Abstract
Background
There are currently no scoring-type predictive models using only easily available pre- and intraoperative data developed for assessment of the risk of advanced axillary lymph node metastasis (ALNM) in patients with breast cancer with metastatic sentinel lymph nodes (SLNs). We aimed to develop and validate a scoring system using only pre- and intraoperative data to distinguish between non-advanced (≤ 3 lymph nodes) and advanced (> 3 lymph nodes) ALNM in patients with breast cancer with metastatic SLNs.
Methods
We retrospectively identified 804 patients with breast cancer (cT1-3cN0) who had metastatic SLNs and had undergone axillary lymph node dissection (ALND). We evaluated the risk factors for advanced ALNM using logistic regression analysis and developed and validated a scoring system for the prediction of ALNM using training (n = 501) and validation (n = 303) cohorts, respectively. The predictive performance was assessed using the receiver operating characteristic (ROC) curve, area under the curve (AUC), and calibration plots.
Results
Ultrasound findings of multiple suspicious lymph nodes, SLN macrometastasis, the ratio of metastatic SLNs to the total number of SLNs removed, and the number of metastatic SLNs were significant risk factors for advanced ALNM. Clinical tumor size and invasive lobular carcinoma were of borderline significance. The scoring system based on these six variables yielded high AUCs (0.90 [training] and 0.89 [validation]). The calibration plots of frequency compared to the predicted probability showed slopes of 1.00 (training) and 0.85 (validation), with goodness-of-fit for the model. When the cutoff score was set at 4, the negative predictive values (NPVs) of excluding patients with advanced ALNM were 96.8% (training) and 96.9% (validation). The AUC for predicting advanced ALNM using our scoring system was significantly higher than that predicted by a single independent predictor, such as the number of positive SLNs or the proportion of positive SLNs. Similarly, our scoring system also showed good discrimination and calibration ability when the analysis was restricted to patients with one or two SLN metastases.
Conclusion
Our easy-to-use scoring system can exclude advanced ALNM with high NPVs. It may contribute to reducing the risk of undertreatment with adjuvant therapies in patients with metastatic SLNs, even if ALND is omitted.
Similar content being viewed by others
Background
Recently, several trials have explored the safety of omitting axillary lymph node (ALN) dissection (ALND) and administering appropriate adjuvant therapy in patients with early breast cancer having limited axillary involvement [1,2,3]. However, precise information on the total number of involved lymph nodes cannot be obtained if ALND is omitted in patients with metastatic sentinel lymph nodes (SLNs). In previous studies, 13–33% of patients who had undergone ALND for SLN metastases had non-SLN metastases [1,2,3], and 13.7% of patients had ≥ 4 lymph node metastases [3]. When determining systemic therapy and regional irradiation strategies for patients with breast cancer, it is important to distinguish between non-advanced ALN status (i.e., 0–3 positive ALNs) and advanced ALN metastasis (ALNM) (i.e., ≥ 4 positive ALNs) [4]. Although performing ALND in patients with non-advanced ALNM may lead to overtreatment, omitting ALND in patients with advanced ALNM may lead to undertreatment. Therefore, it is important to accurately estimate whether a patient has non-advanced or advanced ALNM if omitting ALND in patients with metastatic SLNs. Several nomograms reportedly predict the risk of advanced ALNM in patients with metastatic SLNs; however, most nomograms use data obtained from surgery, such as pathological tumor size or lymphovascular invasion; therefore, it is difficult to use these nomograms intraoperatively [5,6,7,8,9]. Other nomograms use the total tumor load of SLNs evaluated by one-step nucleic acid amplification as a predictor [10, 11], but this method is not yet commonly used in clinical practice. Therefore, a model that can accurately predict the likelihood of a patient with metastatic SLN having advanced ALNM using only easily available preoperative and intraoperative data is required.
The number of suspicious nodes on axillary ultrasound (US) is related to the number of positive ALNs [12,13,14]. The histologic type of invasive lobular histology is related to advanced ALNM [7, 12, 15] as well. Although these factors may improve the predictive performance of ALN status, no model has been developed to predict advanced ALNM by combining preoperative data of axillary US imaging and histology with intraoperative data of SLNs.
We previously developed an easy-to-use scoring system with only preoperatively available data that could distinguish between advanced and non-advanced ALNM with a high degree of accuracy for patients with cT1-T3cN0-1 breast cancer [12]. However, some patients that were used to develop the previous predictive model had undergone ALND without SLN biopsy (SLNB) or had not undergone ALND when one to two SLNs were positive. Especially, we might have underestimated the total number of positive nodes because not all patients had undergone ALND. Additionally, the previous predictive model was not a model specific to clinically node-negative patients. Therefore, we conducted a new study to develop and evaluate a scoring model that can differentiate non-advanced and advanced ALNM cases with a combination of available preoperative and intraoperative data in clinically node-negative patients with metastatic SLNs who had undergone ALND.
Methods
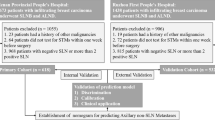
The dataset comprised consecutive patients who had operable primary breast cancer (clinical TNM stage, T1-T3, and N0 as per the 8th edition of the American Joint Committee of Cancer [AJCC] Cancer Staging Manual [16]) in our institutional database from January 2010 to October 2021. We excluded patients who had locally advanced disease (T4 or N2-3) and those who had received neoadjuvant chemotherapy (NAC). We also excluded patients who had not undergone SLNB and those with negative SLNs. Patients with positive SLNs who had not undergone ALND were also excluded. We identified 804 patients, who were randomly divided into the training and the validation cohorts in a ratio of 5:3 using the statistical software STATA SE version 13 (Stata Corp., College Station, TX, USA). The training and validation cohorts were used to develop the scoring system and for validation, respectively. The detailed exclusion criteria are presented in Fig. 1.
Data collection
We obtained patients’ medical records regarding age at diagnosis, clinical tumor size evaluated by US, total number of suspicious lymph nodes detected by the axillary US, histologic tumor type, histologic tumor grade, estrogen receptor (ER) status, progesterone receptor (PR) status, human epidermal growth factor receptor 2 (HER2) status, Ki-67 level, and total number of metastatic lymph nodes in SLNB and ALND. ER and PR positivity were defined as immunohistochemical staining of > 1% of tumor cells. Hormone receptor (HR) positivity was defined as ER positivity and/or PR positivity. HER2 positivity was defined as a score of 3+ on immunohistochemistry or on amplification of fluorescence in situ hybridisation [16, 17]. Regarding the classification of Ki-67 levels, in the St. Gallen International Consensus Guidelines for treatment of early breast cancer 2021, the panel generally supported the recommendation that tumors with Ki-67 ≥ 30% receive chemotherapy, but the Ki-67 threshold for recommending chemotherapy in ER-positive cases could not be consistently defined as 10–25% [18]. Considering this point, we classified the tumors according to the Ki-67 level into the following three groups: ≤ 10%, 10–30%, and ≥ 30%. Diffuse cortical thickness > 5 mm, asymmetric cortical thickness > 3 mm, and complete or near-complete absence of fatty hilum on the axillary US were considered as suspicious lymph nodes [19, 20]. Fine-needle aspiration cytology was performed for suspicious ALNs. The most suspicious node was sampled in patients with multiple suspicious lymph nodes, and the number of suspicious nodes was recorded.
Surgical procedure
SLNB was performed on all patients. SLNs were identified using lymphoscintigraphy (technetium-99m phyrate) and/or indocyanine green. Completion level I–II ALND was performed in all patients regardless of the metastatic size of the SLNs.
Pathological evaluation
ALNs were evaluated using hematoxylin and eosin staining. Each ALN was classified as negative or positive for metastasis, and the number of metastatic ALNs was recorded. According to the current AJCC criteria [21], isolated tumor cells (deposit < 0.2 mm) were classified as negative (pN0i+), and micrometastatic deposits of 0.2–2.0 mm were classified as positive for metastasis (pN1mi). Pathologic nodal staging was determined by the number of metastatic ALNs as follows: pN0, none; pN1 (1–3 lymph node metastases), limited; and pN2-3 (> 3 lymph node metastases), advanced.
Statistical analysis
Tumor characteristics and axillary US scans of patients in the training and validation cohorts were compared using the Mann–Whitney U test or chi-square test, as appropriate. In the training cohort, the odds ratios (ORs) and 95% confidence intervals (CIs) for advanced ALNM were calculated using univariate logistic regression analysis. Baseline variables (P < 0.10 on univariate analysis were assessed for multicollinearity using the variance inflation factor (VIF). A VIF of > 10 indicated multicollinearity between the variables [22]. Baseline variables (P < 0.10 on univariate analysis) were included in the multivariate regression analysis, which was used to devise the scoring system. For each of these variables (P < 0.10 on multivariate analysis), a score was calculated using the β-coefficient by the value rounded to the nearest integer as each score. The total score was derived from the sum of the scores for each variable. Then, discrimination and calibration accuracy of the scoring system was evaluated to distinguish between advanced and non-advanced ALNM cases. The discrimination ability of each scoring system was evaluated using the receiver operating characteristic (ROC) curve, and then assessed by calculating the area under the curve (AUC) with a 95% CI. Calibration was evaluated by comparing the expected number of patients with advanced ALNM (as predicted by each total score) with the observed number of patients with advanced ALNM. The calibration of our scoring system was tested by performing the Hosmer–Lemeshow goodness-of-fit test on the training cohort [23]. To evaluate the generalisability of the scoring system, a 5-fold cross-validation (CV) was performed [24] using the training cohort dataset.
The diagnostic performance of the scoring system for predicting advanced ALNM was estimated in terms of its AUC, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of each cutoff value of the scoring system. The feasibility of the scoring system was evaluated with the validation cohort.
All statistical analyses were conducted using the statistical software STATA SE version 13 (Stata Corp). P < 0.05 was set as the threshold for significance.
Results
Factors associated with advanced ALNM in the training cohort
Patient demographics and tumor characteristics of both the training and validation cohorts are summarized in Table 1. Patient and tumor characteristics were well-balanced between the training and validation cohorts.
The factors associated with advanced ALNM are summarized in Table 2. Univariate analysis revealed that the significant factors associated with advanced ALNM were the clinical tumor size, histologic type, type of surgery, axillary US findings of suspicious lymph nodes, size of SLN metastasis, ratio of the number of positive SLNs to the total number of SLNs removed, and number of positive SLNs. Variables with P < 0.10 in univariate analysis were assessed for multicollinearity (Table S1). No variable with a VIF > 10 was found, indicating no collinearity between the variables. In the multivariate analysis, patients with advanced ALNM were more likely to have US findings of multiple suspicious lymph nodes, SLN macrometastasis, higher ratio of the number of metastatic SLNs to the total number of SLNs removed, and two or three metastatic SLNs. A clinical tumor size of 4–5 cm or > 5 cm and a histologic type of invasive lobular carcinoma were of borderline significance.
Scoring system for distinguishing between non-advanced and advanced ALNM
Using the results of the multivariate analysis, a scoring system was devised to assess the likelihood of advanced ALNM (Table 3). The factors included were the clinical tumor size, axillary US findings, histologic type, size of SLN metastasis, ratio of the number of positive SLNs to the total number of SLNs removed, and number of positive SLNs. A score was calculated using the β-coefficient from the multivariate analysis, and the value rounded to the nearest integer was used as each score. The total score was derived from the sum of the scores for each variable. The percentage of patients with advanced ALNM increased significantly as the total score increased (Table 4).
Predictive accuracy of the scoring system in the training cohort
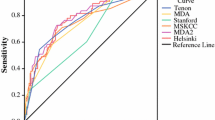
The ROC curves for the scoring system in the training cohort are shown in Fig. 2A. The AUC was 0.90, and the 5-fold CV showed a mean AUC of 0.90. The calibration plots of frequency compared to the predicted probability of the scoring model showed a slope of 1.00 for the training cohort (Fig. 2C), and the Hosmer-Lemeshow test indicated goodness-of-fit for the model in the training cohort (P = 0.69). The predictive accuracy of the scoring system for differentiating between non-advanced and advanced ALNM cases at each cutoff value is presented in Table 5. The AUC value was highest when the cutoff value was a total score of 4. At this score, the NPV for excluding advanced ALNM was 96.8%, and the sensitivity, specificity, and PPV were 85.3%, 79.1%, and 41.8%, respectively.
ROC curves of the scoring system for differentiating between non-advanced and advanced ALNM in the training cohort (A) and the validation cohort (B), and calibration plots of the system for the training cohort (C) and the validation cohort (D). The Hosmer–Lemeshow test indicated goodness-of-fit for the model in the training (χ2 = 3.09, P = 0.69) and validation cohorts (χ2 = 9.44, P = 0.31). The calibration plot of the observed frequency compared to the predicted probability of the scoring model showed slopes of 1.000 for the training cohort (C) and 0.852 for the validation cohort (D). ROC, receiver operating characteristic; ALNM, axillary lymph node metastasis; AUC, area under the curve; CI, confidence interval
Performance of the scoring system for the validation cohort
The percentage of patients with advanced ALNM in the validation cohort also increased significantly as the total score increased (Table 4). The ROC curve for the scoring system in the validation cohort is shown in Fig. 2B. The AUC was 0.89, and the calibration plots of frequency compared to the predicted probability of the scoring model showed a slope of 0.852 (Fig. 2D). The Hosmer–Lemeshow test indicated goodness-of-fit for the model in the validation cohort (P = 0.31). At a total score of 4 points, the AUC was 0.81 (95% CI, 0.76–0.87); the NPV for excluding advanced ALNM was 96.9%; and sensitivity, specificity, and PPV were 87.8%, 74.8%, and 40.2%, respectively (Table 5).
Discussion
In the present study, we developed a scoring system using available preoperative clinicopathological factors and the intraoperative SLN status to differentiate between non-advanced and advanced ALNM in patients with breast cancer having positive SLNs following ALND. We evaluated the predictive accuracy of the scoring system by assessing the discrimination and calibration ability in the training cohort and then evaluated its feasibility using the validation cohort. The results revealed that the scoring system had a high predictive performance. Therefore, our scoring system may identify patients with positive SLNs who are likely to have non-advanced ALNM.
The tumor size, histologic type, size of SLN metastasis, number of positive SLNs, proportion of positive SLNs, and suspicious lymph nodes on the axillary US are potential factors that would be useful in predicting the likelihood of advanced ALNM [5,6,7,8,9, 11, 12], which was confirmed by our study. Therefore, we confirmed the non-collinearity between these variables before developing the scoring system.
The pathological tumor size has often been reported as a factor for predicting advanced ALNM [5,6,7,8, 11], while the clinical tumor size has been less frequently reported [9, 12]. Although pathological tumor size is a more accurate factor than clinical tumor size, it is unavailable preoperatively; therefore, we used clinical tumor size evaluated by US to develop our scoring system, which assigned 2 and 0 points for a clinical tumor size > 4 cm and ≤ 4 cm, respectively. Among the 717 patients in our entire cohort whose clinical tumor size was estimated to be < 4 cm, only 71 (9.9%) had a pathological tumor size > 4 cm (data not shown). Thus, the NPV of patients whose clinical tumor size was estimated to be ≤ 4 cm was as high as 90.1%, suggesting that the risk of underestimating the tumor size was low. The clinical tumor size is easy to estimate by US, which is an advantage of our scoring system.
ILC was an independent risk factor for advanced ALNM in our study. US findings of axillary nodes coupled with FNA have been reported to be useful in predicting heavy axillary burden [25]. Advanced ALNM with false-negative US findings was more prevalent in patients with ILC than in those with infiltrating ductal carcinoma (IDC) because of the morphological features of ILC [26, 27]. Fine-needle aspiration biopsy of suspicious ALNs on US was less sensitive in patients with ILC than in those with IDC [28, 29]. Therefore, we believe that the inclusion of histologic type as a predictive factor in the scoring system is an important complement to US findings.
A suspicious ALN on US often corresponds to an SLN. Considering that the false-negative rate for SLNB is 7.3–9.8% [30, 31], adding axillary US findings to the scoring system may reduce the risk of underestimating non-SLN metastasis. The AUC value for predicting advanced ALNM using our scoring system was significantly higher than that predicted by a single independent predictor, such as the number of positive SLNs or the proportion of positive SLNs (Figure S1).
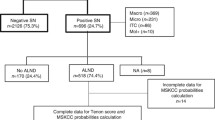
In the analysis restricted to patients with one or two SLN metastases, our scoring system showed similarly good discrimination and calibration abilities (Figure S2). Specifically, 386 (77.0%) of 501 patients in the training cohort and 238 (78.5%) of 303 patients in the validation cohort had 1–2 SLN metastases, while 54 (14.0%) of 386 patients in the training cohort and 31 (13.0%) of 238 patients in the validation cohort had advanced ALNM; these frequencies were similar to those previously reported [3]. Assuming that these patients with advanced ALNM undergo only SLNB, the indications for postoperative chemotherapy and regional irradiation may be determined based on the underestimated lymph node status of the SLNB, thereby resulting in undertreatment.
In the training cohort, when the cutoff point of our scoring system was set to 4, 262 (67.9%) patients with 1–2 metastatic SLNs had a score of ≤ 4 points, and the NPV was 95.8% (Tables S2 and S3). A high NPV indicated that our scoring system accurately detected patients with 1–2 metastatic SLNs but a low risk of advanced ALNM. Therefore, even if ALND is omitted in patients with a score ≤ 4 and the indication for postoperative chemotherapy or regional irradiation is determined based only on SLNB results, the risk of undertreatment is low. Although no adverse prognostic effect of ALND omission has been observed [3], at each individual patient level, underestimating the number of lymph node metastases due to ALND omission may affect decisions regarding adjuvant treatment, leading to a risk of undertreatment. As our study was not a prospective study, the effectiveness of using the total score to determine whether ALND should be performed (and whether adjuvant therapy should be administered) is unclear. However, the ability of our scoring system to intraoperatively predict the risk of non-advanced and advanced ALNM at the individual level in patients with 1–2 metastatic SLNs may help reduce the risk of undertreatment with adjuvant therapy even if ALND is omitted.
The strength of our model is that it is based on available clinicopathological features from preoperative and intraoperative evaluations conducted in routine clinical oncology practice. The first advantage of including US findings in the predictive model is that US is a non-invasive, reproducible, and low-cost diagnostic tool. Second, while axillary assessment by magnetic resonance imaging is affected by body mass index and has decreased sensitivity in obese patients [32], US has been reported to have similar sensitivity in obese and non-obese patients and better specificity in obese patients [33]. All patients underwent level I–II ALND completion, which provided accurate information regarding ALNM. Additionally, the scoring system-type prediction model is relatively simple compared to the nomogram-type model and is easily implemented in daily clinical practice.
This study had several limitations. First, it was performed at a single institution. Second, although we collected data from consecutive patients with invasive breast carcinoma, we did not control for selection bias. Patients who had undergone NAC were excluded. Patients with HR−/HER2+ and HR−/HER2− tended to receive NAC compared to those with HR+/HER2−, even if they were clinically node-negative, and the inclusion of these patients might have affected our results.
Conclusions
We developed a scoring system to accurately differentiate non-advanced ALNM from advanced ALNM in patients with breast cancer demonstrating SLN metastasis. This scoring system is easy to use, requires only preoperative and intraoperative available data, and can exclude advanced ALNM with a high NPV. Hence, it may contribute to reducing the risk of undertreatment with adjuvant therapy in patients with metastatic SLNs, even if ALND is omitted.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AJCC:
-
American Joint Committee of Cancer
- ALN:
-
Axillary lymph node
- ALND:
-
Axillary lymph node dissection
- ALNM:
-
Axillary lymph node metastasis
- AUC:
-
Area under the receiver operating characteristic curve
- CI:
-
Confidence interval
- CV:
-
Cross-validation
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hormone receptor
- IDC:
-
Invasive ductal carcinoma
- ILC:
-
Invasive lobular carcinoma
- LVI:
-
Lymphovascular invasion
- NAC:
-
Neoadjuvant chemotherapy
- NPV:
-
Negative predictive value
- OR:
-
Odds ratio
- PPV:
-
Positive predictive value
- PR:
-
Progesterone receptor
- ROC:
-
Receiver operating characteristic
- SLN:
-
Sentinel lymph node
- SLNB:
-
Sentinel lymph node biopsy
- US:
-
Ultrasound
- VIF:
-
Variance inflation factor
References
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–75.
Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981–22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15:1303–10.
Galimberti V, Cole BF, Zurrida S, Viale G, Luini A, Veronesi P, et al. Trial 23-01 investigators. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23–01): a phase 3 randomised controlled trial. Lancet Oncol. 2013;14:297–305.
Burstein HJ, Curigliano G, Loibl S, Dubsky P, Gnant M, Poortmans P, et al. Estimating the benefits of therapy for early-stage breast cancer: the St. Gallen International Consensus Guidelines for the primary therapy of early breast cancer 2019. Ann Oncol. 2019;30:1541–57.
Yang Z, Lan X, Huang Z, Yang Y, Tang Y, Jing H, et al. Development and external validation of a nomogram to predict four or more positive nodes in breast cancer patients with one to three positive sentinel lymph nodes. Breast. 2020;53:143–51.
Chagpar AB, Scoggins CR, Martin RC 2nd, Cook EF, McCurry T, Mizuguchi N, et al. Predicting patients at low probability of requiring postmastectomy radiation therapy. Ann Surg Oncol. 2007;14:670–7.
Katz A, Smith BL, Golshan M, Niemierko A, Kobayashi W, Raad RA, et al. Nomogram for the prediction of having four or more involved nodes for sentinel lymph node-positive breast cancer. J Clin Oncol. 2008;26:2093–8.
Unal B, Gur AS, Beriwal S, Tang G, Johnson R, Ahrendt G, et al. Predicting likelihood of having four or more positive nodes in patient with sentinel lymph node-positive breast cancer: a nomogram validation study. Int J Radiat Oncol Biol Phys. 2009;75:1035–40.
Kim I, Ryu JM, Kim JM, Choi HJ, Lee SK, Yu JH, et al. Development of a nomogram to predict N2 or N3 stage in T1-2 invasive breast cancer patients with no palpable lymphadenopathy. J Breast Cancer. 2017;20:270–8.
Jimbo K, Kinoshita T, Ogura T, Watase C, Murata T, Shiino S, et al. Prediction score model for non-sentinel and four or more nodal metastases using a combined method of one-step nucleic acid amplification and histology in sentinel node-positive breast cancer patients. Eur J Surg Oncol. 2020;46:516–21.
Shimazu K, Sato N, Ogiya A, Sota Y, Yotsumoto D, Ishikawa T, et al. Intraoperative nomograms, based on one-step nucleic acid amplification, for prediction of non-sentinel node metastasis and four or more axillary node metastases in breast cancer patients with sentinel node metastasis. Ann Surg Oncol. 2018;25:2603–11.
Murata T, Watase C, Shiino S, Jimbo K, Iwamoto E, Yoshida M, et al. Development and validation of a preoperative scoring system to distinguish between nonadvanced and advanced axillary lymph node metastasis in patients with early-stage breast cancer. Clin Breast Cancer. 2021;21:e302–11.
Harris CK, Tran HT, Lee K, Mylander C, Pack D, Rosman M, et al. Positive ultrasound-guided lymph node needle biopsy in breast cancer may not mandate axillary lymph node dissection. Ann Surg Oncol. 2017;24:3004–10. https://doi.org/10.1245/s10434-017-5935-y.
Lim GH, Upadhyaya VS, Acosta HA, Lim JMA, Allen JC, Leong LCH. Preoperative predictors of high and low axillary nodal burden in Z0011 eligible breast cancer patients with a positive lymph node needle biopsy result. Eur J Surg Oncol. 2018;44:945–50.
Schumacher K, Inciardi M, O’Neil M, Wagner JL, Shah I, Amin AL, et al. Is axillary imaging for invasive lobular carcinoma accurate in determining clinical node staging? Breast Cancer Res Treat. 2021;185:567–72.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human epidermal growth factor Receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. J Clin Oncol. 2018;36:2105–22.
Burstein HJ, Curigliano G, Thürlimann B, Weber WP, Poortmans P, Regan MM, et al. Customizing local and systemic therapies for women with early breast cancer: the St. Gallen International Consensus Guidelines for treatment of early breast cancer 2021. Ann Oncol. 2021;32:1216–35.
Abe H, Schacht D, Sennett CA, Newstead GM, Schmidt RA. Utility of preoperative ultrasound for predicting pN2 or higher stage axillary lymph node involvement in patients with newly diagnosed breast cancer. AJR Am J Roentgenol. 2013;200:696–702.
Mainiero MB, Cinelli CM, Koelliker SL, Graves TA, Chung MA. Axillary ultrasound and fine-needle aspiration in the preoperative evaluation of the breast cancer patient: an algorithm based on tumor size and lymph node appearance. AJR Am J Roentgenol. 2010;195:1261–7.
Giuliano AE, Edge SB, Hortobagyi GN. Eighth Edition of the AJCC Cancer Staging Manual: Breast cancer. Ann Surg Oncol. 2018;25:1783–5.
Myers RH. Classical and modern regression with applications 2nd Edition; Pacific Grove: Duxbury/Thompson Learning Publishing Company; 1990.
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21:128–38.
Luque-Fernandez MA, Redondo-Sanchez D, Maringe C. Cross-validated area under the curve. GitHub repository; 2019. https://github.com/migariane/cvaurocAccessed, Accessed 17 Nov 2021
Buzatto IPC, Dos Reis FJC, de Andrade JM, Rodrigues TCGF, Borba JMC, Netto AH, et al. Axillary ultrasound and fine-needle aspiration cytology to predict clinically relevant nodal burden in breast cancer patients. World J Surg Oncol. 2021;19:292.
Cserni G, Bianchi S, Vezzosi V, Peterse H, Sapino A, Arisio R, et al. The value of cytokeratin immunohistochemistry in the evaluation of axillary sentinel lymph nodes in patients with lobular breast carcinoma. J Clin Pathol. 2006;59:518–22.
Boughey JC, Middleton LP, Harker L, Garrett B, Fornage B, Hunt KK, et al. Utility of ultrasound and fine-needle aspiration biopsy of the axilla in the assessment of invasive lobular carcinoma of the breast. Am J Surg. 2007;194:450–5.
Topps A, Clay V, Absar M, Howe M, Lim Y, Johnson R, et al. The sensitivity of pre-operative axillary staging in breast cancer: comparison of invasive lobular and ductal carcinoma. Eur J Surg Oncol. 2014;40:813–7.
Morrow E, Lannigan A, Doughty J, Litherland J, Mansell J, Stallard S, et al. Population-based study of the sensitivity of axillary ultrasound imaging in the preoperative staging of node-positive invasive lobular carcinoma of the breast. Br J Surg. 2018;105:987–95.
Kim T, Giuliano AE, Lyman GH. Lymphatic mapping and sentinel lymph node biopsy in early-stage breast carcinoma: a metaanalysis. Cancer. 2006;106:4–16.
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Ashikaga T, et al. Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol. 2007;8:881–8.
Chen ST, Lai HW, Wu WP, Chen ST, Liao CY, Wu HK, et al. The impact of body mass index (BMI) on MRI diagnostic performance and surgical management for axillary lymph node in breast cancer. World J Surg Oncol. 2022;20:45.
Shah AR, Glazebrook KN, Boughey JC, Hoskin TL, Shah SS, Bergquist JR, et al. Does BMI affect the accuracy of preoperative axillary ultrasound in breast cancer patients? Ann Surg Oncol. 2014;21:3278–83.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
TM, MY, and SS conceptualized the study. TM worked on the methodology of the study. TM, CW, AO, AK, SS, KJ, EI, and ST participated in the formal analysis and investigation. TM was responsible for the preparation of the original draft, and SS and TM reviewed and edited the manuscript. AS supervised the study. All authors appraised the previous versions of the manuscript and have read and approved its final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review board and ethical committee of our institution approved this study (approval no. 2017-278). The requirement for informed consent was waived because of the retrospective design of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Comparison of ROC curves of the scoring system between the training (A) and validation (B) cohorts and the analysis of independent factors to differentiate between non-advanced and advanced ALNM in both these cohorts. Figure S2. ROC curves of the scoring system compared between the training (A) and validation cohorts (B) and presentation of independent factors for differentiating between non-advanced and advanced ALNM in the two cohorts and calibration plots of the scoring system for the training cohort (C) and the validation cohort (D) in patients with one or two metastatic SLNs.
Additional file 2: Table S1.
Evaluation of multivariable collinearity with P < 0.1 in the univariate analysis. Table S2. Distribution of advanced ALNM (pN2-N3) stratified by the total score in the training and validation cohorts in patients with one or two metastatic SLNs. Table S3. Predictive ability of the scoring system to differentiate between non-advanced and advanced ALNM at each cutoff point in the training cohort (A) and validation cohort (B) in patients with one or two metastatic sentinel lymph nodes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Murata, T., Watase, C., Shiino, S. et al. Development and validation of a pre- and intra-operative scoring system that distinguishes between non-advanced and advanced axillary lymph node metastasis in breast cancer with positive sentinel lymph nodes: a retrospective study. World J Surg Onc 20, 314 (2022). https://doi.org/10.1186/s12957-022-02779-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02779-9