Abstract
Background
There are no definitive criteria for identifying which patients with The International Federation of Gynecology and Obstetrics (FIGO) stage IB cervical cancer will benefit from adjuvant therapy after radical hysterectomy. The aims of this study were to clarify the efficacy of adjuvant therapy and assess complications after radical hysterectomy in patients with FIGO stage IB1 cervical cancer with intermediate risk factors.
Methods
Between January 2005 and December 2009, the medical records of 75 stage IB1 patients’ intermediate risk factors (i.e., tumor size 2–4 cm, lymphovascular involvement, and/or deep stromal invasion >1/2) who underwent radical hysterectomy at six institutions were collected, and these patients were enrolled in this nonrandomized retrospective study. We simplified the criteria of intermediate risk factors as much as possible, as the criteria adopted in some clinical studies are complicated in practice.
Results
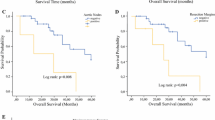
The patients were grouped according to the receipt of adjuvant therapy as follows: 46 patients, no further treatment; 19 patients, external beam radiation treatment, including 9 patients who received brachytherapy; 5 patients, concurrent chemoradiotherapy (CCRT); and 5 patients, chemotherapy (CT). The clinical outcomes and complications in each group were analyzed. After an average follow-up of 82.6 months (range, 24–135 months), only one patient with all three risk factors who received radiotherapy (RT) experienced recurrence. Excluding this patient, the remaining patients who received RT, CCRT, or CT had two or three risk factors. Lymphedema was significantly more common among patients who received RT or CCRT, whereas the incidence of ileus and ureteral obstruction was not different among the treatment groups. However, an unsutured peritoneum increased the risk of ileus.
Conclusions
The findings of this study suggest that RT and CCRT after radical hysterectomy are not beneficial in patients with intermediate risk factors. In particular, RT and CCRT appeared to increase the incidence of lymphedema. A prospective randomized study is needed to verify the findings of this study.
Similar content being viewed by others
Background
Cervical cancer is the fourth most common cancer among women worldwide and the second most diagnosed cancer in developing countries [1]. Radical hysterectomy with pelvic lymphadenectomy has been a primary treatment in women with stage IB cervical cancer, and the procedure is associated with a 5-year survival rate of 87–92 % [2]. Radiotherapy (RT) is a feasible technique that provides similar outcomes as radical hysterectomy [2–4]. Surgery enables pathological examination by surgeons, permitting identification of risk factors for cancer recurrence. In general, patients with parametrial invasion, a positive vaginal margin, or positive pelvic lymph nodes who are diagnosed as being at high risk are assigned to receive adjuvant therapies. By contrast, large tumor size, deep stromal invasion, and lymphovascular invasion are classified as intermediate risk factors, and adjuvant therapy for patients with these risk factors remains controversial. Although the criteria for intermediate risk factors defined by the Gynecologic Oncology Group (GOG) study [5] have been widely accepted, each institution offers adjuvant therapy to patients based on its own protocol. Thus, there is always a problem of interpreting discrepant results between studies because of the different study models. On the contrary, it has been recognized that postoperative RT results in a significant increase in the incidence of adverse events affecting quality of life, such as lymphedema, ileus, and ureteral obstruction [6–8].
The GOG study concluded that pelvic RT after radical hysterectomy significantly improves progression-free survival and benefits patients with histological types of adenocarcinoma and adenosquamous carcinoma [9]. The aims of the current retrospective study were to evaluate the effect of RT and treatment-related morbidity after radical hysterectomy for patients with intermediate risk as defined by simplified criteria.
Methods
Between 2005 and 2009, the medical records of 89 stage IB1 patients with intermediate risk factors (i.e., tumor size 2–4 cm, lymphovascular involvement, and/or deep stromal invasion >1/2) who underwent type III radical hysterectomy as defined by Piver et al. [10] and bilateral pelvic lymphadenectomy were obtained for this retrospective study from six institutions belonging to the Gynecologic Oncology Trial and Investigation Consortium of North Kanto (GOTIC): Gunma University, Tsukuba University, Jichi Medical University, National Defense Medical College, Saitama Medical University International Medical Center, and Tochigi Prefectural Cancer Center. None of the patients had received preoperative treatment such as neoadjuvant chemotherapy (CT) or RT. Informed consent was not obtained from each participant because this was a retrospective study. Instead of that, all participants were given the right to withdraw the use of the data. The protocol of this study was approved based on the necessity of the individual institutions’ ethical committees.
Based on each institution’s criteria, patients received adjuvant therapy, including RT, CT, or concurrent chemoradiotherapy (CCRT). RT consisted of conventional external beam (EBRT) to the pelvis (28–42 Gy) in fractions of 1.8–2.0 Gy for 28–42 days. Nine patients in the RT group also received vaginal brachytherapy (BRA) in fractions of 4–7 Gy for a total dose of 7–21 Gy. In the CCRT group, cisplatin (40 mg/m2) was infused intravenously every week. In the CT group, patients received paclitaxel (175 mg/m2) plus carboplatin (AUC 6) every 3 weeks for 6 cycles.
Data regarding tumor size (MS), histopathological findings, depth of stromal invasion [11], and lymphovascular space invasion (LVSI) are summarized in Table 1. All patients received regular follow-up. During follow-up, complications such as ileus and ureteral obstruction were classified according to the Common Toxicity Criteria. The severity of lymphedema was rated according to the staging system of the International Society of Lymphology as follows: stage 0, a latent or sub-clinical condition in which swelling in not evident; stage 1, temporary visible swelling that can be reduced by elevation of the limb; stage 2, clear pitting and limb elevation cannot reduce tissue swelling; and stage 3, also known as lymphostatic elephantiasis, tissue becomes extremely swollen, leading to skin changes such as acanthosis, fat deposits, and warty overgrowths [12].
Statistically significant differences in the severity of adverse events, namely lymphedema, ileus, and ureteral obstruction, as a result of no further treatment (NFT, n = 46), RT and CCRT (n = 24), or CT (n = 5) were analyzed using the Kruskal-Wallis or chi-squared test. All tests were two-tailed, and a P value <0.05 was considered statistically significant.
The presence or absence of complications was determined, and cross-tabulation was performed when the retroperitoneum was opened or closed during surgery and when RT was or was not administered. In addition, odds ratios and 95 % confidence intervals for the presence or absence of complications were calculated using logistic regression analyses based on whether the retroperitoneum was opened or whether RT was performed.
JMP ver. 9 (SAS Institution Japan Inc., Tokyo, Japan) was used for all analyses.
Results
Eighty-nine patients were enrolled in this retrospective study from six institutions; meanwhile, 14 patients were excluded because of incompatibility with the inclusion criteria and incomplete follow-up data. Overall, the study included 51, 20, and 4 patients with squamous cell carcinoma, adenocarcinoma, and adenosquamous histology, respectively (Table 1). One patient with all three intermediate risk factors who received EBRT and BRA died of a recurrent tumor in the lungs 24 months later. All other patients are alive without recurrence, and they have been followed up for an average of 84.3 months (range, 47–135 months).
Table 2 shows the characteristics of intermediate risk factors in this group of patients. Among the 75 patients, 24 received either RT or CCRT and 5 were treated with CT alone. Only a single patient who had one intermediate risk factor received EBRT and BRA. By contrast, 19/24 (79.2 %) patients who had all three intermediate risk factors as defined in this study received adjuvant therapy.
Lymphedema was observed more frequently in patients who received postoperative RT than in those who did not receive RT or CT (P < 0.001). The risks of ileus and ureteral obstruction were not significantly different between patients who received NFT/CT or RT/CCRT. Other radiation-related adverse effects such as cystitis and proctitis were extremely rare (Table 3). We further assessed the severity of lymphedema associated with RT, finding that more patients who receive RT developed grade 2 or 3 lymphedema (P < 0.001) (Table 4).
Retroperitoneal suturing after lymphadenectomy was also assessed to evaluate the prophylactic effect of an unsutured pelvic peritoneum on lymphedema risk. The overall lymphedema rate was comparable between patients with an unsutured pelvic peritoneum and those with a sutured pelvic peritoneum (Table 5). However, an unsutured pelvic peritoneum was significantly associated with ileus among patients who did not receive adjuvant RT (Fig. 1).
Discussion
The outcome of surgery with or without adjuvant RT in patients with early-stage cervical cancer has been debated by many researchers. In general, RT has been demonstrated to significantly decrease the risk of local recurrence. However, overall survival is not conclusively improved, whereas certain subset analyses illustrated a positive effect of RT on the reduction of recurrence, for example, the GOG 92 study suggested that RT is effective for patients with a combination of deep stromal invasion and large tumor size (≥4 cm) [9]. Tumor size ≥4 cm has been strongly correlated with recurrence [13–17]. As we assumed that tumor size ≥4 cm was a high risk factor even in the intermediate risk group, we excluded patients with tumor diameters ≥4 cm in this study. It is also accepted that stromal invasion by tumors is an important prognostic factor, and a majority of studies evaluated invasion depth via measurements in absolute millimeters or fractions of muscle layer [9, 17]. Stromal invasion in fractional seconds was used in this study because variable thickness in the cervical wall might not reflect the extent of stromal invasion. In addition, measurement in fractional thirds appeared difficult, especially in patients with a thin cervical wall, and it might increase discrepancies because of the multi-institutional nature of the study. Previously, a combination of intermediate risk factors, such as large tumor size, LVSI, and stromal invasion, was associated with incremental recurrence rates of up to 15–20 % [5, 13, 16, 17]. In this study, only one patient (1/24) with a single risk factor received adjuvant RT, whereas 28/51 patients with multiple risk factors received adjuvant therapy (Table 2). However, this study has some limitations, including its retrospective nature and the possible diversity of treatment modalities among institutions, resulting in heterogeneity among the treatment groups. For example, the introduction of CCRT for treating high risk cervical cancer probably influenced some institutions to utilize CCRT, as 4/5 patients who received CCRT had all three risk factors (Table 1), which may result in bias in interpreting the results. In this study, only one patient with all three intermediate risk factors who received RT and BRA died of recurrent tumor in the lungs 24 months later. This finding suggests that adjuvant RT does not benefit patients with intermediate risk factors as defined in this study. These issues can be addressed via a randomized design study in the future.
Another purpose of this study was to assess adverse events associated with RT, as adjuvant RT has long been known to increase complications [18, 19]. Adjuvant CT alone for post-radical hysterectomy patients has been revealed to provide a better postoperative quality of life by eliminating RT-related morbidities such as small-bowel obstruction or leg edema [6, 8], as also supported by our results (Table 3). Based on the small number of cases of ileus and ureteral obstruction, there was no difference between NFT/CT and RT/CCRT, which was consistent with a meta-analysis [11] of two combined trials by Bilek et al. [20] and GOG 92 [9]. Conversely, the incidence of lymphedema was significantly higher and the adverse event was of greater severity for patients who received RT or CCRT (P < 0.001). Several studies indicated that an unsutured peritoneum after pelvic lymphadenectomy reduced the risk of lymphocyst formation [21, 22]. In this study, we assessed whether the incidence of lymphedema improved when the retroperitoneum was left open. In contrast to a previous report suggesting that an unsutured peritoneum significantly reduced the risk of lymphedema [23], this strategy did not provide a significant advantage in avoiding lymphedema in this study (Table 5). Lymphedema is most commonly diagnosed within the first year, but a certain number of patients manifest symptoms in later years [24, 25]. Thus, the possible reason for discrepant results between studies may be attributable to the follow-up duration; specifically, the average observation period was 82.6 months in our study, whereas other studies evaluated patients for 3 years after surgery. Intriguingly, our study demonstrated that an unsutured peritoneum without RT significantly increased the incidence of ileus, whereas there was no difference between an unsutured and sutured peritoneum regarding the risks of lymphedema and ureteral obstruction (Fig. 1).
Conclusions
In the present study, postoperative adjuvant RT significantly increased adverse events for intermediate risk patients as defined in this study. To date, no trial has established a solid consensus regarding RT after surgery for early-stage cervical cancer. Although this retrospective study included a limited number of patients, the results provide useful information for further consideration in the management of patients with intermediate risk cervical cancer.
Abbreviations
BRA, brachytherapy; EBRT, external beam radiation therapy; CCRT, concurrent chemoradiotherapy; CT, chemotherapy; LVSI, lymphovascular space invasion; MS, tumor size; NFT, no further treatment; RT, radiation treatment; SI, stromal invasion
References
Bermudez A, Bhatla N, Leung E. Cancer of the cervix uteri. Int J Gynaecol Obstet. 2015;131 Suppl 2:S88–95.
Gray HJ. Primary management of early stage cervical cancer (IA1-IB) and appropriate selection of adjuvant therapy. J Natl Compr Canc Netw. 2008;6:47–52.
Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, Favini G, Ferri L, Mangioni C. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997;350:535–40.
Peters 3rd WA, Liu PY, Barrett 2nd RJ, Stock RJ, Monk BJ, Berek JS, Souhami L, Grigsby P, Gordon W, Jr., Alberts DS. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000;18:1606–13.
Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: a Gynecologic Oncology Group Study. Gynecol Oncol. 1999;73:177–83.
Takeshima N, Umayahara K, Fujiwara K, Hirai Y, Takizawa K, Hasumi K. Treatment results of adjuvant chemotherapy after radical hysterectomy for intermediate- and high-risk stage IB-IIA cervical cancer. Gynecol Oncol. 2006;103:618–22.
Hosaka M, Watari H, Takeda M, Moriwaki M, Hara Y, Todo Y, Ebina Y, Sakuragi N. Treatment of cervical cancer with adjuvant chemotherapy versus adjuvant radiotherapy after radical hysterectomy and systematic lymphadenectomy. J Obstet Gynaecol Res. 2008;34:552–6.
Lee KB, Lee JM, Ki KD, Lee SK, Park CY, Ha SY. Comparison of adjuvant chemotherapy and radiation in patients with intermediate risk factors after radical surgery in FIGO stage IB-IIA cervical cancer. Int J Gynecol Cancer. 2008;18:1027–31.
Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach LI, Zaino RJ. A phase III randomized trial of postoperative pelvic irradiation in stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006;65:169–76.
Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974;44:265-272.
Rogers L, Siu SS, Luesley D, Bryant A, Dickinson HO. Radiotherapy and chemoradiation after surgery for early cervical cancer. Cochrane Database Syst Rev. 2012;5, CD007583.
International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema. Consensus document of the International Society of Lymphology. Lymphology. 2003;36:84–91.
van der Velden J, Samlal R, Schilthuis MS, Gonzalez DG, ten Kate FJ, Lammes FB. A limited role for adjuvant radiotherapy after the Wertheim/Okabayashi radical hysterectomy for cervical cancer confined to the cervix. Gynecol Oncol. 1999;75:233–7.
Lai CH, Hsueh S, Hong JH, Chang TC, Tseng CJ, Chou HH, Huang KG, Lin JD. Are adenocarcinomas and adenosquamous carcinomas different from squamous carcinomas in stage IB and II cervical cancer patients undergoing primary radical surgery? Int J Gynecol Cancer. 1999;9:28–36.
Tsai CS, Lai CH, Wang CC, Chang JT, Chang TC, Tseng CJ, Hong JH. The prognostic factors for patients with early cervical cancer treated by radical hysterectomy and postoperative radiotherapy. Gynecol Oncol. 1999;75:328–33.
Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1990;38:352–7.
Ryu SY, Kim MH, Nam BH, Lee TS, Song ES, Park CY, Kim JW, Kim YB, Ryu HS, Park SY, et al. Intermediate-risk grouping of cervical cancer patients treated with radical hysterectomy: a Korean Gynecologic Oncology Group study. Br J Cancer. 2014;110:278–85.
Barter JF, Soong SJ, Shingleton HM, Hatch KD, Orr Jr JW. Complications of combined radical hysterectomy-postoperative radiation therapy in women with early stage cervical cancer. Gynecol Oncol. 1989;32:292–6.
Fiorica JV, Roberts WS, Greenberg H, Hoffman MS, LaPolla JP, Cavanagh D. Morbidity and survival patterns in patients after radical hysterectomy and postoperative adjuvant pelvic radiotherapy. Gynecol Oncol. 1990;36:343–7.
Bilek K, Ebeling K, Leitsmann H, Seidel G. Radical pelvic surgery versus radical surgery plus radiotherapy for stage Ib carcinoma of the cervix uteri. Preliminary results of a prospective randomized clinical study. Arch Geschwulstforsch. 1982;52:223–9.
Jensen JK, Lucci 3rd JA, DiSaia PJ, Manetta A, Berman ML. To drain or not to drain: a retrospective study of closed-suction drainage following radical hysterectomy with pelvic lymphadenectomy. Gynecol Oncol. 1993;51:46–9.
Lopes AD, Hall JR, Monaghan JM. Drainage following radical hysterectomy and pelvic lymphadenectomy: dogma or need? Obstet Gynecol. 1995;86:960–3.
Tanaka T, Ohki N, Kojima A, Maeno Y, Miyahara Y, Sudo T, Takekida S, Yamaguchi S, Sasaki H, Nishimura R. Radiotherapy negates the effect of retroperitoneal nonclosure for prevention of lymphedema of the legs following pelvic lymphadenectomy for gynecological malignancies: an analysis from a questionnaire survey. Int J Gynecol Cancer. 2007;17:460–4.
Beesley V, Janda M, Eakin E, Obermair A, Battistutta D. Lymphedema after gynecological cancer treatment: prevalence, correlates, and supportive care needs. Cancer. 2007;109:2607–14.
Le Borgne G, Mercier M, Woronoff AS, Guizard AV, Abeilard E, Caravati-Jouvenceaux A, Klein D, Velten M, Joly F. Quality of life in long-term cervical cancer survivors: a population-based study. Gynecol Oncol. 2013;129:222–8.
Acknowledgements
We do not have anyone to acknowledge for this study.
Funding
This study was not supported by any funding resource.
Availability of data and materials
We did not use particular software or databases for this study.
Authors’ contributions
KN designed the study. YK analyzed the data. KN, TS, YT, MT, SN, IS, and MS collected the clinical data. KN drafted the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Consent to publish was not obtained because an individual person’s information is not included in this study.
Ethics approval and consent to participate
Informed consent was not obtained from each participant because this was a retrospective study. Instead of that, all participants were given the right to withdraw the use of the data. The protocol of this study was approved based on the necessity of the individual institutions’ ethical committees since we do not need to obtain the IRB approval for retrospective non-invasive research in Japan. Thus, some of the institutions involved in this research claimed IRB consent: the acquisition numbers of IRB for Gunma University, Tsukuba University, and National Defense Medical College are 11-3, H23-20, and #52, respectively.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nakamura, K., Kitahara, Y., Satoh, T. et al. Analysis of the effect of adjuvant radiotherapy on outcomes and complications after radical hysterectomy in FIGO stage IB1 cervical cancer patients with intermediate risk factors (GOTIC Study). World J Surg Onc 14, 173 (2016). https://doi.org/10.1186/s12957-016-0931-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-016-0931-4