Abstract
Background
Positive results for clinical outcomes should be not only statistically significant, but also clinically significant. The minimum clinically important difference (MCID) is used to define the minimum threshold of clinical significance. The anchor-based method is a classical method for ascertaining MCID. This study aimed to summarise the design of the anchors of the anchor-based method by reviewing the existing research and providing references and suggestions.
Method
This study was mainly based on literature research. We performed a systematic search using Web of Science, PubMed, CNKI, Wanfang, and VIP databases. Two reviewers independently screened titles and abstracts to identify relevant articles. Data were extracted from eligible articles using a predefined data collection form. Discrepancies were resolved by discussion and the involvement of a third reviewer.
Result
Three hundred and forty articles were retained for final analysis. For the design of anchors, Subjective anchors (99.12%) were the most common type of anchor used, mainly the Patient’s rating of change or patient satisfaction (66.47%) and related scale health status evaluation items or scores (39.41%). Almost half of the studies (48.53%) did not assess the correlation test between the anchor and the research indicator or scale. The cut-off values and grouping were usually based on the choice of the anchor types. In addition, due to the large number of included studies, this study selected the most calculated SF-36 (28 articles) for an in-depth analysis. The results showed that the overall design of the anchor and the cut-off value were the same as above. The statistical methods used were mostly traditional (mean change, ROC). The MCID thresholds of these studies had a wide range (SF-36 PCS: 2–17.4, SF-36 MCS: 1.46–10.28), and different anchors or statistical methods lead to different results.
Conclusion
It is of great importance to select several types of anchors and to use more reliable statistical methods to calculate the MCID. It is suggested that the order of selection of anchors should be: objective anchors > anchors with established MCID in subjective anchors (specific scale > generic scale) > ranked anchors in subjective anchors. The selection of internal anchors should be avoided, and anchors should be evaluated by a correlation test.
Similar content being viewed by others
Introduction
In 1989, Jaeschke and Guyatt formally defined MCID as the smallest difference in score in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient’s management [1]. MCID can provide the basis for judging the clinical significance and clinical decision making of test results [2]. MCID was first proposed to better explain the clinical significance of the changes in the scores of patient-reported outcomes, such as the Quality of Life Scale. Later, the application of MCID was gradually extended to the 6 min walk test (6MWT) [3]、the fall rate [4]、the troponin [5], bridging the gap between statistics and clinical practice.
Currently, the commonly used MCID calculation methods include anchor-based method, distribution-based method, literature analysis method and expert consensus method. The anchor method is also called “external reference” method, that is, one anchor is selected as the external indicator and examines the relationship between scores on the instrument whose interpretation is under question (the target instrument) and some independent measure (an anchor) [6]. The distribution-based method is to ascertain MCID based on the distribution of sample data. Common indicators include 0.5SD, SEM, etc., but the estimation results obtained from a statistical perspective alone cannot scientifically explain the MCID. The literature analysis systematically reviews the published literature and synthesizes the results as the reference basis for MCID [7]. Obviously, it relies on the secondary literature, which should only play an auxiliary role in determining MCID. The expert consensus method is based on the group decision and consensus method to determine MCID [8], but the results only rely on the subjective judgment of experts and are also only used as an auxiliary method. Therefore, the anchor-based method is generally the preferred method for ascertaining the MCID. When it is difficult to find a suitable anchor, the distribution-based method is adopted, the distribution-based method is also commonly used. The literature analysis method and the expert consensus method are relatively niche approaches.
For the selection of anchors, the existing anchors can be divided into subjective anchors and objective anchors. A subjective anchor is a judgment about the changes in the disease in the past period, which is prone to multiple biases. The objective anchor can select laboratory examination indicators, physiological examination indicators and clinical outcomes [9]. However, whether the anchor selection is appropriate still depends on the correlation test between the anchor and the change in the scores on the research indicators or scale after the investigation, that is, the selected external anchor and the target measurement instrument should have a moderate correlation, and the correlation coefficient recommended by Revicki should be > 0.3–0.35 [7]. In addition, although recent studies have shown that the reliability and the degree of current state bias for the selected anchor can be assessed, it is still used as a subsequent verification method and is only limited to the transition ratings [10]. There is still a lack of research on anchor selection strategies. At the same time, after selecting the appropriate anchor, the patients need to be grouped according to the anchor cut-off value, which is the threshold value for dividing the patients into slight change groups and unchanged groups according to the anchor. However, the determination of the anchor cut-off value has not reached a consensus. For the statistical methods, traditional methods include mean change (within or between groups), ROC curve method, and linear regression method. In recent years, these methods have been criticized [11] and we have seen the emergence of a new method: the adjusted predictive modelling method [12], which is more reliable.
At present, there are a large number of articles that use the anchor-based method to calculate MCID. But for the anchor-based method, more attention is paid to the improvement of the statistical method, few people pay attention to the selection of anchors, which plays an important role in the calculation of MCID. Since there is no research on the anchor design of anchor-based method to calculate MCID, this study focused on the anchor design and aimed to summarise the anchor design rules in the existing research, so as to provide references for the standardised calculation of MCID by anchor-based method from a new perspective.
Method
Search and selection strategy
There are numerous articles in the field of MCID. We preliminarily searched for relevant research on MCID with “minimal clinically important difference” and found that research on calculating MCID generally clearly mentions MCID and the calculation method used (such as anchor-based or distribution-based method) in the title or abstract. In terms of setting search terms, we attempted various combinations and ultimately found that the articles retrieved using “minimal clinically important difference” and “anchor” as search terms best met our requirements. On this basis, the Chinese search terms take into account the differences in translation, and all use the subject term retrieval. Finally, Web of Science, PubMed, CNKI, Wanfang and VIP databases were retrieved, with the retrieval time limit from 2000 to June 2022. The following search strategy was used (taking PubMed as an example): (minimal clinically important difference[Title/Abstract]) AND (anchor[Title/Abstract]). The inclusion criteria: ①MCID was calculated by anchor-based method; ②The selected anchors and cut-off values were illustrated; ③The calculation process and results were relatively complete. The exclusion criteria: ①Repetitive literature; ② Irrelevant literature; ③Literature reviews; ④MCID was not calculated by anchor-based; ⑤Full text cannot be obtained.
Data extraction
Two reviewers independently screened titles and abstracts to identify relevant articles. Data were extracted from eligible articles using a predefined data collection form. Discrepancies were resolved by discussion and the involvement of a third reviewer. This study focused on the anchor design and specific statistical process (including the determination of cut-off value and the selection of statistical methods) in the existing research. Therefore, the final content of literature information extraction mainly includes: ①Basic information included in the study, including the first author, publication time, research purpose and disease field; ②Research indicators or scales; ③Anchor design: anchor selection and the determination of cut-off value and grouping.
Data analysis
Firstly, all studies were classified according to the anchor selection (subjective anchor or objective anchor). Since there were many types of subjective anchors, but there was no classification standard for subjective anchor types at present, based on the types of subjective anchors in existing research, divides them into two categories: ①Health status evaluation items or scores in the relevant scales of research indicators, such as the Health Transition Item of the SF-36(“In general, would you say your health is: excellent, very good, good, fair, or poor?”) and the scores of St George's Respiratory Questionnaire (SGRQ). ②Patient’s ratings of change or patient satisfaction, such as the Global Rating of Change Scale (GROC) and the Clinical Global Impression (CGI). Secondly, we summarised the determination of cut-offs and groupings according to different anchors. Finally, we selected one scale for further analysis.
Result
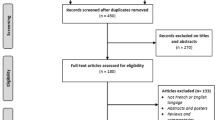
The literature screening process is shown in Fig. 1. This study finally included and summarised 340 literatures on anchor-based method of calculating MCID (Appendix 1).
Table 1 shows the basic information of the included literature. The existing research has covered many disease fields, mainly focusing on orthopedic diseases (40.29%), nervous system diseases (14.41%), respiratory system diseases (12.35%) and cancer fields (7.06%). The research indicators are mainly patient-reported outcomes (94.12%).
For the design of the anchor, most studies used a single anchor (73.24%) to calculate MCID, and some studies used multiple anchors (26.76%). The type of anchor selected was mainly the subjective anchor (99.12%), it mainly includes: ①Items of health status evaluation or scores in the scale related to research indicators or scales (39.41%). There mainly were specific scale② The patient’s rating of change or patient satisfaction (66.47%). The articles using objective anchors (5.58%) are rarely used, and most of them use subjective anchors together to calculate MCID. In addition, nearly half (48.53%) of the included studies did not evaluate correlation tests between anchors and research indicators and scales.
The determination of the anchor cutoff value and grouping is shown in Table 2 (according to the situation of most studies summarised in the included study). The determination of the cut-off value and grouping was related to the selected anchor. For the anchor with MCID established, the MCID of the anchor was the cut-off value; for rank anchors, 5, 7 or 15 point Likert scales were most commonly used, and certain grade options were selected as the cut-off value.
Due to the large number of studies included, only the SF-36 (n = 28) with the highest number of calculations was selected for detailed analysis. Table 3 shows the design of the anchors for the SF-36. For the design of the anchor, the most commonly used anchor is the patient’s change rating of change with 5, 7 or 15 point Likert scales (n = 14), followed by the Healthy Transition Item of SF-36 (n = 9), and finally the related scale scores (n = 5). More than half of the articles (n = 15) did not test the correlation between the anchor and the SF-36 scores. The determination of cut-off values and grouping mostly conformed to the conditions summarised in Table 2, but two articles were special, they were anchored by SF-36 scores and its physician function scores, and the results of their statistical distribution were taken as cut-off values.
For the selection of statistical methods, the traditional methods were still mainly used, among which the mean change was the most, followed by the ROC curve, and the linear regression method is the least. Most studies calculated the PCS and MCS scores of the SF-36 scale, where the MCID threshold range of the PCS was 2–17.4 and the MCID threshold range of the MCS was 1.46–10.28. And different anchors or statistical methods give different results.
Discussion
This study systematically summarised and analysed the anchor design based on the existing research of using anchor-based method to ascertain MCID. Although this study did not fully cover all the research, it was representative enough. For the design of anchors, the existing research mainly used subjective anchors. In general, although the types of anchors used in the existing research were different, some rules can still be summarised, which can provide references and suggestions for further research.
For the design of the anchor, firstly, the existing research mainly used subjective anchors. This could be due to the fact that the existing research objects were still mainly PROs, and the disease field involved was mainly functional diseases. Therefore, there are few objective indicators that can reflect changes in diseases, making it difficult to find appropriate objective anchors. However, from the perspective of methodology, the results of MCID estimation using objective anchors are more stable and reliable than those using subjective anchors. This is because subjective anchors are prone to memory bias, which can lead to some bias in the estimated MCID. Secondly, some existing research has used the internal items of the research scale as anchors. For example, when ascertaining the MCID of SF-36, using its internal Health Transition Item or its dimension scores as the anchor, this may be problematic because the “externality” of the anchor-based method is not reflected, and the estimation results may not be reliable enough. In addition, this study found that almost half of the included literature did not test the correlation between anchors and research scales or indicators, which may also lead to unreliable results. In this regard, it is suggested that the priority in selecting anchors should be: objective anchor > anchor with MCID established in subjective anchor (special scale > generic scale) > rank variable anchor in subjective anchor (the cut-off point value of rank anchor is difficult to determine compared to that of MCID established anchor)), and avoid selecting internal anchor. The selected anchor must assess the correlation test (correlation coefficient > 0.3) before selecting the anchor to ascertain the MCID. If it does not reach 0.3, consider using the distribution-based method to ascertain MCID. At the same time, it is recommended that multiple anchors can be selected to ascertain MCID because one of the major shortcomings of the anchor-based method is that the estimated MCID may change with the change of the anchor, and when ascertaining the MCID of different dimensions of a scale, the correlation between the same anchor and different dimensions of the scale may not be the same, and the robustness and complementarity of the results obtained by checking the use of multiple anchors, the MCID can be estimated more accurately [41].
After selecting the appropriate anchor, the patients shall be grouped according to the cut-off values, and then the MCID can only be further calculated using the anchor-based method if the groups are statistically significant and can represent clinically significant changes [42]. A common limitation was the small sample size in the anchor categories. If the number of patients in each anchor category is insufficient, then the resulting MCID may not be reliable and robustness in this case is questionable. The appropriate sample size of each category should be calculated systematically before the investigation, and interim analysis and determination can be carried out during the investigation. If the sample size of the MCID group is small, a larger sample size should be considered [41]. In addition, because there are many types of rank anchors, there is no unified consensus on the cut-off values. The cut-off value and grouping in existing research can be used as a reference (Table 2). It can be adjusted flexibly according to the research design. For example, if the number of people choosing a grade option in the rank anchor is too low, it may be considered to combine it with its neighbouring rank options for the calculation. Moreover, there were two studies in which the MCID of the SF-36 was specifically determined, with the cut-off values based directly on the statistical distribution of their scores. In fact, it can be understood as using the distribution-based method to estimate the MCID of the anchor, but the distribution-based method is not accurate enough to estimate the MCID, so it may be questionable.
Through an in-depth analysis of the statistical process of the MCID of the SF-36 scale, we found that the current selection of statistical methods was still mainly the traditional method, and the results of its MCID threshold values (taking SF-36 PCS and SF-36 MCS as examples) range were relatively large, and the results of MCID were slightly different due to different anchors or statistical methods. Therefore, it is of great significance to select more types of anchors and use more reliable statistical methods to calculate the MCID.
In summary, further research is needed to standardise the anchor design of the anchor-based method, for example by creating a standardised list of anchor choices and priority levels according to different disease types or study indicators, and by specifying the corresponding cut-off values. And more studies should be conducted using the standardised anchor-based method to calculate the MCID. This study also has some limitations. First, all the literature on anchor-based method calculation of MCID are not available. Second, due to the large scope of research, this study did not conduct in-depth mining on the MCID calculation process of scales or clinical indicators in some specific disease areas, which still needs further exploration.
Conclusion
This study systematically searched the published literature on MCID calculation using the anchor-based method. And the anchor design was summarised and analysed. The results showed that for the design of anchors, subjective anchors were mainly adopted, which were mainly the patient’s rating of change or patient satisfaction and related scale health status evaluation items or scores. Almost half of the studies did not assess the correlation test between the anchor and the research indicator or scale. The cut-off values and grouping were usually based on the selection of the anchor types. Due to the large number of included studies, this review selected the most calculated SF-36 (28 articles) for an in-depth analysis. The results showed that the overall design of the anchor and the cut-off value were the same as above. The statistical methods were mostly the traditional method (mean change、ROC). The MCID threshold values of these studies had a wide range (SF-36 PCS: 2–17.4, SF-36 MCS: 1.46–10.28), and different anchors or statistical methods lead to different results. It is important to select different types of anchors and use more reliable statistical methods to calculate the MCID. The priority of anchor selection is suggested to be objective anchors > anchor with MCID established in subjective anchors (special scale > generic scale) > rank anchor in subjective anchors. Internal anchors should be avoided and anchors should be evaluated by correlation test.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MCID:
-
Minimum Clinically Important Difference
- SGRQ:
-
St George's Respiratory Questionnaire
- GROC:
-
Global Rating of Change Scale
- CGI:
-
Clinical Global Impression
- PRO:
-
Patient-reported Outcome
References
Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–15. https://doi.org/10.1016/0197-2456(89)90005-6
YANG Lihong, XIAO Jingmin, LIU Shaonan, WU Daron, GE Long, GUO Xinfeng. Determination of the Minimal Clinically Important Difference and Its Application. Journal of Guangzhou University of Traditional Chinese Medicine. 2022;39(04):959–965. https://doi.org/10.13359/j.cnki.gzxbtcm.2022.04.037
Polkey MI, Spruit MA, Edwards LD, et al. Six-minute-walk test in chronic obstructive pulmonary disease: minimal clinically important difference for death or hospitalization. Am J Respir Crit Care Med. 2013;187(4):382–6. https://doi.org/10.1164/rccm.201209-1596OC.
Henderson EJ, Morgan GS, Amin J, Gaunt DM, Ben-Shlomo Y. The minimum clinically important difference (MCID) for a falls intervention in Parkinson’s: A delphi study. Parkinsonism Relat Disord. 2019;61:106–10. https://doi.org/10.1016/j.parkreldis.2018.11.008.
Täger T, Giannitsis E, Greve K, et al. Long-term biological variation of high-sensitivity cardiac troponin T using minimal important differences and reference change values in stable outpatients with cardiovascular disease. Clin Biochem. 2019;67:7–11. https://doi.org/10.1016/j.clinbiochem.2019.03.003.
Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR. Methods to explain the clinical significance of health status measures. Mayo Clin Proc. 2002;77(4):371–83. https://doi.org/10.4065/77.4.371.
Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61(2):102–9. https://doi.org/10.1016/j.jclinepi.2007.03.012.
van der Heijde D, Lassere M, Edmonds J, Kirwan J, Strand V, Boers M. Minimal clinically important difference in plain films in RA: group discussions, conclusions, and recommendations. OMERACT Imaging Task Force J Rheumatol. 2001;28(4):914–7.
Lihong YANG, Shaonan LIU, Daron WU, Long GE, Xinfeng GUO. Minimal clinically important difference: terminology and estimated methods. Chin J Evid Based Med. 2020;20(11):1345–52.
Griffiths P, Terluin B, Trigg A, Schuller W, Bjorner JB. A confirmatory factor analysis approach was found to accurately estimate the reliability of transition ratings. J Clin Epidemiol. 2022;141:36–45. https://doi.org/10.1016/j.jclinepi.2021.08.029.
Terwee CB, Peipert JD, Chapman R, et al. Minimal important change (MIC): a conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual Life Res. 2021;30(10):2729–54. https://doi.org/10.1007/s11136-021-02925-y.
Terluin B, Eekhout I, Terwee CB. The anchor-based minimal important change, based on receiver operating characteristic analysis or predictive modeling, may need to be adjusted for the proportion of improved patients. J Clin Epidemiol. 2017;83:90–100. https://doi.org/10.1016/j.jclinepi.2016.12.015.
Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45(4):384–91. https://doi.org/10.1002/1529-0131(200108)45:4%3c384::Aid-art352%3e3.0.Co;2-0.
Escobar A, Quintana JM, Bilbao A, Aróstegui I, Lafuente I, Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage. 2007;15(3):273–80. https://doi.org/10.1016/j.joca.2006.09.001.
Bilbao A, Quintana JM, Escobar A, et al. Responsiveness and clinically important differences for the VF-14 index, SF-36, and visual acuity in patients undergoing cataract surgery. Ophthalmology. 2009;116(3):418–424.e1. https://doi.org/10.1016/j.ophtha.2008.11.020.
Coteur G, Feagan B, Keininger DL, Kosinski M. Evaluation of the meaningfulness of health-related quality of life improvements as assessed by the SF-36 and the EQ-5D VAS in patients with active Crohn’s disease. Aliment Pharmacol Ther. 2009;29(9):1032–41. https://doi.org/10.1111/j.1365-2036.2009.03966.x.
Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. The spine journal : official journal of the North American Spine Society. 2010;10(6):469–74. https://doi.org/10.1016/j.spinee.2010.02.007.
Merkies IS, van Nes SI, Hanna K, Hughes RA, Deng C. Confirming the efficacy of intravenous immunoglobulin in CIDP through minimum clinically important differences: shifting from statistical significance to clinical relevance. J Neurol Neurosurg Psychiatry. 2010;81(11):1194–9. https://doi.org/10.1136/jnnp.2009.194324.
Xiaoxia L. Study on the minimum clinically important difference of health status measurement instrument for cardiac insufficiency, MA Thesis. Bejing University of Chinese Medicine; 2010. https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD2010&filename=2010145180.nh.
Ingram M, Choi YH, Chiu CY, et al. USE OF THE MINIMAL CLINICALLY IMPORTANT DIFFERENCE (MCID) FOR EVALUATING TREATMENT OUTCOMES WITH TMJMD PATIENTS: A PRELIMINARY STUDY(). J Appl Biobehav Res. 2011;16(3–4):148–66. https://doi.org/10.1111/j.1751-9861.2011.00068.x.
Auffinger BM, Lall RR, Dahdaleh NS, et al. Measuring surgical outcomes in cervical spondylotic myelopathy patients undergoing anterior cervical discectomy and fusion: assessment of minimum clinically important difference. PloS one. 2013;8(6):e67408. https://doi.org/10.1371/journal.pone.0067408
Lauche R, Langhorst J, Dobos GJ, Cramer H. Clinically meaningful differences in pain, disability and quality of life for chronic nonspecific neck pain - a reanalysis of 4 randomized controlled trials of cupping therapy. Complement Ther Med. 2013;21(4):342–7. https://doi.org/10.1016/j.ctim.2013.04.005.
Antonescu I, Scott S, Tran TT, Mayo NE, Feldman LS. Measuring postoperative recovery: what are clinically meaningful differences? Surgery. 2014;156(2):319–27. https://doi.org/10.1016/j.surg.2014.03.005.
Carlson ML, Tveiten Ø V, Yost KJ, Lohse CM, Lund-Johansen M, Link MJ. The Minimal Clinically Important Difference in Vestibular Schwannoma Quality-of-Life Assessment: An Important Step beyond P < .05. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2015;153(2):202–8. https://doi.org/10.1177/0194599815585508
Zhou F, Zhang Y, Sun Y, Zhang F, Pan S, Liu Z. Assessment of the minimum clinically important difference in neurological function and quality of life after surgery in cervical spondylotic myelopathy patients: a prospective cohort study. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2015;24(12):2918–23. https://doi.org/10.1007/s00586-015-4208-3.
Erez G, Selman L, Murtagh FE. Measuring health-related quality of life in patients with conservatively managed stage 5 chronic kidney disease: limitations of the Medical Outcomes Study Short Form 36: SF-36. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2016;25(11):2799–809. https://doi.org/10.1007/s11136-016-1313-7.
Park KB, Shin JS, Lee J, et al. Minimum Clinically Important Difference and Substantial Clinical Benefit in Pain, Functional, and Quality of Life Scales in Failed Back Surgery Syndrome Patients. Spine. 2017;42(8):E474–e481. https://doi.org/10.1097/brs.0000000000001950.
Badhiwala JH, Witiw CD, Nassiri F, et al. Minimum Clinically Important Difference in SF-36 Scores for Use in Degenerative Cervical Myelopathy. Spine. 2018;43(21):E1260–e1266. https://doi.org/10.1097/brs.0000000000002684.
Yuksel S, Ayhan S, Nabiyev V, et al. Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? The spine journal : official journal of the North American Spine Society. 2019;19(1):71–8. https://doi.org/10.1016/j.spinee.2018.07.005.
Brigden A, Parslow RM, Gaunt D, Collin SM, Jones A, Crawley E. Defining the minimally clinically important difference of the SF-36 physical function subscale for paediatric CFS/ME: triangulation using three different methods. Health Qual Life Outcomes. 2018;16(1):202. https://doi.org/10.1186/s12955-018-1028-2.
Kato S, Oshima Y, Matsubayashi Y, Taniguchi Y, Tanaka S, Takeshita K. Minimum clinically important difference in outcome scores among patients undergoing cervical laminoplasty. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019;28(5):1234–41. https://doi.org/10.1007/s00586-019-05945-y.
Carton P, Filan D. Defining the Minimal Clinically Important Difference in Athletes Undergoing Arthroscopic Correction of Sports-Related Femoroacetabular Impingement: The Percentage of Possible Improvement. Orthop J Sports Med. 2020;8(1):2325967119894747. https://doi.org/10.1177/2325967119894747.
Ogura K, Bartelstein MK, Yakoub MA, Nikolic Z, Boland PJ, Healey JH. Minimal clinically important differences in SF-36 global score: Current value in orthopedic oncology. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2021;39(10):2116–23. https://doi.org/10.1002/jor.24944.
Yao M, Xu BP, Li ZJ, et al. A comparison between the low back pain scales for patients with lumbar disc herniation: validity, reliability, and responsiveness. Health Qual Life Outcomes. 2020;18(1):175. https://doi.org/10.1186/s12955-020-01403-2.
Pintér D, Janszky J, Kovács N. Minimal Clinically Important Differences for Burke-Fahn-Marsden Dystonia Rating Scale and 36-Item Short-Form Health Survey. Movement disorders : official journal of the Movement Disorder Society. 2020;35(7):1218–23. https://doi.org/10.1002/mds.28057.
Kawakami D, Fujitani S, Morimoto T, et al. Prevalence of post-intensive care syndrome among Japanese intensive care unit patients: a prospective, multicenter, observational J-PICS study. Critical care (London, England). 2021;25(1):69. https://doi.org/10.1186/s13054-021-03501-z.
Kang M, Veeraraghavan S, Martin GS, Kempker JA. An updated approach to determine minimal clinically important differences in idiopathic pulmonary fibrosis. ERJ open research. 2021;7(4). https://doi.org/10.1183/23120541.00142-2021
Filan D, Carton P. Chronic Hip Injury Has a Negative Emotional Impact on the Male Athlete With Femoroacetabular Impingement. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2021;37(2):566–76. https://doi.org/10.1016/j.arthro.2020.10.035.
Fu V, Weatherall M, McNaughton H. Estimating the minimal clinically important difference for the Physical Component Summary of the Short Form 36 for patients with stroke. J Int Med Res. 2021;49(12):3000605211067902. https://doi.org/10.1177/03000605211067902.
Hara T, Kogure E, Iijima S, Fukawa Y, Kubo A, Kakuda W. Minimal clinically important difference in postoperative recovery among patients with gastrointestinal cancer. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2022;30(3):2197–205. https://doi.org/10.1007/s00520-021-06632-9.
Ousmen A, Touraine C, Deliu N, et al. Distribution- and anchor-based methods to determine the minimally important difference on patient-reported outcome questionnaires in oncology: a structured review. Health Qual Life Outcomes. 2018;16(1):228. https://doi.org/10.1186/s12955-018-1055-z.
Trøstrup J, Andersen H, Kam CAM, Magnusson SP, Beyer N. Assessment of Mobility in Older People Hospitalized for Medical Illness Using the de Morton Mobility Index and Cumulated Ambulation Score-Validity and Minimal Clinical Important Difference. J Geriatr Phys Ther. 2019;42(3):153–60. https://doi.org/10.1519/jpt.0000000000000170.
Acknowledgements
Not applicable
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Yu Zhang and Yuankai Huang independently screened titles and abstracts to identify relevant articles. Data were extracted from eligible articles using a predefined data collection form. Discrepancies were resolved by discussion and the involvement of a third reviewer Xiaoyu Xi. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Y., Xi, X. & Huang, Y. The anchor design of anchor-based method to determine the minimal clinically important difference: a systematic review. Health Qual Life Outcomes 21, 74 (2023). https://doi.org/10.1186/s12955-023-02157-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-023-02157-3