Abstract
Background
VascuQoL-6 (VQ-6) is a disease-specific quality of life (QoL) instrument validated for use in clinical practice and vascular registries before and after treatment for peripheral arterial disease (PAD). To improve future interpretation of self-reported outcome, an unselected cohort was followed through one year to provide observational data after both conservative and invasive treatment.
Methods
Consecutive patients with intermittent claudication (IC) or critical limb ischemia (CLI) were included. All patients completed VQ-6 and Short Form-36 (SF-36), and were evaluated with ankle-brachial index (ABI) measurement pre- and post-exercise, a constant load treadmill test and clinical consultation at baseline and after one year. Change statistics and correlation analysis were used to describe self-reported outcome after conservative and invasive treatment for PAD.
Results
One hundred seventy-one patients with peripheral arterial disease (PAD) were included, 70 (41%) female. 147 (86%) of the patients suffered from IC. 136 (80%) patients had one-year follow up, death, amputation and withdrawal were the major causes of loss to follow-up. Forty-eight patients (35%) evaluated their health to be unchanged compared to one year ago. There was a strong correlation between self-reported general health status based on SF-36 item 2 and VQ-6 summary score (Spearmans rho = − 0.536). Patients admitted to invasive intervention (endovascular or surgery) improved in all domains of SF-36, and in the physical component summary score (SF-36 PCS). Patients admitted to best medical treatment, smoking cessation and walking exercise (conservative group) improved only in the physical domains. There was significant improvement in VQ-6 summary score for both groups, mean 2.20 (95%CI 1.14–3.27) in the conservative group, 4.68 (95%CI 3.67–5.70) in the invasive group. VQ-6 sum score improved more than four points for 56% in the invasive group, 36% in the conservative group.
Conclusions
Treatment for symptomatic PAD, both invasive and conservative, improves self-reported health status and disease specific QoL after one year. Interpretation of patient-reported outcome measured with VQ-6 after surgery or endovascular treatment must be seen in light of the improvement from conservative treatment alone.
Trial registration
ISRCTN14846962 (retrospectively registered).
Similar content being viewed by others
Background
Patient reported outcome measures (PROMS), such as self-reported health status and disease-specific quality of life (QoL), are regarded as important and valuable outcome variables after treatment for peripheral arterial disease (PAD), supplementing the clinical evaluation and evaluation of peripheral arterial pressure measurements and walking tests [1]. For patients with intermittent claudication, self-reported outcome measures can capture improvement beyond clinical testing.
VascuQoL-6 (VQ-6) is a short version of the disease-specific quality of life instrument VascuQoL-25 [2, 3], intended both for intermittent claudication (IC) and critical limb ischemia (CLI). VascuQoL-6 was found to be valid, reliable and responsive to change [4]. The VascuQoL-6 study aimed both to validate the VQ-6-instrument based on registrations at baseline and after 4 weeks, and to investigate the development in self-reported health status, measured with SF-36, and disease-specific QoL, measured with VQ-6, after one year for consecutive patients treated for peripheral arterial disease in clinical practice.
Self-reported health status (SF-36) of PAD patients are substantially reduced at baseline compared to healthy people in the same age group, but show improvement after both invasive (endovascular/surgery) and conservative treatment [4, 5]. In order to improve interpretation of future self-reported outcome measured with VQ-6 from procedural registries in vascular surgery, the validation study cohort was followed through a year as an observational study. There is a lack of knowledge of how QoL measured with VQ-6 change for patients who receive conservative treatment with best medical treatment (BMT), smoking cessation advice and walking exercise.
Purpose
The aim of this study was to investigate change in self-reported health status measured with SF-36 and VQ-6 one year after treatment for PAD, in an unselected population of conservatively and invasively treated patients.
Methods
Inclusion and exclusion
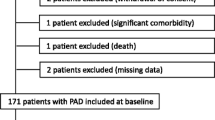
Consecutive patients with new referral for evaluation of peripheral arterial disease (IC or CLI) at the vascular surgery department at two different hospitals were invited to participate in the VascuQol-6 study, based on the information given by the referring physician. The inclusion period ran from August 2014 to August 2015. Inclusion, exclusion and follow-up of patients are described in detail in a previously published paper [4], and summarized in Fig. 1.
Patients received written information about the study and the two questionnaires, VQ-6 and SF-36, by mail before the scheduled appointment at the outpatient clinic. The questionnaires were not available to the treating physician.
Work up
In the vascular laboratory, arterial pressures were measured with a hand held Dopplerdevice, and the ankle-brachial index (ABI) was calculated. Patients with claudication were tested on a constant load treadmill with a speed of 2.5 km/h and no inclination. A post-exercise ABI drop exceeding 0.1 was regarded significant. Intermittent claudication distance (ICD) and maximum walking distance (MWD) were registered in meters. There is a ceiling effect at 416 m, as the test was terminated after 10 min for all patients.
Risk factors, comorbidity, medication and Fontaine classification [6] were registered by the vascular surgeon during the clinical consultation.
Follow-up
All eligible patients from the VascuQoL-6 study were scheduled for a new consultation with completion of questionnaires, arterial pressure measurements, treadmill-test and clinical evaluation after one year. The conservative treatment group included patients with best medical treatment (BMT) alone (information about the disease, the value of walking exercise and medical treatment) and patients with additional referral for supervised exercise therapy (SET). The invasive treatment group included patients with endovascular and/or vascular surgical procedures in addition to BMT. The referral algorithm for imaging and invasive treatment was unaltered from usual practice.
VascuQoL-6
VascuQoL-6 (VQ-6) is a short disease-specific QoL instrument intended for use in clinical practice and vascular registries [3, 4, 7]. Each of the six items scores from one to four, sum score range is from six to 24, and a higher score indicates better health.
SF-36
SF-36 (version 1) was used to measure general self-reported health status. This instrument has been used in prior validation of VascuQoL-25 [8,9,10,11] and in a range of PAD studies [12,13,14,15] . Subscale (PF –physical functioning, RP –physical role, BP –bodily pain, GH –general health, VT –vitality, SF -social functioning, RE –emotional role, MH –mental health) and component summary scoring (PCS –physical component score, MCS –mental component score) was performed using Qualimetric Health Outcomes Scoring Software 4.0, using the original scoring method [16]. This software uses the 1998 US norm population for calculation of component summary scores, as US norm has been recommended for western countries [17]. Data from the Norwegian norm population from 1998 [18] was used in Fig. 2 for illustrative purposes.
The subscale scores of SF-36 range from 0 to 100, and the highest score indicates no health-related reduction of QoL. The component summary scores relates to the normative population (mean 50, SD 10), and a score lower than 50 indicates lower QoL than the normative population.
Statistic methods
All statistics were calculated using Statistical Package for the Social Sciences version 21 (IBM/SPSS Inc., Armonk, NY, USA). Change analysis was done using t-test for normally distributed continuous data, Wilcoxon signed rank test for non-parametric continuous data and McNemar’s test for dichotomous data. The relationship between perceived general health change and change in VQ-6 sum score was investigated using non parametric statistics, Spearmans rank correlation coefficient, interpreted using Cohens criteria (1988, p79–81) (small: rho 0.1–0.29, medium 0.3–0.49, large > 0.5).
Missing data
Analysis was performed using all available data at baseline and during follow-up. For missing items for VQ-6 (2 patients, 1 and 2 missing items, conservative treatment group) we did a single imputation using the last value carried forward. One patient missed three items after treatment, and the sum score of VQ-6 was omitted from analysis. For SF-36, imputation was done using the scoring software (Qualimetric Health Outcomes Scoring Software 4.0). The mean subscale score is used if the patient has answered more than half of the items in the domain.
Results
One hundred seventy-one patients were included, 41% female. Some 53 (31%) had a previous history of evaluation or treatment for PAD. Patient characteristics are given in Table 1. Of the patients, 147 (86%) were claudicants (Fontaine IIA/B) and 24 (14%) suffered from critical limb ischemia (Fontaine III and IV). A total of 142 (83%) participated in a treadmill test. At baseline, 116 (68%) received treatment with platelet inhibitors and statins.
One hundred thirty-six patients had follow up after one year, 12 (9%) of these were treated for CLI, the remaining IC. Half of the 24 CLI patients included at baseline were lost to follow up (major amputation 6, death 3, and other 3). Arterial pressures, treadmill walking capacity and QoL-summary scores at baseline and one year follow up is shown in Table 2.
Self-reported health status
Based on item 2 in SF-36 (“Compared to one year ago, how would you rate your health in general now?”), 30 patients (22%) reported their health to be much improved, 29 (21%) somewhat improved, 48 (35%) unchanged, 25 (18%) somewhat worse, and 6 (4%) much worse.
There was a strong correlation between item 2 in SF-36 and change in VascuQoL-6 sum score, Spearmans rho = − 0.536, n = 136, p < 0.01, where a large improvement in sum score was associated with better health now than one year ago.
For the patients who reported an unchanged health status the mean change in VQ-6 summary score was 2.3 (95%CI: 1.3–3.25). For the 56 (41%) patients where the vascular surgeon evaluated the status to be unchanged, the mean change in VQ-6 summary score was 2.4 (95%CI: 1.44–3.45).
Conservative treatment group
Fifty-nine patients were treated with a conservative approach (IC/CLI: 58/1). There was significant improvement in self-reported physical health status and disease-specific QoL, as shown in Table 2.The mean change in SF-36 subscale score was largest for the physical domains (PF-physical functioning, RP-Physical role and BP –Bodily pain), as shown in Fig. 2. Figure 3 show mean score of VQ-6 at baseline and after treatment. Change in VQ-6 summary score ranged from − 6 to 12. Nine patients (15%) had reduced summary score by 2 or more scale points, 23 patients (39%) had unchanged score (− 1 to 1), and 27 patients (46%) had increased score by 2 or more scale points. Of these, 21 (36%) had increased their summary score by 4 points or more, as shown in Fig. 4.
There was a high proportion of patients able to complete the 10 min walking test at baseline, 38 (64%), increasing to 43 (73%) after one year. There was no significant improvement in ABI at rest or after exercise. Of the 59 patients, 14 completed 18 weeks of supervised exercise treatment with a physical therapist. There were no significant differences between patients with SET compared to BMT alone at baseline or follow up.
Invasive treatment group
Among the 136 patients with QoL follow-up data after one year, 77 patients had been treated with endovascular or surgical procedures (IC/CLI: 66/11) in addition to BMT. Ten patients received both endovascular treatment (PTA/stent) and surgical treatment (by-pass/thrombendarterectomy), 54 patients endovascular treatment and 13 patients surgical treatment. In the group with CLI seven patients received endovascular treatment and four surgical treatments.
There was significant improvement in self-reported physical health status and disease-specific QoL, as shown in Table 2. The mean change in SF-36 subscale score was largest for the physical domains (PF-physical functioning, RP-Physical role and BP –Bodily pain), but also significant for the mental domains (VT-Vitality, SF –Social functioning and RE –Emotional role), as shown in Fig. 2. Figure 3 show mean score of VQ-6 at baseline and after treatment. Change in VQ-6 summary score ranged from − 4 to 16. Four patients (5%) had reduced summary score by 2 or more scale points, 16 patients (21%) had unchanged score (− 1 to 1). Some 56 patients (73%) had increased score by 2 or more scale points, and 43 (56%) had increased their summary score by 4 points or more, as shown in Fig. 4. In addition, there was significant improvement in ABI at rest and after exercise, and in walking capacity. At baseline 24 patients (31%) completed the 10 min walking test, increasing to 46 (60%) after one year.
Discussion
VascuQoL-6 was developed especially for clinical use and for use in vascular registries, where self-reported end points are increasingly important to evaluate outcome. Traditionally, quality of care was monitored in vascular registries by surveillance of adverse events and patency of the vascular reconstruction, but did not include whether life was improved for the patient. A validated instrument used to measure patient-reported outcome allows aggregation of data on a group level, and can be used to picture the treatment’s success in lessening symptoms. In clinical use, in the individual patient, the instrument can be used to evaluate key symptoms and how the patient perceives the impact on daily life.
Improvement or deterioration as shown by VQ-6 must, nevertheless, be interpreted with care. This study shows that both treatment groups improve their disease specific QoL as well as their health status after one year. Expected improvement from conservative treatment must thus be taken into account when interpreting outcome after invasive treatment, as not all improvement can be attributed to the invasive procedure.
Since this study was conducted, the validity and test retest reliability of VQ-6 have been tested in a Swedish population of mainly CLI (70%) [19], and the validity in a Brazilian PAD population with intermittent claudication [20]. Experience with the instrument are emerging also from the national vascular registry of Sweden, Swedvasc [21]. VascoQoL-6 has recently been introduced in NORKAR, the national Norwegian vascular registry.
The two groups of conservatively treated and invasively patients in our study are not directly comparable, as there was a clinically driven indication for choice of treatment, and the invasively treated patients thus had a significantly lower level of function and more advanced disease. Many of the conservatively treated patients did not improve their walking distance due to this selection bias, as their baseline values were close to the tests maximum of 416 m. This selection bias probably also influences the results from SET versus conservative treatment alone, as this study fails to demonstrate the benefit of SET shown in other studies [22]. Compared to arterial pressures and ABI, VQ-6 can detect improvement also in the absence of revascularization. As expected, ABI did not improve in the conservative treatment group, as increased blood flow and reduced symptoms are a result of development of collaterals, with persistent stenosis or occlusion of the artery.
A population-based study from the Swedish national vascular registry, Swedvasc, has indicated 1.7–2.2 scale steps as a minimally important difference (MID), and 3.5–4.5 scale steps as a substantial clinical benefit [7]. MID was estimated using two different methods in the validation study [4]. One method (0.5 SD) gave a value of 1.725 scale points, the other (95%CI) 0.82 for improvement and − 1.38 for deterioration [23, 24]. To use the self-reported health status, SF-36 item 2, after one year to estimate MID will probably be wrong, as the recall bias will be too large. But, the improvement in VQ-6 summary score for the “unchanged” group (2.3) supports that the earlier proposal of two points of change as indicative and four points as a certain change [4].
Self-reported health status based on SF-36 will include comorbidity and reduced QoL from other conditions than the lower extremity arterial disease. Nevertheless, the correlation between SF-36 and VQ-6, indicates that for this patient population, the morbidity from the arterial insufficiency is the main cause of change in self-reported health status.
The qualitative analysis in the Swedish study, published after the validation study, show item four to be vulnerable for emotional status, and the term “concern” was evaluated to be rather weak, the authors suggest “anxious” and “worried” as stronger terms [19]. This can influence the interpretation of the results in our study, as confusion about one item may add or subtract as much as three points to the VQ-6 summary score. In item one, the patients report some confusion regarding the content of the term “activities” [19]. This term was broadened in the Norwegian translation to “activities and daily activities of living” after the cognitive evaluation by patients and health professionals [4].
The number of patients lost to follow up at one year reflects both the increased mortality and morbidity associated with this disease, also among patients with presumptive stable disease [1, 25], as well as the advanced age of the patients. Only half of the original included patients with the most advanced form of the disease, critical limb ischemia (CLI), completed the trial. This means that the results presented here probably are most relevant in interpreting outcome after treatment for IC. Further studies are warranted and future use of VQ-6 in randomized trials would improve the basis for clinical interpretation.
Conclusions
Treatment for symptomatic PAD, both invasive and conservative, improves self-reported health status and disease specific QoL after one year. The natural history and development of the disease and the improvement from conservative treatment alone must be taken into account while interpreting patient-reported outcome in vascular registries.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABI:
-
ankle-brachial index
- BMT:
-
best medical treatment
- CLI:
-
critical limb ischemia
- IC:
-
intermittent claudication
- ICD:
-
intermittent claudication distance
- MID:
-
minimally important difference
- MWD:
-
maximum walking distance
- PAD:
-
peripheral arterial disease
- PROMS:
-
patient reports outcome measures
- QoL:
-
quality of life
- SET:
-
supervised exercise therapy
- SF-36:
-
Short Form-36, subscales (PF physical functioning, RP physical role, BP bodily pain, GH general health, VT vitality, SF social functioning, RE emotional role, MH mental health) and component summary scoring (PCS physical component score, MCS –mental component score)
- VQ-6:
-
VascuQoL-6 --Vascular Quality of Life questionnaire, short version
References
Aboyans V, Ricco JB, MEL B, Bjorck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39:763–816.
Morgan MB, Crayford T, Murrin B, Fraser SC. Developing the vascular quality of life questionnaire: a new disease-specific quality of life measure for use in lower limb ischemia. J Vasc Surg. 2001;33:679–87.
Nordanstig J, Wann-Hansson C, Karlsson J, Lundstrom M, Pettersson M, Morgan MB. Vascular Quality of Life Questionnaire-6 facilitates health-related quality of life assessment in peripheral arterial disease. J Vasc Surg. 2014;59(3):700-7. (Epub 2013 Dec 15).
Larsen ASF, Reiersen AT, Jacobsen MB, Klow NE, Nordanstig J, Morgan M, Wesche J. Validation of the vascular quality of life questionnaire - 6 for clinical use in patients with lower limb peripheral arterial disease. Health Qual Life Outcomes. 2017;15:184.
Nordanstig J, Taft C, Hensater M, Perlander A, Osterberg K, Jivegard L. Improved quality of life after one year with an invasive versus a noninvasive treatment strategy in claudicants: one-year results of the Invasive Revascularization or Not in Intermittent Claudication (IRONIC) trial. Circulation. 2014;130:939–47.
Fontaine R, Kim M, Kieny R. Surgical treatment of peripheral circulation disorders. Helv Chir Acta. 1954;21:499–533.
Nordanstig J, Pettersson M, Morgan M, Falkenberg M, Kumlien C. Assessment of minimum important difference and substantial clinical benefit with the vascular quality of life questionnaire-6 when evaluating revascularisation procedures in peripheral arterial disease. Eur J Vasc Endovasc Surg. 2017;54:340–7.
de Vries M, Ouwendijk R, Kessels AG, de Haan MW, Flobbe K, Hunink MG, van Engelshoven JM, Nelemans PJ. Comparison of generic and disease-specific questionnaires for the assessment of quality of life in patients with peripheral arterial disease. J Vasc Surg. 2005;41:261–8.
Mehta T, Venkata Subramaniam A, Chetter I, McCollum P. Assessing the validity and responsiveness of disease-specific quality of life instruments in intermittent claudication. Eur J Vasc Endovasc Surg. 2006;31:46–52.
Nordanstig J, Karlsson J, Pettersson M, Wann-Hansson C. Psychometric properties of the disease-specific health-related quality of life instrument VascuQoL in a Swedish setting. Health Qual Life Outcomes. 2012;10:45–7525–7510-7545.
Frans FA, van Wijngaarden SE, Met R, Koelemay MJ. Validation of the Dutch version of the VascuQol questionnaire and the Amsterdam linear disability score in patients with intermittent claudication. Qual Life Res. 2012;21:1487–93.
Nylaende M, Abdelnoor M, Stranden E, Morken B, Sandbaek G, Risum O, Jorgensen JJ, Lindahl AK, Arnesen H, Seljeflot I, Kroese AJ. The Oslo balloon angioplasty versus conservative treatment study (OBACT)--the 2-years results of a single Centre, prospective, randomised study in patients with intermittent claudication. Eur J Vasc Endovasc Surg. 2007;33:3–12.
Forbes JF, Adam DJ, Bell J, Fowkes FG, Gillespie I, Raab GM, Ruckley CV, Bradbury AW, Participants B. Bypass versus angioplasty in severe ischaemia of the leg (BASIL) trial: health-related quality of life outcomes, resource utilization, and cost-effectiveness analysis. J Vasc Surg. 2010;51:43S–51S.
Frans FA, Bipat S, Reekers JA, Legemate DA, Koelemay MJ, Collaborators SS. SUPERvised exercise therapy or immediate PTA for intermittent claudication in patients with an iliac artery obstruction--a multicentre randomised controlled trial; SUPER study design and rationale. Eur J Vasc Endovasc Surg. 2012;43:466–71.
Mazari FA, Carradice D, Rahman MN, Khan JA, Mockford K, Mehta T, McCollum PT, Chetter IC. An analysis of relationship between quality of life indices and clinical improvement following intervention in patients with intermittent claudication due to femoropopliteal disease. J Vasc Surg. 2010;52:77–84.
Ware JE, Kosinski M, Gandek B: SF-36 health survey : manual & interpretation guide. [2nd ed.] edn: Health Assessment Lab; 2000.
Ware JE Jr, Gandek B, Kosinski M, Aaronson NK, Apolone G, Brazier J, Bullinger M, Kaasa S, Leplege A, Prieto L, et al. The equivalence of SF-36 summary health scores estimated using standard and country-specific algorithms in 10 countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol. 1998;51:1167–70.
Loge JH, Kaasa S. Short form 36 (SF-36) health survey: normative data from the general Norwegian population. Scand J Soc Med. 1998;26:250–8.
Kumlien C, Nordanstig J, Lundstrom M, Pettersson M. Validity and test retest reliability of the vascular quality of life Questionnaire-6: a short form of a disease-specific health-related quality of life instrument for patients with peripheral arterial disease. Health Qual Life Outcomes. 2017;15:187.
de Almeida CM, Andrade-Lima A, Mesquita de Oliveira PL, Domiciano RM, Ribeiro Domingues WJ, Wolosker N, Puench-Leao P, Ritti-Dias RM, Cucato GG. Translation and validation of the Brazilian-Portuguese short version of vascular quality of life questionnaire in peripheral artery disease patients with intermittent claudication symptoms. Ann Vasc Surg. 2018;51:48–54.e41.
Swedvasc - Vascular Registry in Sweden [http://www.ucr.uu.se/swedvasc/].
Lane R, Ellis B, Watson L, Leng GC. Exercise for intermittent claudication. Cochrane Database Syst Rev. 2014;7:Cd000990.
Norman GR, Sloan JA, Wyrwich KW. The truly remarkable universality of half a standard deviation: confirmation through another look. Expert Rev Pharmacoecon Outcomes Res. 2004;4:581–5.
Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61:102–9.
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, Group TIW. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45(Suppl S):S5–67.
Acknowledgements
The authors would like to thank Anne Rigmor Holten for her contribution with the data collection.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ASL: Study design, Translation of questionnaire, Data collection, Data analysis, Writing. ATR: Study design, Data collection, Writing. IHN: Study design, Data collection, Writing. JW: Study design, Data collection, Data analysis, Writing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Regional Committee for Medical and Health Research Ethics approved the study (reference number 2014/221). License to use SF-36v1 were given from Optuminsight Life Sciences, Inc. (QM020601). Permission to translate and use VQ-6 was given by the original developers: Mark Morgan, Mark.Morgan@bopdhb.govt.nz (copyright) and Joakim Nordanstig, joakim.nordanstig@vgregion.se.
All patients provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Larsen, A.S.F., Reiersen, A.T., Nådland, I.H. et al. Self-reported health status and disease-specific quality of life one year after treatment for peripheral arterial disease in clinical practice. Health Qual Life Outcomes 18, 235 (2020). https://doi.org/10.1186/s12955-020-01477-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-020-01477-y