Abstract
Background
Left ventricular (LV) myocardial work index (WI) and work efficiency (WE) have become the latest indicators for assessing LV function. Reference ranges for normal LV segmental WI and WE have not been established.
Methods
Four hundred eleven healthy Asian subjects (47% men, median age: 35 years) were enrolled prospectively. WI and WE were analysed using the LV pressure–strain loop (LVPSL) with specific software.
Results
WI and WE differed significantly between segments as well as between walls and levels of the left ventricle. The anteroseptal basal segment had the lowest WI and WE (1440 mmHg ± 324 and 92% [88–96], respectively) among the eighteen segments. Significant WI and WE differences were found between sexes and age groups. No correlation was observed between age groups and the average WI of any wall or level in men, while the average WI of several different walls and levels in women showed significant differences between age groups. The average WI of most walls and levels increased with age in women. No correlation was found between age groups and the average WE of any wall or level in either men or women.
Conclusions
This study establishes the normal reference values of WI and WE of eighteen segments for clinical work and clinical experiments. There were significant differences in WI and WE between segments, levels, and walls of the normal left ventricle. Sex should be considered when analysing WI and WE. Age should be considered when analysing WI in women.
Graphical Abstract

Similar content being viewed by others
Background
Noninvasive left ventricular (LV) myocardial work (LVMW) is a novel and reliable indicator for assessing LV systolic function and has been used in several experimental and clinical works [1,2,3,4,5,6,7]. Noninvasive LVMW is obtained by integrating the LV longitudinal strain (LS), mitral and aortic valvular events, and brachial artery pressures using specific software. Normal reference values of global WI and global WE were analysed previously; however, normal reference values of different segmental WI and WE have not been studied. A previous study confirmed that there are significant differences in the LS of different LV segments in a healthy population [8]. Noninvasive myocardial work is derived based on LS; theoretically, there could be differences in the myocardial work of each segment of the left ventricle in healthy subjects.
The study aimed to 1) establish normal reference values for WI and WE of different segments in a healthy Asian population; 2) explore the differences in WI and WE of different segments; and 3) explore the implications of sex and age on WI and WE.
Methods
Population
A total of 452 healthy Asian subjects (age range, 18–65 years) were prospectively recruited from Xiamen Cardiovascular Hospital of Xiamen University between April 2021 and July 2021. The recruited population included hospital staff, people who came to this hospital for medical check-ups and their families, and people who came here for training or visits. The inclusion criteria of this study were as follows: age ≥ 18 years, body mass index < 30 kg/m2, normal physical examination results, normal electrocardiogram results, normal two-dimensional echocardiography (2DE) results, and absence of cardiovascular or respiratory diseases. The Institutional Ethics Committee approved the protocol, and all subjects provided informed consent.
Echocardiographic data acquisition
2DE and four-dimensional echocardiography (4DE) LV images were performed with a Vivid E95 system (GE Vingmed Ultrasound, Horten, Norway) with an M5Sc probe and a 4Vc probe, respectively. All datasets were acquired using electrocardiogram gating over three to five cardiac cycles following the protocols [9, 10]. Data were stored digitally for offline analysis.
Echocardiographic measurements
Standard measurements were performed using software (EchoPAC V.204, GE) in accordance with the guidelines [10].
Quantitative parameters of the left ventricle and left atrium were analysed using 4DE images by the 4D Auto LVQ software package and 4D Auto LAQ software package, respectively; LV end-diastolic volume, LV end-systolic volume, LV ejection fraction, and maximum and minimum volumes of the left atrium were automatically obtained. The transmitral E- and A-wave velocities were obtained by pulse-wave Doppler from the apical four-chamber view. The early diastolic velocities (e’) were measured by pulse-wave tissue Doppler from the apical four-chamber view. LV LS was acquired using three standard LV apical views with a frame rate ≥ 60 frames/s.
LVMW was measured by an LV pressure–strain loop (LVPSL). The mitral and aortic valve event timings were determined by visualization of the apical three-chamber views. LVPSL was generated by integrating the LV LS, valve event timings, and blood pressure readings using the software. The validation of LVMW was performed in several studies [1, 11, 12].
Four LVMW indices were obtained by LVPSL:
-
(i)
Work index (WI): the LVMW derived from the area of LVPSL.
-
(ii)
Constructive work (CW): positive work during shortening in systole and work during lengthening during isovolumic relaxation (IVR).
-
(iii)
Wasted work (WW): negative work during lengthening in systole and work during shortening during IVR.
-
(iv)
Work efficiency (WE): CW/(CW + WW).
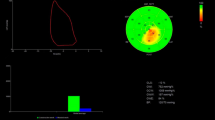
WI and WE were calculated for each LV segment in the software (according to the 18-segment model) [13] (Fig. 1).
A Noninvasive left ventricular pressure–strain loop diagram of a normal subject. The red and green loop areas represent the average global myocardial work index and the represented myocardial work index of the posterior apical segment, respectively. B 18-segment bull's-eye expression of myocardial work index. C Bar graph representing constructive work and wasted work. D 18-segment bull's-eye expression of myocardial work efficiency
Statistical analysis
All statistical analyses were performed using SPSS version 26 (SPSS Inc., IBM Corp). P < 0.05 was considered significant. All data normality was tested by the Kolmogorov–Smirnov test. Data are expressed as the mean ± standard deviation (SD) or median (interquartile range) as appropriate. The 95% confidence interval for WI was calculated as the mean ± 1.96 SD. The lowest (2.5th percentile) expected values for WE were computed using a bootstrap of 1000 samples.
Unpaired t tests or one-way ANOVA were used to compare normally distributed data. The Mann–Whitney U test or Kruskal–Wallis test was used to compare nonnormally distributed data. Correlations between variables were assessed using Spearman correlations.
The intra- and inter-observer variabilities of WI and WE were tested in twenty random individuals using the intraclass correlation coefficients and Bland–Altman analysis. The intra-observer analysis was performed after a 2-week interval. The inter-observer analysis was performed by a second independent blinded observer.
Results
Clinical and echocardiographic characteristics
Forty-one individuals were excluded because of poor image qualities of 2DE or 4DE images. Thus, the feasibility of LVMW measurement was 90.9% in this study. Table 1 summarizes the demographic and echocardiographic data of the enrolled population. LV global LS (LV GLS), LV global WI, LV global CW, and LV global WE were higher in women than in men (P < 0.001), while LV global WW was lower in women than in men (P = 0.005).
Functional nonuniformity
Table 2 and Table 3 summarize the WI and WE of different segments, levels, and walls of the population. Figure 2 displays the mean values of WI and the median values of WE for the 18 segments. Functional nonuniformity was found for all WIs and WEs in the normal left ventricle. WI and WE differed significantly between different segments, as well as different walls and levels of the left ventricle.
A 18-segment bull's-eye diagram shows the functional nonuniformity of the myocardial work index in the normal left ventricle. The values in the different segments are mean values. B 18-segment bull's-eye diagram shows the functional nonuniformity of myocardial work efficiency in the normal left ventricle. The values in the different segments are median values
Normal reference values
The values of WI and WE are summarized in Table 4 and Table 5.
Except for the anteroseptal apical WI, inferior apical WI, and posterior apical WI, all WIs of different segments were lower in men than in women. Similarly, the average WI was significantly lower in men than in women between different levels as well as different walls.
WE was significantly different between sexes in some LV segments. Except for the average values of the inferior and anterior walls of WE, all average values of walls and levels of WE were higher in men than in women.
Sex and age differences
Table 6, Supplement Fig. 1, and Supplement Fig. 2 show the sex and age differences in WI. Except for the septal middle WI increasing with age (R2 = 0.03, P = 0.017) and the inferior basal WI decreasing with age (R2 = 0.05, P = 0.001), there was no significant correlation between age and WI of the eighteen segments or the average WI of the varying walls and levels in men. However, eight of the eighteen segments’ WI increased with age in women. Moreover, except for the average WI of the septal and posterior walls, which showed no correlation with age, all average WIs of different walls and levels increased with age in women. There was no correlation between age groups and average WI of the different walls or levels in men; nevertheless, most of the average WI of different walls and levels in women showed significant differences between age groups. In Supplement Fig. 1 and Supplement Fig. 2, the sex differences in the WI of some segments, levels, and walls in the different age subgroups are shown.
Table 7, Supplement Fig. 3, and Supplement Fig. 4 show the sex and age differences in WE. Except for the posterior middle WE and posterior apical WE decreasing with age (R2 = 0.02, P = 0.036 and R2 = 0.02, P = 0.034, respectively) in men and the posterior basal WE increasing with age (R2 = 0.05, P = 0.001) and the posterior apical WE decreasing with age (R2 = 0.07, P < 0.001) in women, there was no correlation between age and WE of the different segments or the average WE of the varying walls and levels in either men or women. There was no correlation between age groups and average WE of the varying walls and levels in either men or women. In Supplement Fig. 3 and Supplement Fig. 4, WE for only a few of the different segments, levels, and walls in the different age subgroups showed sex differences.
Repeatability and reproducibility
Intra- and inter-observer variabilities for WI and WE of the eighteen segments are summarized in Supplement Table 1, Supplement Fig. 5, Supplement Fig. 6, Supplement Fig. 7, and Supplement Fig. 8. Good intra-observer and inter-observer reproducibility were found.
Discussion
This study is the first to use echocardiography to analyse 18-segment myocardial WI and WE of noninvasive LVMW. The LVMW, derived from the LVPSL, was first derived by Russell et al. [1] as a novel method to assess LV function. The study showed that LV myocardial glucose metabolism (calculated by positron emission tomography) has a strong correlation with noninvasive LVMW. Recently, Edwards et al. [11] revealed that in patients with normal wall motion and ejection fraction, noninvasive LVMW was more sensitive than global LS to detect significant coronary artery disease. These studies revealed that afterload-enrolled noninvasive LVMW could be a reliable method to evaluate LV function.
Multiple studies have already concluded normal LVMW by echocardiography; nevertheless, they only evaluated global myocardial work [14,15,16]. In our study, the LV GLS was higher in women than in men, which parallels the results from other studies [8, 17]. The LV global WI and LV global CW were higher in women than in men; a possible reason could be that the LV global WI and the LV global CW are correlated with the LV GLS [18]. The LV global WI was significantly lower in the present study than it was in a previous study [16], racial differences being a possible reason for the discrepancy (1749 mmHg ± 231 vs. 1896 mmHg ± 308, P < 0.001), though the LV global WE was similar in the two studies.
Our study establishes normal reference values for LV 18-segment WI and WE in a healthy Asian population. The data demonstrated that there are differences in WI and WE between different segments, sexes and age groups. The study further strengthens the necessity for the segment-, sex-, and age-specific normal ranges of WI and WE.
Functional nonuniformity
Functional heterogeneity, as a well-known feature of the left ventricle in the normal population, may influence LV segmental function [19,20,21,22]. In this study, as we expected, an important observation in evaluating the entire population was the variability of WI and WE for different segments, levels, and walls of the left ventricle.
Notably, the anteroseptal basal segment had the lowest WI and WE among all segments. Based on our data, the basal and middle levels demonstrated lower median WI values than the apical level in all walls. The reason could be that WI is significantly correlated with LV GLS, and the strain of apical levels is greater than the strain of middle and basal levels [23]. WI was lower in anterior walls than in the other walls at all levels, which may be the result of the strain of anterior walls being lower than that of the other walls in the normal population [24]. WE showed a lower median value in the basal wall than in the other walls at all levels. Moreover, all 18-segment median values of WI were greater than 95%, except for the anteroseptal basal segment.
Sex and age differences
Our data showed that most WI values were independent of sex (Table 4). In the segments with significant differences, the WI values of males were higher than those of females. The average WI values of different levels and walls were all higher in men than in women. This may be related to the result that LV GLS is higher in women than in men. Moreover, when considering sex and age, all the average WIs of different walls and levels showed no correlation with age in men (Table 6). However, most of the average WI of different walls and levels increased with age in women along with systolic blood pressure. The results above are consistent with the study by Manganaro et al. [16], who demonstrated that increasing afterload may lead to higher WI. Therefore, the ageing-related increase in systolic blood pressure may be the reason for the increase in WI in some segments in women.
There were some differences in WE between the sexes (Table 5). The average WE of all levels and most walls were significantly different in men and women. When both sex and age were considered, none of the average WE values of the different walls or levels showed any correlation with age in women or men (Table 7).
Clinical implications
To our knowledge, LVMW has been studied in the fields of heart failure, hypertension, cardiac resynchronization therapy, diabetes mellitus, cardiomyopathy (nonobstructive hypertrophic cardiomyopathy [HCM], dilated cardiomyopathy [DCM], cardiac amyloidosis [CA]), etc. [2,3,4,5,6,7]. As a noninvasive and novel technique, LVMW could be a reliable method to measure different LV segmental functions in clinical and experimental research.
Coronary artery disease (CAD) is a leading disease worldwide [25]. Boe et al. [26] previously demonstrated that the presence of ≥ 4 adjacent segments with systolic dysfunction (based on WI measurements) showed better sensitivity and specificity in identifying non-ST-segment elevation-acute coronary syndrome than conventional echocardiography parameters. In another study [11], Edwards et al. found that relative segmental WI decreased in the presence of segmental perfusion defects.
HCM is an inherited cardiovascular disease characterized by the presence of thick LV walls [27]. Hiemstra et al. [4] evaluated segmental differences in myocardial work in patients with nonobstructive HCM, and WE for some segments was significantly lower in patients with nonobstructive HCM than in control subjects.
DCM is a common cardiac disease with LV systolic dysfunction caused by many factors [28]. Recently, Schrub et al. [29] analysed the relationship between WE and exercise tolerance in patients with DCM. They demonstrated that septal WE was the best predictor of exercise performance in patients with DCM.
CA has a high incidence rate in elderly individuals [30, 31]. Clemmensen et al. [32] demonstrated that WI in apical, middle, and basal myocardial levels were all lower in patients with CA than in controls. WI gradually decreased from the apical level to the basal level in patients with CA. Moreover, another study [5] by Clemmensen et al. demonstrated that the apical-to-basal WI ratio could predict major adverse cardiac events and all-cause mortality in patients with CA.
Overall, our data showed good agreement and reproducibility in assessing WI and WE of different segments, which suggests the possibility that these normal values could be used as a reference for a variety of diseases in clinical and research practice, such as myocardial infarction, nonobstructive HCM, DCM, and CA.
Limitations
The collection and quantification of the LVMW dataset from a single-provider platform may limit the application of the reference values to data measured by other provider platforms. In addition, the software only provides the values of WI and WE of each segment but does not provide the values of CW and WW of each segment, so the reference values for each segment of CW and WW are not available. Additionally, all enrolled individuals were asymptomatic on routine examinations, but the possibility of subclinical cardiovascular diseases, especially in elderly individuals, cannot be ruled out. Furthermore, whether our results apply to non-Asian populations remains unknown.
Conclusions
To date, this study is the first to use echocardiography to establish reference values for the segment-, sex-, and age-specific normal ranges of WI and WE in a large normal population cohort. There are differences in WI and WE between different segments, levels, and walls of the normal left ventricle. Sex should be considered when attempting to identify WI and WE. Age should be considered when attempting to identify WI in women. The data in this study could enhance the value of echocardiography in LV function evaluation, disease diagnosis risk stratification, and prognosis.
Availability of data and materials
The data and material underlying this article will be shared on reasonable request to the corresponding authors.
Abbreviations
- LV:
-
Left ventricular
- WI:
-
Work index
- WE:
-
Work efficiency
- LVPSL:
-
LV pressure-strain loop
- LVMW:
-
LV myocardial work
- LS:
-
Longitudinal strain
- 2DE:
-
Two-dimensional echocardiography
- 4DE:
-
Four-dimensional echocardiography
- CW:
-
Constructive work
- IVR:
-
Isovolumic relaxation
- WW:
-
Wasted work
- SD:
-
Standard deviation
- LV GLS:
-
LV global LS
- HCM:
-
Hypertrophic cardiomyopathy
- DCM:
-
Dilated cardiomyopathy
- CA:
-
Cardiac amyloidosis
- CAD:
-
Coronary artery disease
- ACO:
-
Acute coronary artery occlusion
References
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Remme EW, Haugaa KH, Opdahl A, Fjeld JG, Gjesdal O, et al. A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J. 2012;33(6):724–33.
Vecera J, Penicka M, Eriksen M, Russell K, Bartunek J, Vanderheyden M, Smiseth OA. Wasted septal work in left ventricular dyssynchrony: a novel principle to predict response to cardiac resynchronization therapy. Eur Heart J Cardiovasc Imaging. 2016;17(6):624–32.
Chan J, Edwards NFA, Khandheria BK, Shiino K, Sabapathy S, Anderson B, Chamberlain R, Scalia GM. A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2019;20(1):31–9.
Hiemstra YL, van der Bijl P, El Mahdiui M, Bax JJ, Delgado V, Marsan NA. Myocardial Work in Nonobstructive Hypertrophic Cardiomyopathy: Implications for Outcome. J Am Soc Echocardiogr. 2020;33(10):1201–8.
Clemmensen TS, Eiskjaer H, Ladefoged B, Mikkelsen F, Sorensen J, Granstam SO, Rosengren S, Flachskampf FA, Poulsen SH. Prognostic implications of left ventricular myocardial work indices in cardiac amyloidosis. Eur Heart J Cardiovasc Imaging. 2021;22(6):695–704.
Huang D, Cui C, Zheng Q, Li Y, Liu Y, Hu Y, Wang Y, Liu R, Liu L. Quantitative Analysis of Myocardial Work by Non-invasive Left Ventricular Pressure-Strain Loop in Patients With Type 2 Diabetes Mellitus. Front Cardiovasc Med. 2021;8: 733339.
Wang CL, Chan YH, Wu VC, Lee HF, Hsiao FC, Chu PH. Incremental prognostic value of global myocardial work over ejection fraction and global longitudinal strain in patients with heart failure and reduced ejection fraction. Eur Heart J Cardiovasc Imaging. 2021;22(3):348–56.
Kleijn SA, Pandian NG, Thomas JD, Perez de Isla L, Kamp O, Zuber M, Nihoyannopoulos P, Forster T, Nesser HJ, Geibel A, et al. Normal reference values of left ventricular strain using three-dimensional speckle tracking echocardiography: results from a multicentre study. Eur Heart J Cardiovasc Imaging 2015, 16(4):410–416.
Cosyns B, Garbi M, Separovic J, Pasquet A, Lancellotti P, Education Committee of the European Association of Cardiovascular Imaging A. Update of the echocardiography core syllabus of the European Association of Cardiovascular Imaging (EACVI). Eur Heart J Cardiovasc Imaging 2013, 14(9):837–839.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015, 28(1):1–39 e14.
Edwards NFA, Scalia GM, Shiino K, Sabapathy S, Anderson B, Chamberlain R, Khandheria BK, Chan J. Global Myocardial Work Is Superior to Global Longitudinal Strain to Predict Significant Coronary Artery Disease in Patients With Normal Left Ventricular Function and Wall Motion. J Am Soc Echocardiogr. 2019;32(8):947–57.
Chen KW, Hsieh WT, Huang CY, Huang CC, Liang HY, Wang GJ. Estimated left ventricular pressure-myocardial strain loop as an index of cardiac work predicts all-cause mortality in patients receiving regular hemodialysis. J Diabetes Complications. 2021;35(5): 107890.
Voigt JU, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R, Pedri S, Ito Y, Abe Y, Metz S, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. J Am Soc Echocardiogr. 2015;28(2):183–93.
Galli E, John-Matthwes B, Rousseau C, Schnell F, Leclercq C, Donal E. Echocardiographic reference ranges for myocardial work in healthy subjects: A preliminary study. Echocardiography. 2019;36(10):1814–24.
Tretter JT, Pradhan S, Truong VT, Mullikin A, Mazur W, Hill GD, Redington AN, Taylor MD. Non-invasive left ventricular myocardial work indices in healthy adolescents at rest. Int J Cardiovasc Imaging. 2021;37(8):2429–38.
Manganaro R, Marchetta S, Dulgheru R, Ilardi F, Sugimoto T, Robinet S, Cimino S, Go YY, Bernard A, Kacharava G, et al. Echocardiographic reference ranges for normal non-invasive myocardial work indices: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2019;20(5):582–90.
Sugimoto T, Dulgheru R, Bernard A, Ilardi F, Contu L, Addetia K, Caballero L, Akhaladze N, Athanassopoulos GD, Barone D, et al. Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2017;18(8):833–40.
Manganaro R, Marchetta S, Dulgheru R, Sugimoto T, Tsugu T, Ilardi F, Cicenia M, Ancion A, Postolache A, Martinez C, et al. Correlation between non-invasive myocardial work indices and main parameters of systolic and diastolic function: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2020;21(5):533–41.
Maffessanti F, Nesser HJ, Weinert L, Steringer-Mascherbauer R, Niel J, Gorissen W, Sugeng L, Lang RM, Mor-Avi V. Quantitative evaluation of regional left ventricular function using three-dimensional speckle tracking echocardiography in patients with and without heart disease. Am J Cardiol. 2009;104(12):1755–62.
Marwick TH, Leano RL, Brown J, Sun JP, Hoffmann R, Lysyansky P, Becker M, Thomas JD. Myocardial strain measurement with 2-dimensional speckle-tracking echocardiography: definition of normal range. JACC Cardiovasc Imaging. 2009;2(1):80–4.
Perez de Isla L, Balcones DV, Fernandez-Golfin C, Marcos-Alberca P, Almeria C, Rodrigo JL, Macaya C, Zamorano J. Three-dimensional-wall motion tracking: a new and faster tool for myocardial strain assessment: comparison with two-dimensional-wall motion tracking. J Am Soc Echocardiogr 2009, 22(4):325–330.
Kleijn SA, Aly MF, Terwee CB, van Rossum AC, Kamp O. Three-dimensional speckle tracking echocardiography for automatic assessment of global and regional left ventricular function based on area strain. J Am Soc Echocardiogr. 2011;24(3):314–21.
Tsugu T, Postolache A, Dulgheru R, Sugimoto T, Tridetti J, Nguyen Trung ML, Piette C, Moonen M, Manganaro R, Ilardi F, et al. Echocardiographic reference ranges for normal left ventricular layer-specific strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2020;21(8):896–905.
Chen Z, Li C, Li Y, Rao L, Zhang X, Long D, Li C. Layer-specific strain echocardiography may reflect regional myocardial impairment in patients with hypertrophic cardiomyopathy. Cardiovasc Ultrasound. 2021;19(1):15.
Khera AV, Kathiresan S. Genetics of coronary artery disease: discovery, biology and clinical translation. Nat Rev Genet. 2017;18(6):331–44.
Boe E, Russell K, Eek C, Eriksen M, Remme EW, Smiseth OA, Skulstad H. Non-invasive myocardial work index identifies acute coronary occlusion in patients with non-ST-segment elevation-acute coronary syndrome. Eur Heart J Cardiovasc Imaging. 2015;16(11):1247–55.
Maron BJ, Maron MS. Hypertrophic cardiomyopathy. Lancet. 2013;381(9862):242–55.
Weintraub RG, Semsarian C, Macdonald P. Dilated cardiomyopathy. Lancet. 2017;390(10092):400–14.
Schrub F, Schnell F, Donal E, Galli E. Myocardial work is a predictor of exercise tolerance in patients with dilated cardiomyopathy and left ventricular dyssynchrony. Int J Cardiovasc Imaging. 2020;36(1):45–53.
Cavalcante JL, Rijal S, Abdelkarim I, Althouse AD, Sharbaugh MS, Fridman Y, Soman P, Forman DE, Schindler JT, Gleason TG, et al. Cardiac amyloidosis is prevalent in older patients with aortic stenosis and carries worse prognosis. J Cardiovasc Magn Reson. 2017;19(1):98.
Bonderman D, Polzl G, Ablasser K, Agis H, Aschauer S, Auer-Grumbach M, Binder C, Dorler J, Duca F, Ebner C, et al. Diagnosis and treatment of cardiac amyloidosis: an interdisciplinary consensus statement. Wien Klin Wochenschr. 2020;132(23–24):742–61.
Clemmensen TS, Eiskjaer H, Mikkelsen F, Granstam SO, Flachskampf FA, Sorensen J, Poulsen SH. Left Ventricular Pressure-Strain-Derived Myocardial Work at Rest and during Exercise in Patients with Cardiac Amyloidosis. J Am Soc Echocardiogr. 2020;33(5):573–82.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Maolong Su conceived the study design, provided project oversight, and performed the final approval of the version to be submitted. Jian Wu conceived the study design, took ultrasound images, interpreted the data, and wrote the manuscript. Xinyi Huang, Kunhui Huang, Qiumei Gao, and Biqin Lin took ultrasound images and revised the article carefully. Yiruo Tang and Xu Chen provided the method for the study and substantively revised the article. Bo Jing and Xinyu Wang revised the article for significant intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by the Institutional Ethics Committee of Xiamen Cardiovascular Hospital of Xiamen University (No. 202226), and all subjects provided written informed consent before undergoing examinations.
Consent for publication
Consent for publication was obtained from all the participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplement Figure 1.
Individual values of left ventricular 18-segment myocardial work index according to sex and age categories. Horizontal lines represent median values or mean values, appropriately. *P value < 0.05 between sexes. #P value < 0.05 between age subgroups.
Additional file 2: Supplement Figure 2.
Individual values of the left ventricular 6-wall and 3-level average myocardial work index according to sex and age categories. Horizontal lines represent median values or mean values, appropriately. *P value < 0.05 between sexes. #P value < 0.05 between age subgroups.
Additional file 3: Supplement Figure 3.
Individual values of left ventricular 18-segment myocardial work efficiency according to sex and age categories. Horizontal lines represent median values. *P value < 0.05 between sexes. #P value < 0.05 between age subgroups.
Additional file 4: Supplement Figure 4.
Individual values of left ventricular 6-wall and 3-level average myocardial work efficiency according to sex and age categories. Horizontal lines represent median values. *P value < 0.05 between sexes. #P value < 0.05 between age subgroups.
Additional file 5: Supplement Figure 5.
The Bland–Altman analysis for assessing intra-observer variability of myocardial work index of eighteen segments.
Additional file 6: Supplement Figure 6.
The Bland–Altman analysis for assessing intra-observer variability of myocardial work efficiency of eighteen segments.
Additional file 7: Supplement Figure 7.
The Bland–Altman analysis for assessing inter-observer variability of myocardial work index of eighteen segments.
Additional file 8: Supplement Figure 8.
The Bland–Altman analysis for assessing inter-observer variability of myocardial work efficiency of eighteen segments.
Additional file 9: Supplement Table 1.
Intra- and inter-observer variabilities of myocardial WI and WE.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, J., Huang, X., Huang, K. et al. Echocardiographic reference ranges for noninvasive left ventricular 18-segment myocardial work index and work efficiency in a healthy Asian population. Cardiovasc Ultrasound 21, 2 (2023). https://doi.org/10.1186/s12947-023-00299-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12947-023-00299-4