Abstract
Background
Patients with non-ischemic heart failure etiology and left bundle branch block (LBBB) show better response to cardiac resynchronization therapy (CRT). While these patients have the most pronounced left ventricular (LV) dyssynchrony, LV dyssynchrony assessment often fails to predict outcome. We hypothesized that patients with favorable outcome from CRT can be identified by a characteristic strain distribution pattern.
Methods
From 313 patients who underwent CRT between 2003 and 2006, we identified 10 patients who were CRT non-responders (no LV end-systolic volume [LVESV] reduction) with non-ischemic cardiomyopathy and LBBB and compared with randomly selected CRT responders (n = 10; LVESV reduction ≥15 %). Longitudinal strain (εlong) data were obtained by speckle tracking echocardiography before and after (9 ± 5 months) CRT implantation and standardized segmental εlong-time curves were obtained by averaging individual patients.
Results
In responders, ejection fraction (EF) increased from 25 ± 9 to 40 ± 11 % (p = 0.002), while in non-responders, EF was unchanged (20 ± 8 to 21 ± 5 %, p = 0.57). Global εlong was significantly lower in non-responders at pre CRT (p = 0.02) and only improved in responders (p = 0.04) after CRT. Pre CRT septal εlong -time curves in both groups showed early septal contraction with mid-systolic decrease, while lateral εlong showed early stretch followed by vigorous mid to late contraction. Restoration of contraction synchrony was observed in both groups, though non-responder remained low amplitude of εlong.
Conclusions
CRT non-responders with LBBB and non-ischemic etiology showed a similar improvement of εlong pattern with responders after CRT implantation, while amplitude of εlong remained unchanged. Lower εlong in the non-responders may account for their poor response to CRT.
Similar content being viewed by others
Background
Cardiac resynchronization therapy (CRT) improves survival by stopping or reversing adverse remodeling that occurs in systolic heart failure [1–3]. The mechanism of CRT is coordination of the contraction pattern of otherwise dyssynchronous opposing left ventricular (LV) walls which are, in a clinically common setting of left bundle branch block (LBBB), septal and lateral ones [4, 5].
While several clinical parameters have been well established as predictors of CRT response [1, 3, 6], failure of CRT occurs even if all of clinical parameters predict otherwise. It is unclear if this is due to a specific contraction pattern of these patients, or some other factors. For this purpose we analyzed the contraction pattern of CRT patients with clinical and procedural characteristics known to be associated with pronounced reverse remodeling response: non-ischemic heart failure etiology, LBBB pattern on electrocardiogram (ECG), QRS duration on ECG >140 ms, and LV electrode located over the mid/base lateral or posterolateral wall [1, 3, 6, 7]. We identified a group of patients who, despite these favorable pre-procedural characteristics, did not show reverse remodeling, and compared it to a group with good CRT response using segmental strain analysis.
Methods
Population
The study population was selected from 313 consecutive heart failure patients who underwent implantation of a biventricular device at the Cleveland Clinic between January 2003 and June 2006, who also had long-term echocardiographic follow-up [3] (Fig. 1). They all had symptomatic heart failure, an ejection fraction of <35 % and QRS duration of >120 ms. CRT was provided in the standard fashion with 3 trans-venous leads, including the LV lead inserted through the coronary sinus.
From those who had a complete baseline echocardiographic study performed within 3 months before device implantation on a Vivid 7 system (GE Healthcare, Horten, Norway) and with echocardiographic follow-up (>3 months), we identified 10 patients who were CRT non-responders (unchanged or increased LV end-systolic volume [LVESV] at follow-up) with the following clinical characteristics: non-ischemic cardiomyopathy, LBBB, and LV lead placed over the base/mid posterior or lateral LV wall. We compared this group with a group of ten patients with the same characteristics except for being CRT responders (reduction of LVESV at follow-up ≥15 %) who were randomly selected from the same study population. The patient data were de-identified and that the study was approved by the Cleveland Clinic Institutional Review Board.
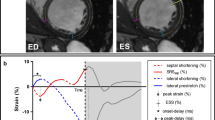
Longitudinal strain-time analysis
Two-dimensional speckle tracking (EchoPAC 10.0, GE Healthcare) was performed using the images acquired in the apical 4 chamber, 2 chamber and long axis views. The peak of the R wave on the ECG was used as a reference time point for end-diastole, and aortic valve closure was used as a time point for end-systole. Segmental longitudinal strain (εlong) curves derived from a single cardiac cycle were exported for analysis, with resulting 18 εlong curves corresponding to the basal-mid-apical septum, anteroseptum, inferior, posterior, lateral and anterior segments obtained in each patient. To correct for RR interval variation, εlong curves were normalized using the two reference time points of end-diastole and end-systole, so that time was expressed as a percentage of systole (% systole) [8, 9]. Care was taken to ensure that the end-diastolic time points for speckle tracking are consistent across all three apical views.
To better characterize segmental εlong profiles in both patient groups pre and post CRT, individual εlong curves were averaged to obtain a characteristic average εlong profile [8, 9]. Figure 2 shows individual εlong curves of the basal anterolateral segment (A), and corresponding group average εlong curve (B) obtained in CRT responders before pacing. Finally, global εlong was calculated by averaging segmental values.
Individual (a) and averaged (b) strain-time curve of basal lateral segment in the responders prior to cardiac resynchronization therapy. a Individual segmental strain-time curves, normalized for systolic duration, obtained from basal lateral segment in the responders group prior to start of cardiac resynchronization therapy. Systolic duration is defined as the time from the mitral valve closure to aortic valve closure. b Averaged normalized segmental strain-time curve (with error bars indicating standard error) obtained by averaging the data shown in Panel a. Arrows depict the time points corresponding to mid systole (50 %), end-systole (100 %) and post-systole (125 %). CRT, cardiac resynchronization therapy
Statistical analysis
Continuous variables with normal distribution were expressed as mean ± SD, and categorical variables were expressed as count and percentage. Between and within-group differences were assessed by Wilcoxon signed-rank test and Mann-Whitney U test as appropriate. To assess opposing wall mechanics before and after CRT, we entered εlong measurements from basal and mid LV levels of the opposing walls (e.g., septal and lateral) obtained at early systole (50 % of systole duration), end-systole (100 % of systole duration) and post-systole (125 % of systole duration) into mixed model analysis, using an unstructured covariance model. The model was constructed with “time” (% systole) as covariate, and “wall” (e.g., septum vs. lateral) and “group” (responders vs. non-responders) as factors. Interaction between time and wall, which quantitates between-wall difference in pattern of εlong development, was taken to represent loss of coordinated contraction (dyssynchrony). The Akaike criterion was used to determine the optimal model. P values <0.05 were considered as statistically significant. Statistical analyses were performed using JMP Pro 10.0.2 (SAS Institute Inc., Cary, North Carolina).
Results
Of the 313 consecutive patients who underwent CRT and follow-up, 155 (50 %) had reverse remodeling and 89 (28 %) patients had no response to CRT. Of those 89 patients, 10 (11 %) patients met the inclusion criteria. Among patients who responded to CRT, 38 patients met the inclusion criteria and 10 patients were randomly selected as the comparison group. The baseline clinical, electrocardiographic, and echocardiographic characteristics were similar between responders and non-responders (Table 1). One non-responder patient was excluded from the analysis because of poor images at baseline. The mean age of the population was 58 ± 8 years, with 89 % having New York Heart Association (NYHA) class III/IV symptoms. All patients had sinus rhythm and left bundle branch block with a QRS duration of 168 ± 20 ms. All implanted devices were biventricular implantable cardioverter defibrillators (CRT-D), with left ventricular lead position in the lateral (n = 12) and posterolateral (n = 7) cardiac veins. There was no difference between these two groups.
Baseline left ventricular volumes and ejection fraction were not different between responders and non-responders (Table 2). At follow-up after an average CRT duration of 9 ± 5 months, responders showed improvement of LV end-diastolic volume (LVEDV) (p = 0.01), LVESV (p = 0.002), and EF (p = 0.002), while non-responders showed significant enlargement of LVEDV (p = 0.004) and LVESV (p = 0.01). Although there was no difference in LV volumes or ejection fractions between the two groups before CRT, LVEDV (p = 0.008) and LVESV (p = 0.002) were significantly smaller, and EF (p = 0.002) was higher in responders after CRT implantation.
Global εlong
Table 3 outlines the global εlong values in responders and non-responders at mid-systole (50 % systole), end-systole (100 % systole) and early post-systole (125 % systole). Before CRT, global εlong at end-systole (p = 0.02) and early post-systole (p = 0.03) were lower in the non-responder group. At a follow up, in addition to end-systole and early post-systole εlong, non-responders showed lower global mid-systole εlong (p = 0.03). In responders, global end-systolic (p = 0.04) and early post-systolic εlong (p = 0.03) demonstrated improvement after CRT implantation, whereas there were no significant improvement in non-responders.
Opposing walls mechanics before and after CRT
Figure 3 showed averaged εlong-time curves of 18 segments in responder and non-responder. Each panel showed pre- and post-CRT septal and lateral wall εlong-time curves of basal, mid, and apical segment for responders and non-responders. Pre- CRT, the basal and mid septal εlong-time curves demonstrated a pattern of early septal contraction with mid-systolic decrease, while basal and mid lateral εlong-time curves demonstrated an early stretch followed by vigorous mid to late contraction. Post-CRT, restoration of contraction synchrony was noted in both the septal and lateral segments. This pattern pre- and post-CRT was to a lesser extent observed in the posterior and anteroseptal walls respectively (Fig. 4) and was lost in the inferior and anterior walls (Fig. 5). While the shapes of the εlong-time curves were similar in responders and non-responders, these two groups differed markedly in amplitude, both pre- and post-CRT.
Averaged normalized segmental longitudinal strain-time curves of septal and lateral segments in responders and non-responders to cardiac resynchronization therapy. The strain-time curves have lower amplitude in non-responders. Cardiac resynchronization therapy results in a more uniform shape of the strain-time curves with cardiac resynchronization therapy. Error bars represent standard errors. Pre: prior to start of cardiac resynchronization therapy; Post: 9 ± 5 months after the start of cardiac resynchronization therapy
Averaged normalized segmental longitudinal strain-time curves of posterior and anteroseptal segments in responders and non-responders to cardiac resynchronization therapy. Error bars represent standard errors. Pre: prior to start of cardiac resynchronization therapy; Post: 9 ± 5 months after the start of cardiac resynchronization therapy
Averaged normalized segmental longitudinal strain-time curves of inferior and anterior segments in responders and non-responders to cardiac resynchronization therapy. Error bars represent standard errors. Pre: prior to start of cardiac resynchronization therapy; Post: 9 ± 5 months after the start of cardiac resynchronization therapy
To quantify these observations, we compared εlong of the opposing walls at mid, end, and post-systole (i.e., 50 %, 100 % and 125 % of systole).
Septal vs. lateral
Prior to CRT, εlong was lower in the lateral than in the septal wall (p = 0.001). Septal and lateral walls were also different in the pattern of εlong increase (p = 0.001; Fig. 6a). There was no difference between responders and non-responders in overall εlong, the pattern of εlong increase, or in the difference between εlong of opposing walls (p = NS for all). After CRT, lateral wall εlong was still higher (p = 0.007), but difference in the pattern of εlong increase disappeared (p = 0.80). Responders showed higher overall εlong (p = 0.02), and more marked εlong increase over time (p = 0.03).
Comparison of opposing wall mechanics during ventricular contraction before and after cardiac resynchronization therapy (CRT). Strain values are measured at mid-systole (50 %), end-systole (100 %) and post-systole (125 %) before (upper panels) and >3 months after the start of CRT (lower panels). a Septal and lateral longitudinal wall strains; b Anteroseptal and posterior longitudinal wall strains; and c Inferior and anterior longitudinal wall strains. Error bars represent standard errors. CRT, cardiac resynchronization therapy
Posterior vs. anteroseptal
Posterior and anteroseptal walls prior to CRT showed different patterns of εlong increase (p = 0.01), but similar average εlong (p = 0.20) (Fig. 6b). Interestingly, responders had higher overall εlong of these two walls (p = 0.02). After 12 months of CRT, difference in the pattern of εlong increase in opposing walls disappeared (p = 0.70). Responders showed a trend towards having higher overall εlong (p = 0.08).
Inferior vs. anterior
Inferior and anterior walls before CRT had similar patterns of εlong increase (p = NS) (Fig. 6c). Responders and non-responders did not differ in the overall εlong, the pattern of εlong increase, or in the difference between opposing wall εlong (p = NS for all). After 12 months of CRT, responders showed higher overall εlong (p = 0.02), again with no difference between εlong of opposing walls (p = NS).
Predicting CRT response with baseline Global εlong
In the logistic regression model, the pre CRT average εlong was significantly associated with CRT response. The area under the receiver operating characteristic curve showed average εlong at end systole -4.0 % as optimal cutoff point (AUC 0.83, 95 % CI 0.64 – 1.00, p = 0.014). This cutoff point predicted CRT response with 78 % specificity and 80 % sensitivity in this population. Other echocardiographic parameters and baseline characteristics did not predict response.
Discussion
In this paper, CRT non-responders despite having favorable predictors of good response to CRT (i.e., non-ischemic heart failure etiology, LBBB, QRS complex duration >140 ms, and appropriate LV electrode placement) have lower global end systolic longitudinal strain but a similar pattern of longitudinal strain contraction heterogeneity pre-CRT as responders. This indicates that the presence of, and subsequent improvement of, dyssynchrony is not sufficient to result in reverse remodeling during CRT. Their markedly lower longitudinal strain suggested myocardial dysfunction burden might be the predictor of reverse remodeling in patients with non-ischemic cardiomyopathy.
Ventricular function in left bundle branch block: characteristic contraction pattern versus dyssynchrony
Animal models have demonstrated that right ventricular pacing (an LBBB surrogate) induces a characteristic pattern of blunted early septal and forceful delayed lateral wall contraction preceded by its early stretch [4, 5, 10]. Traditional dyssynchrony indices are positive scalar numbers that lack the ability to localize the origin of dyssynchrony. As an example, the standard deviation of the time to peak of systolic myocardial tissue velocities [11] will have the same value whether the most delayed segment is in the basal lateral or apical septal LV segment. Some clinical studies have shown that early segmental stretch can be detected in some CRT candidates [12, 13]. In this study, we constructed average segmental strain-time curves from two well-defined patient groups, a characteristic pattern of early, suppressed contraction of the basal and mid septum, and early stretch followed by strong contraction of the basal and mid lateral walls. These characteristic segmental strain-time curves overcome the major drawback of LV dyssynchrony indices [13–18] in defining the characteristic profile of LBBB induced dyssynchrony.
The improvement of LV contraction heterogeneity underlies some of the benefits of CRT. Unfortunately, prospective multi-institutional trials failed to confirm the predictive value of the most frequently used dyssynchrony indices [10, 19]. Even in selected populations that qualify for CRT therapy by current criteria, the predictive value of a dyssynchrony index may be low [19, 20]. Several other factors make relevance of dyssynchrony indices doubtful. Dyssynchrony detected by one index is often not confirmed when a different index is used [21]. Dyssynchrony indices are often positive in the setting of narrow QRS complex [21], where CRT treatment is shown to be ineffective [22, 23]. Velocity-based indices are influenced by myocardial translational motion that is often present in the setting of severe LV dilatation [24]. Finally, the limit of any dyssynchrony index may in the end be the fact that in some patients, myocardium has simply “burnt-out,” hence losing therapeutic and contractile reserve [25]. Similar characteristics of strain-time and their improvement were observed both in responder and non-responder groups in this study and did not predict LV reverse remodeling after CRT implantation. However baseline average longitudinal strain might be a surrogate to distinguish the non-responder group.
LV longitudinal strain as predictors of reverse remodeling
The MADIT-CRT cohort also supported that decreased average longitudinal strain predicts less beneficial effects of CRT, especially in the setting of LBBB [26, 27]. Several studies reported baseline global longitudinal strain predicts LV reverse remodeling after CRT in patients with both ischemic and non-ischemic cardiomyopathy [26, 28]. Our result confirmed these reports by demonstrating it in CRT non-responders with the non-ischemic population, though a small sample size. A recent study showed depressed longitudinal strain was strongly associated with total scar burden assessed by cardiovascular magnetic resonance imaging in ischemic heart failure patients, and it may be a sensitive parameter of LV contractile reserve and the presence of viable myocardium [28–30]. Another report showed longitudinal strain improvement after CRT implantation also indicated better clinical outcome and reverse remodeling, suggesting contractile reserve is associated with reverse remodeling [31]. Since responders showed significant improvement of longitudinal strain in the present study, our findings suggest that underlying myocardial deformation could be the determinant of reverse remodeling after CRT implantation in patients with non-ischemic cardiomyopathy and LBBB.
Study limitations
This is a small, retrospective, observational study. Only longitudinal strains were assessed, although various previous studies have used circumferential or radial strains [5, 16]. However, longitudinal strains have lower measurement error, and the ability of obtaining anatomically accurate views is often easier from the apical rather than from the parasternal position. In addition, as we used very strict selection criteria, the number of patients was relatively small, and we lacked statistical power to perform multivariate analysis to predict CRT response. Therefore response to CRT might be affected by other factors besides LV strain. Additionally, our result seems inefficient in patients with ischemic cardiomyopathy, who often do not show reverse remodeling after CRT. Further large prospective study is required to verify the predictive value of longitudinal strain in assessing LV reverse remodeling.
Conclusions
Our study defines the characteristic segmental pattern of LV contraction in patients with non-ischemic cardiomyopathy and LBBB before and after CRT. CRT non-responders with non-ischemic cardiomyopathy and LBBB demonstrated a qualitatively similar segmental contraction pattern but have dramatically decreased longitudinal strain. These findings may help in predicting the outcome of CRT in these patients.
Abbreviations
- CRT:
-
cardiac resynchronization therapy
- LV:
-
left ventricular
- LBBB:
-
left bundle branch block
- LVESV:
-
left ventricular end-systolic volume
- EF:
-
ejection fraction
- εlong:
-
Longitudinal strain
- ECG:
-
electrocardiogram
- NYHA:
-
New York Heart Association
- CRT-D:
-
biventricular implantable cardioverter defibrillator
- LVEDV:
-
left ventricular end-diastolic volume
References
Goldenberg I, Moss AJ, Hall WJ, Foster E, Goldberger JJ, Santucci P, Shinn T, Solomon S, Steinberg JS, Wilber D et al. Predictors of response to cardiac resynchronization therapy in the Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT). Circulation. 2011;124(14):1527–36.
Solomon SD, Foster E, Bourgoun M, Shah A, Viloria E, Brown MW, Hall WJ, Pfeffer MA, Moss AJ. Effect of cardiac resynchronization therapy on reverse remodeling and relation to outcome: multicenter automatic defibrillator implantation trial: cardiac resynchronization therapy. Circulation.2010;122(10):985–92.
Verhaert D, Grimm RA, Puntawangkoon C, Wolski K, De S, Wilkoff BL, Starling RC, Tang WH, Thomas JD, Popovic ZB. Long-term reverse remodeling with cardiac resynchronization therapy: results of extended echocardiographic follow-up. J Am Coll Cardiol. 2010;55(17):1788–95.
Peschar M, de Swart H, Michels KJ, Reneman RS, Prinzen FW. Left ventricular septal and apex pacing for optimal pump function in canine hearts. J Am Coll Cardiol. 2003;41(7):1218–26.
Prinzen FW, Hunter WC, Wyman BT, McVeigh ER. Mapping of regional myocardial strain and work during ventricular pacing: experimental study using magnetic resonance imaging tagging. J Am Coll Cardiol. 1999;33(6):1735–42.
Cleland J, Freemantle N, Ghio S, Fruhwald F, Shankar A, Marijanowski M, Verboven Y, Tavazzi L. Predicting the long-term effects of cardiac resynchronization therapy on mortality from baseline variables and the early response a report from the CARE-HF (Cardiac Resynchronization in Heart Failure) Trial. J Am Coll Cardiol. 2008;52(6):438–45.
Singh JP, Klein HU, Huang DT, Reek S, Kuniss M, Quesada A, Barsheshet A, Cannom D, Goldenberg I, McNitt S, et al. Left ventricular lead position and clinical outcome in the multicenter automatic defibrillator implantation trial-cardiac resynchronization therapy (MADIT-CRT) trial. Circulation. 2011;123(11):1159–66.
Puwanant S, Park M, Popovic ZB, Tang WH, Farha S, George D, Sharp J, Puntawangkoon J, Loyd JE, Erzurum SC, et al. Ventricular geometry, strain, and rotational mechanics in pulmonary hypertension. Circulation. 2010;121(2):259–66.
Popovic ZB, Grimm RA, Ahmad A, Agler D, Favia M, Dan G, Lim P, Casas F, Greenberg NL, Thomas JD. Longitudinal rotation: an unrecognised motion pattern in patients with dilated cardiomyopathy. Heart. 2008;94(3), e11.
Verbeek XA, Vernooy K, Peschar M, Cornelussen RN, Prinzen FW. Intra-ventricular resynchronization for optimal left ventricular function during pacing in experimental left bundle branch block. J Am Coll Cardiol. 2003;42(3):558–67.
Yu CM, Chau E, Sanderson JE, Fan K, Tang MO, Fung WH, Lin H, Kong SL, Lam YM, Hill MR, et al. Tissue Doppler echocardiographic evidence of reverse remodeling and improved synchronicity by simultaneously delaying regional contraction after biventricular pacing therapy in heart failure. Circulation. 2002;105(4):438–45.
Kirn B, Jansen A, Bracke F, van Gelder B, Arts T, Prinzen FW. Mechanical discoordination rather than dyssynchrony predicts reverse remodeling upon cardiac resynchronization. Am J Physiol Heart Circ Physiol. 2008;295(2):H640–6.
Carasso S, Rakowski H, Witte KK, Smith P, Carasso D, Garceau P, Sasson Z, Parker JD. Left ventricular strain patterns in dilated cardiomyopathy predict response to cardiac resynchronization therapy: timing is not everything. J Am Soc Echocardiogr. 2009;22(3):242–50.
Gorcsan 3rd J, Abraham T, Agler DA, Bax JJ, Derumeaux G, Grimm RA, Martin R, Steinberg JS, Sutton MS, Yu CM. Echocardiography for cardiac resynchronization therapy: recommendations for performance and reporting--a report from the American Society of Echocardiography Dyssynchrony Writing Group endorsed by the Heart Rhythm Society. J Am Soc Echocardiogr. 2008;21(3):191–213.
Helm RH, Leclercq C, Faris OP, Ozturk C, McVeigh E, Lardo AC, Kass DA. Cardiac dyssynchrony analysis using circumferential versus longitudinal strain: implications for assessing cardiac resynchronization. Circulation. 2005;111(21):2760–7.
Suffoletto MS, Dohi K, Cannesson M, Saba S, Gorcsan 3rd J. Novel speckle-tracking radial strain from routine black-and-white echocardiographic images to quantify dyssynchrony and predict response to cardiac resynchronization therapy. Circulation. 2006;113(7):960–8.
Murphy RT, Sigurdsson G, Mulamalla S, Agler D, Popovic ZB, Starling RC, Wilkoff BL, Thomas JD, Grimm RA. Tissue synchronization imaging and optimal left ventricular pacing site in cardiac resynchronization therapy. Am J Cardiol. 2006;97(11):1615–21.
Bax JJ, Bleeker GB, Marwick TH, Molhoek SG, Boersma E, Steendijk P, van der Wall EE, Schalij MJ. Left ventricular dyssynchrony predicts response and prognosis after cardiac resynchronization therapy. J Am Coll Cardiol. 2004;44(9):1834–40.
Chung ES, Leon AR, Tavazzi L, Sun JP, Nihoyannopoulos P, Merlino J, Abraham WT, Ghio S, Leclercq C, Bax JJ, et al. Results of the predictors of response to CRT (PROSPECT) trial. Circulation. 2008;117(20):2608–16.
Delgado V, Ypenburg C, van Bommel RJ, Tops LF, Mollema SA, Marsan NA, Bleeker GB, Schalij MJ, Bax JJ. Assessment of left ventricular dyssynchrony by speckle tracking strain imaging comparison between longitudinal, circumferential, and radial strain in cardiac resynchronization therapy. J Am Coll Cardiol. 2008;51(20):1944–52.
Zhang Q, van Bommel RJ, Chan YS, Delgado V, Liang Y, Schalij MJ, Bax JJ, Fang F, Wai-Kwok Yip G, Yu CM. Diverse patterns of longitudinal and radial dyssynchrony in patients with advanced systolic heart failure. Heart. 2011;97(7):574–8.
Beshai JF, Grimm RA, Nagueh SF, Baker 2nd JH, Beau SL, Greenberg SM, Pires LA, Tchou PJ. Cardiac-resynchronization therapy in heart failure with narrow QRS complexes. N Engl J Med. 2007;357(24):2461–71.
Ruschitzka F, Abraham WT, Singh JP, Bax JJ, Borer JS, Brugada J, Dickstein K, Ford I, Gorcsan J, 3rd, Gras D, et al. Cardiac-resynchronization therapy in heart failure with a narrow QRS complex. N Engl J Med. 2013;369(15):1395–405.
Phillips KP, Popovic ZB, Lim P, Meulet JE, Barrett CD, Di Biase L, Agler D, Thomas JD, Grimm RA. Opposing wall mechanics are significantly influenced by longitudinal cardiac rotation in the assessment of ventricular dyssynchrony. JACC Cardiovasc Imaging. 2009;2(4):379–86.
Otasevic P, Popovic ZB, Vasiljevic JD, Vidakovic R, Pratali L, Vlahovic A, Neskovic AN. Relation of myocardial histomorphometric features and left ventricular contractile reserve assessed by high-dose dobutamine stress echocardiography in patients with idiopathic dilated cardiomyopathy. Eur J Heart Fail. 2005;7(1):49–56.
Knappe D, Pouleur AC, Shah AM, Cheng S, Uno H, Hall WJ, Bourgoun M, Foster E, Zareba W, Goldenberg I, et al. Dyssynchrony, contractile function, and response to cardiac resynchronization therapy. Circ Heart Fail. 2011;4(4):433–40.
Pouleur AC, Knappe D, Shah AM, Uno H, Bourgoun M, Foster E, McNitt S, Hall WJ, Zareba W, Goldenberg I, et al. Relationship between improvement in left ventricular dyssynchrony and contractile function and clinical outcome with cardiac resynchronization therapy: the MADIT-CRT trial. Eur Heart J. 2011;32(14):1720–9.
D'Andrea A, Caso P, Scarafile R, Riegler L, Salerno G, Castaldo F, Gravino R, Cocchia R, Del Viscovo L, Limongelli G, et al. Effects of global longitudinal strain and total scar burden on response to cardiac resynchronization therapy in patients with ischaemic dilated cardiomyopathy. Eur J Heart Fail. 2009;11(1):58–67.
Roes SD, Mollema SA, Lamb HJ, van der Wall EE, de Roos A, Bax JJ. Validation of echocardiographic two-dimensional speckle tracking longitudinal strain imaging for viability assessment in patients with chronic ischemic left ventricular dysfunction and comparison with contrast-enhanced magnetic resonance imaging. Am J Cardiol. 2009;104(3):312–7.
Rosendahl L, Blomstrand P, Brudin L, Todt T, Engvall JE. Longitudinal peak strain detects a smaller risk area than visual assessment of wall motion in acute myocardial infarction. Cardiovasc Ultrasound. 2010;8(2):1476–7120.
Hasselberg NE, Haugaa KH, Bernard A, Ribe MP, Kongsgaard E, Donal E, Edvardsen T. Left ventricular markers of mortality and ventricular arrhythmias in heart failure patients with cardiac resynchronization therapy. Eur Heart J Cardiovasc Imaging. 2015;11.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ACYT, MBChB: acquisition of data, analysis and interpretation of data, and drafting the article RDB, MD: analysis of data, drafting the article. KS, MD: analysis of data, drafting the article. RAG, MD: critical revision and final approval of the article. JDT, MD: critical revision and final approval of the article. BLW, MD: critical revision and final approval of the article. DA, RDCS: acquisition of data and critical revision. ZBP MD, PhD: Conception and design of data, analysis and interpretation of data, critical revision, final approval of the article.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
To, A.C.Y., Benatti, R.D., Sato, K. et al. Strain-time curve analysis by speckle tracking echocardiography in cardiac resynchronization therapy: Insight into the pathophysiology of responders vs. non-responders. Cardiovasc Ultrasound 14, 14 (2015). https://doi.org/10.1186/s12947-016-0057-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12947-016-0057-4