Abstract
A high incidence of left ventricular diastolic dysfunction and increased risk of cardiovascular events have been reported in patients with diabetes mellitus. Sodium glucose cotransporter 2 (SGLT2) inhibitors selectively inhibit kidney glucose and sodium reabsorption, and cardiovascular benefits of SGLT2 inhibitors beyond other antidiabetic drugs have been reported in type 2 diabetes mellitus (T2DM) clinical trials. However, underlying mechanisms contributing to the improvement of cardiovascular outcomes have not been clearly identified. In this review, likely mechanisms of SGLT2 inhibitors contributing to a favorable cardiovascular outcomes are discussed based on experimental and clinical studies on cardiac function.
Similar content being viewed by others
Background
Diabetes mellitus is associated with increased risk of cardiovascular events including cardiovascular death and hospitalization from heart failure. Diabetic cardiomyopathy affects cardiac function as well as cardiac structure such as left ventricular (LV) hypertrophy and fibrosis, which are considered as major contributors of cardiovascular events [1,2,3]. Sodium glucose cotransporter 2 (SGLT2) inhibitors have newly emerged as an anti-hyperglycemic drug for type 2 diabetes mellitus (T2DM) by inhibiting glucose and sodium reabsorption in the kidney. In large clinical trials (EMPA-REG OUTCOME, CANVAS Program and DECLARE-TIMI 58), SGLT2 inhibitors have shown to improve long-term clinical outcome including all cause mortality, cardiovascular death and heart failure hospitalization in T2DM [4,5,6]. Meta-analysis also showed clinical benefit of SGLT2 inhibitors in reducing risk of myocardial infarction, stroke and cardiovascular death in patients with established atherosclerotic cardiovascular disease [7]. Moreover, SGLT2 inhibitors showed risk reduction of heart failure hospitalization in T2DM patients, suggesting that SGLT2 inhibitors play a key role in the improvement of cardiac function in diabetic cardiomyopathy [8]. More recently, DAPA-HF reported that dapagliflozin improved cardiovascular outcomes among patients with heart failure with reduced ejection fraction regardless of diabetic status, therefore SGLT2 inhibitors have been expected that its pharmacological action is beyond antidiabetic drug [9]. To elucidate the effect of SGLT2 inhibitors on cardiovascular event reduction, it is important to clarify the mechanisms contributing to the cardioprotective effect of SGLT2 inhibitors. Accordingly, we reviewed the effect of SGLT2 inhibitors on cardiac function in animal models and clinical studies, and discussed the underlying mechanisms contributing to cardioprotection.
Review methods
We searched English language literatures using PubMed. Search terms were “sodium glucose cotransporter 2”, “cardiac function” and “left ventricular”. In addition, term of “empagliflozin”, “canagliflozin” or “dapagliflozin” was searched in PubMed and the articles evaluating cardiac function were extracted. Article relevance was assessed by subject and study design.
Effect of SGLT2 inhibitors on cardiac function
In experimental diabetic cardiomyopathy models, SGLT2 inhibitors improved both cardiac systolic and diastolic function (Table 1). Moreover, LV pressure-volume loop analysis in vivo showed improvement of end-systolic and end-diastolic pressure volume relationships by SGLT2 inhibitors [10,11,12,13,14]. Pathological experimental studies showed that SGLT2 inhibitors attenuated LV fibrotic area [11, 12, 15,16,17]. These experimental data indicate that plasma volume reduction by SGLT2 inhibitors strongly contributed to the attenuation of pressure-overload-induced cardiac fibrosis and remodeling [18].
In models of myocardial ischemia, SGLT2 inhibitors not only suppressed exacerbation of systolic and diastolic cardiac dysfunction but also prevented LV remodeling and expansion of fibrosis area following ischemic myocardial injury [12, 13, 19,20,21]. These authors suggested that SGLT2 inhibitors reduced mitochondrial damage by stimulating mitochondrial biogenesis, which resulted in the normalization of myocardial uptake and oxidation of glucose and fatty acids. Furthermore, SGLT2 inhibitors increased circulating ketone levels and myocardial ketone utilization indicating enhancement of myocardial energetics [20,21,22]. Evidenced from these reports, SGLT2 inhibitors also exert cardioprotective effect exposed to ischemia.
Two experimental studies investigated cardiac function of SGLT2 inhibitor alone and combined therapy with SGLT2 inhibitor and DPP4 inhibitor. In a mice model, Ye et al. compared three groups; control, dapagliflozin alone and combined therapy with dapagliflozin and saxagliptin [15]. Both dapagliflozin alone and combined therapy groups showed a significant improvement of LV systolic function, LV end-diastolic and end-systolic volume compared to the control. Moreover, combined therapy group showed a larger improvement of LV end-diastolic and end-systolic volume compared to dapagliflozin alone group. Tanajak et al. compared cardiac protective effect of dapagliflozin vs. vildagliptin after ischemia-reperfusion injury in pre-diabetic rats, which showed that dapagliflozin had a greater efficacy than vildagliptin in improving LV dysfunction and infarct size [11]. Combined therapy with dapagliflozin and vildagliptin showed the greatest efficacy in attenuating LV dysfunction and infarct size. However, human study is needed to define the clinical significance of combined SGLT2 inhibitor and dipeptidyl peptidase 4 inhibitor therapy.
Several clinical studies have reported the effect of SGLT2 inhibitors on cardiac function in T2DM (Table 1). EMPA-REG OUTCOME trial retrospectively evaluated the effect of empagliflozin on cardiac function [23]. In this analysis, transthoracic echocardiogram was performed before and 3 months after initiation of empagliflozin in 10 patients with T2DM. This was a single arm and small number analysis, but showed that short-term empagliflozin treatment resulted in a significant improvement of diastolic function and reduction of LV mass index in T2DM patients with established cardiovascular disease. Matsutani et al. prospectively evaluated transthoracic echocardiogram at baseline and 3 months after additional treatment with canagliflozin in 37 T2DM patients and showed improvement of LV diastolic function and reduction of LV mass index [24]. Although brain natriuretic peptide level did not change between baseline and at 6 months of dapagliflozin treatment, Soga et al. showed improvement of diastolic function as well as reduction of LV mass index and left atrial volume index in 58 T2DM patients with previous history of heart failure [25]. These clinical reports indicate that SGLT2 inhibitors have a favorable effect on diastolic function and LV mass. However, these reports were single arm evaluation regarding the effect of SGLT2 inhibitor on cardiac function. Recently, we compared tofogliflozin and propensity-matched antidiabetic therapy not taking SGLT2 inhibitor, and found that tofogliflozin showed a significant improvement of systolic and diastolic function compared to the controls [26].
Cohen et al. investigated the effect of empagliflozin on cardiac functional and structural changes in patients with T2DM treated with standard glucose lowering therapy plus empagliflozin using cardiac magnetic resonance compared with control patients. As a results, LV end-diastolic volume reduced significantly after 6 months treatment of empagliflozin compared with control patients despite of no significant difference in LV mass [27]. Authors concluded that beneficial effect of SGLT2 inhibitor was due to functional improvement from reduction of plasma volume rather than structural remodeling.
Underlying mechanisms of SGLT2 inhibitor and cardiovascular outcomes
SGLT2 receptor is located in the proximal tubule of the kidney, where it mediates approximately 90% of renal glucose reabsorption by coupling with sodium reabsorption at 1:1 ratio [28]. Inhibition of SGLT2 receptor leads to increase of urine glucose and sodium excretion, but the increase in urine sodium excretion by SGLT2 inhibitors appears to be transient [29, 30]. This is probably caused by accelerated sodium reabsorption at the proximal tubule, henle loop and distal tubule against inhibition of sodium reabsorption at SGLT2 receptor (Fig. 1). In contrast, continuous urine glucose excretion is demonstrated with SGLT2 inhibitor treatment in many human and experimental studies [30,31,32,33,34,35,36]. Therefore, osmotic diuresis observed with SGLT2 inhibitor treatment is mainly caused by urine glucose excretion.
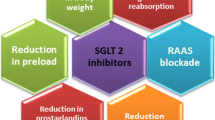
Effect of SGLT2 inhibitors on cardiac function and cardiovascular outcome. Osmotic diuresis mainly caused by urine glucose excretion leads to plasma volume reduction without activating renin angiotensin system and sympathetic nervous system. Plasma volume reduction leads to decreased cardiac workload resulting in the improvement of cardiac function and hence, favorable cardiovascular outcome. Blue box; functional and structural changes, Red box; clinical parameters, Green box; clinical outcome.tab
Experimental and clinical studies have shown no activation of renin angiotensin system by SGLT2 inhibitors [29, 37]. Moreover, Matsutani et al. showed that canagliflozin caused no exacerbation of autonomic function as assessed by baroreflex sensitivity and frequency domain analysis of heart rate variability, which suggest that canagliflozin improved LV diastolic function without activating sympathetic nervous system [24]. Blood pressure lowering effect of SGLT2 inhibitor also caused no compensatory increase in heart rate in EMPA-REG OUTCOME trial, indicating that there was no further sympathetic nervous system activation after SGLT2 inhibitor treatment [38, 39]. As evidenced from these studies, diuresis caused by urine glucose excretion results in continuous but mild intravascular fluid reduction without activating renin angiotensin system and sympathetic nervous system [30, 33, 37], because serum glucose has quite small effect on plasma osmolality compared to serum sodium. Therefore, urine glucose excretion, not accompanied by natriuresis, cause not only reduction of cardiac preload but also afterload without activating renin angiotensin system and sympathetic nervous system (Fig. 1).
Increase in hematocrit due to reduction in plasma volume was observed in patients treated with empagliflozin [29]. Moreover, increase of hematocrit after empagliflozin treatment was associated with more than 50% reduction in cardiovascular mortality [40, 41]. These data indicate that decreased circulatory volume by empagliflozin, especially reduction of LV filling pressure, is an important mechanism contributing to a favorable cardiovascular outcome. Thus, improvement of LV function by SGLT2 inhibitors prevented further cardiac morphologic changes and hence, result in favorable cardiovascular outcomes.
DAPA-HF, a large randomized clinical trial, investigated whether dapagliflozin improves long-term cardiovascular outcomes among patients with heart failure with reduced ejection fraction regardless of diabetic status [9]. Dapagliflozin significantly reduced cardiovascular death and heart failure events not only in T2DM patients but also in non-diabetic patients. This study indicates that underlying mechanisms of SGLT2 inhibitors for the improvement of cardiovascular outcomes is independent of glucose lowering effect. Further study using novel cardiac imaging modalities is needed to confirm the relationship between SGLT2inhibitors on cardiac function and a favorable cardiovascular outcome.
Conclusions
Cardioprotective effect of SGLT2 inhibitors is due to reduction of plasma volume from continuous urine glucose excretion without activating renin angiotensin system and sympathetic nervous system. Therefore, SGLT2 inhibitors have a favorable effect on cardiac function as well as cardiac structure and hence, improvement of cardiovascular outcome.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LV:
-
Left ventricular
- SGLT2:
-
Sodium glucose cotransporter 2
- T2DM:
-
Type 2 diabetes mellitus
References
Rydén L, Grant PJ, Anker SD, et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the task force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of diabetes (EASD). Eur Heart J. 2013;34(39):3035–87.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;62(16):e147–239.
González-Vílchez F, Ayuela J, Ares M, et al. Oxidative stress and fibrosis in incipient myocardial dysfunction in type 2 diabetic patients. Int J Cardiol. 2005;101:53–8.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–80.
Zelniker TA, Wiviott SD, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393(10166):31–9.
Tanaka H, Hirata K. Potential impact of SGLT2 inhibitors on left ventricular diastolic function in patients with diabetes mellitus. Heart Fail Rev. 2018;23(3):439–44.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. New Engl J Med. 2019. in press.
Hammoudi N, Jeong D, Singh R, et al. Empagliflozin improves left ventricular diastolic dysfunction in a genetic model of type 2 diabetes. Cardiovasc Drugs Ther. 2017;31(3):233–46.
Lee HC, Shiou YL, Jhuo SJ, et al. The sodium-glucose co-transporter 2 inhibitor empagliflozin attenuates cardiac fibrosis and improves ventricular hemodynamics in hypertensive heart failure rats. Cardiovasc Diabetol. 2019;18(1):45.
Tanajak P, Sa-Nguanmoo P, Sivasinprasasn S, et al. Cardioprotection of dapagliflozin and vildagliptin in rats with cardiac ischemia-reperfusion injury. J Endocrinol. 2018;236(2):69–84.
Sayour AA, Korkmaz-Icöz S, Loganathan S, et al. Acute canagliflozin treatment protects against in vivo myocardial ischemia-reperfusion injury in non-diabetic male rats and enhances endothelium-dependent vasorelaxation. J Transl Med. 2019;17(1):127.
Connelly KA, Zhang Y, Visram A, et al. Empagliflozin improves diastolic function in a nondiabetic rodent model of heart failure with preserved ejection fraction. JACC Basic Transl Sci. 2019;4(1):27–37.
Ye Y, Bajaj M, Yang HC, et al. SGLT-2 inhibition with dapagliflozin reduces the activation of the Nlrp3/ASC inflammasome and attenuates the development of diabetic cardiomyopathy in mice with type 2 diabetes. Further augmentation of the effects with saxagliptin, a DPP4 inhibitor. Cardiovasc Drugs Ther. 2017;31(2):119–32.
Li C, Zhang J, Xue M, et al. SGLT2 inhibition with empagliflozin attenuates myocardial oxidative stress and fibrosis in diabetic mice heart. Cardiovasc Diabetol. 2019;18(1):15.
Yang CC, Chen YT, Wallace CG, et al. Early administration of empagliflozin preserved heart function in cardiorenal syndrome in rat. Biomed Pharmacother. 2019;109:658–70.
Sakamoto M, Matsutani D, Kayama Y. Possibility of a new therapeutic strategy for left ventricular dysfunction in type 2 diabetes. J Clin Med Res. 2018;10(11):799–805.
Byrne NJ, Parajuli N, Levasseur JL, et al. Empagliflozin prevents worsening of cardiac function in an experimental model of pressure overload-induced heart failure. JACC Basic Transl Sci. 2017;2(4):347–54.
Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, et al. Empagliflozin ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J Am Coll Cardiol. 2019;73(15):1931–44.
Yurista SR, Silljé HHW, Oberdorf-Maass SU, et al. Sodium-glucose co-transporter 2 inhibition with empagliflozin improves cardiac function in non-diabetic rats with left ventricular dysfunction after myocardial infarction. Eur J Heart Fail. 2019;21(7):862–73.
Verma S, Rawat S, Ho KL, et al. Empagliflozin increases cardiac energy production in diabetes: novel translational insights into the heart failure benefits of SGLT2 inhibitors. JACC Basic Transl Sci. 2018;3(5):575–87.
Verma S, Garg A, Yan AT, et al. Effect of empagliflozin on left ventricular mass and diastolic function in individuals with diabetes: an important clue to the EMPA-REG OUTCOME trial? Diabetes Care. 2016;39(12):e212–3.
Matsutani D, Sakamoto M, Kayama Y, et al. Effect of canagliflozin on left ventricular diastolic function in patients with type 2 diabetes. Cardiovasc Diabetol. 2018;17(1):73.
Soga F, Tanaka H, Tatsumi K, et al. Impact of dapagliflozin on left ventricular diastolic function of patients with type 2 diabetic mellitus with chronic heart failure. Cardiovasc Diabetol. 2018;17(1):132.
Otagaki M, Matsumura K, Kin H, et al. Effect of tofogliflozin on systolic and diastolic cardiac function in type 2 diabetic patients. Cardiovasc Drugs Ther. 2019;33(4):435–42.
Cohen ND, Gutman SJ, Briganti EM, et al. The effects of empagliflozin treatment on cardiac function and structure in patients with type 2 diabetes - a cardiac MR study. Intern Med J. 2019;49(8):1006–10.
Gerich JE. Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications. Diabet Med. 2010;27(2):136–42.
Ansary TM, Nakano D, Nishiyama A. Diuretic effects of sodium glucose cotransporter 2 inhibitors and their influence on the renin-angiotensin system. Int J Mol Sci. 2019;20(3):E629.
Heise T, Jordan J, Wanner C, et al. Pharmacodynamic effects of single and multiple doses of empagliflozin in patients with type 2 diabetes. Clin Ther. 2016;38(10):2265–76.
Habibi J, Aroor AR, Sowers JR, et al. Sodium glucose transporter 2 (SGLT2) inhibition with empagliflozin improves cardiac diastolic function in a female rodent model of diabetes. Cardiovasc Diabetol. 2017;16(1):9.
Younis F, Leor J, Abassi Z, et al. Beneficial effect of the SGLT2 inhibitor empagliflozin on glucose homeostasis and cardiovascular parameters in the cohen Rosenthal diabetic hypertensive (CRDH) rat. J Cardiovasc Phamacol Ther. 2018;23(4):358–71.
Yasui A, Lee G, Hirase T, et al. Empagliflozin induces transient diuresis without changing long-term overall fluid balance in Japanese patients with type 2 diabetes. Diabetes Ther. 2018;9(2):863–71.
Tanaka H, Takano K, Iijima H, et al. Factors affecting canagliflozin-induced transient urine volume increase in patients with type 2 diabetes mellitus. Adv Ther. 2017;34(2):436–51.
Hao Z, Huang X, Shao H, et al. Effects of dapagliflozin on serum uric acid levels in hospitalized type 2 diabetic patients with inadequate glycemic control: a randomized controlled trial. Ther Clin Risk Manag. 2018;14:2407–13.
Napolitano A, Miller S, Murgatroyd PR, et al. Exploring glycosuria as a mechanism for weight and fat mass reduction. A pilot study with remogliflozin etabonate and sergliflozin etabonate in healthy obese subjects. J Clin Transl Endocrinol. 2013;1(1):e3–8.
Schork A, Saynisch J, Vosseler A, et al. Effect of SGLT2 inhibitors on body composition, fluid status and renin-angiotensin-aldosterone system in type 2 diabetes: a prospective study using bioimpedance spectroscopy. Cardiovasc Diabetol. 2019;18(1):46.
Sattar N, McLaren J, Kristensen SL, et al. SGLT2 inhibition and cardiovascular events: why did EMPA-REG outcomes surprise and what were the likely mechanisms? Diabetologia. 2016;59(7):1333–9.
Baker WL, Smyth LR, Riche DM, et al. Effects of sodium-glucose co-transporter 2 inhibitors on blood pressure: a systematic review and meta-analysis. J Am Soc Hypertens. 2014;8(4):262–75.
Inzucchi SE, Zinman B, Fitchett D, et al. How does empagliflozin reduce cardiovascular mortality? Insights from a mediation analysis of the EMPA-REG OUTCOME trial. Diabetes Care. 2018;41(2):356–63.
Fitchett DH. Empagliflozin and cardio-renal outcomes in patients with type 2 diabetes and cardiovascular disease - implications for clinical practice. Eur Endocrinol. 2018;14(2):40–9.
Joubert M, Jagu B, Montaigne D, et al. The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents cardiomyopathy in a diabetic lipodystrophic mouse model. Diabetes. 2017;66(4):1030–40.
Pabel S, Wagner S, Bollenberg H, et al. Empagliflozin directly improves diastolic function in human heart failure. Eur J Heart Fail. 2018;20(12):1690–700.
Shi L, Zhu D, Wang S, et al. Dapagliflozin attenuates cardiac remodeling in mice model of cardiac pressure overload. Am J Hypertens. 2019;32(5):452–9.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
KM and TS were primary responsible for the conception and design of review. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Matsumura, K., Sugiura, T. Effect of sodium glucose cotransporter 2 inhibitors on cardiac function and cardiovascular outcome: a systematic review. Cardiovasc Ultrasound 17, 26 (2019). https://doi.org/10.1186/s12947-019-0177-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12947-019-0177-8