Abstract
Background
No previous studies have examined the associations between changes in objectively-measured physical behaviours with follow-up QoL in older adults. Based on cross-sectional evidence, it is biologically plausible that such associations exist. If so, this bolsters the case for the commissioning of activity interventions and for including QoL as an outcome in trials of such interventions.
Methods
We assessed physical behaviours (total physical activity, moderate-to-vigorous physical activity (MVPA), light physical activity, total sedentary time and prolonged sedentary bout time) for 7 days using hip-worn accelerometers at baseline (2006–2011) and follow-up (2012–2016) and health-related quality-of-life (QoL) using EQ-5D questionnaires at follow-up in 1433 participants (≥ 60 years) of the EPIC (European Prospective Investigation into Cancer)-Norfolk study. The EQ-5D summary score was used, with 0 as the worst to 1 as best perceived quality-of-life. We evaluated the prospective associations of baseline physical behaviours with follow-up QoL, and of changes in behaviours with follow-up QoL using multi-level regression.
Results
On average, MVPA decreased by 4.0 min/day/year (SD 8.3) for men and 4.0 min/day/year for women (SD 12.0) between baseline and follow-up. Total sedentary time increased by an average 5.5 min/day/yr (SD 16.0) for men and 6.4 min/day/yr (SD 15.0) for women between baseline and follow-up. Mean (SD) follow-up time was 5.8 (1.8) years.
We found that higher baseline MVPA and lower sedentary time was associated with higher subsequent QoL (e.g. 1 h/day greater baseline MVPA was associated with 0.02 higher EQ-5D score, 95% CI 0.06, 0.36). More pronounced declines in activity were associated with worse Hr-QoL (0.005 (95% CI 0.003, 0.008) lower EQ-5D per min/day/yr decrease in MVPA). Increases in sedentary behaviours were also associated with poorer QoL (0.002 lower EQ-5D, 95% CI -0.003, -0.0007 per hour/day/yr increase in total sedentary time).
Conclusions
Promotion of physical activity and limiting sedentary time among older adults may improve quality-of-life, and therefore this relationship ought to be included in future cost effectiveness analyses so that greater commissioning of activity interventions can be considered.
Similar content being viewed by others
Introduction
More physical activity and less sedentary time are associated with reduced risk of morbidity such as diabetes, depression, cardiac disease and cancer, and premature mortality [1,2,3,4,5,6,7]. However, a significant proportion of UK older adults do not meet current physical activity guidelines [8]. The most recent UK guidelines state older adults should aim to accumulate 150 min of moderate intensity aerobic activity per week [9]. Additionally, they state older adults should break up prolonged periods of being sedentary with light activity when physically possible, or at least with standing, as this has distinct health benefits for older people.
Interventions to prevent declines in physical activity and increases in sedentary time have not achieved sustained changes in behaviour beyond 12 months [10,11,12,13]. Health-related quality of life (QoL) is a comprehensive measure of health and wellbeing, which can be used to assess healthy ageing, complementing standard measures of mortality and morbidity [14]. Lower QoL is inversely associated with risk of hospitalisation [15], adverse post-hospitalisation outcomes [16], and premature mortality [17]. It is also used to inform decisions about the commissioning of health care. Effects of interventions to improve QoL in older adults have varied [18].
Understanding the relationship of physical activity and sedentary time with QoL enables assessment of whether and how changes in activity might translate into improvements in QoL. In future, this could inform interpretation of cost-effectiveness analyses underpinning resource allocation decisions. Previous assessments of the cost-effectiveness of interventions to promote activity may have underestimated their value, as effects on QoL are commonly not taken into account. Instead the focus has traditionally been on mortality and disease incidence outcomes [19]. If there is a strong and causal relationship between physical activity and QoL, this could strengthen the case for investment and commissioning of interventions to promote activity. Further, given that QoL may be more important to older adults than risk of morbidity and premature mortality, such research could be incorporated into motivational messaging in activity-based interventions.
It is biologically plausible that better physical behaviour profiles are causally associated with subsequent Hr-QoL. For example, higher physical activity levels are associated with better physical function/mobility [20, 21], ability to do self-care [22] and other usual activities [23], reduced levels of pain [24] and anxiety/depression [25]. These are all domains of Hr-QoL, and could be potential mechanisms through which physical behaviours may effect Hr-QoL. Higher levels of physical activity and less time spent in sedentary behaviours leads to lower risk of many chronic conditions. These conditions can themselves lead to deterioration in components of Hr-QoL. For example, high levels of physical activity are associated with a lower risk of arthritis (a cause of pain, a component of Hr-QoL) and cognitive decline (a cause of reduced ability to self-care) [26, 27]. Reduced sedentary time and increased physical activity are also linked to improved social functioning, reduced loneliness and social isolation [28] which could all promote better Hr-QoL.
Our current understanding of these relationships is limited in four important ways. Firstly, studies have been almost exclusively cross-sectional limiting interpretation of causality. Secondly, the few existing longitudinal studies have all used subjective rather than more precise and less biased objectively-assessed measures of activity [29,30,31,32,33,34,35]. There have been no longitudinal studies of associations between QoL and objectively-measured activity in adults. Examining longitudinal associations allows us to examine whether there is a directional nature to any observed association, and therefore gives added insight in comparison to cross-sectional analysis. Thirdly, older adults have been neglected in studies of these associations from our review of the literature [36,37,38].
Finally, there are no studies examining the prospective relationship between prolonged sedentary bouts and QoL. Prolonged sedentary bouts are thought to be particularly detrimental to health independent of total time spent sedentary [31,32,33,34,35] though the mechanism of this remains unclear. Prolonged sedentary bouts are associated with worse metabolic health outcomes such as metabolic syndrome [36,37,38] and poor glycaemic control [31, 39]. Therefore, less time in prolonged sedentary bouts could theoretically lead to better QoL through fewer chronic diseases. The advent of objective measures of sedentary time has allowed measurement of sedentary patterns such as prolonged sedentary bouts. Though traditionally researchers have investigated the risk factor of total daily sedentary time, more recently there has been interest in looking at time spent in prolonged bouts (e.g. time in bouts of more than 30 min) as it may be easier to get individuals to break up prolonged bouts than reduce total time (e.g. frailer older adults who are unable to participate in physical activity or stand for prolonged periods).
There is a need for large longitudinal studies that utilise objectively-assessed measures of physical activity and sedentary time in this population. We aimed to describe the prospective associations between accelerometer-assessed activities (total physical activity, total sedentary time, prolonged sedentary bout time, light physical activity (LPA), moderate-to-vigorous intensity PA (MVPA) and QoL in a large sample of older adults.
Methods
We used data from the EPIC-Norfolk (European Prospective Investigation into Cancer-Norfolk) study, a prospective cohort of over 25,500 adults living in the UK [40] who participated in up to five health-checks. Participants were similar to a national population sample in terms of anthropometry, serum lipids, and blood pressure (Health Survey for England) [41]. We used data from two assessment time-points, hereafter described as baseline (2006–2011) and follow-up (2012–2016). Physical behaviour was assessed by accelerometer at baseline (n = 3,784) and follow-up (n = 4,788). QoL was measured by questionnaire at follow-up (n = 2,113). We restricted our analyses to participants who were aged ≥ 60 years at baseline and who had valid accelerometry and QoL data at relevant assessments.
Accelerometry
Estimates of physical behaviours were collected via hip-mounted accelerometers at baseline and follow-up. At baseline, participants wore uniaxial accelerometers (Actigraph GT1M™, USA). At follow-up, participants wore triaxial accelerometers (GT3X™, Actigraph, USA). Participants were asked to wear accelerometers on their right hip for seven days except when bathing, swimming or sleeping. Harmonisation of the data from the two accelerometers was completed using previously described methods [42, 43] and activity was integrated into 60-s epochs before summation [44, 45]. Non-wear time was defined as continuous zero counts of ≥ 90 min [46]. In order to deal with overnight wear, we overlaid self-report sleep timings at epoch level for days with wear-time > 19 h and excluded data accordingly. Variables derived from accelerometry data were total physical activity, MVPA, LPA, total sedentary time, and prolonged sedentary bout time (bouts ≥ 30 min). Total physical activity was calculated by total activity counts divided by wear time (counts/minute). The cut-offs used to define intensity-related behaviours were < 100 counts per minute (cpm) for sedentary time, 100–808 cpm for LPA, and ≥ 809 cpm for MVPA [42, 46,47,48,49,50], in units minutes/day. We calculated the rate of change of accelerometer-assessed variables (min/day/year) as the difference between values at baseline and follow-up divided by the time between assessments. Participants with ≥ 4 days of valid wear-time (≥ 10 h of wear time each day) for each assessment were included in this analysis.
QoL
QoL was measured in follow-up using the EQ-5D-3L, a validated self-completion questionnaire [51] which was mailed to participants. The EQ-5D descriptive system includes domains of mobility, self-care, usual activities, pain and anxiety/depression. It can be summarised using a single value, which reflects how good or bad a person’s QoL is according to the preferences of the general population of a country [52, 53], with 0 as the worst to 1 as best perceived QoL. We derived the summary value using previously described methods utilising the UK value set cited in the EQ5D3L guide.
Covariates
Baseline sociodemographic factors were age, sex, smoking status (never, former, current), body mass index (BMI), and occupation (Registrar-General's Social Classification). We also utilised job status (job vs no job), educational status (O level or lower vs A level or higher), chronic disease status (history of either myocardial infarction, stroke, cancer or diabetes mellitus), marital status (single, married, widowed, separated, divorced) and household financial circumstances (“in general, do you or your family have more money than you needed, just enough or not enough?”). All these were assessed via self-completed questionnaire. BMI (kg/m2) was calculated based on weight and height, which were measured by trained staff following standard operating procedures.
Statistical analyses
We calculated descriptive statistics for all socio-demographic, activity and QoL measures of interest and examined differences between participants included in the main analyses and those that we excluded. We also calculated descriptive statistics for annual change in physical behaviour measures.
We undertook longitudinal analyses using multivariable linear regression to estimate firstly, the association between baseline physical behaviours and follow-up QoL, and secondly, the association between change in behaviours (baseline to follow-up) and follow-up QoL.
We examined each of these associations using three models. We accounted for factors such as age and sex, which are likely confounders, by fitting them into model 2. Older age and being female have been associated with lower Hr-QoL, lower MVPA and higher sedentary time [54, 55]. Other biologically plausible confounders identified a priori were added into model 3. Model 1 was adjusted for season at baseline and follow-up [56, 57], time difference between baseline and follow-up, and accelerometer wear time. Model 2 was additionally adjusted for age and sex. Model 3 was the same as Model 2 but with additional adjustment for baseline job status, smoking status, BMI, chronic disease status, occupational class, marital status, education level and household financial circumstances. For the analyses of change in physical behaviour, adjustment was also made for baseline behaviour across all models. In order to further contextualise our results, we performed a regression of QoL against age, with adjustment for sex, to estimate QoL decline per chronological year of age.
In sensitivity analyses, we examined if valid day inclusion criteria (≥ 5 vs ≥ 4 days of valid data) and behaviour intensity cut-points (i.e. using 809 cpm vs 2,020 cpm to delineate LPA and MVPA) influenced our results. All analyses were conducted in STATA 15.0 (StataCorp, TX, USA) using complete case analyses.
Results
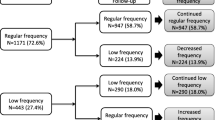
There were 1584 participants adults aged ≥ 60 years that had QoL and activity measurements at appropriate assessments making them eligible for inclusion. Of these, 10 individuals at baseline and 15 individuals at follow-up were excluded due to having < 4 valid days of accelerometry data. A further 126 participants were excluded due to missing covariates, leaving a total of 1433 participants (90%). Participants had an average (SD) age of 70 [7] years at baseline and 54.7% were women (Table 1). Included participants were socio-demographically similar to those excluded (Supplementary Table 1).
Mean (SD) time between baseline and follow-up was 5.8 (1.8) years. On average, MVPA decreased by 4.0 min/day/year (SD 8.3) for men and 4.0 min/day/year for women (SD 12.0) between baseline and follow-up (Table 2). LPA decreased by 4.0 min/day (SD11) and 3.5 min/day for women (SD 8.8). Total sedentary time increased by an average 5.5 min/day/yr (SD 16.0) for men and 6.4 min/day/yr (SD 15.0) for women between baseline and follow-up. Prolonged sedentary bout time increased by 9.3 min/day (SD 19.8) for men and 9.0 min/day for women (SD 16.8). After adjustment for sex, participants had a 0.0069 lower EQ-5D score per year of older age (95% CI -0.0083, -0.0054).
Association of baseline activity with follow-up QoL
Higher baseline total physical activity and MVPA were associated with higher subsequent QoL (Fig. 1, Supplementary Table 2). Specifically, a 100 cpm/day higher total physical activity and an hour/day higher MVPA were associated with a 0.02 unit (95% CI 0.005, 0.03) and a 0.02 unit (95% CI 0.06, 0.36) higher EQ-5D score, respectively. Higher total sedentary time was associated with lower subsequent QoL (1 h/day higher sedentary time was associated with 0.01 unit higher EQ5D score, 95% CI -0.02, -0.004). However, LPA and prolonged sedentary bouts were not statistically significantly associated with Hr-QoL.
Association between physical behaviours at and quality of life for included participants from the EPIC-Norfolk study 2006–2016 (n = 1584). For all panels, MVPA is in green, LPA is in blue, ST is in red and Prolonged ST bouts is in orange. Beta is indicated by central square, 95% CI is indicated by the line. Baseline measures were performed 2006–2011 and follow-up measures were done 2012–2016. In Panel A, results are from model 3 which are adjusted for season and wear time at baseline, age, sex, job status, smoking status, occupational class, retirement status, BMI, ethnicity, chronic disease status, marital status and household financial status. In Panel B, results are additionally adjusted for season and accelerometer wear-time at baseline and follow-up, and baseline activity. A Association between baseline physical behaviours and follow-up Hr-QoL. B Association between change in physical behaviours and follow-up Hr-QoL
Association of change in activity with follow/up QoL
Smaller declines in all physical activity measures were associated with better QoL at follow-up. Greater increases in all sedentary variables were associated with poorer QoL (Supplementary Table 3). Every hour/day/yr increase in MVPA was associated with 0.3 higher EQ-5D units (95% CI 0.2, 0.5). Every hour/day/yr increase in LPA was associated with 0.12 higher EQ-5D units (95% CI 0.02, 0.2). Every hour/day/year increase in total sedentary time was associated with 0.12 fewer subsequent EQ-5D units (95% CI -0.2, –0.06). Every hour/day/year increase in prolonged sedentary bout time was associated with 0.06 fewer subsequent EQ-5D units, 95% CI -0.1, -0.01).
Sensitivity analyses
The results using different cut-points for MVPA and LPA showed similar results (Supplementary Tables 2–3). There were no important differences between our main results (i.e. utilising ≥ 4 days of valid wear-time) and results using stricter inclusion criteria for accelerometry measures (i.e. ≥ 5 days of valid wear-time) (data not shown).
Discussion
We found that higher baseline MVPA and lower total sedentary time were associated with higher QoL approximately 6 years later. Further, smaller declines over time in MVPA and LPA, and smaller increases in total sedentary time and prolonged sedentary bout time were associated with better QoL. Taken together, this suggests that promotion of physical activity and limiting sedentary time in individuals may be an appropriate approach to achieving a higher absolute QoL.
No previous studies have examined the associations between baseline objectively-measured physical behaviours and follow-up QoL in adults of any age. Two studies examined this association using self-reported physical activity [36, 38]. Balboa-Castillo et al. found that greater self-reported physical activity and lower sedentary time were independently associated with better subsequent QoL in older adults (70.3 ± 5.6 years, n = 1,097) [36]. Dugan et al. found that in women (45.9 ± 2.7 years, n = 2,400) higher self-reported physical activity was associated with higher QoL 3 years later [38]. Our study goes beyond this by showing that greater baseline MVPA and lower total sedentary time, as assessed using accelerometry, were associated with higher subsequent QoL.
There are also no previous studies that have examined the association between changes in objectively-measured physical behaviours with follow-up QoL. Only one study of adults examined the association between change in self-reported physical activity and subsequent QoL. Wolin et al. found that women (aged 40–67 years) who self-reported increased physical activity had higher subsequent QoL, compared to women reporting stable physical activity levels over 8 years follow-up [37]. Our study is the first to demonstrate that greater objectively-assessed declines in MVPA and LPA, and increases in all sedentary variables, were negatively associated with subsequent QoL.
To put our results in clinical context, we found that increases in sedentary time of the magnitude achieved in intervention studies (1 h/day/year) led to a 0.002 points/year lower subsequent EQ-5D score [58, 59]. We also found that change in MVPA of the magnitude (but not direction) seen in RCTs (10 min/day/year increase) led to a 0.005 points/year lower subsequent EQ5D score [59, 60]. A 0.1 point improvement in EQ-5D score has been associated with a 6.9% reduction in mortality risk and a 4.2% reduction in risk of hospitalisation [61]. This level of improvement could mitigate the age-related decline in QoL that we observed in this cohort (-0.0069 points per year of older age). Therefore our results suggest that future interventions promoting improvements in activity profiles could lead to small clinical improvements in QoL. In addition, our work suggests that promoting LPA and reducing prolonged sedentary bout time, potentially easier targets, could also lead to improvement in QoL.
Strengths and limitations
Our work has several strengths. Firstly, we used objective measures of physical activity and sedentary time. Secondly, EPIC-Norfolk is a large population-based cohort providing greater power and ability to adjust for confounding in analyses. Thirdly, the longitudinal design of the EPIC-Norfolk study gave us the opportunity to examine prospective associations between activity and QoL, albeit reverse causality cannot be excluded. Further, we used valid measures of QoL which appear stable over time [62, 63]. In addition, we used summary scores for the measure of QoL (EQ-5D), aggregate scores of the original domains. This had the benefit of reducing multiple testing and avoiding reduction in statistical power, and examines a more global measure of QoL [64].
There are also several limitations. EPIC-Norfolk participants were slightly healthier than the general population [41] at the 1st health-check (1993–1997), and additionally those who participated at the 3rd health-check (2004–2011) were even healthier (e.g. lower blood pressure and cholesterol) than those who participated in the 1st health-check only [40] likely due to healthy volunteer bias and selective attrition. Though accelerometers provide objective measures in contrast to self-report, they do not collect information on the type of activity being done (e.g. upper body movements, standing still) which can lead to misclassification bias. Further, they cannot record water-based activity, which can lead to missing data. We minimised non-wear misclassification (i.e. not wearing the accelerometer versus being still) by using an algorithm with a threshold of ≥ 90 min [65].
Conclusions
We found that higher levels of physical activity and fewer minutes spent sedentary measures were associated with better subsequent QoL in a population of UK older adults. This work therefore supports the case for promotion of physical activity and limitation of sedentary time. QoL outcomes should be included in future intervention trials and cost effectiveness analyses. Our results add to the evidence for the wider benefits of interventions promoting physical activity and highlight the need for additional effective interventions.
Availability of data and materials
Data from the EPIC-Norfolk study must be requested directly from their data request team by completing a data request form and emailing it to epic-norfolk@mrc-epid.cam.ac.uk.
References
Ekelund U, Brown WJ, Steene-Johannessen J, Fagerland MW, Owen N, Powell KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019;53:886–94. Available from: https://pubmed.ncbi.nlm.nih.gov/29991570/. [Cited 1 Jul 2020].
Kerr J, Anderson C, Lippman SM. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. 2017;18:e457-71.
Kraus WE, Powell KE, Haskell WL, Janz KF, Campbell WW, Jakicic JM, et al. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med Sci Sports Exerc. 2019;51(6):1270–81.
De Rezende LFM, Rey-López JP, Matsudo VKR, Luiz ODC. Sedentary behavior and health outcomes among older adults: a systematic review. BMC Public Health. 2014;14:333.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–32.
Patterson R, McNamara E, Tainio M, de Sá TH, Smith AD, Sharp SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33:811–29.
Krebs S, Berling-Ernst A, Halle M. Physical Activity and Cancer. Sportverletzung Sportschaden. 2018;32(2):143–7. Available from: https://pubmed.ncbi.nlm.nih.gov/28859204. [Cited 1 Jul 2020].
Statistics on Physical activity - NHS Digital. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2019/part-5-adult-physical-activity. [Cited 1 Jul 2020].
UK Chief Medical Officers’ Physical Activity Guidelines [Internet]. 2019. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf. [cited 2022 Apr 7].
Baxter S, Blank L, Johnson M, Everson-Hock E, Woods HB, Goyder E, et al. Interventions to promote or maintain physical activity during and after the transition to retirement: an evidence synthesis. Public Health Research [Internet]. 2016;4(4):1–354. Available from: https://www.journalslibrary.nihr.ac.uk/phr/phr04040/. [cited 2016 Nov 22].
Hobbs N, Godfrey A, Lara J, Errington L, Meyer TD, Rochester L, et al. Are behavioral interventions effective in increasing physical activity at 12 to 36 months in adults aged 55 to 70 years? a systematic review and meta-analysis. BMC Med. 2013;11(1):75.
Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev. 2016;10(1):89–112. Available from: http://www.tandfonline.com/doi/full/10.1080/17437199.2015.1082146. [Cited 17 Jul 2016].
Martin A, Fitzsimons C, Jepson R, Saunders DH, van der Ploeg HP, Teixeira PJ, et al. Interventions with potential to reduce sedentary time in adults: Systematic review and meta-analysis. British J Sports Med. 2015;49:1056–63. Available from: http://bjsm.bmj.com/lookup/doi/10.1136/bjsports-2014-094524. [Cited 2 Jul 2018].
Choi M, Lee MJJ, Lee MJJ, Jung D. Physical activity, quality of life and successful ageing among community-dwelling older adults. Int Nurs Rev. 2017;64(3):396–404. Available from: http://doi.wiley.com/10.1111/inr.12397. [Cited 24 Sep 2020].
Takahashi PY, Ryu E, Olson JE, Winkler EM, Hathcock MA, Gupta R, et al. Health behaviors and quality of life predictors for risk of hospitalization in an electronic health record-linked biobank. Int J Gen Med. 2015;8:247–54. Available from: https://www.tandfonline.com/doi/full/10.2147/IJGM.S85473. [Cited 2 Jan 2021].
Belayachi J, el Khattate A, Bizrane M, Madani N, Abouqal R. Pre-admission quality of life as predictor of outcome after acute care: the role of emotional well-being. QJM. 2018;111(2):111–5. Available from: https://academic.oup.com/qjmed/article/111/2/111/4568570. [Cited 2 Jan 2021].
Phyo AZZ, Freak-Poli R, Craig H, Gasevic D, Stocks NP, Gonzalez-Chica DA, et al. Quality of life and mortality in the general population: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):1596.
van Rijckevorsel-Scheele J, Willems RCWJ, Roelofs PDDM, Koppelaar E, Gobbens RJJ, Goumans MJBM. Effects of health care interventions on quality of life among frail elderly: a systematized review. Clin Interv Aging. 2019;14:643–58. Dove Medical Press Ltd.
Abu-Omar K, Rütten A, Burlacu I, Schätzlein V, Messing S, Suhrcke M. The cost-effectiveness of physical activity interventions: a systematic review of reviews. Prev Med Rep. 2017;1(8):72–8.
Dugan SA, Gabriel KP, Lange-Maia BS, Karvonen-Gutierrez C. Physical activity and physical function: moving and aging. Obstet Gynecol Clin North Am [Internet]. 2018;45(4):723–36. Available from: https://pubmed.ncbi.nlm.nih.gov/30401553/. [cited 2023 May 14]
Yerrakalva D, Hajna S, Wijndaele K, Dempsey PC, Westgate K, Wareham N, et al. Bidirectional associations of accelerometer-assessed physical activity and sedentary time with physical function among older English adults: the EPIC-Norfolk cohort study. Eur J Ageing [Internet]. 2022;19(4):1507–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/36692782. [cited 2023 May 14].
Yoshimura J, Tanimura C, Matsumoto H, Tokushima Y, Inoue K, Park D, et al. Relationship of physical activity to self-care agency and physical condition among older adults in a rural area. Yonago Acta Med [Internet]. 2021;64(1):18. Available from: /pmc/articles/PMC7902176/. [cited 2023 May 14].
Gomes ESA, Ramsey KA, Rojer AGM, Reijnierse EM, Maier AB. The association of objectively measured physical activity and sedentary behavior with (instrumental) activities of daily living in community-dwelling older adults: a systematic review. Clin Interv Aging [Internet]. 2021;16:1877. Available from: /pmc/articles/PMC8560073/. [cited 2023 May 14].
Niederstrasser NG, Attridge N. Associations between pain and physical activity among older adults. PLoS One [Internet]. 2022;17(1). Available from: https://pubmed.ncbi.nlm.nih.gov/35089966/. [cited 2023 May 14].
Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiatry [Internet]. 2022;79(6):550–9. Available from: https://pubmed.ncbi.nlm.nih.gov/35416941/. [cited 2023 May 14].
Falck RS, Davis JC, Liu-Ambrose T. What is the association between sedentary behaviour and cognitive function? A systematic review. Br J Sports Med [Internet]. 2017;51(10):800–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27153869. [cited 2019 May 24].
Guure CB, Ibrahim NA, Adam MB, Said SM. Impact of physical activity on cognitive decline, dementia, and its subtypes: meta-analysis of prospective studies. Biomed Res Int [Internet]. 2017;2017:9016924. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28271072. [cited 2018 Sep 29].
Schrempft S, Jackowska M, Hamer M, Steptoe A. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health [Internet]. 2019;19(1). Available from: https://pubmed.ncbi.nlm.nih.gov/30651092/. [cited 2022 Apr 7].
Omorou AY, Vuillemin A, Menai M, Latarche C, Kesse-Guyot E, Galan P, et al. 10-year cumulative and bidirecti associations of domain-specific physical activity and sedentary behaviour with health-related quality of life in French adults: Results from the SU.VI.MAX studies. Prev Med (Baltim). 2016;88:66–72. Available from: https://pubmed.ncbi.nlm.nih.gov/27058941/. [Cited 8 Mar 2019].
Feeny D, Garner R, Bernier J, Thompson A, McFarland BH, Huguet N, et al. Physical activity matters: Associations among body mass index, physical activity, and health-related quality of life trajectories over 10 years. J Phys Act Health. 2014;11(7):1265–75. Available from: https://pubmed.ncbi.nlm.nih.gov/24176861/. [Cited 24 Sep 2020].
Kanesarajah J, Waller M, Whitty JA, Mishra GD. Physical activity and body mass shape quality of life trajectories in mid-age women. Aust N Z J Public Health. 2018;42(4):403–9. Available from: https://pubmed.ncbi.nlm.nih.gov/29972259/. [Cited 24 Sep 2020].
Thiel DM, Sayah FA, Vallance J, Johnson ST, Johnson JA. Physical activity and health-related quality of life in adults with type 2 diabetes: results from a prospective cohort study. J Phys Act Health. 2017;14(5):368–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28169577. [Cited 8 Mar 2019].
Suzuki Y, Maeda N, Hirado D, Shirakawa T, Urabe Y. Physical activity changes and its risk factors among community-dwelling japanese older adults during the COVID-19 epidemic: Associations with subjective well-being and health-related quality of life. Int J Environ Res Public Health. 2020;17(18):1–12. Available from: https://www.mdpi.com/1660-4601/17/18/6591?utm_source=researcher_app&utm_medium=referral&utm_campaign=RESR_MRKT_Researcher_inbound. [Cited 24 Sep 2020].
Jantunen H, Wasenius N, Salonen MK, Kautiainen H, von Bonsdorff MB, Kajantie E, et al. Change in physical activity and health-related quality of life in old age—A 10-year follow-up study. Scand J Med Sci Sports. 2019;29(11):1797–804. Available from: https://pubmed.ncbi.nlm.nih.gov/31206811/. [Cited 24 Sep 2020].
Choi M, Prieto-Merino D, Dale C, Nüesch E, Amuzu A, Bowling A, et al. Effect of changes in moderate or vigorous physical activity on changes in health-related quality of life of elderly British women over seven years. Qual Life Res. 2013;22(8):2011–20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23242939. [Cited 8 Mar 2019].
Balboa-Castillo T, León-Muñoz LM, Graciani A, Rodríguez-Artalejo F, Guallar-Castillón P. Longitudinal association of physical activity and sedentary behavior during leisure time with health-related quality of life in community-dwelling older adults. Health Qual Life Outcomes. 2011;9(1):47.
Wolin KY, Glynn RJ, Colditz GA, Lee IM, Kawachi I. Long-term physical activity patterns and health-related quality of life in U.S. Women Am J Prev Med. 2007;32(6):490–9.
Dugan SA, Everson-Rose SA, Karavolos K, Sternfeld B, Wesley D, Powell LH. The impact of physical activity level on SF-36 role-physical and bodily pain indices in midlife women. J Phys Act Health. 2009;6(1):33–42.
Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35(5):976–83. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3329818&tool=pmcentrez&rendertype=abstract. [Cited 25 Feb 2015].
Hayat SA, Luben R, Keevil VL, Moore S, Dalzell N, Bhaniani A, et al. Cohort profile: a prospective cohort study of objective physical and cognitive capability and visual health in an ageing population of men and women in Norfolk (EPIC-Norfolk 3). Int J Epidemiol. 2014;43(4):1063–72.
Day N, Oakes S, Luben R, Khaw KT, Bingham S, Welch A, et al. EPIC-Norfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br J Cancer. 1999;80 Suppl 1:95–103. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10466767. [Cited 13 Jul 2016].
Ried-Larsen M, Brønd JC, Brage S, Hansen BH, Grydeland M, Andersen LB, et al. Mechanical and free living comparisons of four generations of the Actigraph activity monitor. Int J Behav Nutr Phys Act. 2012;9(1):113. Available from: http://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-9-113. [Cited 25 Mar 2019].
Robusto KM, Trost SG. Comparison of three generations of ActiGraphTM activity monitors in children and adolescents. J Sports Sci. 2012;30(13):1429–35. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22857599. [Cited 25 Mar 2019].
Ojiambo R, Cuthill R, Budd H, Konstabel K, Casajús JA, González-Agüero A, et al. Impact of methodological decisions on accelerometer outcome variables in young children. Int J Obes (Lond). 2011;35(Suppl 1):S98-103.
Edwardson CL, Gorely T. Epoch length and its effect on physical activity intensity. Med Sci Sports Exerc. 2010;42(5):928–34. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005768-201005000-00012. [Cited 7 Nov 2016].
Berkemeyer K, Wijndaele K, White T, Cooper AJM, Luben R, Westgate K, et al. The descriptive epidemiology of accelerometer-measured physical activity in older adults. Int J Behav Nutr Phys Act. 2016;13(1):2. Available from: http://www.ijbnpa.org/content/13/1/2. [Cited 5 Feb 2017].
Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, Mcdowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8.
Hall KS, Howe CA, Rana SR, Martin CL, Morey MC. METs and accelerometry of walking in older adults: standard versus measured energy cost. Med Sci Sports Exerc. 2013;45(3):574–82. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3990855&tool=pmcentrez&rendertype=abstract. [Cited 18 Aug 2014].
Gorman E, Hanson HM, Yang PH, Khan KM, Liu-Ambrose T, Ashe MC, et al. Accelerometry analysis of physical activity and sedentary behavior in older adults: a systematic review and data analysis. Eur Rev Aging Phys Act. 2014;11:35–49.
Hajna S, White T, Brage S, van Sluijs EMF, Westgate K, Jones AP, et al. Descriptive epidemiology of changes in objectively measured sedentary behaviour and physical activity: six-year follow-up of the EPIC-Norfolk cohort. Int J Behav Nutr Phys Act. 2018;15(1):122. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30482229. [Cited 9 Mar 2019].
EuroQoL. EQ-5D-3L. Available from: https://euroqol.org/eq-5d-instruments/eq-5d-3l-about/. [Cited 18 Apr 2019].
Van Reenen M, Oppe M, Boye KS, Herdman M, Kennedy-Martin M, Kennedy-Martin T, et al. EQ-5D-3L User Guide. 2018.
Ramos-Goñi JM, Rivero-Arias O. eq5d: A command to calculate index values for the EQ-5D quality-of-life instrument [Internet]. The Stata Journal. 2011;11. Available from: https://journals.sagepub.com/doi/pdf/10.1177/1536867X1101100108. [cited 2020 Oct 12].
Grassi L, Caruso R, Da Ronch C, Härter M, Schulz H, Volkert J, et al. Quality of life, level of functioning, and its relationship with mental and physical disorders in the elderly: Results from the MentDis_ICF65+ study. Health Qual Life Outcomes. 2020;18(1):1–12. Available from: https://hqlo.biomedcentral.com/articles/10.1186/s12955-020-01310-6. [Cited 20 Apr 2023].
Lee KH, Xu H, Wu B. Gender differences in quality of life among community-dwelling older adults in low- and middle-income countries: results from the Study on global AGEing and adult health (SAGE). BMC Public Health. 2020;20(1):1–10. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-8212-0. [Cited 20 Apr 2023] .
Cepeda M, Koolhaas CM, van Rooij FJA, Tiemeier H, Guxens M, Franco OH, et al. Seasonality of physical activity, sedentary behavior, and sleep in a middle-aged and elderly population: the Rotterdam study. Maturitas. 2018;110:41–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29563034. [Cited 5 Dec 2019].
Stolwijk AM, Straatman H, Zielhuis GA. Studying seasonality by using sine and cosine functions in regression analysis. J Epidemiol Community Health. 1999;53(4):235–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10396550. [Cited 5 Dec 2019].
Aunger JA, Doody P, Greig CA. Interventions targeting sedentary behavior in non-working older adults: a systematic review. Maturitas. 2018;116:89–99 Elsevier Ireland Ltd; Available from: 10.1016/j.maturitas.2018.08.002. [Cited 21 Jul 2020].
Stockwell S, Schofield P, Fisher A, Firth J, Jackson SE, Stubbs B, et al. Digital behavior change interventions to promote physical activity and/or reduce sedentary behavior in older adults: A systematic review and meta-analysis. Exp Gerontol [Internet]. 2019;120:68–87. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0531556519300877. [cited 2019 Jun 12].
Chase JAD. Interventions to increase physical activity among older adults: A meta-analysis. Gerontologist. 2015;55:706–18. Available from: https://pubmed.ncbi.nlm.nih.gov/25298530/. [Cited 21 Jul 2020].
Cavrini G, Broccoli S, Puccini A, Zoli M. EQ-5D as a predictor of mortality and hospitalization in elderly people. Qual Life Res. 2012;21(2):269–80.
Brett CE, Dykiert D, Starr JM, Deary IJ. Predicting change in quality of life from age 79 to 90 in the Lothian Birth Cohort 1921. Qual Life Res. 2019;28(3):737–49. https://doi.org/10.1007/s11136-018-2056-4. [Cited 27 May 2021].
Hopman WM, Berger C, Joseph L, Towheed T, vandenKerkhof E, Anastassiades T, et al. Stability of Normative Data for the SF-36. Canadian Journal of Public Health [Internet]. 2004;95(5):387–91. Available from: http://link.springer.com/10.1007/BF03405153. [cited 2021 May 27].
Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Mailey EL, Gothe NP, Wójcicki TR, Szabo AN, Olson EA, Mullen SP, et al. Influence of allowable interruption period on estimates of accelerometer wear time and sedentary time in older adults. J Aging Phys Act. 2014;22(2):255–60.
Acknowledgements
The authors would like to thank the MRC Epidemiology Physical Activity Technical Team for their role in data processing, EPIC-Norfolk Study team for their role in data collection, and all the EPIC-Norfolk Study participants.
Funding
The EPIC-Norfolk study (https://doi.org/10.22025/2019.10.105.00004) has received funding from the Medical Research Council (MR/N003284/1 and MC-UU_12015/1) and Cancer Research UK (C864/A14136). DY was funded by a National Institute for Health Research Doctoral Fellowship (DRF-2017–10-121). SH was supported by the Lifelong Health and Wellbeing Cross-Council Programme, the Medical Research Council (MC_UU_12015/4), and Canadian Institutes of Health Research (FRN 146766). KWi and SB were supported by the Medical Research Council (MC_UU_00006/4 and MC_UU_12015/3) and NJW by MC_UU_12015/1. KWe was supported by the NIHR Cambridge Biomedical Research Centre (IS-BRC-1215–20014). SJG and NJW are NIHR Senior Investigators. The University of Cambridge has received salary support in respect of SJG from the NHS in the East of England through the Clinical Academic Reserve.
Author information
Authors and Affiliations
Contributions
DY contributed to the conception and design of the paper, analysis and interpretation of data, drafting and revision of the paper. SH, SG, SB, KWi, KWe and MS contributed to the conception and design of the paper and data, data acquisition, interpretation of the data and revision of the paper. NJW and KTK contributed to the conception and design of the data, data acquisition and revision of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical procedures in this study were approved by the Norfolk Local Research Ethics and East Norfolk and Waveney NHS Research Governance Committee. EPIC was closely monitored both internally by the University of Cambridge and externally by various governing committees such as the Local Research Ethics Committee and Confidentiality Advisory Group (CAG) of the Health Research Authority. EPIC obtained informed consent from all subjects and/or their legal guardian(if illiterate participants involved). The EPIC-Norfolk Approval Board approved access to data from the study, with all released data already anonymised.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Characteristics of included participants versus those excluded from the EPIC-Norfolk study 2006-2016. Supplementary Table 2. Association of baseline physical activity and sedentary time with follow-up QOL in the EPIC-Norfolk study 2006-2016. Supplementary Table 3. Association of change in physical activity and sedentary time with follow-up QOL in the EPIC-Norfolk study 2006-2016
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yerrakalva, D., Hajna, S., Suhrcke, M. et al. Associations between change in physical activity and sedentary time and health-related quality of life in older english adults: the EPIC-Norfolk cohort study. Health Qual Life Outcomes 21, 60 (2023). https://doi.org/10.1186/s12955-023-02137-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-023-02137-7