Abstract
Background
Granulocyte colony-stimulating factor (G-CSF)-producing esophageal squamous cell carcinoma (ESCC) has been considered to have a poor prognosis. We successfully treated a case of G-CSF-producing ESCC in a 92-year-old woman.
Case presentation
A 92-year-old woman was admitted to our hospital with the complaints of choking while swallowing and dysphagia. Esophagogastroduodenoscopy and contrast-enhanced computed tomography revealed a type 2 esophageal cancer located 26–35 cm from the dental arch, with no distant metastasis. The patient was diagnosed with G-CSF-producing ESCC based on remarkable leukocytosis and high G-CSF levels. The patient underwent radical subtotal esophagectomy. Subsequently, the level of neutrophils (from 23,500/μL to 5000/μL) and the level of G-CSF (from 131 to <19.5 pg/mL) decreased significantly. Immunohistochemistry analysis of the resected tissue specimen showed positive staining for G-CSF in the cytoplasm of the tumor cells. Although the patient developed aspiration pneumonitis, after antibiotic treatment, she promptly recovered and was discharged.
Conclusions
Herein, we describe a case of successfully treated G-CSF-producing ESCC in a 92-year-old woman. Precise detection and safely performed immediate radical operation are considered essential to achieve a good clinical course.
Similar content being viewed by others
Background
In addition to the mass tumor effects, granulocyte colony-stimulating factor (G-CSF)-producing tumors display additional signs and symptoms of inflammation caused by G-CSF-producing malignant cells [1]. There have been a relatively high number of reports on G-CSF-producing lung carcinoma; however, reports on G-CSF-producing esophageal squamous cell carcinoma (ESCC) have been scarce.
With the aging of the population, the number of oldest old patients with cancer comorbidities has been increasing [2]. Therefore, effort should be made to determine the effectiveness of each treatment plan.
We report a very rare case of a 92-year-old woman who was promptly diagnosed with G-CSF-producing ESCC and successfully underwent surgical treatment.
Case presentation
A 92-year-old woman had a major complaint of choking when swallowing or dysphagia. The patient had been healthy and had no particular medical history besides cataract surgery. She had no history of oral medications, smoking, or alcohol. Another physician had previously attended to her was complaint of choking when swallowing. A narrowing of the lumen of the intrathoracic esophagus was detected by esophagogastroduodenoscopy, and the patient was referred to our hospital for detailed examination.
On admission, abnormal symptoms such as fever, anemia, or jaundice were not detected and the performance status was good (score 0 according to the Eastern Cooperative Oncology Group). Laboratory data on admission showed remarkable leukocytosis (leukocytes 23,500/μL, neutrophils 86.1 %, and no blast cells) and slight decrease in the serum albumin (3.5 g/dL) and C-reactive protein (CRP) levels (1.5 mg/dL). The levels of tumor markers, squamous cell carcinoma antigen (SCC-A), and p53 antibody were high (SCC-A, 3.4 ng/mL; p53, 22.2 U/mL). The respiratory functions and electrocardiograms were within normal ranges. However, the renal function was a slight concern.
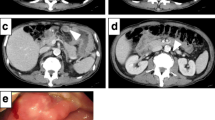
Esophagogastroduodenoscopy revealed a type 2, circumferential cancer of the esophagus, approximately at 26–35 cm from the dental arch (Fig. 1), and the biopsy showed SCC. Contrast-enhanced computed tomography of the chest and abdomen demonstrated circumferential thickening of the wall and narrowing of the lumen of the middle and lower intrathoracic esophagus, and small lymph nodes were detected between the lower mediastinum and paracardiac area. Pleural effusion and ascites or distant metastases were not detected (Fig. 2).
Based on these findings, the patient was diagnosed with T3N0M0, stage IIA (according to the Union for International Cancer Control TNM classification of malignant tumors, 7th edition) ESCC. Furthermore, the laboratory data suggested G-CSF-producing carcinoma with serum G-CSF levels of 131 pg/mL.
Despite her age, the patient had no comorbidities, and most importantly, she consented to a surgical operation. Therefore, we planned to perform esophagectomy. In Japan, the standard treatment for stage IIA esophageal carcinoma is subtotal esophagectomy with three-field lymph node dissection following preoperative chemotherapy [3]. However, considering the age disadvantage, multimodal management of disease with chemotherapy or radiotherapy was not performed.
In fact, the subtotal esophagectomy under the right thoracolaparotomy, right lower partial lobectomy, two-field lymph node dissection (instead of three-field), posterior mediastinal route gastric tube reconstruction, and intra-pleural anastomosis were successfully performed. The operation lasted 4 h and 15 min, and the blood loss was 50 mL. The tumor and the right lobe of the lung were attached; therefore, they were resected en bloc because the tumor was considered infiltrative.
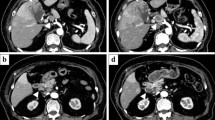
Histopathological examination of the resected specimen revealed that the primary lesion sized 92 × 54 mm was a moderately differentiated squamous cell carcinoma with two lymph node metastases, and it was diagnosed as a stage III tumor (according to the Union for International Cancer Control TNM classification) (Fig. 3a, b). Immunohistochemistry of the resected tissue specimen stained positive for G-CSF in the cytoplasm of the tumor cells (Fig. 3c).
Pathological findings. a Macroscopic examination of the primary lesion of the resected esophagus sized 92 × 54 mm. b Hematoxylin and eosin stains of the resected tissue specimen revealed moderately differentiated squamous cell carcinoma. c Immunohistochemistry of the resected tissue specimen showed positive staining for granulocyte colony-stimulating factor (G-CSF) in the cytoplasm of the tumor cells
After the operation, the patient developed aspiration pneumonitis; however, she promptly recovered with the administration of antibiotics. Three weeks after the operation, the leukocyte counts decreased to 5000/μL and the G-CSF levels to <19.5 pg/mL. Thereafter, the patient exhibited a good clinical course and she was discharged on the 29th postoperative day.
The patient had neutrophilia without any signs of infection or myeloblast genesis before the operation. After esophagectomy, the number of leukocytes and the level of G-CSF had decreased significantly and the presence of G-CSF was confirmed pathologically. Therefore, the patient was definitively confirmed to have a G-CSF-producing tumor.
There have not been any complaints or recurrence, and the patient has remained disease-free from 18 months after the operation until the present day.
Discussion
Robinson first described a G-CSF-producing tumor in 1974 [1], and the number of such cases has been increasing in the recent years. The primary sites of G-CSF cases have been reported as the lung, urinary tract, or the stomach [4–6]; however, reports of G-CSF-producing esophageal carcinoma have been scarce.
G-CSF is a hematopoietic factor produced by the endothelium, macrophages/monocytes, and fibroblasts. It stimulates the bone marrow to produce granulocytes from stem cells and release neutrophils into the bloodstream [7]. It is also produced by the malignant cancer cells. An excess amount of aberrant production causes an inflammatory response such as fever and positive CRP, a kind of leukemoid reaction (leukocytosis >50,000 leukocytes/μL), and paraneoplastic syndrome in clinical oncology. A recombinant form of G-CSF is currently used to prevent infections after chemotherapy or radiological therapy, which causes myelosuppression and neutropenia.
The diagnostic criteria for G-CSF-producing tumors include (1) a marked increase in the leukocyte counts, (2) elevated G-CSF activity, (3) a decrease in leukocyte counts following tumor resection, and (4) the verification of G-CSF production in the tumor [1]. Because all four criteria were fulfilled, we diagnosed the patient with G-CSF-producing ESCC.
Esophageal carcinoma is a disease with a poor prognosis [8]. Furthermore, the prognosis of G-CSF-producing ESCC is considered even poorer (Table 1) [9–18]. All of the cases have been found at rather advanced stage, in 12 cases (including our case), and 9 cases were poor prognosis. The reason might include (1) G-CSF per se having a capacity to expand tumor growth in an autocrine manner, (2) acute renal failure or hyperuricemia (so-called tumor lysis syndrome) by cytolysis of increased neutrophils after chemotherapy, (3) thrombosis by platelet aggregation by G-CSF [19]. The surviving three patients had undergone tumor resection. Furthermore, among the poor prognosis group, the survival period of excised cases was estimated to be longer than that of non-excised cases. From the above, in cases of the G-CSF-producing ESCC, if possible, the complete tumor resection is considered to be important. Since the prognosis of this disease is much poor, if possible, surgery as well, multimodal therapy that combines radiotherapy and/or chemotherapy is considered preferable.
According to Table 1, G-CSF-producing ESCC was male-dominated (83.3 %) and the average age of the 12 patients was 67 years old. These findings were considered to overlap with the population of normal ESCC. Association between leukocyte value, serum G-CSF value, tumor location, tumor stage, histologic grade, and prognosis was not clear. In addition, in one third in these 12 cases, a merger of other organs’ tumor was observed. It is suggested that the characteristic of G-CSF, which was mentioned above, might have influence on tumor growth [19].
In addition, with the aging of the population, the chances that we encounter the oldest old patients are increasing [8]. The appropriate evaluation of overall conditions and the selection of operative method are critical. The operative reports of the elderly are few, and among those cases, the cytoreductive (limited) operations were often chosen [20–22] because of the increase of complications after the operation.
In the present case, the oldest old patient has been alive with a good condition after the operation. In order to improve the quality of life of the oldest old patients, the practical consideration for esophageal carcinoma should be the individualization of therapeutic protocols, tailoring the extent of resection and inclusion or exclusion of preoperative and postoperative procedures. A curative resection with relatively minimal invasion appears to be mandatory for better prognosis with minimal morbidity and mortality in elderly patients.
Conclusions
We described a case of successfully treated G-CSF-producing esophageal squamous cell carcinoma in a 92-year-old woman. We assessed the patient’s will and overall condition and chose the best operative method of radical subtotal esophagectomy and could achieve a good clinical course.
Abbreviations
- CRP:
-
C-reactive protein
- ESCC:
-
Esophageal squamous cell carcinoma
- G-CSF:
-
Granulocyte colony-stimulating factor
- SCC-A:
-
Squamous cell carcinoma antigen
References
Robinson WA. Granulocytosis in neoplasia. Ann NY Acad Sci. 1974;230:212–8.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Yokota T, Ando N, Igaki H, Shinoda M, Kato K, Mizusawa J, Katayama H, Nakamura K, Fukuda H, Kitagawa Y. Prognostic factors in patients receiving neoadjuvant 5-fluorouracil plus cisplatin for advanced esophageal cancer (JCOG9907). Oncology. 2015;89(3):143–51.
Asano S, Urabe A, Okabe T, Sato N, Kondo Y. Demonstration of granulopoietic factor(s) in the plasma of nude mice transplanted with a human lung cancer and in the tumor tissue. Blood. 1977;49(5):845–52.
Yasui H, Sato K, Takeyama Y, Ando A, Kato T, Hashimoto H, Fukui Y, Maeda M, Gonda H, Suzuki R. Granulocyte colony-stimulating factor-producing carcinoma of unknown primary site. Case Rep Oncol. 2014;7(3):780–8.
Obara T, Ito Y, Kodama T, Fujimoto Y, Mizoguchi H, Oshimi K, Takahashi M, Hirayama A. A case of gastric carcinoma associated with excessive granulocytosis. Production of a colony-stimulating factor by the tumor. Cancer. 1985;56(4):782–8.
Metcalf D. The granulocyte-macrophage colony-stimulating factors. Science. 1985;229(4708):16–22.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Watanabe HA, Matsushita H, Matsui H, Komatsu T, Taguchi S, Sata H, Amano N. Esophageal carcinoma with high serum parathyroid hormone-related protein (PTHrP) level. J Gastroenterol. 1999;34(4):510–5.
Ichiishi E, Yoshikawa T, Kogawa T, Yoshida N, Kondo M. Possible paracrine growth of adenocarcinoma of the stomach induced by granulocyte colony stimulating factor produced by squamous cell carcinoma of the oesophagus. Gut. 2000;46(3):432–4.
Matsumoto G, Ise H, Kimura Y, Inoue H, Suzuki N, Ohtani H, Ogawa H, Fukushima K, Matsuno S. Granulocyte-colony stimulating factor-producing esophageal carcinoma: serum level as a marker for monitoring the effects of treatment. Int J Clin Oncol. 2000;5(5):328–33.
Miyuki K, Hiroshi O, Noriko U, Hiroshi H. An autopsy case of esophageal squamous cell carcinoma associated with granulocyte colony-stimulating factor production. Jikeikai Med J. 2002;49(4):191–5.
Komatsu D, Sakurai M, Nakafuji H, Koide N, Morishita H, Nakamura T. Granulocyte colony stimulating factor-producing collision tumor of the gastric cardia. J Gastroenterol. 2003;38(10):1013–5.
Nakata K, Ohtsuka T, Sato S, Tanaka M, Shimonishi T, Mori D, Nakafusa Y, Miyazaki K. Esophageal carcinoma with humoral hypercalcemia and leukocytosis successfully treated by a two-stage operation: report of a case. Esophagus. 2006;3(1):13–7.
Mimatsu K, Oida T, Kano H, Kawasaki A, Amano S. Aggressive progression of granulocyte colony-stimulating factor producing squamous cell carcinoma of the esophagus: case report and literature review. Esophagus. 2008;5(4):205–9.
Tanabe T, Kanda T, Ishihara N, Kosugi S-i, Matsuki A, Watanabe G, Sasamoto R, Hatakeyama K. An esophageal squamous cell carcinoma patient with high serum granulocyte-colony stimulating factor level: report of a case. Esophagus. 2009;6(4):253–8.
Mayanagi S, Niihara M, Goto H, Yokota T, Tabuse H, Yasui H, Ogawa H, Nishimura T, Kusafuka K, Tsubosa Y. Granulocyte colony-stimulating factor-producing esophageal squamous cell carcinoma following chemoradiotherapy and bone marrow transplantation for acute lymphoblastic leukemia. Esophagus. 2013;10(4):258–63.
Shimakawa T, Asaka S, Usuda A, Yamaguchi K, Yoshimatsu K, Shiozawa S, Katsube T, Naritaka Y. Granulocyte-colony stimulating factor (G-CSF)-producing esophageal squamous cell carcinoma: a case report. Int Surg. 2014;99(3):280–5.
Kawachi Y, Watanabe A, Uchida T, Yoshizawa K, Kurooka N, Setsu K. Acute arterial thrombosis due to platelet aggregation in a patient receiving granulocyte colony-stimulating factor. Br J Haematol. 1996;94(2):413–6.
Markar SR, Low DE. Physiology, not chronology, dictates outcomes after esophagectomy for esophageal cancer; outcomes in patients 80 years and older. Ann Surg Oncol. 2013;20(3):1020–6.
Internullo E, Moons J, Nafteux P, Coosemans W, Decker G, De Leyn P, Van Raemdonck D, Lerut T. Outcome after esophagectomy for cancer of the esophagus and GEJ in patients aged over 75 years. Eur J Cardiothorac Surg. 2008;33(6):1096–104.
Morita M, Egashira A, Yoshida R, Ikeda K, Ohgaki K, Shibahara K, Oki E, Sadanaga N, Kakeji Y, Maehara Y. Esophagectomy in patients 80 years of age older with carcinoma of the thoracic esophagus. J Gastroenterol. 2008;43(5):345–51.
Acknowledgements
Not applicable.
Funding
None.
Availability of data and materials
All available data are presented in the case.
Authors’ contributions
All authors have been involved in the management of the patient and in the conception of the manuscript. MK, YY, and YS have been involved in the drafting of the manuscript or its critical revision for important intellectual content. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of the journal.
Ethics approval and consent to participate
We performed this case report in accordance with the Declaration of Helsinki and the Ethics Committee of The University of Tokyo Hospital.
New software
The authors declare that no new software has been used.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kitani, M., Yamagata, Y., Tanabe, A. et al. Radical esophagectomy for a 92-year-old woman with granulocyte colony-stimulating factor-producing esophageal squamous cell carcinoma: a case report. World J Surg Onc 14, 264 (2016). https://doi.org/10.1186/s12957-016-1023-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-016-1023-1