Abstract
Background
A right top pulmonary vein (RTPV) that crosses behind the right main or intermediate bronchus is a variation of the superior posterior pulmonary vein in the right upper lobe. Damage or ligation of this abnormal vessel can lead to massive intraoperative bleeding and serious complications, such as congestion of the posterior segment of the right upper lobe and cardiac tamponade. Subcarinal lymph node dissection is mandatory in radical thoracoscopic esophagectomy for esophageal cancer, and the RTPV is an anomalous vessel of which thoracic surgeons should be aware.
Case presentation
A 70-year-old man underwent thoracoscopic esophagectomy for esophageal cancer (T3N1M0). An anomaly of the superior posterior pulmonary vein in the right lobe was recognized on preoperative computed tomography imaging. With simulation and intraoperative navigation using three-dimensional imaging of the same view as that observed during the operation, radical subcarinal dissection could be performed with preservation of the RTPV.
Conclusion
In our review of the relevant literature, the incidence of RTPV ranged from 0.28 to 9.3%, and its mean vascular diameter was 7.0 mm at the maximum and 2.2 ± 0.72 mm at the minimum, with the right superior pulmonary vein being a relatively common inflow site. Our case in which the RTPV ran dorsal to the right main bronchus is very rare. In radical subcarinal dissection of thoracoscopic esophagectomy, it is important to recognize the posterior pericardial plane and release the ventral fixation of these lymph nodes to free space for the back side. This is also true in the case of RTPV, which should be noted to avoid injury. In cases involving an RTPV larger than 4.5 mm, ligation should be avoided, and preoperative recognition of the exact run of this abnormal vessel using three-dimensional imaging can be very useful.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Pulmonary veins have many anatomical variations, some of which may be affected during esophagectomy for esophageal cancer. The right posterior upper lobe segment vein, known as the right top pulmonary vein (RTPV), is rare anomalous vein running behind the right main or intermediate bronchus from the right upper lobe. The subcarinal portion of the RTPV penetrates the subcarinal lymph nodes (SCLNs). It is important to recognize this vein because SCNL dissection is an essential procedure for curative esophagectomy for esophageal cancer [1].
Case presentation
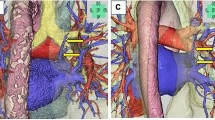
A 70-year-old man complained of difficulty in swallowing food and was referred from another hospital. He was diagnosed with esophageal squamous cell carcinoma T3N1M0 in the median thoracic esophagus, according to the TNM classification, eighth edition. We therefore selected neoadjuvant chemotherapy (bi-weekly DCF: docetaxel 35 mg/m2, cisplatin 40 mg/m2, fluorouracil 400 mg/m2) as preoperative treatment [2, 3]. Preoperative contrast-enhanced computed tomography (CT) imaging revealed an aberrant branch of right posterior segmental vein (V2) passing behind the right main bronchus and merging with left atrium (LA) (Fig. 1). We used a high-speed three-dimensional (3D) image analysis system (SYNAPSE VINCENT, Fuji Photo Film Co., Ltd., Tokyo, Japan) to convert the Digital Imaging and Communication in Medicine (DICOM) data of contrast-enhanced CT images to 3D images, and the RTPV was clearly visualized as it appeared in the operative view in the supine position (Fig. 2). Surgery was performed 4 weeks after the end of neoadjuvant chemotherapy. Thoracoscopic esophagectomy with three-field lymphadenectomy via the right thoracic approach was conducted in the prone position using 6 ports. We synchronized the surgical image and the 3D image on the monitor side-by-side for virtual navigation and the precise location of the RTPV was recognized during surgery.
SCLN dissection started from dissection of the posterior plane of the pericardium membrane. This plane continued to the anterior side of the SCLNs, reaching the cartilage of the tracheal bifurcation and the left main bronchus by recognizing the exact plane and expanding to the cranial and left side. Careful spreading of this released layer to the right revealed the rise of the RTPV embedded in the SCLNs (Fig. 3). Next, the dissection plane was switched to the membranous region of the right main bronchus, exposing the RTPV slightly from the distal side, while preserving the right bronchial artery and the pulmonary branch of the vagus nerve (Fig. 4). Finally, the fixation with the right main bronchus was dissected from the caudal side of the right main bronchus toward the direction of the inferior tracheal bifurcation to complete SCLN dissection for radical esophagectomy without damaging the RTPV (Fig. 5). After the thoracoscopic procedure, we reconstructed the gastric tube via a retrosternal route and hand-sewn anastomosis was performed at the left neck [4]. The operative time was 360 min, and the operative blood loss was approximately 30 mL. The patient recovered without complications and was discharged on the 21st day after surgery, although it took time for rehabilitation of muscle weakness.
Intraoperative findings and schematic illustration. The first step in subcarinal lymph node (SCLN) dissection. Dissect the posterior plane of the pericardium membrane and identify the rise of the right top pulmonary vein (RTPV) after it reaches the aspect of the left main bronchus (red dot arrow in the schematic illustration)
Discussion and conclusions
RTPVs are mainly reported by radiologists, cardiologists, and surgeons. Webb, a radiologist, first reported this anomalous vein using 2-dimensional CT [5]. Since atrial fibrillation is caused by electrical activity originating from the pulmonary veins, an accurate understanding of the pulmonary vein anatomy is important for catheter ablation therapy and has been reported from many Western countries [6,7,8]. In our review of the relevant literature, the incidence of RTPV ranged from 0.28 to 9.3%. Inflow sites included the right superior pulmonary vein (RSPV), the right inferior pulmonary vein (RIPV), the LA, and the V6, with the RSPV being relatively common and the V6 being very rare (Table 1). The location of the RTPV in relation to the right bronchus is mostly in the right intermediate bronchus. Cases such as ours, in which the RTPV runs dorsal to the right main bronchus, are very rare. Akiba et al. categorized the RTPV into six types based on their inflow site and route and reported that most types cross the intermediate bronchus and drain into the LA or pulmonary vein [9]. On the other hand, Miyamoto et al. classified the RTPV into four types based on the inflow site and reported that the type that drained into the inferior pulmonary vein was the most common [10]. Thoracic surgeons should be aware of these classifications and their frequency when performing radical esophagectomy, in which subcarinal lymph node dissection is mandatory.
Only 5 case reports in the literature have described the association of RTPV and SCLN dissection in esophagectomy [11, 15,16,17,18] (Table 2). All the cases, including ours, were reported from Japan, where radical esophagectomy with three-field lymphadenectomy is considered a standard procedure. The operative methods included open thoracotomy, thoracoscopy, and laparoscopic transhiatal approach, and—in all cases—the RTPV could be preserved during SCLN dissection. In thoracoscopic esophagectomy, it has been reported that the prone position is better for securing a good surgical field of view to identify the RTPV because the posterior upper lobe segment (S2) is located in the dorsal side of the right upper lobe [18]. It has been reported that retrosternal reconstruction may be a better method to avoid damaging the RTPV while pulling up the gastric tube [16]; we therefore chose this route. In addition, an increased incidence of incomplete fissure and displaced bronchus (DB) has been reported in patients with RTPV [14]. It is important to recognize the presence of the RTPV preoperatively because DB may lead to difficulty during differential lung ventilation and can lead to bronchial and vascular injury [19]. Preoperative simulation and intraoperative navigation with 3D images, which can be freely rotated and interactively visualized from any angle, are useful methods to enhance the surgeon’s understanding of the anatomy [20,21,22]. The use of 3D imaging enabled the preoperative diagnosis of three cases, including the present case.
An important step in SCLN dissection in thoracoscopic esophagectomy is to recognize the posterior plane of the pericardium and release the ventral fixation of the SCLNs to the free space at the back side. This procedure is important, even in the RTPV cases. After confirming the rise of the RTPV, careful encirclement of the RTPV then results in mesenterization of the SCLN, leaving only its fixation to the right main bronchus.
In our review of the relevant literature, the mean vascular diameter was 7.0 mm at the maximum and 2.2 ± 0.72 mm at the minimum (Table 1). The diameter of the RTPV may be correlated with the amount of venous blood flow from the right upper lobe (S2) [12]. If the RTPV is injured, hemostasis is required in the narrow surgical field due to the massive blood flow from the LA or pulmonary vein [11] and may cause cardiac tamponade [15]. It is also reported that if the large RTPV is ligated, the RTPV should be reconstructed or the S2 should be resected because it is considered to drain the entire venous flow from the S2, which may cause congestion of the S2 [15]. On the other hand, a case has been reported in which the RTPV was ligated and cut during right superior segmentectomy [13]. Although the article did not describe the diameter of the RTPV, no serious complications occurred. It was also reported that no symptoms suggestive of upper lobe congestion occurred after ligation if the RTPV was 4.5 mm or smaller [10]. Based on our review of the relevant literature, an RTPV larger than 4.5 mm should be noted in order to prevent injury and ligation should be avoided. The preoperative recognition of this abnormal vessel using 3D imaging was very useful for radical SCLN dissection during thoracoscopic esophagectomy.
Availability of data and materials
Not applicable.
Abbreviations
- RTPV:
-
Right top pulmonary vein
- SCLN:
-
Subcarinal lymph nodes
- CT:
-
Computed tomography
- V2 :
-
Branch of right posterior segmental vein
- LA:
-
Left atrium
- 3D:
-
Three-dimensional
- DICOM:
-
Digital Imaging and Communication in Medicine
- RSPV:
-
Right superior pulmonary vein
- RIPV:
-
Right inferior pulmonary vein
- S2 :
-
Posterior upper lobe segment
- DB:
-
Displaced bronchus
References
Ando N, Ozawa S, Kitagawa Y, Shinozawa Y, Kitajima M. Improvement in the results of surgical treatment of advanced squamous esophageal carcinoma during 15 consecutive years. Ann Surg. 2000;232(2):225–32.
Tanaka Y, Yoshida K, Yamada A, Tanahashi T, Okumura N, Matsuhashi N, et al. Phase II trial of biweekly docetaxel, cisplatin, and 5-fluorouracil chemotherapy for advanced esophageal squamous cell carcinoma. Cancer Chemother Pharmacol. 2016;77(6):1143–52.
Tanaka Y, Ueno T, Yoshida N, Akutsu Y, Takeuchi H, Baba H, et al. The effect of an elemental diet on oral mucositis of esophageal cancer patients treated with DCF chemotherapy: a multi-center prospective feasibility study (EPOC study). Esophagus. 2018;15(4):239–48.
Yoshida K, Tanaka Y, Imai T, Sato Y, Hatanaka Y, Suetsugu T, et al. Subtotal stomach in esophageal reconstruction surgery achieves an anastomotic leakage rate of less than 1%. Ann Gastroenterol Surg. 2020;4(4):422–32.
Webb WR, Hirji M, Gamsu G. Posterior wall of the bronchus intermedius: radiographic-CT correlation. AJR Am J Roentgenol. 1984;142(5):907–11.
Lickfett L, Kato R, Tandri H, Jayam V, Vasamreddy CR, Dickfeld T, et al. Characterization of a new pulmonary vein variant using magnetic resonance angiography: incidence, imaging, and interventional implications of the “right top pulmonary vein.” J Cardiovasc Electrophysiol. 2004;15(5):538–43.
Weerasooriya R, Lim KT, Murray C. Right top pulmonary vein anomaly. J Cardiovasc Electrophysiol. 2005;16(12):1390.
Shi Y, Mi S, Shi Y, Wang H, Li J, Yu B, et al. Evaluation of pulmonary vein anatomy using 256-slice computed tomography. Turk J Med Sci. 2017;47(5):1526–34.
Akiba T, Morikawa T, Inagaki T, Nakada T, Ohki T. A new classification for right top pulmonary vein. Ann Thorac Surg. 2013;95(4):1227–30.
Miyamoto N, Yoshida M, Takashima M, Matsumoto D, Kawakita N, Tsuboi M, et al. Classifying the destination of right top pulmonary vein in 31 clinical cases. Gen Thorac Cardiovasc Surg. 2021;69(8):1192–5.
Matsubara T. Rare but dangerous anomaly of the right pulmonary vein in subcarinal dissection. Ann Thorac Surg. 2003;75(3):1026.
Arslan G, Dincer E, Kabaalioglu A, Ozkaynak C. Right top pulmonary vein: evaluation with 64 section multidetector computed tomography. Eur J Radiol. 2008;67(2):300–3.
Yamada S, Suga A, Inoue Y, Iwazaki M. Importance of preoperative assessment of pulmonary venous anomaly for safe video-assisted lobectomy. Interact Cardiovasc Thorac Surg. 2010;10(6):851–4.
Yaginuma H, Takao K, Umeda M. Right top pulmonary veins associated with lung incomplete fissure and displaced bronchus: a retrospective study using multidetector computed tomography. Gen Thorac Cardiovasc Surg. 2021;69(2):290–6.
Fujiwara Y, Osugi H, Lee S, Kishida S, Hayashi R, Matsuda Y, et al. Attention to anomalies of the right pulmonary vein in subcarinal lymph node dissection in radical esophagectomy for cancer. Esophagus. 2015;12(3):309–11 [in Japanese].
Shiozaki A, Fujiwara H, Konishi H, Kosuga T, Komatsu S, Ichikawa D, et al. Successful subcarinal dissection using a laparoscopic transhiatal approach for esophageal cancer with an anomalous pulmonary vein. Gen Thorac Cardiovasc Surg. 2016;64(4):239–42.
Onodera Y, Taniyama Y, Sakurai T, Hikage M, Sato C, Takaya K, et al. Thoracoscopic esophagectomy with subcarinal lymph node dissection in the prone position for esophageal cancer with a right superior pulmonary vein anomaly: a case report. Surg Case Rep. 2019;5(1):6.
Matsubara T, Hirahara N, Zotani H, Tabara N, Tabara H, Tajima Y. Three-dimensional computed tomography image-oriented successful thoracoscopic subtotal esophagectomy for an esophageal cancer patient with an anomalous right superior pulmonary vein: a case report. Int J Surg Case Rep. 2020;76:178–82.
Yoshimura T, Ueda KI, Kakinuma A, Nakata Y. Difficulty in placement of a left-sided double-lumen tube due to aberrant tracheobronchial anatomy. J Clin Anesth. 2013;25(5):413–6.
Sato Y, Sugimoto M, Tanaka Y, Suetsugu T, Imai T, Hatanaka Y, et al. Holographic image-guided thoracoscopic surgery: possibility of usefulness for esophageal cancer patients with abnormal artery. Esophagus. 2020;17(4):508–11.
Sato Y, Matsuhashi N, Sugie Y, Kuno M, Kiyama S, Tanaka Y, et al. Total laparoscopic resection by medial-retroperitoneal approach using virtual navigation: two case reports of primary retroperitoneal schwannoma. World J Surg Oncol. 2022;20(1):3.
Matsuhashi N, Sato Y, Tajima JY, Kiyama S, Takahashi T, Kuno M, et al. Evaluation of the SYNAPSE VINCENT for lateral lymph node dissection in rectal cancer with robotic surgery: a preliminary report. World J Surg Oncol. 2022;20(1):56.
Acknowledgements
We thank Rise Japan LLC for editing the English language of this manuscript.
Funding
Funding information is not applicable.
Author information
Authors and Affiliations
Contributions
YS drafted the manuscript. YT, SO, and ME performed the operation. NO, NM, TT, TS, and KY provided academic advice. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This case report was approved by the ethics committee of Gifu University School of Medicine.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the patient’s written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sato, Y., Tanaka, Y., Ohno, S. et al. Right top pulmonary vein is a venous anomaly of which surgeons should be aware in subcarinal dissection for thoracoscopic esophagectomy: a case report and literature review. World J Surg Onc 20, 160 (2022). https://doi.org/10.1186/s12957-022-02635-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02635-w