evidence of systemic metastasis should be considered a regional event in recurrent BC, and thus, a curative approach can be pursued. The next AJCC BC staging should clarify the role of CALNM in recurrent BC to allow for the development of specific treatment guidelines.
Similar content being viewed by others
Introduction
Contralateral axillary lymph node metastasis (CALNM) in breast cancer (BC) is a condition with a rare incidence of 1.9–6% [1,2,3,4,5]. CALNM can occur as a metastasis of the primary BC or a different extramammary primary cancer or with an occult ipsilateral BC as an origin [6,7,8]. Metastasis of the primary BC is the most common cause. It can be detected upon the first diagnosis of the primary BC or at relapse of the BC. Regardless of the origin of CALNM, any metastases of BC to the contralateral axillary lymph nodes are considered to be a distant metastasis, marking stage 4 of cancer, according to the American Joint Committee on Cancer (AJCC) staging system [9]. Considering CALNM as a metastatic disease has profound implications on locoregional management. In clinical practice, staging and treatment of CALNM remain controversial due to lack of evidence especially in the recurrent setting after surgery.
Aberrant lymph node drainage following previous surgery or radiotherapy is commonly described with 18–70% in the literature [10,11,12]. Therefore, CALNM may be considered a regional event rather than systemic disease, and a re-sentinel procedure aided by lymphoscintigraphy permits adequate regional staging [5, 10, 13,14,15,16]. Here, we present a premenopausal Lynch syndrome patient with ipsilateral relapse of invasive ductal BC and CALNM detected by a re-sentinel procedure and subsequent treatment with curative intent.
Results
Patient presentation
In April 2017, a 34-year-old premenopausal primipara woman underwent oncoplastic resection with sentinel biopsy on the right side with diagnosis of a poorly differentiated invasive ductal BC. The lesion was staged as pT1c (15 mm), pN1mi (1/2) (sentinel node (sn)), Bloom–Richardson–Elston (BRE) grade 3, R0, estrogen receptor (ER) 90%, progesterone receptor (PR) 60%, human epidermal growth receptor 2 (HER2) negative, and Ki-67 15%. The initiated oncotype DX showed a score of 18. The patient received adjuvant radiotherapy to the right breast and axilla (50.4 Gray (Gy)), paraclavicular (45 Gy), and a local boost dose of (6 × 2 Gy). Concomitantly, antihormonal therapy with tamoxifen was initiated; however, due to adverse effects (menopause-like symptoms, weight gain, and exacerbation of her depression), treatment was discontinued by the patient after 2 months without further antihormonal treatments.
Genetic counseling and testing showed a familial predisposition towards endometrial, liver, kidney, and lung cancer. A verified Lynch syndrome mutation was identified in the patient’s mother in 2015 and was subsequently confirmed in the patient with diagnosis of the poorly differentiated invasive ductal BC; it is a heterozygous mutation of the mismatch repair gene MSH6: c.2690dupA/p.Asn897LysfsTer3. As a result, the patient opted for a preventive hysterectomy and salpingectomy after completing family planning.
The patient’s medical history included three deep vein thromboses secondary to a hereditary antithrombin deficiency type 1. Her medical history also included a vaginal birth in 2005, newly diagnosed depression and hyperthyroidism in 2020, and 20-pack-year smoking history. Her current medications included Eliquis (5 mg PO, twice a day), escitalopram (20 mg PO once a day), and Tirosint (25 μg PO once a day).
The follow-up mammogram in December 2020, 3 years after the initial diagnosis, revealed increased parenchymal density and progressive micro-calcifications in the right breast compared to the regular previous imaging. These findings were suspicious for an ipsilateral relapse of invasive ductal BC (Fig. 1).
Mammogram and magnetic resonance imaging (MRI) showing ipsilateral breast cancer relapse before neoadjuvant antihormone therapy. a Mammogram of the right breast in a mediolateral oblique view with suspicion of a relapse BIRADS 4, ACRb. It shows increased parenchymal density of the upper right quadrant compared to the previous follow-ups, progressive microcalcifications medial to the clips (arrow), and progressive mamilla retraction. b T1-weighted transverse axial dynamic contrast-enhanced MRI with fat suppression showing asymmetric accumulation of contrast and restricted diffusion of the whole right breast including the mammilla. There is subcutaneous edema of the right breast, but no sign of lymph node metastases or distant metastases
The biopsy confirmed a relapse with infiltrates of a moderately differentiated invasive ductal BC (ER 90%, PR 30%, HER2 negative, Ki-67 25%, microsatellite stable). The patient was started preoperatively on an endocrine therapy with the nonsteroidal aromatase inhibitor (AI) letrozole (2.5 mg PO QD) along with the gonadotropin-releasing hormone agonist goserelin (3.6 mg SQ QM) for ovarian function suppression (OFS).
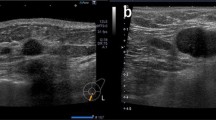
Preoperative evaluation with fluorodeoxyglucose positron emission tomography with computed tomography (FDG PET/CT) and magnetic resonance imaging (MRI) confirmed relapse of the right breast, with no sign of lymph node involvement or distant metastases. However, delayed lymphoscintigraphy (2 h after injection) detected a sentinel lymph node in the contralateral axilla (Fig. 2).
Contralateral lymph node metastasis in recurrent ipsilateral breast cancer. a Planar sentinel node scintigraphy 15 min after periareolar injection of 70 MBq 99mTechnetium-labelled nanocolloid (NanoHSA-ROTOP®), with detection of the sentinel node (pink arrow) in the left axilla (PB = injection site covered with lead). b Maximum intensity projection of the FDG PET/CT scan, demonstrating diffuse multifocal hypermetabolism of the recurrent mamma carcinoma on the right, without lymph node metastases or distant metastases. c Intraoperative left axilla with detection of two patent blue V and technetium-positive lymph nodes
Surgical and medical management
The management options were discussed at the interdisciplinary tumor board and with the patient, and it was decided to pursue a curative approach with re-sentinel procedure.
The patient underwent bilateral mastectomy with sentinel lymph node dissection and surgical reconstruction. In detail, the procedure included the following: (a) skin-sparing mastectomy with thoracodorsal artery perforator flap and implant reconstruction on the right, (b) nipple-sparing mastectomy with implant insertion on the left, and (c) sentinel lymph node dissection bilaterally. During the sentinel node dissection, three technetium and patent blue lymph nodes were identified in the contralateral axilla and removed (Fig. 2).
Histopathological analysis confirmed the presence of an ipsilateral invasive ductal tumor and contralateral lymph node metastases. The patient was staged as rpT3 (96mm), rpN1a (2/3, contralateral) (0/4, ipsilateral), G2, V0, L1, Pn1, R0 (local), ER 90%, PR 30%, HER2 negative, and Ki-67 5%. The following axillary dissection on the left after 4 weeks resulted in no additional positive lymph nodes rpN1a (2/18).
Four days later, the patient returned to the hospital with a ruptured ovarian cyst and ovarian torsion on the right. She underwent right adnexectomy and was discharged on postoperative day 2.
The OFS with goserelin was continued, and adjuvant chemotherapy with 6 cycles of Taxotere and cyclophosphamide (TC) was initiated. After three cycles of TC, she developed methicillin-resistant Staphylococcus aureus cellulitis of the right arm secondary to chemotherapy-induced neutropenia. The cellulitis was treated with incision and drainage, followed by 14 days of IV daptomycin and piperacillin/tazobactam. Thereafter, the remaining 3 cycles of TC were well tolerated without adverse effects.
After completing chemotherapy, endocrine therapy with AI was resumed. Additionally, the patient received the bisphosphonate zoledronic acid (4 mg IV q6month) and underwent regular bone density measurements. In addition to her regular BC follow-up visits, the patient will undergo annual colonoscopy, gastroscopy, abdominal ultrasound screening, and vaginal ultrasound screening. As of August 2022, the patient has been free of progression for 23 months after initiation of treatment for recurrent BC with CALNM until now.
Literature review
In the literature, 49 histologically confirmed CALNM with ipsilateral BC recurrence have been described (Table 1). The literature consists of 7 case reports, 4 small retrospective series, and 5 prospective repeat sentinel biopsy (SNB) studies. Thirty-five of 49 patients were treated with a curative approach, and the therapeutic approach of the remaining 14 patients was not reported. Five of these patients had micrometastases (< 2 mm). SNB was applied in 36.7% (18/49) of the patients and preoperative lymphoscintigraphy in 40.8% (20/49), respectively, with 14 not reported for both methods.
Discussion
Typically, in BC management, a positive contralateral lymph node would be classified as distant site metastasis [9]. However, aberrant lymph node drainage following previous surgery or radiotherapy is common. Alternative routes of lymph node drainage develop because of damage to the usual lymphatic system [10,11,12, 15, 26,27,28,29,30]. This can be caused by previous breast and axillary surgery or irradiation for primary BC [13, 30,31,32].
Therefore, if an ipsilateral BC recurrence is diagnosed, the physical examination and imaging with ultrasound, MRI, and FDG PET/CT can be helpful in detecting a CALNM [33]. Furthermore, delayed lymphoscintigraphy should be considered and can be crucial in the setting of tumor recurrence and expected aberrant lymphatic drainage. As in our case, the FDG PET/CT and MRI showed no signs of lymph node metastasis, whereas the lymphoscintigraphy showed a Tc99m signal in a contralateral lymph node (Fig. 2). Subsequent surgical staging by sentinel procedure was performed. In contrast to FDG PET/CT, the sentinel procedure can detect small volume metastatic disease and may therefore add valuable information for adjuvant treatment decisions and improve regional control [34].
Although there is still a lack of guidelines and consensus on CALNM treatment in the recurrent setting, most patients with ipsilateral breast cancer recurrence and CALNM were treated with a curative approach (Table 1). The curative approach is supported by Moossdorff et al. [26] demonstrating that the prognosis of CALNM (82.6% overall survival after mean 50.3 months) receiving locoregional and systematic treatment in the majority of cases is significantly better than the prognosis of patients with metastatic BC and is in line with the prognosis of patients with a regional recurrence. Therefore, a curative treatment approach for patients with CALNM in recurrent BC may have similar outcomes to those with locally advanced stage 3B BC and could be reclassified as ipsilateral supraclavicular disease from M1/stage 4 to N3c/stage 3C in the 6th edition of the AJCC Cancer Staging Manual [35]. However, prospective trials are needed to validate the results of these case reports and retrospective case series.
Taken together, in the recurrent setting, we consider contralateral lymph node metastasis to be a regional event, and therefore, efforts for early detection should be included in the diagnostic workup to allow for treatment with curative intent. In our case, the patient underwent left axillary dissection, adjuvant chemotherapy, and anti-hormone therapy. A non-anthracycline regimen with 6 cycles of TC was used since there was an increased risk of cardiac complications because of the patient’s history of deep vein thromboses and hereditary antithrombin deficiency.
Based on the literature review provided, the incidence of CALNM in recurrent breast cancer cannot be estimated. Patients presenting with CALNM are usually young, with aggressive histopathological features, and an altered lymphatic spread supports the development of CALNM [21, 36, 37]. Overall, BC in young women is characterized by a higher proportion of basal-like, triple-negative, and HER2-enriched tumors, which are often poorly differentiated with lymphovascular invasion [38]. Additionally, young age is an independent risk factor for increased local recurrence [39, 40].
This patient was 37 years old at relapse with luminal B-like features (ER 90%, PR 30%, and Ki-67 25%) and no HER2 overexpression. Additionally, a pathologic mutation of the mismatch repair gene MSH6 is known, which is associated with microsatellite instability. Lynch syndrome, also called hereditary nonpolyposis colorectal cancer, is an autosomal dominant inherited disorder with changes in the MLH1, MSH2, MSH6, PMS2, or EPCAM gene that increases the risk of various cancer types [41].
For women, there is an increased lifetime risk for colorectal carcinoma (30–45%), endometrial cancer (25–50%), and ovarian cancer (6–14%) with Lynch syndrome [42]. The current data for the risk of BC with Lynch syndrome are inconclusive [42,43,44]. But it has been shown that MSH6 is associated with a 31% [45] higher risk and odds ratio of 1.65 (95% CI, 1.06 to 2.52) [46] for BC. In contrast, the BC relapse in our patient showed no microsatellite instability. Because of the high-risk profile of Lynch syndrome, our patient is scheduled for annual cancer screening, and the removal of the remaining ovary may be an option and would allow to continue the AI without OFS.
Conclusion
The rarity of CALNM in BC relapse, along with the controversial staging, complicates the therapeutic decision-making process. This case highlights the value of delayed lymphoscintigraphy and the contribution of sentinel procedure for local control in the setting of recurrent BC. We propose that CALNM without evidence of systemic metastasis should be considered a regional event in recurrent BC, and thus, a curative approach can be pursued. The next AJCC BC staging should clarify the role of CALNM in recurrent BC and adjust the treatment guidelines accordingly.
Availability of data and materials
The data and materials analyzed for the current case report are presented within the manuscript and are also available from the corresponding author. Clinicopathological patient data used during this study are stored in a privacy-compliant locked database and cannot be made available to protect patient privacy.
Abbreviations
- CALNM:
-
Contralateral axillary lymph node metastasis
- BC:
-
Breast cancer
- LN:
-
Lymph node
- FDG PET/CT:
-
Fluorodeoxyglucose positron emission tomography with computed tomography
- MRI:
-
Magnetic resonance imaging
- SNB:
-
Sentinel lymph node biopsy
- L:
-
Lymphoscintigraphy
References
Daoud J, et al. Controlateral axillary nodal metastases of breast cancer. Bullet Ind Cancer. 1998;85(8):713–5.
Zhou C, et al. Contralateral axillary lymph node metastases at the time of primary breast cancer diagnosis: curative or palliative intent? Case Rep Surg. 2013;2013:389013. https://doi.org/10.1155/2013/389013.
Devitt JE, et al. Significance of contralateral axillary metastases in carcinoma of the breast. Can J Surg. 1969;12(2):178–80.
Strazzanti A, et al. Contralateral lymph node metastasis in a woman with new primary breast cancer: systemic desease or locoregional diffusion? Int J Surg Case Rep. 2018;53:400–2.
Maaskant-Braat AJ, et al. Repeat sentinel node biopsy in patients with locally recurrent breast cancer: a systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2013;138(1):13–20. https://doi.org/10.1007/s10549-013-2409-1.
Gingerich J, et al. Contralateral axillary lymph node metastasis in second primary breast cancer: case report and review of the literature. Int J Surg Case Rep. 2017;40:47–9. https://doi.org/10.1016/j.ijscr.2017.08.025.
Vlastos G, et al. Feasibility of breast preservation in the treatment of occult primary carcinoma presenting with axillary metastases. Ann Surg Oncol. 2001;8(5):425–31. https://doi.org/10.1007/s10434-001-0425-6.
Jaffer S, et al. Contralateral axillary lymph node metastasis as the first evidence of locally recurrent breast carcinoma. Cancer. 1995;75(12):2875–8. https://doi.org/10.1002/1097-0142(19950615)75:12<2875::aid-cncr2820751213>3.0.co;2-a.
Amin MB, et al. The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67(2):93–9. https://doi.org/10.3322/caac.21388.
Port ER, et al. Reoperative sentinel lymph node biopsy: a new frontier in the management of ipsilateral breast tumor recurrence. Ann Surg Oncol. 2007;14(8):2209–14. https://doi.org/10.1245/s10434-006-9237-z.
Roumen RM, et al. Lymphatic mapping and sentinel node harvesting in patients with recurrent breast cancer. Eur J Surg Oncol. 2006;32(10):1076–81. https://doi.org/10.1016/j.ejso.2006.08.007 Epub 2006 Sep 22.
Maaskant-Braat AJ, et al. Lymphatic mapping after previous breast surgery. Breast. 2012;21(4):444–8. https://doi.org/10.1016/j.breast.2011.10.007.
Lim I, et al. Drainage across midline to sentinel nodes in the contralateral axilla in breast cancer. Clin Nucl Med. 2004;29(6):346–7. https://doi.org/10.1097/01.rlu.0000127087.12686.81.
Agarwal A, et al. Contralateral uptake and metastases in sentinel lymph node mapping for recurrent breast cancer. J Surg Oncol. 2005;92(1):4–8. https://doi.org/10.1002/jso.20282.
Taback B, et al. Sentinel lymph node biopsy for local recurrence of breast cancer after breast-conserving therapy. Ann Surg Oncol. 2006;13(8):1099–104. https://doi.org/10.1245/ASO.2006.08.026.
Tasevski R, et al. Reoperative sentinel lymph node biopsy in ipsilateral breast cancer relapse. Breast. 2009;18(5):322–6. https://doi.org/10.1016/j.breast.2009.09.009.
Nishimura S, et al. Contralateral axillary node metastasis from recurrence after conservative breast cancer surgery. Clin Nucl Med. 2014;39(2):181–3. https://doi.org/10.1097/RLU.0b013e318286bbbf.
Tokmak H, et al. Management of sentinel node re-mapping in patients who have second or recurrent breast cancer and had previous axillary procedures. World J Surg Oncol. 2014;12:205. https://doi.org/10.1186/1477-7819-12-205.
Wang W, et al. Management of contralateral axillary lymph node metastasis from breast cancer: a clinical dilemma. Tumori. 2014;100(6):600–4. https://doi.org/10.1700/1778.19258.
Chkheidze R, et al. Isolated contralateral axillary lymph node involvement in breast cancer represents a locally advanced disease not distant metastases. Clin Breast Cancer. 2018;18(4):298–304. https://doi.org/10.1016/j.clbc.2017.10.019.
Magnoni F, et al. Contralateral axillary lymph node metastases from breast carcinoma: is it time to review TNM cancer staging? Ann Surg Oncol. 2020;27(11):4488–99. https://doi.org/10.1245/s10434-020-08605-4.
Herrera-Martínez Y, et al. Contralateral axillary lymph node metastasis in a patient with relapsed breast cancer: locoregional event or distant metastasis disease? Oncol Res Treat. 2021;44(3):128–31. https://doi.org/10.1159/000513661.
Maseki H, et al. A case of lymph node dissection for contralateral axillary lymph node metastasis of ipsilateral breast tumor recurrence after identifying the primary lymphatic drainage by lymphoscintigraphy. Int Cancer Conf J. 2021;10(2):154–8. https://doi.org/10.1007/s13691-021-00470-6.
Salih AM, et al. Breast cancer metastasizing to the contralateral axilla several years after treatment: a case report with literature review. Int J Surg Case Rep. 2021;82:105900. https://doi.org/10.1016/j.ijscr.2021.105900.
Goh IY, Dauway EL. Synchronous contralateral axillary lymph node metastasis in a recurrent breast cancer following previous axillary clearance. BMJ Case Rep. 2022;15(3):e248741. https://doi.org/10.1136/bcr/-2022-248741.
Moossdorff M, et al. Contralateral lymph node recurrence in breast cancer: regional event rather than distant metastatic disease. A systematic review of the literature. Eur J Surg Oncol. 2015;41(9):1128–36. https://doi.org/10.1016/j.ejso.2015.05.015.
Boughey JC, et al. Sentinel lymph node surgery in locally recurrent breast cancer. Clin Breast Cancer. 2006;7(3):248–53. https://doi.org/10.3816/CBC.2006.n.037.
Wellner R, et al. Altered lymphatic drainage after breast-conserving surgery and axillary node dissection: local recurrence with contralateral intramammary nodal metastases. Clin Breast Cancer. 2007;7(6):486–8. https://doi.org/10.3816/CBC.2007.n.006.
Sood A, et al. Alternative lymphatic pathway after previous axillary node dissection in recurrent/primary breast cancer. Clin Nucl Med. 2004;29(11):698–702. https://doi.org/10.1097/00003072-200411000-00005.
Estourgie SH, et al. Excision biopsy of breast lesions changes the pattern of lymphatic drainage. Br J Surg. 2007;94(9):1088–91. https://doi.org/10.1002/bjs.5763.
Lizarraga IM, et al. Review of risk factors for the development of contralateral breast cancer. Am J Surg. 2013;206(5):704–8. https://doi.org/10.1016/j.amjsurg.2013.08.002.
Perre CI, et al. Altered lymphatic drainage after lymphadenectomy or radiotherapy of the axilla in patients with breast cancer. Br J Surg. 1996;83(9):1258. https://doi.org/10.1046/j.1365-2168.1996.02349.x.
Kim SJ, et al. The detection of recurrent breast cancer in patients with a history of breast cancer surgery: comparison of clinical breast examination, mammography and ultrasonography. Acta Radiol. 2011;52(1):15–20. https://doi.org/10.1258/ar.2010.100261.
Kasem J, et al. Sensitivity, specificity and the diagnostic accuracy of PET/CT for axillary staging in patients with stage i-iii cancer: a systematic review of the literature. In Vivo. 2021;35(1):23–30. https://doi.org/10.21873/invivo.12228.
Singletary SE, et al. Staging system for breast cancer: revisions for the 6th edition of the AJCC Cancer Staging Manual. Surg Clin North Am. 2003;83(4):803–19. https://doi.org/10.1016/S0039-6109(03)00034-3.
Morcos B, Jaradat I, El-Ghanem M. Characteristics of and therapeutic options for contralateral axillary lymph node metastasis in breast cancer. Eur J Surg Oncol. 2011;37:418–21.
Huston TL, et al. The presentation of contralateral axillary lymph node metastases from breast carcinoma: a clinical management dilemma. Breast J. 2007;13(2):158–64. https://doi.org/10.1111/j.1524-4741.2007.00390.x.
Azim HA Jr, et al. Biology of breast cancer in young women. Breast Cancer Res. 2014;16(4):427. https://doi.org/10.1186/s13058-014-0427-5.
Bantema-Joppe EJ, et al. Early-stage young breast cancer patients: impact of local treatment on survival. Int J Radiat Oncol Biol Phys. 2011;81(4):e553–9. https://doi.org/10.1016/j.ijrobp.2011.02.060.
Botteri E, et al. Analysis of local and regional recurrences in breast cancer after conservative surgery. Ann Oncol. 2010;21(4):723–8. https://doi.org/10.1093/annonc/mdp386.
Lynch HT, et al. Milestones of Lynch syndrome: 1895-2015. Nat Rev Cancer. 2015;15(3):181–94. https://doi.org/10.1038/nrc3878.
Barrow E, et al. Cancer risk in Lynch syndrome. Fam Cancer. 2013;12(2):229–40. https://doi.org/10.1007/s10689-013-9615-1.
Kohlmann W. Lynch syndrome and breast cancer risk: weighing the data. JCO Precis Oncol. 2020;4:PO.19.00376. https://doi.org/10.1200/PO.19.00376.
Win AK, et al. Risk of breast cancer in Lynch syndrome: a systematic review. Breast Cancer Res. 2013;15(2):R27. https://doi.org/10.1186/bcr3405.
Roberts ME, et al. MSH6 and PMS2 germ-line pathogenic variants implicated in Lynch syndrome are associated with breast cancer. Genet Med. 2018;20(10):1167–74. https://doi.org/10.1038/gim.2017.254.
LaDuca H, et al. A clinical guide to hereditary cancer panel testing: evaluation of gene-specific cancer associations and sensitivity of genetic testing criteria in a cohort of 165,000 high-risk patients. Genet Med. 2020;22(2):407–15. https://doi.org/10.1038/s41436-019-0633-8.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All the authors made substantial contributions and gave permission for their names to be included as co-authors. TZ, FS, WW, and CK conceived and designed the case report and literature review. TZ, FK, NS, DS, FS, and FG collected the data. TZ, JG, FS, NS, DS, VHS, and CK analyzed and interpreted the data. All authors contributed to manuscript drafting, critical review of the manuscript, and final approval of the manuscript in its current form. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to the ethics committee of Northwest and Central Switzerland (EKNZ), this project did not fall under the remit of the cantonal or federal law, Human Research Act (HRA), because the project was not defined as a research project as per HRA Article 2. Therefore, Institutional Review Board approval was not needed. The patient gave her written consent to participate in this case report and waived any claims. The anonymization of personal data was guaranteed.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review upon request.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zwimpfer, T.A., Schwab, F.D., Steffens, D. et al. Contralateral lymph node metastasis in recurrent ipsilateral breast cancer with Lynch syndrome: a locoregional event. World J Surg Onc 21, 40 (2023). https://doi.org/10.1186/s12957-023-02918-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-02918-w