Abstract
Background
Implantable venous access port (IVAP)-related blood stream infections (BSIs) are one of the most common complications of implantable venous ports. The risk factors and pathogens for IVAP-related BSIs are still controversial.
Methods
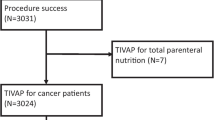
We retrospectively reviewed all patients who received IVAPs at a Hospital in Taiwan from January 1, 2011 to June 31, 2014. Two types of venous port, BardPort® 6.6 fr (Bard port) and Autosuture Chemosite® 7.5 fr (TYCO port) were used. All patients with clinically proven venous port-related BSIs were enrolled.
Results
A total of 552 patients were enrolled. There were 34 episodes of IVAP-related BSIs during the study period for a total incidence of 0.177 events/1000 catheter days. Port type (TYCO vs. Bard, HR = 7.105 (95 % confidence interval (CI), 1.688–29.904), p = 0.0075), age > 65 years (HR = 2.320 (95 % CI, 1.179–4.564), p = 0.0148), and lung cancer (HR = 5.807 (95 % CI, 2.946–11.447), p < 0.001) were risk factors for port infections. We also found that no local sign of infection was significantly associated with the growth of gram-negative bacilli (p = 0.031).
Conclusions
TYCO venous ports, age > 65 years, and lung cancer were all significant risk factors for IVAP-related BSIs, and no sign of infection was significantly associated with the growth of gram-negative bacilli.
Similar content being viewed by others
Background
Venous port implantation is widely used for the safe delivery of systemic chemotherapy in patients with cancer. However, various complications have been reported with an overall complication rate ranging from 0.4 to 29 % [1–4]. The major complications of implantable venous access port (IVAP) placement include infection, thrombosis, catheter obstruction, extravasation, and catheter migration [1, 5, 6], of which IVAP-related infection is the most common. Catheter-related blood stream infections (BSIs) have been reported in 2.4 to 16.4 % of cases [4, 7–11]. Several studies have reported factors that increase infectious port complications, with one of the most significant being hematologic malignancy. However, to the best of our knowledge, only a few studies have systematically analyzed the risk factors for IVAP-related blood infections. Samaras et al. reported that port-associated infections are mostly observed in younger patients with hematologic neoplasms [12]. Recently, Shim et al. concluded that hematologic malignancy and receiving palliative chemotherapy were independent risk factors for IVAP-related BSIs [8]. In addition, a case control study performed by Lee et al. showed that prolonged catheter placement was a risk factor for catheter-related BSIs and that the risk was lower in patients with primary gastrointestinal cancer than in other types of cancer [10]. However, to date, no studies have investigated whether the type of venous port is a possible risk factor for venous port infections. The aim of this retrospective study, therefore, was to investigate the risk factors for IVAP-related BSIs in a university affiliated hospital in Taiwan. We also reviewed the related literature.
Methods
The study population included all patients who received IVAPs for chemotherapy at Kaohsiung Municipal Ta-Tung Hospital from January 1, 2011 to June 30, 2014. The IVAPs included the BardPort® 6.6 fr implantable port (Bard, NJ, USA (Bard port)) and the Autosuture Chemosite® Fr.7.5 port (Tyco Healthcare Group, CT, USA (TYCO port)). The Bard port was made of silicon, and the TYCO port was made of polyurethane. All IVAPs were placed by surgeons under local anesthesia and aseptic conditions without the use of prophylactic antibiotics. The vessel cutdown method was used for catheter cannulation. After venostomy, the distal end of the entry vessel was controlled and the catheter was inserted via the superior vena cava. The cephalic vein was the first choice for entry, and the subclavian vein was used as the point of the entry if the cephalic vein was difficult to approach. All locations of the implanted venous ports were confirmed by fluoroscopy and postoperative X-rays. The surgeon ensured that all of the tips of the venous catheters were located at the junction of the superior vena cava and right atrium (cavo-atrial junction) intraoperatively. IVAPs placed in the femoral veins were excluded.
For all patients with signs and symptoms of IVAP-related BSIs, we routinely perform aerobic and anaerobic microorganism cultures with whole blood samples. Blood culture results that were positive for a fungus or bacteria were recorded. The possibility of a contaminated blood culture was determined after agreement by two physicians (Dr. Hsu JF and Dr. Chang HL). The catheter tips of the removed IVAPs were placed on agar plates and sent to our laboratory for microbiology studies.
An IVAP-related BSI was defined according to the definition reported by Liaw et al. [13] as (1) clinical features of infection, fever, and chills but no identifiable focus of infection elsewhere and (2) isolation of the same organism from the catheter tip and peripheral blood cultures. A probable IVAP-related BSI was considered on the basis of fever and chills following port flush and a positive blood culture result but no identifiable focus of infection elsewhere. One of the following criteria was also required: (1) isolation of the same organism from the port and peripheral blood cultures at the same time but a negative catheter tip culture and (2) isolation of the same organism from peripheral blood cultures when fever and chills occurred following port flush but a negative catheter tip culture. Local infection was defined as the presence of signs of local inflammation, including erythema, warmth, tenderness, and pus formation. When signs of a local infection were noted, wound swab cultures were obtained. To calculate the incidence rate (events per 1000 catheter days), the duration of IVAP catheter use was calculated using the last day of the patients’ medical records instead of the day of IVAP removal.
The Institutional Review Board (IRB) of Kaohsiung Medical University Hospital (KMUH) approved this study (KMUH-IRB-20140366) according to Taiwan national regulations. Considering the retrospective nature of the study, we could not obtain patient consent for the use of clinical data, and the IRB of KMUH waived the need for written informed consent from the participants. In addition, information in the patient records was anonymized and de-identified prior to analysis.
Data were entered and analyzed using JMP statistical software (version 9.0, SAS Institute Inc., Cary, NC, USA). Demographic data, underlying cancer, and related covariates were compared between the groups with and without port infections using Fisher’s exact test for categorical variables and the Wilcoxon rank sum test for continuous variables. To identify the major factors associated with port infections, Cox multivariate logistic regression analysis with stepwise variable selection was performed. Statistical significance was set at p < 0.05.
Results
A total of 552 patients were enrolled. There were 34 episodes of IVAP-related BSIs during the study period, for a total incidence of IVAP-related BSIs of 0.177 events/1000 catheter days. Table 1 shows the clinical characteristics of the patients according to the port used, and the TYCO venous port had a higher infection rate than the Bard type (p = 0.0185) (Fig. 1).
Venous port infections were more common in males, those age > 65 years and those with lung cancer (Table 2). In multivariate Cox regression analysis, port type (TYCO vs. Bard, hazard ratio (HR) = 7.105 (95 % confidence interval (CI), 1.688–29.904), p = 0.0075), age > 65 years (HR = 2.320 (95 % CI: 1.179–4.564), p = 0.0148), and lung cancer (HR = 5.807 (95 % CI, 2.946–11.447), p < 0.001) were risk factors for port infections (Table 3).
We further analyzed the pathogens and found that 19 (55.8 %) cases involved gram-negative bacteria, with Klebsiella pneumoniae being the most common pathogen followed by Acinetobacter baumannii, Escherichia coli, and Pseudomonas aeruginosa (Table 4). Fifteen (39.4 %) infections involved gram-positive bacteria, with Staphylococcus aureus being the most common pathogen. Oxacillin-sensitive Staphylococcus aureus was more common than oxacillin-resistant Staphylococcus aureus. In addition, there were four (10.5 %) fungal infections, all of which involved Candida spp. No local infections significantly grew gram-negative bacilli (p = 0.031) (Table 5).
Discussion
The results of this study suggest that the type of venous port may affect the rate of BSIs. In addition, the patients who were older than 65 years or had lung cancer also had a significantly higher infection rate. Furthermore, we also found that the patients without signs of infection over the port had a significantly higher rate of gram-negative bacilli infections. The overall incidence of IVAP-related BSIs was 0.177 events/1000 catheter days, which is similar to previously reports (0.16 to 0.35 events/1000 port days) [2, 12, 14].
The Bard port is made of silicon, whereas the TYCO port is made of polyurethane. In our previous study, we found that the Bard fr 6.6 venous port had a significantly higher migration rate of up to 6.7 % compared with the Autosuture Chemosite fr 7.5 venous port (0 %) (p = 0.0006) because the Bard port was more flexible with a smaller caliber [15]. Silicone is a polymer that contains silicon, hydrogen, oxygen, and carbon, and silicone catheters are used for long-term vascular access (weeks to months), such as that required for the prolonged administration of chemotherapy. Polyurethane is a versatile polymer, and it is used in vascular catheters as it can provide enough tensile strength to allow for the catheter to pass through the skin and subcutaneous tissues without kinking. Polyurethane catheters are often used for short-term vascular cannulation, and they have been reported to have slightly higher colonization/infection rates although biofilm has been reported to form on both silicone and PU catheters [16].
The pathogenesis of IVAP-associated infections centers around multifaceted interactions between the bacteria, catheter, and host. Bacterial factors are probably the most important in the pathogenesis of infection, whereas catheter factors are the most modifiable with regard to preventing infection [17]. Bacterial adherence to catheters may depend, in part, on the nature of the biomaterial, and some substances eluted from the catheter may affect the viability and growth of different microorganisms [16, 18]. Catheters made of silicone have demonstrated a tendency towards an increased infection rate than those made of PU in some in vitro studies. However, these effects have only been demonstrated in vitro and in short-term studies using direct inoculation of bacteria onto the catheter [17, 19, 20]. To date, few studies have investigated late catheter-related infections with different catheter materials or infections following exposure to blood-borne bacteria in humans. Moreover, the time during which catheter materials have been shown to have an effect is very early, when catheter infection rates are already low [16, 19, 20]. Further large scale in vivo studies are needed to elucidate this issue.
In previous studies, the incidence of infection has been reported to be significantly higher in patients with hematologic malignancies, [8, 21, 22] with hematologic malignancies being more strongly related to delayed bloodstream infections than immediate local infections. The more intensive chemotherapy used for hematologic malignancies compared to that used for solid tumors may explain the increased infection rate [23]. However, no cases of IVAP-related BSIs in the patients with hematological malignancies were recorded in this retrospective study. Furthermore, the IVAP-related BSIs occurred mainly among the patients with lung cancer. Marín et al. indicated that in cases of bacteremia in patients with solid tumors, the most frequent neoplasms were hepatobiliary tumors (19 %), followed by lung cancer (18 %), and lower gastrointestinal malignancies (16 %) [9]. In addition, Anatoliotaki et al. reported that breast cancer (22 %) was most common followed by lung cancer (18 %) [11]. Lee et reported that the most common cancers in patients with IVAP-related BSIs were those of the lung, head, and neck [10].
Cutaneous microbial flora has been reported to play a major role in the IVAP-related BSIs that develop within a venous port [24], and gram-positive cocci are therefore considered to be the most prevalent organisms in patients with IVAP [3, 4, 25]. Gram-positive cocci may account for 50–80 % of IVAP-related BSIs [26]. In this study, Staphylococcus aureus was the most common single pathogen among all of the patients, and oxacillin-sensitive Staphylococcus was more common than oxacillin-resistant Staphylococcus. However, half of the enrolled patients had gram-negative bacilli, the most common being Klebsiella pneumoniae, followed by Acinetobacter baumannii, Escherichia coli, and Pseudomonas aeruginosa. An increased incidence of central venous port-related bacteremia due to gram-negative pathogens has been reported in cancer patients [27, 28]. Furthermore, gram-negative bacilli, and especially glucose non-fermenting pathogens, tend to be the most common microorganisms accounting for port-related infections [7, 28]. Interestingly, Liaw et al. [13] reported that in patients with local inflammation, Staphylococcus species were the most common; however, in patients without local port inflammation, up to 91 % of the cases involved nosocomial glucose non-fermenting gram-negative bacilli, with Acinetobacter baumannii and Enterobacter cloacae being the most common. We further found that the patients with no signs of local venous port infection had a significantly higher rate of gram-negative bacilli. Based on these findings, empiric antibiotics for venous port infections should cover both gram-positive and gram-negative bacilli in patients with venous port infections but without signs of local infection.
There are several limitations to this study. First, it was a retrospective, single-hospital study, and the sample size was small. Second, some of the infections may have resulted from other sites of unrecognized infection. Third, not all patients had positive tip cultures in this study, and catheter tip cultures may not be sufficiently sensitive to diagnose port-related infections. Catheter tip cultures have been reported to be 100 % specific but less than 50 % sensitive for a diagnosis [29, 30].
Conclusions
In conclusion, port type, age > 65 years, and lung cancer were all independent risk factors for IVAP-related BSIs. In addition, we also found that patients without signs of local infection over the port were significantly related to a higher rate of gram-negative bacilli infections.
References
Poorter RL, Lauw FN, Bemelman WA, Bakker PJ, Taat CW, Veenhof CH. Complications of an implantable venous access device (Port-a-Cath) during intermittent continuous infusion of chemotherapy. Eur J Cancer. 1996;32A:2262–6.
Biffi R, Corrado F, de Braud F, de Lucia F, Scarpa D, Testori A, et al. Long-term, totally implantable central venous access ports connected to a Groshong catheter for chemotherapy of solid tumours: experience from 178 cases using a single type of device. Eur J Cancer. 1997;33:1190–4.
Kock HJ, Pietsch M, Krause U, Wilke H, Eigler FW. Implantable vascular access systems: experience in 1500 patients with totally implanted central venous port systems. World J Surg. 1998;22:12–6.
Zaghal A, Khalife M, Mukherji D, El MN, Shamseddine A, Hoballah J, et al. Update on totally implantable venous access devices. Surg Oncol. 2012;21:207–15.
Kim HJ, Yun J, Kim HJ, Kim KH, Kim SH, Lee SC, et al. Safety and effectiveness of central venous catheterization in patients with cancer: prospective observational study. J Korean Med Sci. 2010;25:1748–53.
Yeste SL, Galbis Caravajal JM, Fuster Diana CA, Moledo EE. Protocol for the implantation of a venous access device (Port-A-Cath System). The complications and solutions found in 560 cases. Clin Transl Oncol. 2006;8:735–41.
Huang WT, Chen TY, Su WC, Yen CJ, Tsao CJ. Implantable venous port-related infections in cancer patients. Support Care Cancer. 2004;12:197–201.
Shim J, Seo TS, Song MG, Cha IH, Kim JS, Choi CW, et al. Incidence and risk factors of infectious complications related to implantable venous-access ports. Korean J Radiol. 2014;15:494–500.
Marin M, Gudiol C, Garcia-Vidal C, Ardanuy C, Carratala J. Bloodstream infections in patients with solid tumors: epidemiology, antibiotic therapy, and outcomes in 528 episodes in a single cancer center. Medicine (Baltimore). 2014;93:143–9.
Lee GJ, Hong SH, Roh SY, Park SR, Lee MA, Chun HG, et al. A case–control study to identify risk factors for totally implantable central venous port-related bloodstream infection. Cancer Res Treat. 2014;46:250–60.
Anatoliotaki M, Valatas V, Mantadakis E, Apostolakou H, Mavroudis D, Georgoulias V, et al. Bloodstream infections in patients with solid tumors: associated factors, microbial spectrum and outcome. Infection. 2004;32:65–71.
Samaras P, Dold S, Braun J, Kestenholz P, Breitenstein S, Imhof A, et al. Infectious port complications are more frequent in younger patients with hematologic malignancies than in solid tumor patients. Oncology. 2008;74:237–44.
Liaw CC, Chen JS, Chang HK, Huang JS, Yang TS, Liau CT. Symptoms and signs of port-related infections in oncology patients related to the offending pathogens. Int J Clin Pract. 2008;62:1193–8.
Caers J, Fontaine C, Vinh-Hung V, De MJ, Ponnet G, Oost C, et al. Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Support Care Cancer. 2005;13:325–31.
Fan WC, Wu CH, Tsai MJ, Tsai YM, Chang HL, Hung JY, et al. Risk factors for venous port migration in a single institute in Taiwan. World J Surg Oncol. 2014;12:15.
Pascual A. Pathogenesis of catheter-related infections: lessons for new designs. Clin Microbiol Infect. 2002;8:256–64.
Darouiche RO. Device-associated infections: a macroproblem that starts with microadherence. Clin Infect Dis. 2001;33:1567–72.
Mehall JR, Saltzman DA, Jackson RJ, Smith SD. Catheter materials affect the incidence of late blood-borne catheter infection. Surg Infect (Larchmt ). 2001;2:225–9.
Galliani S, Cremieux A, van der Auwera P, Viot M. Influence of strain, biomaterial, proteins, and oncostatic chemotherapy on Staphylococcus epidermidis adhesion to intravascular catheters in vitro. J Lab Clin Med. 1996;127:71–80.
Kristinsson KG. Adherence of staphylococci to intravascular catheters. J Med Microbiol. 1989;28:249–57.
Fischer L, Knebel P, Schroder S, Bruckner T, Diener MK, Hennes R, et al. Reasons for explantation of totally implantable access ports: a multivariate analysis of 385 consecutive patients. Ann Surg Oncol. 2008;15:1124–9.
Ahn SJ, Kim HC, Chung JW, An SB, Yin YH, Jae HJ, et al. Ultrasound and fluoroscopy-guided placement of central venous ports via internal jugular vein: retrospective analysis of 1254 port implantations at a single center. Korean J Radiol. 2012;13:314–23.
Gapany C, Tercier S, Diezi M, Clement C, Lemay K, Joseph JM. Frequent accesses to totally implanted vascular ports in pediatric oncology patients are associated with higher infection rates. J Vasc Access. 2011;12:207–10.
Laurenzi L, Natoli S, Benedetti C, Marcelli ME, Tirelli W, DiEmidio L, et al. Cutaneous bacterial colonization, modalities of chemotherapeutic infusion, and catheter-related bloodstream infection in totally implanted venous access devices. Support Care Cancer. 2004;12:805–9.
Heibl C, Trommet V, Burgstaller S, Mayrbaeurl B, Baldinger C, Koplmuller R, et al. Complications associated with the use of Port-a-Caths in patients with malignant or haematological disease: a single-centre prospective analysis. Eur J Cancer Care (Engl ). 2010;19:676–81.
Penzak SR, Gubbins PO, Stratton SL, Anaissie EJ. Investigation of an outbreak of gram-negative bacteremia among hematology-oncology outpatients. Infect Control Hosp Epidemiol. 2000;21:597–9.
Groeger JS, Lucas AB, Thaler HT, Friedlander-Klar H, Brown AE, Kiehn TE, et al. Infectious morbidity associated with long-term use of venous access devices in patients with cancer. Ann Intern Med. 1993;119:1168–74.
Castagnola E, Garaventa A, Viscoli C, Carrega G, Nantron M, Molinari C, et al. Changing pattern of pathogens causing broviac catheter-related bacteraemias in children with cancer. J Hosp Infect. 1995;29:129–33.
Barbut F, Soukouna S, Lalande V, Garcia ML, Neyme D, de Gramont A, et al. [Totally implantable venous access ports: frequency of complications and analysis of bacterial contamination after ablation]. Pathol Biol (Paris). 2004;52:566–74.
Douard MC, Arlet G, Longuet P, Troje C, Rouveau M, Ponscarme D, et al. Diagnosis of venous access port-related infections. Clin Infect Dis. 1999;29:1197–202.
Acknowledgements
The authors express their gratitude to the staff of the Statistical Analysis Laboratory, Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung Medical University for their assistance. The grant was supported by kmtth-102-035 and kmtth-103-027 in Kaohsiung Municipal Ta-Tung Hospital, Taiwan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CJY designed the study and is the corresponding author. JFH and HLC drafted the manuscript and were responsible for ensuring contaminated blood cultures were excluded. MJT did the statistical analysis and wrote the results. YMT and PHC participated in the study design and data collection. YLL, WCF, and YCS collected and processed data. All of the authors read and approved the final manuscript.
Jui-Feng Hsu and Hsu-Liang Chang contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hsu, JF., Chang, HL., Tsai, MJ. et al. Port type is a possible risk factor for implantable venous access port-related bloodstream infections and no sign of local infection predicts the growth of gram-negative bacilli. World J Surg Onc 13, 288 (2015). https://doi.org/10.1186/s12957-015-0707-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-015-0707-2