Abstract
Background
Patients with sickle cell disease (SCD) experience daily pain and acute episodes known as sickle cell pain crises (SCPCs). The Sickle Cell Pain Diary-Caregiver Report (SCPD-C) is an observer-reported diary for use by caregivers of children ages < 12 years with SCD. This study reports on the content validity of the SCPD-C.
Methods
The SCPD-C was developed based on a literature review, measurement expert input, and a patient advisory board including clinicians. Three rounds of interviews (including both concept elicitation and cognitive debriefing methodologies) were conducted with caregivers of children with SCD aged < 12 to evaluate the content validity of the SCPD-C.
Results
Across three rounds of interviews, caregivers confirmed concepts in the SCPD-C and described observed impacts that were important and were added. Overall, caregivers evaluated the SCPD-C as easy to understand, with some minor adaptations for clarity. Additionally, the diary was split into two versions based on the child’s age and school enrollment status (SCPD-CS for school-aged and SCPD-CN for non-school age children).
Conclusions
Caregivers provided valuable input that led to important additions and changes to the measures. The SCPD-CS and SCPD-CN are appropriate and fit-for-purpose observer-reported outcome measures of SCPC-related pain frequency and severity, and impacts on health-related quality of life.
Similar content being viewed by others
Introduction
Sickle cell disease (SCD) is a genetic, progressive disease affecting approximately 100,000 children and adults in the United States (US) [1]. SCD particularly affects African Americans and Hispanic Americans in the US, as 1 out of every 365 African-Americans are born with SCD and 1 out of every 16,300 Hispanic Americans are born with SCD [1,2,3]. Starting in early childhood, clinical features of SCD include pain, fatigue, cognitive difficulty, jaundice, hearing loss, eye damage, nausea, insomnia, susceptibility to infections, priapism, and asthma [4,5,6,7,8]. Children and adolescents with SCD experience impacts on psychological well-being, including high pain burden, depression, perceived health-related and racial stigma [9,10,11], and reduced health-related quality of life (HRQoL) compared to peers [12].
Vaso-occlusive crises, often referred to by patients as sickle cell pain crises (SCPCs), are a hallmark complication of SCD and are associated with increased risk of morbidity and mortality [8]. SCPCs occur as a consequence of vaso-occlusion, which occurs when the lumen of one or more vessels in the microvasculature is occluded due to the formation of a multi-cellular complex. Recent research has demonstrated that overexpression of adhesion molecules such as p-selectin, on the surface of the endothelium, leukocytes and platelets in patients with SCD, plays a key role in adhering the cells together and to the surface of the endothelium [4, 13, 14]. SCPCs are characterized by acute, often debilitating pain, and have been reported as the most problematic complication of SCD in children and adults [5]. SCPCs can lead to life-threatening events including stroke and acute chest syndrome [4, 5, 15], have been shown to impact patients’ quality of life and ability to function [8], and are a primary cause of healthcare resource utilization (HCRU) [6,7,8, 16, 17].
While many studies have focused on evaluating rates of mortality, medical expenditures, or HCRU (i.e., hospitalizations and emergency department visits) among patients with SCD [18,19,20], fewer studies have focused on outcomes such as HRQoL and daily functioning to provide a more complete understanding of the patient experience [21,22,23]. As newborn screening for SCD in the US has become routine [24] and infant mortality rates have decreased [25], the goal of treatment has shifted toward improving the quality of patients’ lives [26] rather than focusing only on reducing mortality. In recognition of these new treatment goals, it is important to ensure that clinicians and researchers have measurement strategies that appropriately assess the types of outcomes that are most relevant to patients. Reliance on hospital records and HCRU alone may not be sufficient to capture the totality of the patient experience, particularly for pediatric patients whose pain is often managed at home [7]. As such, alternative measures that provide a more comprehensive evaluation of the daily experience of patients with SCD, and in particular children with SCD, should be considered.
Daily diaries represent one way to evaluate outcomes that may be especially difficult to capture through medical records, during clinic visits, or with less-frequently administered surveys. Because SCD-related pain can occur with or without an SCPC, vary day-to-day, and the onset, severity, and impacts of SCPCs are both unpredictable and variable, evaluation of such experiences may be best measured through daily diaries. Prior studies using a daily diary self-report format for children with SCD have included measures primarily focused on capturing how pain is managed at home and how pain impacts daily and physical activities [16, 27,28,29,30,31]. Despite the utility of self-report daily diaries, there are limitations when this methodology is applied to specific populations. In particular, guidelines suggest that children < 5 years old cannot provide reliable and valid self-report data [32]. While children ages 5–11 may be able to self-report, they may experience difficulty understanding the survey content, which can affect the reliability of data obtained through these measures [32]. Moreover, research has suggested that when caregivers enter daily diary data on behalf of their children, adherence for completing the daily diary is increased [16]. Given the utility of daily diaries in assessing pain in children with SCD, along with the constraints that exist in obtaining self-reported data from children under the age of 12, assessment of pain and other impacts of SCD in this specific population may be best accomplished through use of a daily observer-reported outcome (ObsRO) diary.
The Sickle Cell Pain Diary—Caregiver Report (SCPD-C) was developed as a daily ObsRO measure for caregivers of children with SCD who are under the age of 12. The objective of this study was to evaluate the content validity of the SCPD-C, through a series of qualitative interviews with caregivers of children with SCD.
Methods
Diary development
A draft version of the daily diary, titled SCPD-C v.01, was developed using multiple resources. First, key concepts were identified from the literature, using a structured review of pre-existing instruments that measure pain and HRQoL in an SCD population, and a published conceptual model of SCD impacts [33]. Additionally, consultation with measurement experts, feedback collected during a day-long patient advisory board meeting that included clinicians, and individual discussions with clinicians helped to identify additional concepts which were used by the research team to draft the items.
The SCPD-C v.01 was intended to measure pain severity, pain duration, fatigue, medication use in children with SCD to manage pain, and impact of pain on the child’s HRQoL during an SCPC, as observed by the caregiver. The diary included 11 items that pertained to caregivers’ observations during an SCPC and the subsequent impact of the SCPC on their child’s HRQoL in the past 24 h. Most items either used a 5-point Likert scale (e.g., “Not at All” to “Extremely”) or were Yes/No. One item asked the caregiver to provide the approximate number hours and minutes of the observed SCPC. If signs of an SCPC were not observed in the past 24 h, the caregiver would complete one item using a 5-point Likert scale about non-SCPC-related pain their child may have experienced.
Participant sample
The study was approved by the New England Independent Review Board, and informed consent was obtained from all participants. Participants were invited to participate in the study through collaboration with a healthcare research recruitment agency. Individuals were eligible to participate in the study if they were a primary caregiver of a child < 12 years of age with SCD, observed their child experiencing at least one SCPC in the 12 months prior to screening, spoke English fluently, and were willing and able to participate in a 60–90 min interview.
Interview procedure
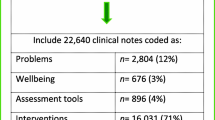
Interviews with caregivers of children with SCD were designed to collect data on the relevance, comprehensiveness, and comprehensibility of the SCPD-C. To meet this objective, two different interview approaches were employed: concept elicitation (CE) and cognitive debriefing (CD). An overview of each round of interviews is presented in Fig. 1. Interviews were conducted across three rounds in multiple US locations in-person and via telephone using semi-structured interview guides. All interviews were completed by experienced researchers with training in conducting qualitative interviews, and were audio-recorded with the permission of each participant. After the interviews were completed, caregivers received an honorarium in compensation for their time.
Description of study methodology, divided by interview round. CD cognitive debriefing, CE concept elicitation, SCD sickle cell disease, SCPD-C sickle cell pain diary-caregiver report, SCPD-CN sickle cell pain diary-caregiver report for non-school age children, SCPD-CS sickle cell pain diary-caregiver report for school age children
Concept elicitation
An open-ended CE approach was used across the first two rounds of interviews to explore concepts of SCD that were important to participants, helping to provide evidence that the SCPD-C is comprehensive in the concepts it includes and informing additional content. Caregivers were asked to report on their observations of their child’s daily experience of SCD symptoms and the impact of those symptoms on aspects of their child’s life. They were then asked to discuss their child’s symptoms, signs, or changes in behaviors during an SCPC, what a typical day looks like during and outside of an SCPC, and what treatment they seek when their child is experiencing an SCPC.
Cognitive debriefing
A CD approach was used in all three rounds of interviews to test the relevance and comprehensibility of each element of the diary (instructions, items, response options, and skip patterns). A think-aloud process was used: caregivers were asked to complete the diary, answering all items while verbalizing their thoughts about the item and its response options [34]. Caregivers were then asked to describe any aspects of the diary they found challenging or confusing; the interviewer also probed areas that appeared to be confusing based on caregivers’ verbal and non-verbal cues during the think-aloud process. Finally, the interviewer asked a set of structured queries to ensure the relevance and comprehensibility of any elements of the diary that had not already been discussed.
Data analysis
Interview audio-recordings were transcribed verbatim, and transcripts were coded and analyzed using identical methodology for each round of interviews. All interview data were coded using NVivo version 11.0 software.
For the CE approach, interview data were content coded and analyzed using content thematic analysis [35]. This strategy is in accordance with the principles of grounded theory [36]. Saturation—the point at which no new relevant information emerges– was evaluated using a constant comparative approach, whereby initial interviews were analyzed and compared contemporaneously with subsequent interviews [36,37,38].
For the CD approach, after each interview, a Microsoft Excel spreadsheet was populated with any issues that emerged that suggested a change be made. Such issues included survey elements (item, response choice, etc.) perceived as confusing or difficult to answer, or suggestions to improve clarity. Each unique suggestion was recorded in a single row, with a separate column for each interview. Next, transcripts of each interview were reviewed for quality then cross-checked against the Excel spreadsheet to confirm all data had been coded correctly. Changes to the diary were tracked in an item-tracking matrix [39, 40].
Results
Results of all three rounds of caregiver interviews are presented below. In total, interviews were conducted with 22 caregivers (see Table 1 for demographic information). A summary of all revisions made to the diary as a result of feedback from the caregiver interviews is presented in Fig. 2.
Concept elicitation
During the CE portion of round one and round two interviews (n = 9), caregivers generally differentiated between every day experiences of SCD and experiences specific to SCPCs.
Symptoms
The two most frequently reported symptoms related to SCD observed on a day-to-day basis were pain and tiredness (both n = 5). SCD symptoms observed day-to-day included: fatigue, swelling, jaundice (all n = 2), constipation, bone aches, vomiting, headaches, loss of appetite, and shortness of breath (all n = 1).
All caregivers during round one and round two interviews (n = 9) reported observing their children experience intense pain during an SCPC, and that their children communicated their pain through verbal report or through nonverbal expressions and behaviors such as crying, moaning, screaming, irritability, or a change in posture. Other less common symptoms observed during an SCPC included lack of appetite (n = 3), vomiting (n = 2), dehydration, fatigue, jaundice, numbness, infection, and a high fever (all n = 1). SCPCs varied in length ranging from two hours to two weeks. The number of SCPCs observed by caregivers in a year also varied (range: 1–20).
Impacts and healthcare resource utilization
Caregivers reported numerous aspects of their child’s daily life that are negatively impacted by SCD (Table 2). Impacts were either the result of daily symptoms, or caregivers imposing limitations on their child due to concern of triggering an SCPC. Caregivers also reported impacts of SCPCs on multiple aspects of their child’s life (Table 3). Impacts were the result of SCPC symptoms (especially pain) or medical intervention.
Most caregivers indicated seeking treatment for their child’s SCPCs outside of the home every time or almost every time they experience an SCPC (n = 8). Six caregivers reported immediately seeking care in the emergency department after observing signs of an SCPC, such as change in behavior (e.g., screaming or crying), fever, or becoming immobile. All caregivers in rounds one and two (n = 9) reported medication use and other treatment during an SCPC, such as over-the-counter medications, prescription medications, intravenous therapy, and transfusions.
Caregiver burden during an SCPC
All caregivers described impacts on their own lives as a result of their child’s SCPCs (n = 9; Table 4). Work absenteeism (n = 7) was the most commonly reported impact. While some caregivers reported employers accommodated their need to miss work to care for their child, others described less flexibility in their work schedules. For these caregivers, missing work to care for their child meant the loss of income or risks to their overall employment status. Caregivers also described emotional health problems (n = 6) that resulted from watching their child experience SCPCs.
Saturation
A saturation analysis was conducted to evaluate whether additional CE interviews were needed. Thematic saturation was reached by the 9th interview indicating no need for additional CE interviews. Specifically, in interviews 1–2, 36 concepts were identified; in interviews 3–4, 23 new concepts were identified. Ten new concepts were identified in interviews 5–6, 5 new concepts were identified in interviews 7–8, and no new concepts were identified in interview 9. The lack of new concepts in the final interview confirmed that 9 interviews were sufficient to reach saturation.
Cognitive debriefing
Round one
Round one CD interviews (n = 6) tested the SCPD-C v.01. Overall, caregivers reported the diary was relevant, easy to answer, and would not be burdensome to complete during an SCPC, even if their child was in the hospital. All caregivers (n = 6) reported the initial instructions were clear, though a definition of the term “caregiver” was added. Instructions regarding daily experiences were added and edited for clarity.
Several items were revised in response to caregiver feedback (see Table 5 for a sample of SCPD-C v.01 items that were tested and modified as a result of round one interviews). Revisions were made to several items to increase ease of responding, reduce confusion, or provide a more complete set of response options. One item was removed from the diary entirely, while eight items were added (see Table 6 for examples of added items with quotes from caregivers). These revisions resulted in the SCPD-C v.02.
One caregiver reported that items regarding school attendance, school work, and daily activities (including chores, social and recreational activities) were not appropriate for her to complete because her child was three years old and did not yet attend school or do the same types of activities as older children. She suggested removing these items when the diary is to be completed by a caregiver of a child not yet in elementary school. This feedback suggested that two different diaries would be most appropriate: one for caregivers of young children not yet attending school, and one for caregivers of school-age children. To explore this insight, the interview guide for round two was modified to specifically ask caregivers whether splitting the diary into two versions would be necessary.
Round two
The purpose of round two interviews (n = 3) was to evaluate the SCPD-C v.02, confirming that no additional concepts needed to be included in the diary, and evaluating the clarity and appropriateness of all items and response choices.
Overall, caregivers confirmed the relevance and comprehensiveness of the diary items and initial instructions. Minor edits were made to the wording of various items to improve clarity. One item’s response options were edited based on caregiver feedback.
Caregivers in round two affirmed the diary should take into account the age of the child and whether or not they are attending school. Based on caregiver feedback, the diary was split into two versions: the SCPD-CS v.01 for school-age children and the SCPD-CN v.01 for non-school age children. An item was added to the start of the diary asking if the child currently attends school; this item ensures administration of the correct version during electronic implementation.
The SCPD-CN v.01 mirrored the SCPD-CS v.01 with two primary exceptions. One item on interference with schoolwork was removed. Additionally, an item was added asking the age of the child, and skip patterns were added in the SCPD-CN v.01 to allow caregivers of children under the age of two to skip items that are difficult to answer based on the child’s age. Specifically, caregivers of children < 2 years old would now skip items related to their child’s emotional difficulty and interference in activities of daily living and social/recreational activities. These changes allow the SCPD-CN to be appropriate for all non-school age children, regardless of age.
Round three
Round three interviews used only cognitive debriefing techniques and evaluated the two versions of the caregiver diary separately. Seven caregivers of children < 12 years of age who were currently enrolled in school completed and evaluated the SCPD-CS v.01. Six caregivers of non-school-age children evaluated the SCPD-CN v.01. These interviews reaffirmed the importance of establishing two caregiver diaries to capture the unique experiences of children with SCD enrolled in school as compared to children with SCD not yet enrolled in school. Items were viewed as relevant, appropriate, and understandable to caregivers of children < 12 years old. No new items were added. Minor edits were made to the diaries to increase clarity, accuracy, and comprehension. For example, an edit was made to clarify the definition of “school,” in order to specify that school includes kindergarten and all subsequent grades. Additional minor changes were made to the diaries to facilitate electronic administration, resulting in the SCPD-CS v1.0 and the SCPD-CN v1.0.
Summary of final diary content
As a result of the three rounds of caregiver interviews, 19 items were included in the SCPD-CS v1.0 and 18 items were included in the SCPD-CN v1.0. The final diaries measure pain severity, pain duration, fatigue, and medication use and HCRU in children with SCD to manage pain, and impact of pain on the child’s HRQoL during an SCPC, as observed by the caregiver (Table 7). The final diaries also include non-SCPC related pain and its impact on the child’s HRQoL observed by the caregiver during times when signs of an SCPC were not observed in the past 24 h.
Discussion
The goal of this study was to evaluate the content validity of an ObsRO measure diary (SCPD-C) for caregivers of children with SCD aged < 12 years. Early caregiver interviews revealed that the impacts and experiences of school-aged children differed meaningfully from those of non-school-aged children. As a result, the diary was split into two versions: the SCPD-CS (for school-aged children) and SCPD-CN (for non-school-aged children). Both diaries include questions related to the pain, sleep, and fatigue on days the child is not experiencing an SCPC; additional questions related to SCPC duration, treatment, impacts, and interference with various daily activities are administered on days the child is experiencing an SCPC. Both versions of the diary also provide the opportunity for the caregiver to report on impacts they have experienced as a result of their child’s SCD. The precise item content is tailored based on the child’s age and school enrollment status. Both diaries capture the daily impact of SCD and have the ability to capture the variability within and across SCPCs. The inclusion of items related to HRQoL allows for a broader characterization of a patient’s health status, moving beyond what can be assessed by HCRU data alone, ultimately providing a more holistic view of the impact of SCPCs and SCD on children.
Caregivers described the burdensome impact SCD and SCPCs have on their child’s overall HRQoL. Concepts that emerged as especially important were the impact of SCD on the child’s emotional health, social and recreational activities, physical functioning, daily activities, and school (both school attendance and schoolwork). These same issues were further compounded by the impact of SCPCs; and SCPCs additionally impacted sleep. In addition to the myriad of impacts on HRQoL experienced by children with SCD, caregivers reported a high rate of HCRU for SCPCs as compared to published HCRU rates of children with SCD [7, 41, 42]. Given that healthcare visits generally increase with age in children with SCD up to early adulthood [43], these findings support the importance of capturing children’s healthcare experience and impacts on HRQoL. Caregivers themselves experienced substantial emotional and work-related burdens as a result of caring for their children during an SCPC.
These findings should be interpreted in the light of some limitations. One limitation is that this study tested a paper version in all three rounds of interviews; future work should include usability testing of the programmed survey in electronic format. An electronic administration, such as on a smartphone or tablet, will allow for management of skip patterns, reminders to complete the diary, and include other features that will make it easier for caregivers to complete the diary.
Additionally, the inclusion of various types of caregivers (e.g., legal guardian, single parent, independent caregiver) and additional male caregivers is recommended in future work as our sample included 18 parents and 18 female caregivers. Seventeen caregivers in our sample had at least some college education. Future studies should include caregivers with a greater mix of education levels. Additional validation testing in ex-US samples should be conducted if the diaries will be used outside the US.
Strengths of this study include having a rigorous research design with many in-person interviews in multiple regions, a large sample size given SCD is a rare condition, and input from expert clinicians, and a patient advisory board in the instrument design phase. The sample size of this study was guided in part by saturation analysis findings, and by literature recommendations for instrument development. Thematic saturation was met after the 9th interview. Additional cognitive debriefing interviews (round three) were needed to test that the SCPD-CS and SCPD-CN were appropriate, easy to understand, and relevant to caregiver observed experiences.
While some measures, such as the PedsQL Sickle Cell Disease Module, have been developed and tested to capture the impact of SCD symptoms on children’s with SCD HRQoL [44, 45], this is the first daily diary with evidence of content validity that is designed for a caregiver to report for children with SCD ages < 12 years. When children have SCPCs, they are often unable to move or think clearly, and completing a survey themselves is not feasible. Caregivers are able to observe the impact of SCD and SCPCs on children and report daily. The content of the diaries is similar to the PedsQL Sickle Cell Disease Module as the diaries also capture the pain impact, emotional impact, and treatment management of pain. The ability to report daily is important given the fluctuating nature of SCPCs in terms of duration, severity, and impacts within and across individuals. Additionally, the diaries’ capture caregiver’s burden during their child’s SCPC event. Clinicians (from the day-long patient advisory board meeting) and caregivers felt having an available daily diary, preferably completed on a smartphone or other electronic device, would be useful to improve communication with clinicians and hospitals and improve patient care.
While these findings support the content validity of the SCPD-CS v1.0 and SCPD-CN v1.0, additional work including development of scoring algorithms and user’s manuals, and conducting psychometric evaluation of the diaries with larger sample sizes will be needed. Use of the diaries is anticipated in future clinical trials with caregivers of children who experience SCPCs as a way to capture the HRQoL impacts of new interventions designed to reduce the frequency and intensity of SCPCs.
Conclusions
The SCPD-CS v1.0 and SCPD-CN v1.0 are appropriate and fit-for-purpose ObsRO measures of SCPC-related pain frequency and severity and the impacts on HRQoL. This study highlights the important of including caregiver input when developing a pediatric ObsRO.
Availability of data and materials
Specific data points can be made available upon reasonable request, due to the complex qualitative nature of the study design.
Abbreviations
- SCD:
-
Sickle cell disease
- SCPC:
-
Sickle cell pain crisis
- SCPD-C:
-
Sickle Cell Pain Diary-Caregiver Report
- SCPD-CS:
-
Sickle Cell Pain Diary-Caregiver Report for School Age Children
- SCPD-CN:
-
Sickle Cell Pain Diary-Caregiver Report for Non-School Age Children
- US:
-
United States
- HRQoL:
-
Health-related quality of life
- HCRU:
-
Healthcare resource utilization
- ObsRO:
-
Observer-reported outcome
- CE:
-
Concept elicitation
- CD:
-
Cognitive debriefing
References
Centers for Disease Control and Prevention. Sickle Cell Disease (SCD): Data & Statistics. December 17, 2020. https://www.cdc.gov/ncbddd/sicklecell/data.html. Accessed 28 Sep 2021.
Brousseau DC, Panepinto JA, Nimmer M, Hoffmann RG. The number of people with sickle-cell disease in the United States: national and state estimates. Am J Hematol. 2010;85:77–8. https://doi.org/10.1002/ajh.21570.
Nelson SC, Hackman HW. Race matters: perceptions of race and racism in a sickle cell center. Pediatr Blood Cancer. 2013;60:451–4. https://doi.org/10.1002/pbc.24361.
Kanter J, Kruse-Jarres R. Management of sickle cell disease from childhood through adulthood. Blood Rev. 2013;27:279–87. https://doi.org/10.1016/j.blre.2013.09.001.
U.S. Food and Drug Administration. The FDA Encourages New Treatments for Sickle Cell Disease. 2014. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm418232.htm. Accessed 25 Sep 2017.
Ballas SK, Kesen MR, Goldberg MF, Lutty GA, Dampier C, Osunkwo I, et al. Beyond the definitions of the phenotypic complications of sickle cell disease: an update on management. Sci World J. 2012;2012: 949535. https://doi.org/10.1100/2012/949535.
Dampier C, Ely B, Brodecki D, Coleman C, Aertker L, Sendecki JA, et al. Pain characteristics and age-related pain trajectories in infants and young children with sickle cell disease. Pediatr Blood Cancer. 2014;61:291–6. https://doi.org/10.1002/pbc.24796.
Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research, U.S. Food and Drug Administration, editors. The Voice of the Patient_ Sickle Cell Report: A series of reports from the U.S. Food and Drug Administrations's (FDA's) Patient-Focused Drug Development Initiative; 2014.
Martin SR, Cohen LL, Mougianis I, Griffin A, Sil S, Dampier C. Stigma and pain in adolescents hospitalized for sickle cell vasoocclusive pain episodes. Clin J Pain. 2018;34:438–44. https://doi.org/10.1097/AJP.0000000000000553.
Wakefield EO, Popp JM, Dale LP, Santanelli JP, Pantaleao A, Zempsky WT. Perceived racial bias and health-related stigma among youth with sickle cell disease. J Dev Behav Pediatr. 2017;38:129–34. https://doi.org/10.1097/DBP.0000000000000381.
Badawy SM, Thompson AA, Lai J-S, Penedo FJ, Rychlik K, Liem RI. Adherence to hydroxyurea, health-related quality of life domains, and patients’ perceptions of sickle cell disease and hydroxyurea: a cross-sectional study in adolescents and young adults. Health Qual Life Outcomes. 2017;15:136. https://doi.org/10.1186/s12955-017-0713-x.
Adeyemo TA, Ojewunmi OO, Diaku-Akinwumi IN, Ayinde OC, Akanmu AS. Health related quality of life and perception of stigmatisation in adolescents living with sickle cell disease in Nigeria: A cross sectional study. Pediatr Blood Cancer. 2015;62:1245–51. https://doi.org/10.1002/pbc.25503.
Ugwu AO, Ibegbulam OG, Nwagha TU, Madu AJ, Ocheni S, Okpala I. Clinical and Laboratory Predictors of Frequency of Painful Crises among Sickle Cell Anaemia Patients in Nigeria. J Clin Diagn Res. 2017;11:EC22–5. https://doi.org/10.7860/JCDR/2017/26446.10042.
Merle NS, Paule R, Leon J, Daugan M, Robe-Rybkine T, Poillerat V, et al. P-selectin drives complement attack on endothelium during intravascular hemolysis in TLR-4/heme-dependent manner. Proc Natl Acad Sci U S A. 2019;116:6280–5. https://doi.org/10.1073/pnas.1814797116.
Bender MA. Gene Reviews: Sickle Cell Disease. 1993–2017. https://www.ncbi.nlm.nih.gov/books/NBK1377/. Accessed 25 Sep 2017.
Heath LE, Heeney MM, Hoppe CC, Adjei S, Agbenyega T, Badr M, et al. Successful utilization of an electronic pain diary in a multinational phase 3 interventional study of pediatric sickle cell anemia. Clin Trials. 2017;14:563–71. https://doi.org/10.1177/1740774517723307.
Lewandowski AS, Palermo TM, Kirchner HL, Drotar D. Comparing diary and retrospective reports of pain and activity restriction in children and adolescents with chronic pain conditions. Clin J Pain. 2009;25:299–306. https://doi.org/10.1097/AJP.0b013e3181965578.
Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303:1288–94. https://doi.org/10.1001/jama.2010.378.
Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Hartzema AG. The cost of health care for children and adults with sickle cell disease. Am J Hematol. 2009;84:323–7. https://doi.org/10.1002/ajh.21408.
Shankar SM, Arbogast PG, Mitchel E, Cooper WO, Wang WC, Griffin MR. Medical care utilization and mortality in sickle cell disease: a population-based study. Am J Hematol. 2005;80:262–70. https://doi.org/10.1002/ajh.20485.
Wallen GR, Minniti CP, Krumlauf M, Eckes E, Allen D, Oguhebe A, et al. Sleep disturbance, depression and pain in adults with sickle cell disease. BMC Psychiatry. 2014;14:207. https://doi.org/10.1186/1471-244X-14-207.
Dampier C, LeBeau P, Rhee S, Lieff S, Kesler K, Ballas S, et al. Health-related quality of life in adults with sickle cell disease (SCD): a report from the comprehensive sickle cell centers clinical trial consortium. Am J Hematol. 2011;86:203–5. https://doi.org/10.1002/ajh.21905.
Matthie N, Hamilton J, Wells D, Jenerette C. Perceptions of young adults with sickle cell disease concerning their disease experience. J Adv Nurs. 2016;72:1441–51. https://doi.org/10.1111/jan.12760.
El-Haj N, Hoppe C. Newborn screening for SCD in the USA and Canada. IJNS. 2018;4:36. https://doi.org/10.3390/ijns4040036.
Quinn CT, Rogers ZR, Buchanan GR. Survival of children with sickle cell disease. Blood. 2004;103:4023–7. https://doi.org/10.1182/blood-2003-11-3758.
Chaturvedi S, DeBaun MR. Evolution of sickle cell disease from a life-threatening disease of children to a chronic disease of adults: The last 40 years. Am J Hematol. 2016;91:5–14. https://doi.org/10.1002/ajh.24235.
Maikler VE, Broome ME, Bailey P, Lea G. Childrens’ and adolescents’ use of diaries for sickle cell pain. J Soc Pediatr Nurs. 2001;6:161–9.
Dampier C, Ely E, Eggleston B, Brodecki D, O’Neal P. Physical and cognitive-behavioral activities used in the home management of sickle pain: a daily diary study in children and adolescents. Pediatr Blood Cancer. 2004;43:674–8. https://doi.org/10.1002/pbc.20162.
Dampier C, Ely B, Brodecki D, O’Neal P. Characteristics of pain managed at home in children and adolescents with sickle cell disease by using diary self-reports. J Pain. 2002;3:461–70.
Dampier C, Ely E, Brodecki D, O’Neal P. Home management of pain in sickle cell disease: a daily diary study in children and adolescents. J Pediatr Hematol Oncol. 2002;24:643–7. https://doi.org/10.1097/00043426-200211000-00008.
Karlson CW, Baker AM, Bromberg MH, David Elkin T, Majumdar S, Palermo TM. Daily pain, physical activity, and home fluid intake in pediatric sickle cell disease. J Pediatr Psychol. 2017;42:335–44. https://doi.org/10.1093/jpepsy/jsw061.
Matza LS, Patrick DL, Riley AW, Alexander JJ, Rajmil L, Pleil AM, Bullinger M. Pediatric patient-reported outcome instruments for research to support medical product labeling: report of the ISPOR PRO good research practices for the assessment of children and adolescents task force. Value Health. 2013;16:461–79. https://doi.org/10.1016/j.jval.2013.04.004.
Treadwell MJ, Hassell K, Levine R, Keller S. Adult sickle cell quality-of-life measurement information system (ASCQ-Me): conceptual model based on review of the literature and formative research. Clin J Pain. 2014;30:902.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 6th ed. California: SAGE Publications, Inc.; 2005.
Assarroudi A, Heshmati Nabavi F, Armat MR, Ebadi A, Vaismoradi M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J Res Nurs. 2018;23:42–55. https://doi.org/10.1177/1744987117741667.
Corbin JM, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks: SAGE Publications, Inc.; 2015.
Kolb SM. Grounded theory and the constant comparative method: Valid research strategies for educators. JETERAPS. 2012;3:83–6.
Turner-Bowker DM, Lamoureux RE, Stokes J, Litcher-Kelly L, Galipeau N, Yaworsky A, et al. Informing a priori sample size estimation in qualitative concept elicitation interview studies for clinical outcome assessment instrument development. Value Health. 2018;21:839–42. https://doi.org/10.1016/j.jval.2017.11.014.
U.S. Food & Drug Administration. Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. 2009. https://www.fda.gov/downloads/drugs/guidances/ucm193282.pdf. Accessed 4 Jun 2018.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, Ring L. Content validity–establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2–assessing respondent understanding. Value Health. 2011;14:978–88. https://doi.org/10.1016/j.jval.2011.06.013.
Raphael JL, Dietrich CL, Whitmire D, Mahoney DH, Mueller BU, Giardino AP. Healthcare utilization and expenditures for low income children with sickle cell disease. Pediatr Blood Cancer. 2009;52:263–7. https://doi.org/10.1002/pbc.21781.
Mvundura M, Amendah D, Kavanagh PL, Sprinz PG, Grosse SD. Health care utilization and expenditures for privately and publicly insured children with sickle cell disease in the United States. Pediatr Blood Cancer. 2009;53:642–6. https://doi.org/10.1002/pbc.22069.
Blinder MA, Vekeman F, Sasane M, Trahey A, Paley C, Duh MS. Age-related treatment patterns in sickle cell disease patients and the associated sickle cell complications and healthcare costs. Pediatr Blood Cancer. 2013;60:828–35. https://doi.org/10.1002/pbc.24459.
Panepinto JA, Torres S, Varni JW. Development of the PedsQLTM sickle cell disease module items: Qualitative methods. Qual Life Res. 2012;21:341–57.
Panepinto JA, Torres S, Bendo CB, McCavit TL, Dinu B, Sherman-Bien S, et al. PedsQLTM sickle cell disease module: feasibility, reliability, and validity. Pediatr Blood Cancer. 2013;60:1338–44. https://doi.org/10.1002/pbc.24491.
Acknowledgements
Not applicable.
Funding
This study was funded by Novartis Pharmaceutical Corporation.
Author information
Authors and Affiliations
Contributions
MKW, MB, DD, and PS conceived this study and made substantive contributions to the study design, analysis, and interpretation. MKW, CS, AF, and PS conducted interviews and coded interview data. All authors contributed to interpretation of results. MKW, CS, AF, AAR, and DS drafted the first version of the manuscript and all authors reviewed that version and later drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The informed consent form, protocol, and recruitment materials were approved by the New England Independent Review Board (IRB #120170305). All participants provided consent to participate prior to participating in the interview.
Consent for publication
Not applicable.
Competing interests
MKW, AF, AAR, and CS are full-time employees of QualityMetric and received research funding from Novartis Pharmaceuticals Corporation to conduct the study. MB and DD are full-time employees of the study sponsor, Novartis Pharmaceuticals Corporation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
White, M.K., Foster, A.M., Bailey, M. et al. Content validation of observer-reported sickle cell pain diaries (SCPD-CS and SCPD-CN): results from interviews with caregivers. Health Qual Life Outcomes 19, 257 (2021). https://doi.org/10.1186/s12955-021-01888-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-021-01888-5