Abstract
Background
The objective of this study is to analyze the treatment outcome and secondary reactions in 98 patients with stage I–III cervical carcinoma who underwent postoperative radiotherapy.
Methods
From 2006 to 2014, 98 patients with stage I–III cervical carcinoma were treated with postoperative radiotherapy. The major histological type, found in 92.86% of the patients (91 cases), was squamous cell carcinoma. Patients were staged according to the 2002 TNM guidelines. The postoperative radiotherapy methods included two-field irradiation (16 patients, 16.32%), four-field box irradiation (16 patients, 16.32%), and intensity-modulated radiotherapy (IMRT; 66 patients, 67.36%). The survival rates were represented using Kaplan-Meier curves, and prognosis analyses were performed using Cox multivariate analyses.
Results
The 5-year overall survival and progression-free survival rates were 82.0 and 76.0%, respectively. Only one patient (1.02%) developed a grade 3 acute radiation enteritis, while grade 3 and 4 myelosuppression was noted in 17 patients (17.35%) and one patient (1.02%), respectively. Multivariate analyses showed that anemia before radiotherapy and tumor size were predictors of the OS (P = 0.008, P = 0.045) rates.
Conclusions
Postoperative radiotherapy for patients with risk factors of cervical cancer procured good efficacy levels with mild side effects. Anemia and tumor size were important OS predictors.
Similar content being viewed by others
Background
As the third most frequent cancer among women worldwide, cervical cancer is the fourth leading cause of cancer deaths in women [1]. According to the global cancer statistics of 2012, 528,000 new cases of cervical cancer were diagnosed each year and 266,000 patients died just in 2012 [2]. According to previous reports, most of the cervical cancer patients in the early stage (IB to IIA) who have accepted proper treatment experienced positive outcome, with only 10 to 15% of the patients with risk factors experiencing recurrence [3]. Therefore, it is very important for cervical cancer patients to receive timely, accurate diagnosis and appropriate treatment to reduce the chances of recurrence.
The mechanism of action of cisplatin involves the formation of platinum-DNA adducts. The mechanisms underlying the interaction between chemotherapy and radiotherapy may include inhibition of the tumor’s impaired damage repair systems and an increase in the radiosensitivity of hypoxic cells. Compliance with treatment is very important for local control and overall survival (OS) in patients with cervical carcinoma.
Adjuvant chemoradiotherapy has been shown to improve the progression-free and overall survival outcome for patients with positive surgical margins, positive lymph nodes, or involvement of the parametrium [4]. Radiotherapy (RT), when delivered in a postoperative setting, has been associated with an increased risk of treatment-related toxicity, including gastrointestinal (GI), genitourinary, and lymphatic system toxicities compared with patients undergoing RT alone [5]. This study was conducted to evaluate the outcome and the prognostic factors of postoperative cervical cancer after concurrent chemoradiotherapy (CCRT).
Methods
The present study retrospectively analyzes previous clinical trial results involving patients with cervical cancer who had undergone postoperative radiotherapy in the Radiation Oncology Department of the Tai Zhou Central Hospital. All patients had signed informed consent prior to entering the trials.
Patient population
All the materials were obtained with agreement of patients and signed informed consent. The usage of human materials for analysis was approved by the ethical committee of Tai Zhou Central Hospital.
A total of 98 patients who underwent surgical resection for cervical cancer with at least one high-risk factor, such as primary tumor diameter ≥ 40 mm, deep invasion, lymphovascular space invasion (LVSI), and so on, were enrolled in this study between 2006 and 2014. The age of enrolled patients ranged from 29 to 76 years old, the mean age being 52. Postoperative pathological staging was performed according to the 2002 guidelines of the Federation International of Gynecology and Obstetrics (FIGO).
Evaluation
Postoperative radiotherapy was performed approximately 4 weeks after radical surgery. Prior to the treatment protocol, each patient underwent physical, laboratory, and radiological examinations. Laboratory examinations included a complete blood cell count, measurement of liver and renal functions, and electrocardiography. All of the abovementioned indexes met the radiotherapy standard before the start of the treatment.
Treatments
Radiotherapy
External whole pelvis irradiation using a 6- or 15-MV photon beam was performed with a dose of 1.8 Gy per fraction five times per week for a total dose of 45 Gy. Of the 98 patients, 16 were irradiated using the anteroposterior parallel opposing technique, 16 with four-field box irradiation, and 66 with intensity-modulated radiotherapy (IMRT).
Chemotherapy
Of the 98 patients, 71 underwent CCRT, which was given according to one of the three following cisplatin-based regimens: (i) weekly cisplatin (40 mg/m2) in 66 patients, (ii) weekly nedaplatin (35 mg/m2) in two patients, and (iii) carboplatin (AUC = 2) plus paclitaxel (135 mg/m2) every 3 weeks in three patients.
Toxicity
Clinical data regarding treatment-related complications were also collected. Complications occurring within 90 days from starting the primary treatment were considered as acute, and those occurring later than 90 days were considered as late complications. The severity of acute complications was classified according to the NCI Common Terminology Criteria for Adverse Events, Version 2.0. Late complications were graded according to the Radiation Therapy Oncology Group (RTOG) Late Radiation Morbidity Scoring Scheme [6].
Follow-up evaluations
After treatment completion, the patient’s follow-ups were scheduled at 1 month, then every 3 months for the first 2 years, and every 6 months thereafter. Follow-ups included a physical examination, tumor marker detection, and pelvic imaging. Central or parametrial pelvic failure was defined as disease persisting or recurring in the pelvis. Distant failure was defined as a disease occurring outside of the pelvis, including the paraaortic lymph nodes.
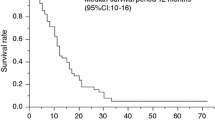
Statistical analysis
OS and progression-free survival (PFS) analyses were performed using the Kaplan–Meier method. Differences in survival were compared using the log-rank statistical test. Survival prognostic factor analyses were performed using the Cox regression method. Hazard ratios were given with 95% confidence intervals (95% CI). SPSS software 22.0 was used for statistical analyses. A P value < 0.05 was considered statistically significant.
Results
Patient characteristics
The patients and tumor-associated characteristics were summarized in Table 1. Seven patients (7.14%) were older than 70 years old. The major histological subtype of the tumors was squamous cell carcinoma (92.86%). The distribution of TNM stage among the patients was as follows: stage I, 32.65%; stage II, 29.59%; and stage III, 37.76%. In addition, 43.88% of the patients presented bulky tumors (larger or equal to 4 cm), 37.76% of the patients were lymph-node-positive, and 27.55% were anemic before the radiotherapy.
Survival
All patients completed the radiotherapy treatment as planned. More than three cycles of weekly cisplatin were administered to 62 patients, and nedaplatin was administered to two patients. Two cycles of tri-weekly chemotherapeutic agents in combination were administered to two patients. In the presence of grade 3 myelosuppression, concurrent chemotherapy was suspended and the whole treatment was delayed while maintaining supportive care. After resolution, the chemotherapeutic agent dosage was reduced by 20% in the next cycle. In case of hepatic or renal toxicity, chemotherapy was suspended.
The median follow-up time was 37 months (range 6–118 months). At the time of analysis, 80 patients were alive without evidence of disease and five patients were alive with disease and 12 patients died of cervical cancer and one patient died of another cause. The 5-year OS and PFS rates were 82.0 and 76.0%, respectively (Fig. 1).
No significant correlation with OS was identified for TNM stage, pathological classification, age, lymphovascular space invasion (LVSI), or deep stromal invasion. However, anemia was identified as a significant unfavorable OS factor (P = 0.00, Fig. 2), as well as lymph node (P = 0.04, Fig. 3) and tumor size (P = 0.00, Fig. 4). Similar correlation results were obtained for PFS (Table 2). We examined the aforementioned significant variables using multivariate analyses. Anemia and tumor size were also identified as significantly unfavorable factors for OS (P = 0.008, P = 0.045) (Table 3).
Acute toxicity
The detailed acute toxicities for the entire study population (n = 98) are listed in Table 4. The incidence of acute grade 3 rectal toxicity was of 1.02% (one patient). No grade 4 gastrointestinal toxicity occurred. The incidences of acute grade 3 and 4 hematologic toxicity were 17.35 and 1.02%, respectively. Additionally, one case of acute grade 3 bladder toxicity and two cases of acute grade 3 skin toxicity were identified.
Failure rate
At the time of analysis, treatment failure was observed in 18 patients (18.37%), including 10 patients 55.56(%) with pelvic recurrence, four patients (22.22%) with postoperative stump recurrence, two patients (11.11%) with lung metastasis, and one patient (5.56%) with brain metastasis while one patient (5.56%) died of adhesions. The time to recurrence ranged from 5.2 to 26.7 months (median of 11.3 months). Ten patients (10.20%) relapsed within 1 year of radiotherapy start, accounting for 55.56% of all treatment failures.
Discussion
The poor prognosis factors for operable cervical cancer include positive margins, deep invasion, larger tumors, LVSI, and lymph node metastasis [7,8,9,10,11,12]. The results of this study showed that the 5-year OS and PFS were 82.0 and 76.0%, respectively. The frequency of grade 3 or more adverse reactions caused by the radiation was low. Furthermore, in patients for whom the overall therapeutic effect was satisfactory, there was no unacceptable side effect.
A lot of research on postoperative radiotherapy for cervical cancer worldwide has focused on the benefits of adjuvant radiotherapy, radiotherapy indications, and comprehensive radiotherapy and chemotherapy. Several of the early studies about adjuvant radiotherapy or chemoradiotherapy for cervical cancer revealed that postoperative radiotherapy or chemoradiotherapy could reduce the risk of tumor recurrence. In a phase III clinical study named GOG92, which enrolled 277 patients with multiple risk factors, 137 patients were given radiotherapy with 46 Gy (23 F) or 50.4 Gy (28 F), and the others were followed up regularly. The study found a significant reduction in relapse within the radiotherapy group (HR = 0.54, 90% CI 0.35–0.81, p = 0.007) and a decreased risk of death (HR = 0.58, 90% CI 0.40–0.85, p = 0.009). The GOG109 American study [4] enrolled 243 stage IA2, IB, and IIA cervical cancer patients who were randomly divided into two groups: 127 patients received chemoradiotherapy and 116 received radiotherapy alone. This study reported significant differences in the relapse and overall survival rates between the two groups (P = 0.003 and P = 0.007, respectively). Postoperative chemoradiotherapy reduced the 4-year PFS and OS by 17 and 10%, respectively, compared with the radiotherapy alone group. Song et al. [13] enrolled 110 cervical cancer patients who were divided into three groups: radiotherapy (1990–1999), radiotherapy (2000–2010), and chemoradiotherapy (2000–2010). They found that chemoradiotherapy reduced local recurrence (P = 0.012) and distant metastasis (P = 0.027).
Previous reviews have strongly suggested that concurrent chemotherapy and radiotherapy (CCRT) improves the OS and PFS rates in cervical cancer patients, regardless of whether platinum-based chemotherapeutic agents are used, with an absolute benefit of 10 and 13%, respectively [14, 15]. The National Comprehensive Cancer Network (NCCN) has established CCRT as the standard of treatment for cervical cancer in patients with high-risk factors. Based on previous studies [1, 3,4,5,6, 16], we used cisplatin alone in most of the patients enrolled in this study, totaling 71 cases (72.45%) with CCRT. However, the 5-year OS and PFS rates were lower than in previous studies. This difference may be attributable to the smaller sample size of our study, especially for the low number of patients followed beyond 5 years.
In this study, the age of the enrolled patients ranged from 29 to 76 years, with a median age of 52 years. It has been reported that patients younger than 35 years old were more susceptible to local recurrence or distant metastasis [17]. Kastritis [18] divided 218 patients into three groups according to age as follows: younger than 35 years old, between 35 and 70 years old, and older than 70 years old. They found that the median survival time in the younger group, median group, and older group was 9 months (95% CI 5.8–12), 14.5 months (95% CI 11–18), and 10 months (95% CI 6.9–13, P = 0.004), respectively. However, in our study, age was not identified as a prognostic factor for OS and PFS, possibly because of the small number of patients in the younger age group. Future studies in larger cohorts of patients will be necessary to validate this question.
Histology, FIGO stage, and deep stromal invasion were previously reported as prognostic factors for cervical cancer patients treated with RT [19,20,21]. In contrast, our study showed that these parameters did not affect the OS and PFS rates, which may be associated with the lower number of positive cases. Recently, perineural invasion (PNI) has attracted attention as a new prognostic factor in cancer patients. Therefore, we aimed to investigate the prognostic value of PNI in patients with cervical cancer. Cho et al. [22] showed that the significance of PNI as an independent predictor for prognosis was limited but was significantly associated with other prognostic factors. We did not reach the same conclusion with our patient cohort.
Lymph node status has been reported as a prognostic factor for cervical cancer [23]. Likewise, our study showed that lymph node status was a prognostic factor of OS (P = 0.04) and PFS (P = 0.02) by univariate analyses. However, multivariate analyses did not yield the same result. Regarding tumor size, a previous study [24] reported that tumor diameter was one of the main factors impacting local control by radiotherapy and prognosis. Likewise, we obtained a similar result of OS.
The lack of cellular oxygen is a known factor influencing the effects of radiation. Consequently, anemia may decrease tumor sensitivity to CCRT. Lee [25] found that anemia was an important indicator of poor prognosis or a sign of advanced disease, especially in pelvic tumor patients (P < 0.01). A retrospective analysis of 2454 cases of cervical cancer divided the patients into three groups according to their hemoglobin levels (9, 10, and 12 g/dl) based on the data obtained before and during the treatment. The researchers found that anemia was associated with disease recurrence, metastasis, and disease-specific survival rates (P < 0.001) [26]. Our study showed that anemic patients had significantly lower OS and PFS rates (P = 0.00 and P = 0.01, respectively). The same outcome was obtained using multivariate analyses (P = 0.008 and P = 0.048, respectively). Therefore, correcting an anemic condition before radiotherapy may improve OS and PFS.
The incidence of lung metastasis from cervical cancer is low, with an average incidence of 2.1–6.1% [27]. Ki [28] et al. retrospectively analyzed 56 cases of cervical cancer with lung metastases. They found that the median survival time was 12 months and that the average survival time was 40.7 months for patients with less than three metastases and 25 months for the others (P < 0.05). In our study, for patients who developed lung metastasis, the metastases appeared 5 months after the CCRT, followed by death 8 months later, which was significantly shorter than in the abovementioned report in terms of median survival time.
Blood metastases with cervical cancer are mainly found in the liver, lungs, and bones and rarely in the brain [29], which was reported to occur with an incidence of 0.4 to 1.2% [30]. Brain metastasis usually indicates a poor prognosis. Sato [31] reported the case of a cervical cancer patient who was diagnosed with brain metastases as the first symptom. Although the patient received CCRT, lung and liver metastasis rapidly appeared. The patient died 7 months after the brain metastases were identified. A retrospective analysis of 11 cases of cervical cancer patients with brain metastases showed that the small cell type was prone to metastasize to the lungs, which was a risk factor for cervical cancer brain metastases [32]. One patient developed brain metastases 11 months after the postoperative CCRT and died 2 months later.
Several studies have reported adverse reactions following postoperative radiotherapy. The frequency of these reactions is slowly declining, especially since the development of IMRT. Pu et al. [33] found a low incidence of approximately 5.6% of grade III and IV radiotherapy side effects in 285 cervical cancer patients who received CCRT. In our study, grade III and IV acute radiation enteritis was present in 1.02% of the patients, and only one patient died of adhesions. The incidence of grade I and II myelosuppression was 21.42 and 37.36%, respectively, and only one patient developed grade IV myelosuppression, which was found to be a symptom of the treatment. Similar to the above findings, we found 12 cases with more than three types of adverse reaction, accounting for 12.24% of the cases.
Some limitations of our study need to be addressed. First, the sample size was relatively small, and the follow-up time was slightly short (median of 37 months). In addition, because of its retrospective nature, potential important confounding biases might have been disregarded in the analysis, such as the selection bias introduced by the surgeons who determined which patients should be considered for CCRT. Moreover, the surgical and radiological techniques or histopathological diagnosis methods might have changed during the study period duration, which could have influenced our results. These factors can only be eliminated in a prospective randomized, controlled study.
Conclusions
The clinical outcome from alternating chemoradiotherapy for high-risk cervical cancer patients, especially in those with highly advanced nodal disease, is promising in terms of both the sufficient efficacy level and the acceptably low toxicity level. However, perineural invasion was identified as another factor of poor prognosis, which should capture sufficient attention in the future.
Abbreviations
- CCRT:
-
Concurrent chemotherapy and radiotherapy
- LNM:
-
Lymph node metastasis
- PNI:
-
Perineural invasion
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
J. Ferlay, I. Soerjomataram, R. Dikshit, et al.Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012, Int. J.Cancer 136 (2015) E359-E386.
Ohara K, Sugahara S, Kagei K, Hata M, Igaki H, Tokuuye K, et al. Retrospective comparison of clinical outcome between radiotherapy alone and surgery plus postoperative radiotherapy in the treatment of stages IB-IIB cervical squamous cell carcinoma. Radiat Med. 2004;22:42–8.
Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000;18:1606–13.
Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997;350:535–40.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31:1341–6.
Boyce J, Fruchter RG, Nicastri AD, Ambiavagar PC, Reinis MS, Nelson JH. Prognostic factors in stage I carcinoma of the cervix. Gynecol Oncol. 1981;12:154–65.
Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective surgical pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a gynecologic oncology group study. Gynecol Oncol. 1990;38:352–7.
Fuller AF Jr, Elliott N, Kosloff C, Hoskins WJ, Lewis JL. Determinants of increased risk for recurrence in patients undergoing radical hysterectomy for stage IB and IIA carcinoma of the cervix. Gynecol Oncol. 1989;33:34–9.
Chung CK, Nahhas WA, Stryker JA, Curry SL, Abt AB, Mortel R. Analysis of factors contributing to treatment failures in stages IB and IIA carcinoma of the cervix. Am J Obstet Gynecol. 1980;138:550–6.
Samlal RA, van der Velden J, Schilthuis MS, González González D, Ten Kate FJ, et al. Identification of high-risk groups among node-positive patients with stage IB and IIA cervical carcinoma. Gynecol Oncol. 1997;64:463–7.
Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach L, et al. A phase III randomized trial of postoperative pelvic irradiation in stage IB cervical carcinoma with poor prognostic features:follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006;65:169–76.
Song S, Song C, Kim HJ, HG W, Kim JH, Park NH, et al. 20 year experience of postoperative radiotherapy in IB-IIA cervical cancer patients with intermediate risk factors: impact of treatment period and concurrent chemotherapy. Gynecol Oncol. 2012;124:63–7.
Pearcey R, Miao Q, Kong W, Zhang SJ, Mackillop WJ. Impact of adoption of chemoradiotherapy on the outcome of cervical cancer in Ontario: results of a population based cohort study. J Clin Oncol. 2007;25:2383–8.
Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: a systematic review and meta-analysis of individual patient data from 18 randomized trials. J Clin Oncol. 2008;26:5802–12.
Choi IJ, Cha MS, Park ES, Han MS, Choi Y, Je GH, et al. The efficacy of concurrent cisplatin and 5-flurouracil chemotherapy and radiation therapy for locally advanced cancer of the uterine cervix. J Gynecol Oncol. 2008;19:129–34.
Wang J, Wang T, Yang YY, Chai YL, Shi F, Liu ZI. Patient age, tumor appearance and tumor size are risk factors for early recurrence of cervical cancer. Mol Clin Oncol. 2015;3:363–6.
Kastritis E, Bamias A, Bozas G, Koutsoukou V, Voulgaris Z, Vlahos G, et al. The impact of age in the outcome of patients with advanced or recurrent cervical cancer after platinum-based chemotherapy. Gynecol Oncol. 2007;104:372–6.
Kasuya G, Ogawa K, Iraha S, Nagai Y, Hirakawa M, Toita T, et al. Postoperative radiotherapy for uterine cervical cancer: impact of lymph node and histological type on survival. Anticancer Res. 2013;33:2199–204.
Okazawa M, Mabuchi S, Isohashi F, Suzuki O, Yoshioka Y, Sasano T, et al. Impact of the addition of concurrent chemotherapy to pelvic radiotherapy in surgically treated stage IB1-IIB cervical cancer patients with intermediate-risk or high-risk factors: a 13-year experience. Int J Gynecol Cancer. 2013;23(3):567–75.
Eifel PJ, Jhingran A, Levenback CF, Tucker S. Predictive value of a proposed subclassification of stages I and II cervical cancer based on clinical tumor diameter. Int J Gynecol Cancer. 2009;19:2–7.
Cho HC, Kim H, Cho HY, Kim K, No JH, Kim YB. Prognostic significance of perineural invasion in cervical cancer. Int J Gynecol Pathol. 2013;32:228–33.
Lee DW, Kim YT, Kim JH, Kim S, Kim SW, Nam EJ. Clinical significance of tumor volume and lymph node involvement assessed by MRI in stage IIB cervical cancer patients treated with concurrent chemoradiation therapy. J Gynecol Oncol. 2010;21:18–23.
Wakayama A, Inamine M, Kudaka W, Nagai Y, Nakamoto T, Ooyama T, et al. Concurrent chemoradiotherapy for non-bulky stage IB/II cervical cancer without pelvic node enlargement. Anticancer Res. 2013;33:5123–6.
Lee HN, Mahajan MK, Das S, Sachdeva J, Tiwana MS. Early hematological effects of chemo-radiation therapy in cancer patients and their pattern of recovery—a prospective single institution study. Gulf J Oncolog. 2015;1:43–51.
Bishop AJ, Allen PK, Klopp AH, Meyer LA, Eifel PJ, et al. Relationship between low hemoglobin levels and outcomes after treatment with radiation or chemoradiation in patients with cervical cancer: has the impact of anemia been overstated? Int J Radiat Oncol Biol Phys. 2015;91:196–205.
Barter JF, Soong SJ, Hatch KD, Orr JW, Shingleton HM. Diagnosis and treatment of pulmonary metastases from cervical carcinoma. Gynecol Oncol. 1990;38:347–51.
Ki EY, Lee KH, Park JS, Hur SY. A clinicopathological review of pulmonary metastasis from uterine cervical cancer. Cancer Res Treat. 2016;48:66–72.
Agrawal A, Kumar A, Sinha AK, Kumar M, Pandey SR, Khaniya S. Intracranial metastases from carcinoma of the cervix. Singap Med J. 2007;48:154–6.
Chura JC, Shukla K, Argenta PA. Brain metastasis from cervical carcinoma. Int J Gynecol Cancer. 2007;17:141–6.
Sato Y, Tanaka K, Kobayashi Y, Shibuya H, Nishigaya Y, Momomura M, et al. Uterine cervical cancer with brain metastasis as the initial site of presentation. J Obstet Gynaecol Res. 2015;41:1145–8.
Hwang JH, Yoo HJ, Lim MC, Seo SS, Kang S, Kim JY, et al. Brain metastasis in patients with uterine cervical cancer. J Obstet Gynaecol Res. 2013;39:287–91.
Pu J, Qin SS, Ding JX, Zhang YZ, Wei G, Yu CH, et al. A randomized controlled study of single-agent cisplatin and radiotherapy versus docetaxel/cisplatin and radiotherapy in high-risk early-stage cervical cancer after radical surgery. J Cancer Res Clin Oncol. 2013;139:703–8.
Acknowledgements
Thanks to my teacher Mr. Ying for the guidance. Thanks to my classmates and colleagues for the help. We are thankful to professor Hu for the study conception and design and to our colleagues for all of their work.
Funding
The collection, analysis, and interpretation of data of the study were supported by the Taizhou science and technology fund (no.111KY07).
Availability of data and materials
The datasets supporting the conclusions of this article are shared.
Author information
Authors and Affiliations
Contributions
SPY designed the research. YM, SP, QLL, WJC, and LQN administered the treatments. YML and SPY analyzed the data. YM wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical committee of Tai Zhou Central Hospital.
Consent for publication
Written informed consent was obtained from the patient for publication of this report and the accompanying images.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liu, YM., Ni, LQ., Wang, SS. et al. Outcome and prognostic factors in cervical cancer patients treated with surgery and concurrent chemoradiotherapy: a retrospective study. World J Surg Onc 16, 18 (2018). https://doi.org/10.1186/s12957-017-1307-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-017-1307-0