Abstract
Background
In recent years, more importance is being given to the assessment of quality of life (QoL) among diabetic patients as a measure of their health and the goal of all health interventions. Other studies have reported a high prevalence of diabetes-related effects on; however, there is a knowledge gap in the region of Sub-Saharan Africa, as is the case for Rwanda, where the prevalence of diabetes is expected to rise over the next decade. The aim of this study is to report on the translation and cultural adaptation of the Diabetes-39 (D-39) questionnaire into the Kinyarwanda and its psychometric properties among diabetic patients in Rwanda.
Methods
The D-39 questionnaire—a five-scale, disease-specific QoL questionnaire—was translated from English to Kinyarwanda, then back-translated to English. A consensus meeting discussed discrepancies and agreed on changes. Interviews were conducted with 26 participants before producing a final version. For the psychometric evaluation, the adapted version was administered to 309 patients with diabetes mellitus. Participants either came from a separate cluster-randomised controlled trial or were recruited ad hoc for this study. The evaluation included testing internal consistency, known group validity, and construct validity.
Results
Participants’ mean age was 51 ± 12.7 years with a predominance of women (64%) in the sample. All five scales of the questionnaire showed a good internal consistency, with composite reliability of above 0.7. The five-factor model of the questionnaire was fitted to the 39 items. Although the fit was not exact, there was a satisfactory approximate fit (CFI = 0.93, TLI = 0.92, RMSEA = 0.05). There was a good discriminant validity except for the “social burden” and “anxiety and worry” scales (inter-factor correlation = 0.80).
Conclusions
Diabetes-39 is a questionnaire developed in English that was adapted and translated into Kinyarwanda. The Kinyarwanda version of D-39 is a reliable and valid instrument to measure QoL among diabetic patients in Rwanda. The questionnaire can be helpful in research and clinical practice improving health outcomes for patients with diabetes in Rwanda and other Kinyarwanda-competent areas in the sub-region. However, certain cross-cultural differences should be considered.
Similar content being viewed by others
Introduction
It is estimated by the World Health Organisation (WHO) that, in 2016, diabetes mellitus (DM) was a top seven cause of death [1]. DM is a life-changing disease with a high incidence of micro- and macrovascular complications [2]. These include neuropathy, nephropathy, retinopathy, peripheral vascular disease, coronary heart disease, and stroke. These complications are associated with high morbidity and mortality, which markedly reduce the quality of life (QoL) of the patient [3]. QoL is defined by the WHO as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” [4]. Assessing QoL helps in uncovering the needs of patients, in setting up preventative programmes, and in planning service delivery. Unfortunately, there is still limited evidence on ‘QoL’ of diabetes patients in Sub-Saharan Africa region as compared to the large number of studies done in higher-income countries. In Rwanda, the prevalence of DM has been estimated at 5.1% [5]. A sharp increase in the prevalence on-communicable chronic diseases is anticipated over the next decade owing to urbanization and increasingly sedentary lifestyles. Much evidence has already been generated elsewhere on the impact of diabetes on QoL as well as its associations with socio-demographic characteristics such as gender, age, education, and income; clinical factors such as severity and management of the disease; lifestyle and diet; as well as acute and chronic complications [6,7,8,9,10].
The increasing understanding of the importance of measuring QoL in diabetics is driving research into specific interventions and into QoL management in clinical settings [11]. The Diabetes-39 (D-39) questionnaire is a widely-used self-reporting tool, which has been significantly associated with glycaemic control, adherence to treatment and complications, and has been linked to other associated constructs of QoL [12, 13].
There are a number of existing tools—both generic and disease-specific—for measuring QoL in diabetes [14]. Generic instruments are used in the general population to measure a wide range of domains applicable to a variety of health states, conditions, and diseases. The symptoms disease-specific instruments can include the most important aspects of health, as considered by patients or clinicians [15]. Because disease-specific instruments are more focused, they can be more responsive to changes in health and provide a more detailed and accurate assessment of patients concerns. Among generic instruments for diabetes, the Medical Outcomes Study ‘Short Form (36) Health Survey’ (or SF-36) is commonly-used, but the D-39 is the preferred instrument, as it has good psychometric properties [16]. The D-39 has been translated into multiple languages, has high internal reliability and good responsiveness to change, and has been used in a wide range of interventions [11, 14,15,16,17,18].
To the best of our knowledge, in all of Africa, the D-39 questionnaire has only been translated and adapted into Arabic [19, 20]. There is no validated version of the D-39 questionnaire for the Sub-Saharan African context, which includes Rwanda. The aim of this paper, therefore, was to report on the translation and cultural adaption of the D-39 questionnaire into a local language- Kinyarwanda, and to evaluate its psychometric properties.
Material and methods
The diabetes-39 questionnaire
The instrument used was the D-39 questionnaire, a multidimensional scale developed in United States of America [21], which consists of 39 items grouped in five dimensions: Energy and mobility (15 items), diabetes control (12), social burden (5), anxiety and worry (4), and sexual functioning (3). The D-39 is used to assess the QoL of patients with type 1 and type 2 diabetes; regardless of their treatment regimen [16]. Patient themselves could rate their QoL during the last month for each item. Each item can be answered using a seven-point scale ranging from 0.5 (not affected at all) to 7.5 (extremely affected). Each of the five dimensions were summed up, and the resulting raw scores were transformed into scales ranging from 0 to 100 using a linear transformation: (raw score − minimum value)/(maximum value − minimum value) × 100 according to the developer’s instructions. The questionnaire also includes two supplementary “overall ratings”, in which respondents use the same seven-box Likert scale to evaluate their perceived overall QoL (ranging from “lowest quality” to “highest quality”) and the severity of their diabetes (ranging from “not severe at all” to “extremely severe”). The self-rating overall health status was also evaluated with a single item asking participants to rate their overall health using a five-point Likert scale [22]. Participants responded to this item from ‘’one = very poor’’; ‘’two = poor’’; ‘’three = moderate’’; ‘’four = good’’ and ‘’ five = very good).
Translation and cross-cultural adaptation procedures
Translation of D-39 to Kinyarwanda, back-translation and consensus version in English
Permission to use the D-39 was obtained from the D-39 developers. Then, for the translation of the questionnaire, we used a standard approach [23] coupled with known steps in the process of adaption [24, 25]. The translation was carried out by two native Rwandans. One of the translators possess a university degree in English literature and has twelve years of work experience, while the other is a medical doctor with work experience of seven years, who also has taught English for more than eight years. Both have a certificate of proficiency in English, and they translated the questionnaire into Kinyarwanda independently, following an ‘item intent’ guide. The two translations were synthesised into one, addressing any discrepancies. The Kinyarwanda back-translation of Kinyarwanda questions into English were done by two English native speakers. One of the back-translators has a university degree in International Studies, while the other one has studied linguistics, African studies and computational linguistics. Both back-translators had excellent language skills in Kinyarwanda. They back-translated the Kinyarwanda questions into English, while blinded to the original version. Subsequently, the two backward translations were reconciled into one.
Assessment by expert committee
An expert committee was set up comprised of seven members, including two Rwandan forward translators, one of the back-translators, an epidemiologist, a local bilingual representative, and the two researchers conducting the study. All members of the committee were fluent in English. The aim was to appraise the results of the translations, evaluating their semantic, idiomatic, experiential and conceptual equivalence, and produce a pre-final version. A report was prepared providing an account of these steps, the controversial items, and the ways they were resolved in the consensus translation. The report and the pre-final version were shared with the questionnaire developer, and consent was received.
Pre-testing
The pre-final version was assessed by conducting interviews using a sample of patients (n = 26) with DM. The objective was to evaluate patient comprehension of the translated questions and the answer categories whether respondents could retrieve relevant information from memory, the effort required to answer the degree of interest and social desirability bias. To attain maximum variability of the participants, the interviews were conducted in four different hospitals. After each round, modifications were proposed for some items, based on the interview transcripts and notes. A new iteration of the questionnaire was then prepared and tested in the following round. Lastly, a final version was produced, and a report was made available to the original D-39 developers.
Psychometric properties and statistical analysis
Study participants, data collection and sample size
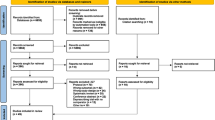
Evaluating Psychometric Properties of D-39 was part of a cluster-randomised controlled trial (RCT), that aimed at determining the efficacy of an integrated mobile-health and community-health-worker programme for the management of diabetes in primary healthcare in Rwanda. The protocol of this RCT (ClinicalTrials.gov registration: NCT03376607) consists of a mixed-methods study, and has been published elsewhere [26].
For the purpose of conducting the confirmatory factor analysis (CFA), at least 200 participants would be necessary [24, 26,27,28]. The power analysis of the RCT indicated a sample size of 324 participants, which was also adequate for conducting the CFA. Nonetheless, the pre-enrolment screening revealed that a sufficient number of patients living with diabetes could not be recruited in the specific recruitment areas selected for the RCT [26]. Furthermore, logistical challenges impeded the prompt activation of the last two of the nine hospitals (Kabutare and Ruhango).
For these reasons an additional sample was also recruited for the purposes of the evaluation, following the inclusion criteria of the RCT: patients aged 21–80 years and diagnosed with DM at least six months prior to study onset. This supplementary cohort consisted of patients residing in additional zones in the catchment areas of same hospitals, except for the hospitals of Kibungo, Kibuye and Kinihira, where the number of patients was particularly low. The recruitment was carried out between June and December 2019. Exclusion criteria for both samples were illiteracy, severe hearing or visual impairments, severe mental health conditions and pregnancy, or in the post-partum period. The classification of DM type was based on the patients’ clinical records available at the hospitals. As the precise date of the diagnosis of DM was unknown for some participants, only those with at least one year of diagnosis were included so as to limit the effect of the emotional distress linked to recent diagnosis [18, 21]. Reliability analysis and known groups validity To assess internal reliability Cronbach’s α and composite reliability were calculated. Mean differences in total score and in the scales of the model with the closest fit were investigated across socio-demographic and clinical groups with Mann–Whitney U test. Effect sizes were calculated based on z values; r of 0.10, 0.30 and 0.50 were interpreted as small, medium and large effects respectively [29]. For continuous variables, Spearman’s correlation was used to determine which of them were associated with the total score and scales. Correlation coefficients below 0.4 were considered as weak, those between 0.4 and 0.7 as moderate, and those above 0.7 as strong [30, 31].
Construct and discriminant validity analysis To assess construct validity, a CFA was conducted. The five-factor model was fitted to the 39 items of the questionnaire with no cross-loadings or correlated errors terms. The estimation strategy, in line with the standard underlying assumptions of the CFA [32], is reliable, given the relatively different nature of the 5 dimensions (energy and mobility, diabetes control, social burden, anxiety and worry, and sexual functioning) used to group the 39 items under analysis.
The discriminant validity of D-39 was studied by calculating inter-factor correlations. Inter-factor correlations have been included in Table 5, supporting the assumption of a sufficient discriminant validity for all scales. The weighted least square mean and variance adjusted (WLSMV) estimator was used in the CFA. The root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the Tucker Lewis index (TLI) were used to examine the approximate model fit. For RMSEA, values of less than 0.05 were indicative of a close fit and those between 0.05 and 0.08 were interpreted as adequate fit [27, 28]. The 90% confidence intervals of RMSEA were also evaluated, as they should be less than 0.05 for the lower bound and no worse than 0.08 for the upper one [27]. For CFI and TLI, values of 0.90 and above were regarded as acceptable fit [27, 28]. Hu’s and Bentler’s recommendation of raising such cut-offs to 0.95 was also taken into account [27, 33]. The relative χ2 was also calculated and a value of 2 or less was deemed adequate [27]. Finally, although the weighted root mean-square residual (WRMR) was computed and values of 1 or lower were considered a good fit, the experimental nature of this statistic thwarted drawing conclusions based on it [27, 28, 34].
Statistical analyses were performed using Stata version 16. Mplus version 7, and JASP version 16.2.
Ethical and research clearance
The study protocol was developed, and research authorisation was sought from the Rwandan Health and Education Ministries. Ethical approval was obtained from the Rwanda National Ethics Committee and the Ethics Review Panel of the University of Luxembourg.
Results
Cultural adaptation
The expert panel evaluated all translations and reached a consensus (Additional file 1), particularly regarding the items without precise translation into Kinyarwanda. This include the following dimensions: Energy and Mobility (item question 10, 33, 35 and 36), Diabetes Control (item question 15 and 28) and Social Burden (item question 19 and 26). Three rounds of interviews were conducted thereafter, with a total of 26 diabetic participants: 22 women and 4 men, with the median age of 47 (IQR = 39–62), median years of completed education of 6 (IQR = 6–8) and the median years of diabetes 3.5 (IQR = 2–6). Comprehension of the translated items was good, and amendments were made to increase clarity and resolve any ambiguities. Table 1 summarises the consensus translation, and reasons for modification of the item questions of the D-39.
In the first round we used a layout similar to the original English instrument, in which the introductory phrase “During the past month how much was the quality of your life affected by:” was repeated once at the top of each page, and the questions beneath stated only the second part of the sentence (e.g. “your daily medication for your diabetes”). During that round, it was noticed that most of the interviewees could not understand the questions that referred to “how the quality of their life was affected during the past month”. To resolve this issue, a new layout was tested, in which every question was preceded with the introductory phrase, and the question was written in bold (e.g. “During the past month how much was the quality of your life affected by your daily medication for your diabetes”).
According to the developer’s scoring instructions, each item is scored with a 0.5 step depending on where the cross is placed by the participants (e.g., if a mark is placed on the right-side margin of the last box, that should be interpreted as 7.5). Hence, the effective possible scoring range for each item is between 0.5 and 7.5. However, during pretesting, we observed participants having difficulty marking with precision different parts of the box space. Consequently, we adopted a simplification of scoring by considering only the area of the seven boxes (i.e., each item could be scored from 1 to 7, with a step of 1), similarly to the method recommended in the Brazilian adaptation of D-39.
Characteristics of the subjects
Table 2 shows the patients’ characteristics. Two hundred and five participants were included from the RCT, and 122 were recruited additionally for the purposes of the evaluation. A total of 18 patients were excluded as there were marked. The total sample (N = 309). were included in the analysis of the D-39. The mean total score of D-39 for the sample was 51 (SD = 12.7), the median was 52 (IQR = 42–60) and 64% were female. More than half of the participants were married and completed secondary level education. The mean and median years of completed education were 7.6 (SD = 12.7), and 6 (IQR = 5–9) respectively. Eighty-nine percent (88.7%) of the participants reported having type 2 diabetes according to their clinical record. Six (SD = 5.8) and five (IQR = 2–9) were the mean and median years since diagnosis of diabetes in the study population respectively. All the subjects were of Rwandan nationality and spoke Kinyarwanda.
Internal consistency
Table 3 shows that composite reliability for all scales was acceptable (> 0.7). Similarly, Cronbach’s α ranged from 0.72 for “anxiety and worry” to 0.90 for “sexual functioning”, and McDonald’s ω ranged from 0.73 for “anxiety and worry” to 0.90 for “sexual functioning”.
The standardised factor loadings ranged from 0.39 to 0.67 for the “diabetes control” scale; from 0.54 to 0.75 for the “anxiety and worry” scale; from 0.53 to 0.72 for the “social burden” scale; from 0.90 to 0.91 for the “sexual functioning” scale, and from 0.38 to 0.71 for “energy and mobility” (Table 4).
Construct validity (confirmatory factor analysis)
Construct validity was assessed with CFA based on weighted least square mean and variance adjusted estimator. The five-factor model was fitted to the 39 items of the questionnaire and did not yield an exact fit (χ2 = 1228.6, df = 692, p < 0.0001, relative χ2 = 1.8); however, the fit indices indicated a satisfactory approximate fit (CFI = 0.93, TLI = 0.92, RMSEA = 0.05 (90% CI 0.046–0.055)).
There was sufficient discriminant validity for all scales with the exception of “social burden” and “anxiety and worry” with a reported inter-factor correlation of 0.8 (Table 5).
Table 6 demonstrates the relationships between socio-demographic variables, the five dimensions of the D-39, and the two additional “overall ratings” items. Overall, there were significant gender differences in the “diabetes control”, “anxiety and worry” and “energy and mobility” scales (small effect sizes), and “sexual functioning” scale (medium effect size). Small correlations were observed between years of completed education and the “anxiety and worry”, “social burden” and “energy and mobility” scales. The self-rated overall health was also weakly correlated with all D-39 scales but for the “sexual functioning”. Finally, “energy and mobility” differed significantly, albeit with a small effect size, between the two types of diabetes.
Concerning the two “overall rating” items, the mean perceived quality of life was 3.9 (SD = 1.3) and the mean perceived severity of the disease was 3.9 (SD = 1.4). Question X2 (mean = 3.9, SD = 1.4, median = 4, IQR = 3–5).
Discussion
Our research indicates that the tool we adapted to assess diabetic QoL was the first of its kind, being the only such tool to be tailored specifically with the Rwandan and sub-Sahara Africa cultural contexts in mind. We analysed, made cultural adaptations to, and translated the D-39 Questionnaire into Kinyarwanda. With approximately 20 million speakers, Kinyarwanda is one of the most widely-spoken bantu languages, known to have both grammatical and lexical reduplications and is a national language in Rwanda [35].
There are a number of dialects and word substitutions throughout Rwanda, and so we aimed to account for these so that the Kinyarwanda version could be understood by the majority. Sometimes, different words may be used to express a single concept, and there is precedent for this approach [35]. We aimed to assemble a varied consensus panel, in order to enable a comprehensive assessment of the translated version. The feedback from patients regarding comprehension was particularly useful in achieving consensus on highlighted discrepancies; agreement was reached not only on the wording and formulation of items, but also on the changes which needed to be made. These adaptations were intended to improve respondent understanding, and to increase consistency in responses.
The full scale showed a good internal reliability in line with previous studies [14, 15, 36, 37]. Overall, some items did not load highly in some scales (e.g., diabetes control), while others performed better (e.g., sexual functioning). Discriminant validity was assessed through inter-factor correlations. In this study, there was good discriminant validity for all scales with the exception of the “anxiety and worry” and “social burden” scale (0.80). A similar lower correlation coefficient were observed in the Brazilian study [38] for the domain “anxiety and worry” (0.21) and for the domain “social burden” (0.34) in a study from Jordan [19].
All of the D-39 domains are higher than the composite reliability standard of 0.7 that previously justified as a value to support claims of internal reliability of the instrument [37, 39]. Previous studies have shown that a Cronbach’s alpha coefficient of below 0.70 can undermine the instrument’s internal consistency [40]. For each of the five scales in the 39-item instrument, the Cronbach's coefficient alpha was calculated. The results of the D-39 item and scales tests assumption in this study showed that the internal consistency reliability Cronbach’s alpha in the diabetic population in Rwanda ranged between 0.72 and 0.92. This is similar (or higher) to those obtained in a study population of Jordan [19] (0.80 to 0.92), of the United states [21] (0.82 to 0.93 and 0.81 to 0.93 for Iowa and Carolina studies respectively) and of the Nordic countries [41] (0.83 to 0.92, 0.83 to 0.91 and 0.82 to 0.92 for Finnish, Norwegian and Danish studies respectively). The Cronbach’s alpha of this study differed from a Moroccan study [20] (0.65–0.93), and a Brazilian study [38] (0.58 to 0.85). It is worth mentioning that our sample size of 309 was approximate to the one used in the Jordan study [19] (N = 368) and higher than the studies in Brazil N = 52 and Morocco N = 92 [20, 38].
Despite the fact that a lot of effort was engaged in reaching out the communities to recruit a large sample, there have been significant logistical and systemic barriers, and this was marked as the study limitation. The presentation of diabetes specific QoL may differ between patients depending on the form of the disease, and this should be noted as a possible limitation of this study. For example, Insulin dependent diabetes mellitus patients may present with a higher fear of hypoglycaemia [42]. Although we observed no significant differences between the two forms of the disease, our sample consisted predominantly of patients with type 2 DM. Notwithstanding this, such distinctions between forms of the disease need to be treated cautiously due to the possibility of misclassification and/or atypical disease forms [42,43,44,45]. The treatment type may also cause a separate effect, particularly pertaining to the use of insulin [46]; however, information on insulin use was not collected for this study.
As it was not possible to identify another established and previously validated tool in the Rwandan population—either generic or diabetes-specific—there was a lack of testing for convergent validity, and this may also be considered a limitation of our study. Test–retest reliability was not carried out, and further research is therefore indicated. We were also unable to evaluate the correlation of D-39 with glycated haemoglobin, as in Rwanda this was not routinely measured during the time we conducted this study, and ad hoc measurements for the entire study sample were not possible. Finally, as reliable diagnoses were not easily obtained from patients’ medical records, it was difficult to effectively investigate comorbidity.
The results show the perceptions of patients and their health care providers on gaps in the readiness of the society, patients, and the health care system to ensure improved health related QoL of diabetes patients. A programme to ensure QoL would tackle many challenges that are currently being faced by diabetic patients in Rwanda while at the same time addressing the increasing prevalence of the disease in the country. Such a study would help generate new insight around factors influencing the health related QoL within the Rwandan social, cultural and demographic context [47, 48], thus informing researchers and clinical practice for better health outcomes.
Conclusion
Diabetes-39 is a questionnaire originally developed in English which was adapted and translated into Kinyarwanda for the purposes of this study. Our results confirm that this Kinyarwanda version is a both reliable and valid instrument to measure the health related QoL of diabetic patients, and could help both researchers and clinicians in their practice to improve health outcomes for patient with diabetes in Rwanda and its sub-region. It can provide insights into the factors that impact QoL, in the context of Rwandan values and culture, and also for the purposes of assessment in disease management. Further scale assessment, using larger samples with a more diverse population across sub-Saharan Africa, would strengthen the evidence for the viability of this questionnaire as a health related QoL tool for diabetic patients.
Availability of data and materials
The data used to support the findings of this study are restricted by the Government of Rwanda, and cannot be released or shared partially or totally with third parties without the written permission of the Rwanda Biomedical Centre. Data are available from the corresponding author for researchers who meet the criteria for access to confidential data, and only after authorisation from the Rwanda Biomedical Centre.
References
World Health Organization (WHO). Diabetes-Key facts [Internet]. WHO. 2020 [cited 2020 Jun 12]. https://www.who.int/news-room/fact-sheets/detail/diabetes.
Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: distinct or continuum? Indian J Endocrinol Metab. 2016;20:546–51.
Spasi A, Veli R, Cati A, Stefanovi N, Cvetkovi T. Quality of life in type 2 diabetic patients. Sci J Fac Med Niš. 2014;31:193–200.
The WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998;46:1569–85.
The International Diabetes Federation (IDF). Diabetes atlas regional factsheet 9th edition 2019 [Internet]. idf.org. 2019 [cited 2020 Jun 30]. p. 1–14. https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/159-idf-diabetes-atlas-ninth-edition-2019.html.
Werfalli M, Kassanjee R, Kalula S, Kowal P, Phaswana-Mafuya N, Levitt NS. Diabetes in South African older adults: prevalence and impact on quality of life and functional disability—as assessed using SAGE Wave 1 data. Glob Health Action. 2018;11:1449924.
Solli O, Stavem K, Kristiansen I. Health-related quality of life in diabetes: The associations of complications with EQ-5D scores. Health Qual Life Outcomes. 2010;8:18.
Redekop WK, Koopmanschap MA, Stolk RP, Rutten GEHM, Wolffenbuttel BHR, Niessen LW. Health-related quality of life and treatment satisfaction in dutch patients with type 2 diabetes. Diabetes Care. 2002;25:458–63.
Thapa S, Pyakurel P, Baral DD, Jha N. Health-related quality of life among people living with type 2 diabetes: a community based cross-sectional study in rural Nepal. BMC Public Health. 2019;19:1171.
Khunkaew S, Fernandez R, Sim J. Demographic and clinical predictors of health-related quality of life among people with type 2 diabetes mellitus living in northern Thailand: a cross-sectional study. Health Qual Life Outcomes. 2019;17:177.
Alvarado-Martel D, Velasco R, Sánchez-Hernández RM, Carrillo A, Nóvoa FJ, Wägner AM. Quality of life and type 1 diabetes: a study assessing patients’ perceptions and self-management needs. Patient Prefer Adherence. 2015;9:1315–23.
Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20:69–72.
Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–60.
Wells GA, Russell AS, Haraoui B, Ware CF, Wells GA, Russell AS, et al. Validity of quality of life measurement tool—from generic to disease-specific. J Rheumatol Suppl. 2011;88(88):2–6.
Levterova BA, Dimitrova DD, Levterov GE, Dragova EA. Instruments for disease-specific quality-of-life measurement in patients with type 2 diabetes mellitus—a systematic review. Folia Med (Plovdiv). 2013;55:83–92.
Watkins K, Connell CM. Measurement of health-related QOL in diabetes mellitus. Pharmacoeconomics. 2004;22:1109–26.
Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15(3):205–18.
Speight J, Reaney MD, Barnard KD. Not all roads lead to Rome-a review of quality of life measurement in adults with diabetes. Diabet Med. 2009;26:315–27.
Khader YS, Bataineh S, Batayha W. The Arabic version of Diabetes-39: psychometric properties and validation. Chronic Illn. 2008;4:257–63.
Adarmouch L, Sebbani M, Elansari N, Amine M. Adaptation and validation of the diabetes-39 quality-of-life questionnaire for the Moroccan population. Ser Endocrinol Diabetes Metab. 2020;2:7–14.
Boyer JG, Earp JA. The development of an instrument for assessing the quality of life of people with diabetes: diabetes-39. Med Care. 1997;35:440–53.
Krause NM, Jay GM. What do global self-rated health items measure? Med Care. 1994;32:930–42.
Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417–32.
Echevarría-guanilo ME, Bspas S, Ser P, En A, Quemados P, Bspas S, et al. Cross-cultural adaptation of the Burns Specific Pain Anxiety Scale-BSPAS to be used with Brazilian burned patients. Rev Lat Am Enfermagem. 2006;14:526–33.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25:3186–91.
Lygidakis C, Uwizihiwe JP, Kallestrup P, Bia M, Condo J, Vögele C. Community- and mHealth-based integrated management of diabetes in primary healthcare in Rwanda (D2Rwanda): the protocol of a mixed-methods study including a cluster randomised controlled trial. BMJ Open. 2019;9:e028427.
Wang J, Wang X. Structural equation modeling: applications using Mplus. 2nd ed. Hoboken: Wiley; 2019.
Byrne BM. Structural equation modeling with Mplus: basic concepts, applications, and programming. 1st ed. New York: Taylor & Francis; 2011.
Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141:2–18.
Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18:91–3.
Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126:1763–8.
Bollen K, Lennox R. Conventional wisdom on measurement: a structural equation perspective. Psychol Bull. 1991;110:305–14. https://doi.org/10.1037/0033-2909.110.2.305.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J. 1999;6:1–55.
Yu C-Y. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes [Internet]. Doctoral dissertation. University of California, Los Angeles; 2002. https://www.statmodel.com/download/Yudissertation.pdf.
Kimenyi A. Syntax and semantics of reduplication in Kinyarwanda: a semiotic account. La Linguist. 1987;23:147–56.
Sigurdardottir AK, Benediktsson R. Reliability and validity of the Icelandic version of the Problem Area in Diabetes (PAID) scale. Int J Nurs Stud. 2008;45:526–33.
Ellis JL. A standard for test reliability in group research. Behav Res Methods. 2013;45:16–24.
de Queiroz FA, Pace AE, dos Santos CB. Cross-cultural adaptation and validation of the instrument Diabetes-39 (D-39): Brazilian version for type 2 diabetes mellitus patients-stage 1. Rev Lat Am Enfermagem. 2009;17:708–15. https://doi.org/10.1590/S0104-11692009000500018.
Hundleby JD. Reviews: Nunnally, Jum. Psychometric Theory. New York: McGraw-Hill, 1967. 640 + xiii pp. $12.95. Am Educ Res J. 1968;5:431–3. https://doi.org/10.3102/00028312005003431.
Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42.
Wändell PE. Quality of life of patients with diabetes mellitus an overview of research in primary health care in the Nordic countries. Scand J Prim Heal Care. 2005;3432:68–74.
Perrin NE, Davies MJ, Robertson N, Snoek FJ, Khunti K. The prevalence of diabetes-specific emotional distress in people with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2017;34:1508–20.
Tapela N, Habineza H, Anoke S, Harerimana E, Mutabazi F, Hedt-Gauthier B, et al. Diabetes in rural Rwanda: high retention and positive outcomes after 24 months of follow-up in the setting of chronic care integration. Int J Diabetes Clin Res. 2016 [cited 2020 Jul 5];3. http://clinmedjournals.org/articles/ijdcr/international-journal-of-diabetes-and-clinical-research-ijdcr-3-058.php?jid=ijdcr.
Gill GV, Mbanya J-C, Ramaiya KL, Tesfaye S. A sub-Saharan African perspective of diabetes. Diabetologia. 2008;52:8.
Mauvais-Jarvis F, Sobngwi E, Porcher R, Riveline J-P, Kevorkian J-P, Vaisse C, et al. Ketosis-prone type 2 diabetes in patients of sub-Saharan African origin: clinical pathophysiology and natural history of -cell dysfunction and insulin resistance. Diabetes. 2004;53:645–53. https://doi.org/10.2337/diabetes.53.3.645.
Papathanasiou A, Koutsovasilis A, Shea S, Philalithis A, Papavasiliou S, Melidonis A, et al. The Problem Areas in Diabetes (PAID) scale: psychometric evaluation survey in a Greek sample with type 2 diabetes. J Psychiatr Ment Health Nurs. 2014;21:345–53.
Ferrari AL, Baptista PCP, Felli VEA, Coggon D. Translation, adaptation and validation of the “Cultural and Psychosocial Influences on Disability (CUPID) Questionnaire” for use in Brazil. Rev Lat Am Enfermagem. 2010;18:1092–8.
Novato TdS, Grossi SAA, Kimura M. Cultural adaptation and validation of the “Diabetes Quality of Life for Youths” measure of Ingersoll and Marrero into Brazilian culture. Rev Lat Am Enfermagem. 2008;16:224–30.
Acknowledgements
We extend our gratitude to Mireille Uwineza, Marie Rose Uwizeye, Anastase Nzeyimana, Esperance Mukangango, Hortense Umurerwa, and Janvier Kayitare for their help in conducting the cognitive interviews and data collection; and to Josiane Uwineza, John Doldo IV and Jake Freyer for the translations and participation in the expert panel. Finally, we would like to thank Dr Nicholas Karugahe and Dr Garry Welch for his support and guidance.
Funding
The study was supported by the Karen Elise Jensens Foundation and the Universities of Luxembourg and Aarhus. The funding sources had no role in study design, data collection and analysis, interpretation of data, or writing the manuscript.
Author information
Authors and Affiliations
Contributions
JPU, CL, CV and PK conceptualised the study and developed the design. JPU overviewed the data collection, analysis, and interpretation of results. CL overviewed parts of the data collection and conducted statistical analyses. MB carried out the statistical analysis. JPU, CL, CV, NS and PK overviewed the entire paper. DD and BAK participated in the translations and expert panel sessions. All authors contributed to editing and revising the manuscript critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no known competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix
. The Kinyarwanda Version of the Diabetes-39 (D-39) Questionnaire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Uwizihiwe, J.P., Lygidakis, C., Bia, M. et al. Cultural adaptation and psychometric evaluation of the Kinyarwanda version of the diabetes-39 (D-39) questionnaire. Health Qual Life Outcomes 20, 122 (2022). https://doi.org/10.1186/s12955-022-02034-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-022-02034-5