Abstract
Adult intussusception is rare and usually caused by a tumor acting as the lead point. Therefore, laparotomy should be considered for the treatment. Laparoscopic procedures for use in cases of adult intussusception have been recently reported; however, there is no consensus regarding the safety and efficacy. Here, we describe a successful case of laparoscopic management of an octogenarian adult intussusception caused by an ileal lipoma, which was preoperatively suspected. An 87-year-old male presented with progressive abdominal distention and vomiting. Contrast radiography of the small intestine showed an ileal tumor, and magnetic resonance imaging indicated a target-like mass, consistent with an ileal intussusception. The patient was suspected with an intussusception due to an ileal lipoma, and laparoscopic surgery was performed. An approximately 10-cm-long ileal intussusception with a preceding tumor was present, and partial resection of the ileum, including the tumor, was performed. Macroscopic examination of the excised specimen showed a pedunculated tumor measuring 4.0 × 3.5 × 1.9 cm with an uneven surface, yielding a histological diagnosis of lipoma. The patient had an uneventful recovery and was discharged on postoperative day 8. This successful case showed that laparoscopic surgery can be a useful, safe, and efficacious procedure for adult intussusception, even in octogenarians.
Similar content being viewed by others
Background
Adult intussusceptions constitute approximately 5% to 10% of all intussusceptions and are usually caused by a tumor that acts as the lead point [1,2]. While laparoscopic devices and surgical techniques have recently been improved and applied to adult intussusceptions, there is no consensus regarding safety and efficacy. This report presents a case of an octogenarian adult intussusception caused by an ileal lipoma, which was preoperatively suspected and successfully managed by laparoscopic surgery.
Case presentation
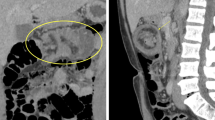
An 87-year-old male presented at our department with progressive abdominal distention and vomiting for 2 weeks. His medical history included hypertension and revealed that he had undergone laparoscopic-assisted ileocecal resection for cecal cancer in January 2004. Physical examination revealed a distended abdomen and a tender right lower quadrant. Laboratory test results, including serum levels of carcinoembryonic antigen and carbohydrate antigen 19–9, were within normal limits. Abdominal radiography revealed a prominently dilated small intestine with some air-fluid interfaces. A long tube was inserted to reduce the internal pressure of the small intestine, and Gastrografin contrast radiography was performed. It showed an approximately 40-mm-diameter ileal tumor (Figure 1). The ileus temporally improved, and subsequent magnetic resonance imaging (MRI) showed a target-like mass consistent with an ileal intussusception (Figure 2A,B). The patient was diagnosed with intermittent intussusception with an ileal tumor, which was suspected to be a lipoma. Laparoscopic surgery was performed in May 2014.
The patient was placed under general anesthesia in the supine position. A 12-mm cannula for a camera was inserted in the periumbilical region by the open technique, and 10 mmHg of abdominal pressure was established by carbon dioxide insufflation of the pneumoperitoneum. Using direct laparoscopic visualization, two 5-mm ports were created in the left upper and lower quadrant for the surgeon, and two 5-mm ports were created in the right middle quadrant and just above the pubic bone for the assistant. An approximately 10-cm-long ileal intussusception with a preceding tumor was identified 40 cm proximal to the neo-terminal ileum (Figure 3A). Manual repositioning under laparoscopy did not reduce intussusception. There were sparse adhesions between the intussuscepted ileum and the retroperitoneum, which were exfoliated with a harmonic scalpel. Once the entire intussuscepted ileum had been mobilized within the abdominal cavity, a 4-cm incision was made in the periumbilicus, through which the intussuscepted ileum was delivered (Figure 3B). Partial resection of the delivered ileum including the tumor and a functional end-to-end anastomosis were performed. There were no signs of lymphadenopathy, and the liver had an unremarkable surface. Surgical blood loss was 5 ml, and operating time was 115 min. The excised tumor measured 4.0 × 3.5 × 1.9 cm and had an uneven surface with mucosal erythema (Figure 4A). Ulcerative mucosal change caused by the intussusception was observed in the oral side of the ileum from the tumor. Sectioning of the tumor revealed a solid, yellowish tissue. Histological examination of the excised tumor showed mature fat cells in the submucosa to the muscularis propria of the ileum (Figure 4B). Thickened mucosa on the tumor showed abundant micro vessels and epithelial ductal hyperplasia; however, no tumor was observed in that location.
The patient had an uneventful recovery; he passed flatus on postoperative day (POD) 1, commenced oral fluids on POD 2, and was discharged on POD 8.
Discussion
Intussusception is rare in adults compared with that in children, and the frequency is approximately 5% to 10% of all intussusceptions [1,2]. Of the cases of intussusception in children, 95% are idiopathic with no structural lead points. On the other hand, adult intussusception is caused by an identifiable etiology in approximately 80% of the cases [3]. Previous reports have suggested that approximately 70% of the cases of adult small intestinal intussusception are caused by benign entities, such as lipomas, hamartomatous polyps, inflammatory polyps, hyperplastic polyps, and Meckel’s diverticulum [4-6]. Preoperative diagnosis is difficult because of the variability of the clinical presentation. Namikawa et al. [7] reviewed 50 cases of lipoma with intussusception and reported that the accuracy of preoperative diagnosis was 39.1% to 44.4%. There are several reasons why the accuracy of preoperative diagnosis is low. Patients develop intussusception as an acute abdominal condition, and there is a limit to preoperative diagnostics, particularly in the case of small intestinal intussusception. In the present case, contrast radiography showed a tumor in the ileum, and MRI findings were typical of an intussusception, that is, a target-like mass [8]. We had two reasons to preoperatively suspect that this ileal tumor was a lipoma. First, MRI showed a hyper-intense tumor in the T2-weighted image, and second, lipoma is the most common benign tumor that causes adult intussusception confined to the small intestine [9].
First treatment for adult intussusception is debatable. Many cases of adult intussusceptions are caused by an identifiable etiology; laparotomy should be considered as the first line of treatment. As a result of the marked improvement in laparoscopic devices and surgical techniques, there are reports of its use in cases of adult intussusception [10,11]. However, there is no consensus on whether laparoscopic surgery can be applied to adult intussusception with respect to safety and efficacy. Siow et al. [12] and Tartaglia et al. [13] reported that laparoscopic surgery for adult intussusception was a safe and feasible treatment, particularly in cases with an uncertain preoperative diagnosis. In the present case, laparoscopic surgery was selected for the following reasons: i) the patient’s clinical condition was stable, so he was able to undergo relaparotomy; ii) the patient was an octogenarian; therefore, we had to reduce the risk of postoperative complications, such as obstructive pneumonitis or disuse syndrome, as much as possible, which could develop from wound pain; and iii) the patient had previously undergone ileocecal resection for cecal cancer, and laparoscopic surgery would be able to exfoliate any adhesions identified in the abdominal cavity. In the English literature from the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed/), there have been 14 reported cases described by the words ‘adult intussusception,’ ‘lipoma,’ and ‘laparoscopy’ including the present case (Table 1) [14-26]. The average age of the patients in these reports was 59.3 years (range 36 to 87 years), and the present case involved the oldest patient who was successfully managed by laparoscopic surgery. In most of these patients, the tumors were preoperatively diagnosed as lipomas (78.6%), and this is different from those reported by Namikawa et al. [7]. This difference may be attributed to the fact that laparoscopic surgery tends to be selected because of a correct preoperative diagnosis of lipoma. Eight cases (57.1%) were classified as enteric intussusceptions, which suggest that laparoscopic surgery was an effective method for adult enteric intussusception. In most cases, the number of ports was three to five; however, Chen et al. [25] reported on a single-port laparoscopic surgery. Although there were no data in two patients, the average postoperative stay was 7.4 days (range 3 to 15), and there were no postoperative complications. From these results, laparoscopic surgery may safely and efficaciously be used as the therapeutic method for adult intussusceptions with lipomas, even for oldest patients.
Conclusions
Laparoscopic surgery in experienced hands may be considered for the treatment for adult intussusception, even in octogenarians, as it is a safe and efficacious procedure.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- POD:
-
Postoperative day
References
Weilbaecher D, Bolin JA, Hearn D, Ogden 2nd W. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121(5):531–5.
Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173(2):88–94.
Sanders GB, Hagan WH, Kinnaird DW. Adult intussusception and carcinoma of the colon. Ann Surg. 1958;147(6):796–804.
Eisen LK, Cunningham JD, Aufses Jr AH. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188(4):390–5.
Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226(2):134–8.
Chiang JM, Lin YS. Tumor spectrum of adult intussusception. J Surg Oncol. 2008;98(6):444–7.
Namikawa T, Hokimoto N, Okabayashi T, Kumon M, Kobayashi M, Hanazaki K. Adult ileoileal intussusception induced by an ileal lipoma diagnosed preoperatively: report of a case and review of the literature. Surg Today. 2012;42(7):686–92.
Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, et al. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol. 2003;36(1):18–21.
Bilgin M, Toprak H, Ahmed IC, Yardimci E, Kocakoc E. Ileocecal intussusception due to a lipoma in an adult. Case Rep Surg. 2012;2012:684298.
Alonso V, Targarona EM, Bendahan GE, Kobus C, Moya I, Cherichetti C, et al. Laparoscopic treatment for intussusception of the small intestine in the adult. Surg Laparosc Endosc Percutan Tech. 2003;13(6):394–6.
Ruiz-Tovar J, López-Delgado A, Santos JE, Arroya A, Calpena R. Laparoscopic treatment of sigmoid colon intussusception secondary to giant submucosal lipoma. Acta Gastroenterol Latinoam. 2013;43(1):36–8.
Siow SL, Mahendran HA. A case series of adult intussusception managed laparoscopically. Surg Laparosc Endosc Percutan Tech. 2014, Apr 12. [Epub ahead of print].
Tartaglia D, Bertolucci A, Palmeri M, Kauffmann EF, Napoli N, Galatioto C, et al. The role of laparoscopy in adult bowel obstruction caused by intussusception. Ann Ital Chir. 2014; May 19;85. Pil: S0003469X14022210. [Epub ahead of print].
Park KT, Kim SH, Song TJ, Moon HY. Laparoscopic-assisted resection of ileal lipoma causing ileo-ileo-colic intussusception. J Korean Med Sci. 2001;16(1):119–22.
Ladurner R, Mussack T, Hohenbleicher F, Folwaczny C, Siebeck M, Hallfeld K. Laparoscopic-assisted resection of giant sigmoid lipoma under colonoscopic guidance. Surg Endosc. 2003;17(1):160.
Jelenc F, Brencic E. Laparoscopically assisted resection of an ascending colon lipoma causing intermittent intussusception. J Laparoendosc Adv Surg Tech A. 2005;15(2):173–5.
Mckay R. Ileocecal intussusception in an adult: the laparoscopic approach. JSLS. 2006;10(2):250–3.
Tsushimi T, Matsui N, Kurazumi H, Takemoto Y, Oka K, Seyama A, et al. Laparoscopic resection of an ileal lipoma: report of a case. Surg Today. 2006;36(11):1007–11.
Lin MW, Chen KH, Lin HF, Chen HA, Wu JM, Huang SH. Laparoscopy-assisted resection of ileoileal intussusception caused by intestinal lipoma. J Laparoendosc Adv Surg Tech A. 2007;17(6):789–92.
Oyen TL, Wolthuis AM, Tollens T, Aelvoet C, Vanrijkel JP. Ileo-ileal intussusception secondary to lipoma: a literature review. Acta Chir Belg. 2007;107(1):60–3.
Ako E, Morisaki T, Hasegawa T, Hirakawa T, Tachimori A, Nakazawa K, et al. Laparoscopic resection of ileal lipoma diagnosed by multidetector-row computed tomography. Surg Laparosc Endosc Percutan Tech 2. 2010;20(6):e226–229.
Lucas LC, Fass R, Krouse RS. Laparoscopic resection of a small bowel lipoma with incidental intussusception. JSLS. 2010;14(4):615–8.
Ferrara F, Duburque C, Quinchon JF, Gaudissart Q. Laparoscopic resection of small bowel lipoma causing obscure gastrointestinal bleeding. Updates Surg. 2012;64(2):153–6.
Hou YC, Lee PC, Chang JJ, Lai PS. Laparoscopic management of small-bowel intussusception in a 64-year-old female with ileoal lipoma. World J Gastrointest Surg. 2012;4(9):220–2.
Chen JH, Wu JS. Single port laparoscopic right hemicolectomy for ileocolic intussusception. World J Gastroenterol. 2013;19(9):1489–93.
Son DN, Jung HG, Ha DY. Laparoscopic surgery for an intussusception caused by a lipoma in the ascending colon. Ann Coloproctol. 2013;29(2):80–2.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for reviewing the English language of the original manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JS wrote the manuscript. TN and Takanobu T performed surgery. SS, HU, and Takafumi T drafted the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Shimazaki, J., Nakachi, T., Tabuchi, T. et al. Laparoscopic management of an octogenarian adult intussusception caused by an ileal lipoma suspected preoperatively: a case report. World J Surg Onc 13, 75 (2015). https://doi.org/10.1186/s12957-015-0504-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-015-0504-y