Abstract
Background
Huntington’s disease (HD) is a progressive neurodegenerative disease with a devastating impact on patients and their families. Quantifying how treatments affect patient outcomes is critical for informing reimbursement decisions. Many countries mandate a formal value assessment in which the treatment benefit is measured as quality-adjusted life-years, calculated with the use of utility estimates that reflect respondents’ preferences for health states.
Objective
To summarize published health state utility data in HD and identify gaps and uncertainties in the data available that could be used to inform value assessments.
Methods
We conducted a systematic literature review of studies that used preference-based instruments (e.g., EQ-5D and SF-6D) to estimate utility values for people with HD. The studies were published between January 2012 and December 2022.
Results
Of 383 articles screened, 16 articles reported utility values estimated in 11 distinct studies. The utility measure most frequently reported was EQ-5D (9/11 studies). Two studies reported SF-6D data; one used time trade-off methods to value health state descriptions (vignettes). Although utility scores generally worsened to a lower value with increased HD severity, the estimates varied considerably across studies. The EQ-5D index range was 0.89 − 0.72 for mild/prodromal HD and 0.71 − 0.37 for severe/late-stage disease.
Conclusions
This study uncovered high variability in published utility estimates, indicating substantial uncertainty in existing data. Further research is needed to better understand preferences and valuation across all stages and domains of HD symptoms and the degree to which generic utility measures capture the impact of cognitive changes on quality of life.
Similar content being viewed by others
Introduction
Huntington’s disease (HD) is a hereditary neurodegenerative disease characterized by cognitive and motor decline and behavioral symptoms [1]. Although HD is considered rare, it affects patients worldwide. A recently published meta-analysis estimated the pooled prevalence across studies in Europe, North America, South America, and Asia to be 4.88 per 100,000 people (95% confidence interval, 3.38–7.06) [2]. The impact of HD on patients and their family members is significant [3,4,5]. According to a cohort study of medical records of primary care patients in the United Kingdom, a significantly higher relative risk of psychotic disorders, depression, insomnia, dementia, weight loss, pneumonia, and falls was observed in patients with HD compared with the demographically matched general population [4]. Despite the well-documented substantial disease burden of HD, the benefits of currently available treatments are limited to the management of motor and psychiatric symptoms. There are several new compounds under investigation that have the potential to improve symptoms or delay progression of symptomatology [6]. Further evidence may be required to ensure approved treatments are reimbursed by payers.
In many countries, determining whether the price of a new treatment is justified by the benefits that it brings to patients and their care partners requires a formal value assessment on the incremental cost per quality-adjusted life-year (QALY) gained [7]. To ensure that patients will have the ability to access innovative treatments if and when they receive market authorization, quantifying the degree to which the new treatment impacts patients’ QALYs is needed. The gain in QALYs with a treatment is estimated by adjusting the value of each year of life according to patients’ health state and quality of life (QOL). Each year of life is weighted with the use of health state utility (HSU) values, where a value of 1 represents full health and 0 represents dead (or a health state equivalent to being dead) [8]. Although health-related quality-of-life (HRQOL) can be measured by both disease-specific instruments (such as the Huntington’s Disease health-related Quality of Life questionnaire [HDQoL]) and generic instruments (such as 36-Item Short-Form Survey [SF-36]), HSU values are recommended to be based on generic measures so that the QALYs can be compared across health conditions. Furthermore, to place higher value on treatments that improve problems that are more important to patients and the general population, payers typically prefer utility values based on preference-based instruments that account for trade-offs among people’s preferences across different dimensions of health attributes. Hence, the value of a life-year is often estimated using generic, preference-based, HRQOL measures, such as the EQ-5D and the short-form 6-dimension (SF-6D), to estimate HSUs and reflect preferences for various health states across a disease continuum [9].
A systematic review by van Lonkhuizen and colleagues [10] summarized studies describing or evaluating self-reported QOL and HRQOL by individuals with genetically or clinically confirmed HD (i.e., premanifest or manifest HD). While that article made a significant contribution toward researchers’ understanding the determinants of a variety of multidimensional QOL outcomes in individuals with premanifest and/or manifest HD, the search strategy focused on identifying general QOL and HRQOL literature rather than studies that report HSU values. As a result, preference-based utility values were available in only 2 of the 30 studies included in their review. To evaluate the availability of published, preference-based utility values associated with different health states in patients with HD and to assess which estimation methods may be most appropriate for HSUs in HD, a review of the existing literature is required. To our knowledge, no article reviewing the existing literature reporting utility values of patients with HD has been published.
The primary objective of this study was to identify published utility data in HD and identify any gaps and/or uncertainty in the data that may suggest caution for use in value assessments or the need for further research. We conducted a systematic literature review to identify studies reporting utility estimates for people with HD and summarized the data for the overall population as well as by stage of disease.
Materials and methods
Databases, search strategy, and selection process
A systematic literature review to identify studies reporting utility estimates for people with HD was conducted according to a predefined protocol. An electronic literature search from January 2012 to December 2022 was performed using the electronic medical literature databases Embase, MEDLINE, and Cochrane Library. To identify research abstracts not indexed in medical literature databases, we also included in the search conference abstracts published in the last 2 years (2020–2022) from the Professional Society for Health Economics and Outcomes Research (ISPOR), Huntington Study Group, European Huntington’s Disease Network, and International Society for Quality-of-Life Research.
The inclusion and exclusion criteria (provided in Online Resource 1, Table S1), were based on a strategy to identify the population and disease condition, interventions, comparators, outcomes, and study types of interest). Our search strategy targeted articles and conference abstracts that included utility estimation studies and utility estimates generated as part of economic evaluations for HD. The search string included the key Medical Subject Headings (MeSH) term “Huntington Disease” (and variants) in combination with a variety of key terms pertaining to utility studies (such as “health utility,” “TTO,” “EQ-5D,” “SF-36,” “SF-6D,” “health related quality of life,” “quality adjusted life years”). Details of the full search strategy used in PubMed are provided in Online Resource 1, Table S2; the strategy was adapted for the other database searches. Reference lists of identified review studies were checked for source articles that may have been missed in the primary searches. Articles not published in English, and studies that did not explicitly estimate utility outcomes of patients with HD were excluded.
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to ensure transparency in performing and the reporting of the review [11]. Each title and abstract of a study identified from an electronic database or from Internet searches was reviewed by 2 researchers for eligibility according to the inclusion and exclusion criteria. Discrepancies were resolved by consensus. When a consensus was not reached, a third researcher was consulted. Full texts of studies selected were obtained and reviewed by two research team members for eligibility according to the inclusion and exclusion criteria. Each selected study was reviewed by another study member to check for and avoid potential error and bias. Any discrepancies were resolved by consensus; when a consensus was not reached, a third researcher was consulted.
Outcomes extraction strategy
Once the full set of published studies reporting utility values was identified, evidence tables were created for the following items: title, author(s), publication year, study type, HD severity distribution and method/measure used for severity determination, other population features (e.g., sample size, average age, percentage male vs. female), and key utility outcomes (e.g., measure used, value set applied, respondent type [patient or proxy]) when reported. Utility values were further broken down by HD staging, when available, to capture utility changes throughout disease progression.
Data were extracted from full-text publications, where available. When a single study’s results were reported in multiple publications (i.e., an abstract or poster and a subsequent full-text publication or multiple full-text publications), the final full-text publication with the richest source of data was selected for data extraction. When relevant information (e.g., respondent type, value set applied) was not reported in the full-text journal publication, we searched secondary reports (e.g., abstract, poster, subsequent publications) to seek information that could be reported elsewhere.
Results
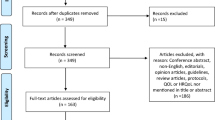
The inclusion and exclusion processes are shown in the PRISMA flowchart (Fig. 1) [11, 12]. A total of 383 unique publication abstracts, including conference abstracts, were retrieved from database searches. A review of these abstracts identified 66 articles and 9 conference posters that could have met the inclusion criteria for our review. After the full text of the 66 articles were reviewed, 52 were excluded because they did not report utility values for individuals with HD. The final number of articles and conference posters included in this systematic literature review was 16 (14 articles reporting 11 unique studies and 2 conference posters).
PRISMA diagram for study inclusion and exclusion
HRQOL = health-related quality of life, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Adapted from Moher et al. [12]
Table 1 presents a list of the included studies and key features of each study. Four of the 14 articles [13,14,15,16] identified in Fig. 1 reported utility data originating from the same study. Carlozzi et al. [16] was identified as the primary report due to the richness of reported utility data, and the other 3 articles [13,14,15] were examined for any additional relevant information. In addition, two conference abstracts identified were earlier presentations of data published in subsequent articles by the same authors (Claassen et al. [17], Rodriguez Santana et al. [18]). Therefore, 11 distinct studies from the 16 identified publications were included in our analysis. Table 1 lists the characteristics of the 11 studies. Among the 11 distinct studies, 4 included participants located in the US, 2 in the UK, and 3 were multinational (2 including European countries and 1 including both US and European countries). The remaining 2 studies included participants located in Spain and Canada.
The utility measure used most frequently was the EQ-5D index (9 of 11 studies, Table 1). Two studies used the 3-level version of the instrument [19, 20], 2 studies used the 5-level version [18, 21], 1 study mapped the EQ-5D from SF-36 data [22], and the remaining 4 studies did not report the EQ-5D version. Two studies used the SF-6D to estimate utility by disease stage in patients with HD [18, 23], one of which also reported EQ-5D utility values [18]. One study did not report EQ-5D or SF-6D but instead estimated utility values associated with 4 levels of chorea severity described in vignettes using time trade-off methods in a sample of the general population [17].
A variety of disease-specific HRQOL measures were used in the studies alongside preference-based generic utility measures, including the HD-PRO-TRIAD, Quality of Life in Neurological Disorders, HDQLIFE Short Form, the Huntington Quality of Life Instrument (H-QoL-I), and the HDQoL. Also, EQ-5D visual analogue scale (VAS) scores were often reported alongside the EQ-5D index scores. For example, a cross-sectional survey study by Exuzides and colleagues [21] reported both the EQ-5D index and VAS scores.
The demographic and clinical characteristics of the populations included in the 10 studies that included patients with HD are reported in Table 1 (the 11th study, Claassen et al. [17], was a vignette valuation study in the general population). The study populations appear to be generally representative of the overall HD population, with a similar number of men and women [1]. However, we identified 3 cross-sectional surveys with more unbalanced samples (Exuzides et al. [21] with 68.3% female; Shaw et al. [22] with 28% female; Rodriguez Santana et al. [18] with 35% female). The average age of the participants was between 40 and 58 years, which appears to be consistent with other studies in HD that describe age at onset (mean = 30–50 years; range = 2–85) and disease duration (mean = 17–20 years) [24]. The verification of diagnosis differed somewhat among the studies (Table 1), with studies conducted at clinical sites using clinical diagnosis [16, 18, 23] or a positive gene status [20]. Two studies did not report details on how diagnoses were verified [19, 25], and 4 studies allowed participant self-reported diagnoses, either by genetic identification or clinical diagnosis [21, 22, 26, 27]. Only one of these studies [26] reported the proportion of patients in which the diagnosis was based on gene mutation status or clinical diagnosis: 87% of participants reported a positive gene mutation status and 67% reported clinical diagnosis. Where reported, the mean number of years since diagnosis varied from 3.97 (Carlozzi et al. [16]) to 9.0 years (Shaw et al. [22]); in 4 studies, it was not reported.
Among the 11 studies, 2 were based on site-administered surveys along with clinical observations [16, 23], and 5 were cross-sectional self-administered surveys [21, 22, 25,26,27]. Two studies were based on cross-sectional survey data collected from patients and physicians in an existing HD dataset (Rodriguez Santana et al. [18]; Huntington’s Disease Burden of Illness Study, Dorey et al. [19]; European-Huntington’s disease burden study). The remaining 2 studies included a vignette study in the general population [17] and a randomized controlled trial [20].
Among the surveys of patients with HD, more than half (7/9) were cross-sectional studies that relied on self-/proxy- or physician survey–reported outcomes completely; the remaining 2 studies [16, 23] were longitudinal, prospective, observational studies that required clinicians to collect at least some of the key clinical outcomes, such as clinical diagnoses of HD, years since HD diagnosis, staging, and severity. All 9 survey-based studies collected self-reported outcomes from patients with HD; 1 of these studies also collected proxy-rated utility values for all participants [27]. One study collected proxy-rated utility values only for patients who could not respond due to advanced disease [18].
Table 2 summarizes the utility estimates reported in each of the 11 studies identified. Among the 9 studies reporting EQ-5D utility index data, utility estimates for the overall HD population ranged from 0.81 (mean age = 48.74 years, 41.0% male, mean years since diagnosis = 3.97, prodromal HD 38.5%, early HD 38.0%, late HD 23.5%) [16] to 0.3 (mean age = 57.1 years, 45.1% male, mean years since diagnosis = 4.9) [25]. In early-stage and mid-stage disease, the anxiety and depression dimension was the main driver of poor EQ-5D utility scores, while in patients with advanced-stage disease, the main drivers were mobility, followed by the self-care and usual activities [18]. One study used the EQ-5D utility index to compare HD patients with an age- and sex-matched general population cohort [21]. In the cross-sectional survey conducted by Exuzides and colleagues in the US, the mean EQ-5D-5 L index score was significantly lower for patients with HD than for the general population (0.66 vs. 0.81; P < 0.001); almost half of the HD group had early-stage disease.
Where data were reported for different levels of severity of HD, utility scores generally worsened with increasing HD severity. In the cross-sectional US Huntington’s Disease Burden of Illness Study, Rodriguez Santana and colleagues [18] reported a decline in the mean (standard deviation [SD]) EQ-5D-5 L index score for patients with advancing disease (early-stage: 0.72 [0.22]; mid-stage: 0.62 [0.18]; and advanced-stage: 0.37 [0.30]). Carlozzi et al. [16] and Dorey et al. [19] also reported decreasing EQ-5D index scores with advancing disease.
Although all studies exploring EQ-5D values for different disease stages observed lower utility values with advancing disease, the score ranges within each disease stage varied considerably across studies. For example, in the cross-sectional study of patients with HD by Rodriguez Santana et al. [18], the mean (SD) EQ-5D index score for patients with early- (Total Functional Capacity sum of score [TFC] 13 − 7), mid- (TFC 6 − 4), or advanced-stage (TFC 3 − 0) HD, as defined by Wild et al. [28], was reported to be 0.72 (0.22), 0.62 (0.18), and 0.37 (0.30), respectively. However, Carlozzi and colleagues’ [16] longitudinal observational study reported the mean (SD) EQ-5D utility index scores for patients in prodromal, early (TFC 13 − 7), and late (TFC 6 − 0) stages of HD to be 0.89 (0.12), 0.80 (0.14), and 0.71 (0.17), respectively. The utility estimate for TFC 13 − 7 was higher in Carlozzi and colleagues (0.80 versus 0.72), and the estimate for TFC 6 − 0 in Carlozzi and colleagues was higher than the estimate for TFC 6 − 4 in Rodriguez Santana (0.71 versus 0.62), despite the latter excluding later stage patients (TFC 3 − 0) where utility was lower (0.37). Both were large studies (336 and 536 patients, respectively, with sample sizes ranging from 88 to 205 within each severity category), with clinician-verified diagnosis and similar mean age (47.3 vs. 48.74 years). There were fewer women in the Rodriguez Santana sample (35% vs. 59% in the Carlozzi sample). Some of the difference between studies may be attributed to differences in the EQ-5D version and value set used. Rodriguez Santana and colleagues [18] used the EQ-5D-5L with utility calculated using the England value set (the specific version of the England value set was not reported); Carlozzi and colleagues [16] did not report which version of the EQ-5D instrument or which value set was used. Rodriguez Santana and colleagues used proxy completion for patients with a severe cognitive deficit (the mean for all respondents is reported earlier in this paragraph); Carlozzi and colleagues [16] did not report use of proxy completion. The use of proxy completion may also explain some of the difference in utility estimates, as the proxy utility value for advanced-stage disease was much lower than the patient-reported value (0.13 versus 0.42, respectively).
A visual comparison of mean EQ-5D index utility scores across studies in patients with differing numbers of years since HD diagnosis does not reveal any obvious trend between time since HD diagnosis and mean utility value (Fig. 2). For example, in a US cross-sectional survey of patients with a mean 4.8 years since diagnosis, the mean (SD) EQ-5D index score was estimated to be 0.6 (0.3) [27]. In contrast, a Canadian cross-sectional survey [22] of patients with a substantially longer average number of years since diagnosis (9.9 years) estimated the mean (SD) EQ-5D index score to be higher (0.72 [0.24]) than that in the US survey. In both studies, HD diagnosis and time since diagnosis were self-reported. Some of the difference in utility estimates may be explained by the fact that the Canadian study [22] estimated EQ-5D utility index from SF-36 data using the mapping algorithm by Rowen et al. [29], which has been reported to overpredict utility for more severe health states. However, a regression analysis of SF-6D data by Hawton and colleagues [23] found no significant relationship between utility and time since diagnosis. The authors acknowledged some individuals are diagnosed in the premanifest stage because of family history of the condition and early predictive testing and may live for decades after diagnosis without any clinical expression, while others may be diagnosed much later at the point of significant functioning loss. Such heterogeneity in the timing of diagnosis might have made it difficult to interpret the relationship between years since diagnosis and severity levels or health statuses of patients with HD.
Two studies reported SF-6D estimates [18, 23]. In a longitudinal, observational study of patients with clinically diagnosed HD in 12 European countries, Hawton and colleagues [23] reported that SF-6D utility estimates declined with disease stage: TFC 13 − 11: 0.767 through TFC 2 − 0: 0.575. Utility estimates were not markedly lower than general population normative data for older people. For example, SF-6D utility was 0.68 compared with 0.73 for the general population in people aged 75–79 years. Rodriguez Santana et al. also reported that a decline in SF-6D utility corresponded with progression of disease stage, with early stage (TFC 13 − 7) yielding 0.61, through advanced stage (TFC 3 − 0) characterized by significant and total dependence on external care [28] experiences the most severe symptoms and require assistance in all activities of daily living, yielding 0.50. The decline in SF-6D utility with worsening TFC (0.61 to 0.50 from early to advanced stage) was smaller than the change in EQ-5D utility measured in the same study (0.72 to 0.37 from early manifest HD to advanced stage HD). A larger difference in EQ-5D utility between patients with HD and the general population was observed by Exuzides and colleagues [21] (0.66 and 0.81, respectively), suggesting that SF-6D may be less sensitive to the changes in HRQOL with HD progression than EQ-5D.
One vignette valuation study was identified [17]. In this study, health state descriptions (vignettes) were developed for different severities of HD chorea (with other manifestations remaining constant), and the health states were valued by general population participants using time trade-off methods. The mean (SD) utility values declined as chorea severity increased (mild: 0.64 [0.41]; mild/moderate: 0.48 [0.47]; moderate/severe: 0.26 [0.50]; severe: 0.07 [0.52]).
Among the 11 studies reviewed, 2 reported utility values assessed by proxy respondents on behalf of patients (Fig. 3). In a cross-sectional survey by Carlozzi et al. [27], the patient- and proxy-reported mean EQ-5D utility index scores were identical (both 0.6), although the mean proxy-reported TFC score was substantially lower than the mean patient-reported score (5.4 vs. 6.8), suggesting a disconnect in functioning capabilities by perspective. Similarly, in a cross-sectional survey by Rodriguez Santana et al. [18], proxy respondents reported similar mean EQ-5D scores as patients with mid-stage HD (0.62 [patient reported] vs. 0.66 [proxy reported]). However, large differences were reported in patients with advanced HD, where the mean (SD) score for patients was 0.42 (0.27) compared with 0.13 (0.31) for proxies. Part of this difference may be attributed to the study design in that proxy rating was used only for participants with a severe cognitive deficit.
Comparison of published utility scores for patients with HD by rater type. a. Utility Scores Measured by EQ-5D. b. Utility Scores Measured by SF-6D
HD = Huntington’s disease; EQ-5D = EuroQol 5-dimension; EQ-5D-5L = EuroQol 5-dimension 5-level; SF-6D = short-form 6-dimension; TFC = total functional capacity
Note: Error bars represent 95% confidence intervals derived from reported standard deviation and sample size (size of diamond represents the sample size). Country refers to location of residence of study participants
a Range for published mean EQ-5D and SF-6D utility for general US population of ages 35 to 64 years [49].
Discussion
This systematic literature review confirmed that published HSU scores estimated via generic preference-based utility measures (EQ-5D and SF-6D) are available for patients with HD. In studies that reported utility estimates for different stages of HD (such as early-, mid-, and late-stage HD), mean utility scores were numerically lower in patients with more advanced stages of manifest HD. Figure 4 illustrates the EQ-5D index scores associated with different severity levels of HD. While mean utility values for patients with prodromal or early manifest HD were between 0.89 and 0.72, mean utility values for patients with late-manifest HD ranged from 0.71 to 0.37. This variability in estimates among studies is problematic for researchers developing formal value assessments based on QALYs, as the different utility estimates would be expected to result in very different QALY estimates. While some of the variability may be explained (e.g., by differences in the definition of the severity categories, in the EQ-5D version and value set used, and/or in the use of proxy respondents for some patients in some studies), it is unclear which estimates are most appropriate to use in cost-effectiveness analyses.
Comparison of published EQ-5D index scores for patients with HD
HD = Huntington’s disease; EQ-5D = EuroQol 5-dimension; EQ-5D-5L = EuroQol 5-dimension 5-level; EQ-5D-5L = EuroQol 5-dimension 3-level; NR = not reported; TFC = total functional capacity
Note: Error bars represent 95% confidence intervals derived from reported standard deviation and sample size (size of diamond represents the sample size). Country refers to location of residence of study participants
a Range for published mean EQ-5D utility for the general US population ages 35 to 64 years [49]
The high mean EQ-5D index score in patients with early manifest HD reported in Carlozzi et al. [16] may indicate a challenge associated with using EQ-5D to quantify the impact of early manifest HD, as the estimate is close to published data for the general population matched by age and sex (0.81) [21]. However, Rodriguez Santana et al. [18] reported a somewhat lower EQ-5D index for early-stage disease (0.72). People in the early manifest stages of HD are likely to have cognitive, behavioral, and motor impairment, which may significantly impact their day-to-day functioning, QOL, and ability to stay independent [16, 30,31,32]. Additionally, those who have manifest HD may have significant cognitive impairment and not be fully aware of or able to accurately reflect on their own health status, and proxy reporting may be appropriate in such cases [33].
Our review confirmed that SF-6D–based utility estimates decreased with worsening HD severity in both studies (Fig. 5) [18, 23]. Hawton et al. [23] identified strong relationships between behavioral symptoms (such as sad mood, low self-esteem, guilt, disruptive or aggressive behavior, obsessions, hallucinations, irritable behavior) as well as functional independence and SF-6D utility values, but little relationship between cognitive symptoms or motor symptoms and SF-6D scores. This highlights a potential limitation of using SF-6D for capturing the effects of cognitive and motor impairments on the HSU in HD. Furthermore, the change in SF-6D utility with TFC decline was substantially smaller than the change in EQ-5D utility measured in Rodriguez Santana et al. [18]. SF-6D seems to be less sensitive than EQ-5D to the changes in HRQOL with HD symptom progression.
Cognitive symptoms are a key driver of disability and functioning deficits in HD, and often results in loss of work and independent functioning [32, 34]. Therefore, it is unclear whether EQ-5D is appropriate for measuring HRQOL impacts associated with cognitive impairment in HD. The EuroQol Group (which administers the EQ-5D instrument) has recognized that several studies have identified cognition as an area for which the psychometric properties of the EQ-5D may be weak [e.g. 35,36,37]; further research is ongoing. McGrath et al. [38] concluded that the EQ-5D descriptive system seemed to have poorer alignment with the impacts of Alzheimer’s Disease than other generic utility measures, and this also may be the case for the impacts of cognitive impairment in HD. Addition of cognition bolt-on dimensions has been shown to affect preference values for EQ-5D health states [39, 40], which suggests that preferences for cognition health states could be better measured than by the EQ-5D alone.
No value set (providing utility values for all the possible health states) is currently available for the EQ-5D including the cognition bolt-on, so this cannot be used to calculate QALYs. Cognitive changes often appear in the prodromal stage, prior to motor onset (diagnostic confidence level < 4) [41, 42] and can include a decline in executive function (including working memory, flexible thinking, and self-control), memory problems, and difficulty concentrating [34]. Further research into the appropriateness of the EQ-5D and whether other generic utility measures such as the Health Utilities Index, 15 Dimensions, or EQ Health and Wellbeing (EQ-HWB) instrument, which include specific dimensions for cognition and mental function, would be valuable. Vignette valuation studies or development of a new disease-specific utility measures could provide a possible solution given the lack of alternatives [43]; however, their use comes with recognized limitations [44, 45]. The EQ-HWB measure (currently under development) may also address this gap for measuring cognition [46].
Comparison of published SF-6D utility scores for patients with HD
HD = Huntington’s disease; SF-6D = short-form 6-dimension; TFC = total functional capacity
Note: Error bars represent 95% confidence intervals derived from reported standard deviation and sample size (size of diamond represents the sample size). Country refers to location of residence of study participants
a Range for published mean SF-6D utility for general US population of ages 35 to 64 years [49]
Conclusions
Health utility in HD has been studied using the EQ-5D, SF-6D, and vignette valuation. Studies identified in this systematic literature review showed high variability in published utility estimates, indicating substantial uncertainty in the existing data. It is unclear which reported utility values should be utilized in value assessments of new treatments for HD. There is some evidence to suggest that SF-6D may be less sensitive than EQ-5D to measuring HRQOL impairment in HD.
Further research is needed to better understand preferences and valuation in all stages and symptom clusters of HD, the impact of symptoms and manifestations of HD on patients, and the degree to which current generic utility measures are sensitive in capturing the impact of symptoms and manifestations of HD on patients’ HRQOL. Challenges in measuring health utility in patients with HD during functional decline may be due to the fact that cognitive impairment and behavioral changes are major symptoms that manifest in the early phase in the disease course. These symptoms are generally not captured by generic instruments such as the EQ-5D and SF-6D. Appropriateness of generic utility measures in HD should be explored.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- EQ-5D-5L:
-
EuroQol 5-Dimension 5-Level
- EQ-5D-3L:
-
EuroQol 5-Dimension 3-Level
- EQ-5D:
-
EuroQol 5-Dimension
- EQ-HWB:
-
EQ Health and Wellbeing
- H-QoL-I:
-
Huntington Quality of Life Instrument
- HD-PRO-TRIAD:
-
Huntington’s Disease-specific patient-reported outcome instrument of the HD symptom triad
- HD:
-
Huntington’s Disease
- HDQLIFE:
-
Huntington Disease Health-Related Quality of Life
- HDQoL:
-
Huntington’s Disease health-related Quality of Life
- HRQOL:
-
Health-related quality-of-life
- HSU:
-
Health state utility
- ISPOR:
-
Professional Society for Health Economics and Outcomes Research
- MeSH:
-
Medical Subject Headings
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QALY:
-
Quality-adjusted life-year
- QOL:
-
Quality of life
- SD:
-
Standard deviation
- SF-36:
-
36-Item Short-Form Survey
- SF-6D:
-
Short-Form 6-Dimension
- TFC:
-
Total Functional Capacity
- TTO:
-
Time trade-off
- VAS:
-
Visual analogue scale
References
Huntington’s Together. About Huntington’s disease. 2021. https://www.huntingtonsdiseasehcp.com/about-huntingtons-disease.html
Medina A, Mahjoub Y, Shaver L, Pringsheim T. Prevalence and incidence of Huntington’s disease: an updated systematic review and meta-analysis. Mov Disord. 2022.
Domaradzki J. The impact of Huntington disease on family carers: a literature overview. Psychiatr Pol. 2015;49(5):931–44.
Furby H, Siadimas A, Rutten-Jacobs L, Rodrigues FB, Wild EJ. Natural history and burden of Huntington’s disease in the UK: a population‐based cohort study. Eur J Neurol. 2022;29(8):2249–57.
Bayen E, de Langavant LC, Youssov K, Bachoud-Lévi A-C. Informal care in Huntington’s disease: assessment of objective-subjective burden and its associated risk and protective factors. Ann Phys Rehabil Med. 2023;66(4):101703.
Ferguson MW, Kennedy CJ, Palpagama TH, Waldvogel HJ, Faull RL, Kwakowsky A. Current and possible future therapeutic options for Huntington’s disease. J Cent Nerv Syst Disease. 2022;14:11795735221092517.
Drummond MF, Hartgers-Gubbels ES, Chambers M. Value Insider season 1 episode 1: the importance of payers and HTA: how did we end up here?(introduction to value)[podcast]. Int J Gen Med. 2022:7487–92.
Rutten-van Mölken, Maureen PMH, Hartgers-Gubbels E, Sophia CM. Value Insider season 1 episode 4: how are costs measured, and how are CEAs constructed and used?(CEA)[podcast]. Int J Gen Med. 2022:8055–61.
Devlin NJ, Hartgers-Gubbels ES, Chambers M. Value Insider season 1 episode 2: how to measure quality of life and utility?(QoL)[podcast]. Int J Gen Med. 2022:7773–9.
van Lonkhuizen PJ, Frank W, Heemskerk A-W et al. Quality of life, health-related quality of life, and associated factors in Huntington’s disease: a systematic review. J Neurol. 2023:1–22.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Carlozzi NE, Kratz AL, Downing NR, et al. Validity of the 12-item World Health Organization disability assessment schedule 2.0 (WHODAS 2.0) in individuals with Huntington disease (HD). Qual Life Res. 2015;24:1963–71.
Carlozzi NE, Hahn EA, Goodnight SM, et al. Patient-reported outcome measures in Huntington disease: quality of life in neurological disorders (Neuro-QoL) social functioning measures. Psychol Assess. 2018;30(4):450.
Carlozzi NE, Goodnight S, Kratz AL, et al. Validation of Neuro-QoL and PROMIS mental health patient reported outcome measures in persons with Huntington disease. J Huntingtons Dis. 2019;8(4):467–82.
Carlozzi NE, Schilling S, Lai J-S, et al. HDQLIFE: development and assessment of health-related quality of life in Huntington disease (HD). Qual Life Res. 2016;25:2441–55.
Claassen DO, Ayyagari R, Goldschmidt D, Zhou M, Leo S, Ribalov R. Defining utility values for chorea health states in patients with Huntington’s disease. Adv Ther. 2022;39(4):1784–93.
Rodriguez Santana I, Frank S, Doherty M, et al. Humanistic burden of Huntington Disease: evidence from the Huntington disease burden of illness study. Neurol Clin Pract. 2022;12(6):e172–80.
Dorey J, Clay E, Khemiri A, Belhadj A, Cubillo PT, Toumi M. The quality of life of Spanish patients with Huntington’s disease measured with H-QoL-I and EQ-5D. J Mark Access Health Policy. 2016;4(1):27356.
Quinn L, Hamana K, Kelson M, et al. A randomized, controlled trial of a multi-modal exercise intervention in Huntington’s disease. Parkinsonism Relat Disord. 2016;31:46–52.
Exuzides A, Matos JE, Patel AM, Martin AA, Ricker B, Bega D. Understanding the burdens associated with Huntington’s disease in manifest patients and care partners–comparing to Parkinson’s disease and the general population. Brain Sci. 2022;12(2):161.
Shaw E, Mayer M, Ekwaru P et al. Disease burden of Huntington’s disease (HD) on people living with HD and care partners in Canada. J Huntingtons Dis. 2022(Preprint):1–15.
Hawton A, Green C, Goodwin E, Harrower T. Health state utility values (QALY weights) for Huntington’s disease: an analysis of data from the European Huntington’s disease network (EHDN). Eur J Health Econ. 2019;20:1335–47.
Roos RAC. Huntington’s disease: a clinical review. Orphanet J Rare Dis. 2010;5(1):40.
Calvert M, Pall H, Hoppitt T, Eaton B, Savill E, Sackley C. Health-related quality of life and supportive care in patients with rare long-term neurological conditions. Qual Life Res. 2013;22:1231–8.
Hocaoglu M, Gaffan EA, Ho AK. The Huntington’s Disease health-related quality of life questionnaire (HDQoL): a disease‐specific measure of health‐related quality of life. Clin Genet. 2012;81(2):117–22.
Carlozzi NE, Victorson D, Sung V, et al. HD-PRO-TRIAD™ validation: A patient-reported instrument for the symptom triad of Huntington’s Disease. Tremor Other Hyperkinet Mov (N Y). 2014;4.
Wild EJ, Tabrizi SJ, Wood N. Huntington’s disease. Neurogenetics: A Guide for Clinicians Cambridge. Cambridge University Press; 2012. pp. 64–82.
Rowen D, Brazier J, Roberts J. Mapping SF-36 onto the EQ-5D index: how reliable is the relationship? Health Qual Life Outcomes. 2009;7(1):1–9.
Billet J, Levine A, Johannesen J, et al. Patient experiences in early Huntington’s disease-qualitative research to inform development of a patient-reported instrument of everyday functioning (P3-11.003). AAN Enterprises; 2022.
Petrillo J, Sawant R, Lee A et al. Cognitive Performance and self-reported functioning in Huntington’s disease: results from a real-world study. Presented at the CHDI Foundation 2023 Huntington’s Disease Therapeutics Conference; 2023. Dubrovnik, Croatia.
Watkins K, Purks J, Kumar A, Sokas RK, Heller H, Anderson KE. Huntington’s disease and employment: the relative contributions of cognitive and motor decline to the decision to leave work. J Huntington’s Disease. 2018;7(4):367–77.
Wolowacz SE, Briggs A, Belozeroff V, et al. Estimating health-state utility for economic models in clinical studies: an ISPOR good research practices task force report. Value Health. 2016;19(6):704–19.
Boileau NR, Stout JC, Paulsen JS, et al. Reliability and validity of the HD-PRO-Triad TM, a health-related quality of life measure designed to assess the symptom triad of Huntington’s disease. J Huntingtons Dis. 2017;6(3):201–15.
Geraerds AJ, Polinder S, Spronk I, et al. Sensitivity of the EQ-5D-5L for fatigue and cognitive problems and their added value in Q-fever patients. Qual Life Res. 2022;31(7):2083–92.
de Graaf JA, Kuijpers MM, Visser-Meily JM, Kappelle LJ, Post MW. Validity of an enhanced EQ-5D-5L measure with an added cognitive dimension in patients with stroke. Clin Rehabil. 2020;34(4):545–50.
Keetharuth AD, Hussain H, Rowen D, Wailoo A. Assessing the psychometric performance of EQ-5D-5L in dementia: a systematic review. Health Qual Life Outcomes. 2022;20(1):139.
Mcgrath C, Rofail D, Gargon E, Abetz L. Using qualitative methods to inform the trade-off between content validity and consistency in utility assessment: the example of type 2 diabetes and Alzheimer’s disease. Health Qual Life Outcomes. 2010;8(1):1–13.
Finch AP, Brazier J, Mukuria C. Selecting bolt-on dimensions for the EQ-5D: testing the impact of hearing, sleep, cognition, energy, and relationships on preferences using pairwise choices. Med Decis Mak. 2021;41(1):89–99.
Krabbe PF, Stouthard ME, Essink-Bot M-L, Bonsel GJ. The effect of adding a cognitive dimension to the EuroQol multiattribute health-status classification system. J Clin Epidemiol. 1999;52(4):293–301.
Sun Z, Ghosh S, Li Y, et al. A probabilistic disease progression modeling approach and its application to integrated Huntington’s disease observational data. JAMIA Open. 2019;2(1):123–30.
Stimming EF. A Roadmap for HD - What comes next? 2015. http://hdsa.org/wp-content/uploads/2015/07/HD-Roadmap2.pdf
Rowen D, Brazier J, Ara R, Azzabi Zouraq I. The role of condition-specific preference-based measures in health technology assessment. PharmacoEconomics. 2017;35:33–41.
Brazier J, Rowen D. NICE DSU Technical Support Document 11: alternatives to EQ-5D for generating health state utility values. 2011. Accessed 16 Mar 2017. http://www.nicedsu.org.uk
Rowen D, Brazier J, Wong R, Wailoo A. Measuring and valuing health-related quality of life when sufficient EQ-5D data is not available. Rep Decis Support Unit. 2020. https://www.sheffield.ac.uk/nice-dsu/methods-development/measuring-health-related-quality-life
Brazier J, Peasgood T, Mukuria C et al. The EQ health and wellbeing: overview of the development of a measure of health and wellbeing and key results. Value Health. 2022.
Claassen DO, Goldschmidt D, Zhou M, Leo S, Ribalov R, Ayyagari R. Defining utility values for chorea health states in patients with Huntington’s disease (4360). Neurology. 2021;96(15 Supplement):4360.
Rodriguez Santana I, Frank S, Fisher A, et al. POSB348 Differences in the health-related quality of life of Huntington’s disease patients by disease stage in the US and EU5 from the Huntington’s Disease Burden of Illness Study (HDBOI). Presented at the Value Health; 2022.
Fryback DG, Dunham NC, Palta M, et al. US norms for six generic health-related quality-of-life indexes from the national health measurement study. Med Care. 2007;45(12):1162.
Acknowledgements
Editorial support was provided by John Forbes, Bethan Pickering, and Jason Mathes of RTI Health Solutions. Logistical support was provided by Boston Strategic Partners, Inc. (funded by Sage Therapeutics, Inc.).
Funding
This study was funded by Sage Therapeutics, Inc. Sage has an ongoing clinical development program in Huntington's Disease for cognitive impairment.
Author information
Authors and Affiliations
Contributions
RS and JP contributed to study conception and design, and data analysis and interpretation. KP, SW, and NR contributed to study conception and design, collection and assembly of data, and data analysis. AK and HR contributed to study conception and design, and data interpretation. All authors reviewed and approved the final content of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Jennifer Petrillo, Ruta Sawant, and Aaron Koenig are employees of Sage Therapeutics, Inc, and may hold stock. Kyle Paret, Sorrel Wolowacz, and Naoko Ronquest are employees of RTI Health Solutions. Dr. Hugh Rickards is an employee of the University of Birmingham. This study was conducted by RTI Health Solutions under the direction of Sage Therapeutics, Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sawant, R., Paret, K., Petrillo, J. et al. Health state utility estimates for value assessments of novel treatments in Huntington’s disease: a systematic literature review. Health Qual Life Outcomes 22, 33 (2024). https://doi.org/10.1186/s12955-024-02242-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-024-02242-1