Abstract
Background
Left ventricular hypertrophy (LVH) is a critical factor in heart failure and cardiovascular event-related mortality. While the prevalence of LVH in diabetic patients is well-documented, its occurrence and risk factors in non-diabetic populations remain largely unexplored. This study addresses this issue by investigating the independent risk factors of LVH in non-diabetic individuals.
Methods
This cross-sectional study, conducted meticulously, utilized data from a robust and comprehensive source, DATADRYAD, in the Sierra Leone database, collected between October 2019 and October 2021, including LVH and various variables. All variables were described and screened using univariate analysis, Spearman correlation, and principal component analysis (PCA). The lipid profile, including total cholesterols (TC), triglycerides (TG), high-density lipoprotein (HDL-C), non-high-density lipoprotein (Non-HDL-C), and low-density lipoprotein cholesterol (LDL-C), TC/HDL-C ratio, TG/HDL-C ratio, Non-HDL-C /HDL-C ratio and LDL-C/HDL-C ratio, which quartiles were treated as categorical variables, with the lowest quartile serving as the reference category. Three adjusted models were constructed to mitigate the influence of other variables. To ensure the robustness of the model, receiver operating characteristic (ROC) curves were used to calculate the cutoff values by analyzing the ROC curves. A sensitivity analysis was performed to validate the findings further.
Results
The dataset encompasses information from 2092 individuals. After adjusting for potential factors that could influence the results, we found that TC (OR = 2.773, 95%CI: 1.805–4.26), Non-HDL-C (OR = 2.74, 95%CI: 1.7723–4.236), TC/HDL-C ratio (OR = 2.237, 95%CI: 1.445–3.463), Non-HDL-C/HDL-C ratio (OR = 2.357, 95%CI: 1.548–3.588), TG/HDL-C ratio (OR = 1.513, 95%CI: 1.02–2.245) acts as independent risk factors of LVH. ROC curve analysis revealed the predictive ability of blood lipids for LVH, with Non-HDL-C exhibiting area under the curve (AUC = 0.6109), followed by TC (AUC = 0.6084).
Conclusions
TC, non-HDL-C, TC/HDL-C ratio, Non-HDL-C/HDL-C ratio, and TG/HDL-C ratio were independent risk factors of LVH in non-diabetic people. Non-HDL-C and TC were found to be essential indicators for predicting the prevalence of LVH.
Similar content being viewed by others
Introduction
Heart failure (HF) syndrome is a major clinical and public health problem associated with notable morbidity and mortality [1], which affects more than 64 million people worldwide [2]. Adverse changes in cardiac structure and function, known as cardiac remodeling, play a crucial role in the development of heart failure [3]. A particularly significant aspect of this process is LVH, defined as LVMI greater than 95 g/m²in women and greater than 115 g/m²in men [4, 5]. In LVH, the thickening of the heart wall leads to increased muscle stiffness, known as diastolic dysfunction, which impairs the heart’s ability to relax and appropriately fill with blood during the resting phase of the cardiac cycle [6, 7]. Consequently, the heart’s efficiency in pumping blood is diminished, resulting in decreased cardiac output and an increased workload on the heart [8]. Over time, this can lead to the heart being unable to pump with the necessary force [9, 10]. Approximately 8.7–13% of patients with LVH develop dysfunction of the left ventricular ejection fraction, which is a significant risk factor for cardiovascular mortality [11]. Early identification of individuals at higher risk for developing LVH is crucial for reducing related disability and mortality [12, 13]. According to some cross-sectional studies, diabetic individuals with high levels of glycated hemoglobin (HbA1c) may have increased left ventricular mass, which may be related to blood glucose uncontroled [14]; the prevalence of LVH in diabetes was 17.1-20.7% in Italy and Iran [15, 16]. Most studies have concentrated on examining risk factors for heart failure (HF) among individuals with diabetes, leaving a significant void in understanding the same in populations without diabetes [17]. Triglycerides and high-density lipoprotein have been observed to be associated with LVH in the general population in China [18]. In comparison, this study aimed to investigate whether lipid profile, including TC, TG, HDL-C, LDL-C, and Non-HDL-C, are independent risk factors that will predict LVH in the non-diabetic population and to assess their predictive value.
Methods
Study population
This cross-sectional clinical data was collected from pedestrians living in Western Area Urban, Freetown, Sierra Leone, between October 2019 and October 2021 to evaluate the prevalence of cardiometabolic risk factors among adults in Sierra Leone. This study examined the prevalence of cardiometabolic risk factors, target organ damage, and their associated factors among adults [19]. This project’s data were segregated from the “DATADRYAD” database (https://datadryad.org/stash). As the study was a secondary study examining public data from a database, no ethical approval was required. This study obtained data from a database comprising information on 2,394 participants. After exclusions, which involved removing 199 participants with a history of diabetes mellitus and 103 participants with pre-diabetes, the final cohort included 2,092 individuals. Among them, 287 were identified as LVH, while the remaining 1,805 were classified as non-LVH (Fig. 1).
Variables of interest
Physical examinations were conducted on all participants as part of the study, encompassing various aspects such as demographic data (age, gender, and income), lifestyle factors (fruit and vegetable consumption, smoking, and alcohol consumption), medical history (family history of hypertension and diabetes mellitus), anthropometric measurements (Body weight, height, and waist circumference), echocardiography, and blood tests. Information about the participants was collected using standard survey questionnaires. Blood pressure was measured using an Omron electronic sphygmomanometer with an appropriately sized cuff. Participants were seated during the recording, preceded by 3–5 min of rest. The average of two recordings was taken as the blood pressure reading. Weight, height, and waist circumference measurements were taken while participants were lightly clothed and barefoot. These measurements provide insight into body composition and health status. Blood samples were collected from the median cubital vein after an overnight fast (8–10 h) on the morning of the second day. Hypertension was defined as an average systolic blood pressure of 140 mm Hg or higher, diastolic blood pressure of 90 mm Hg or greater, or a participant-reported current use of antihypertensive medication. A participant who smoked more than 100 sticks of cigarettes in their lifetime and was still smoking at the interview was referred to as a smoker, while an ex-smoker was someone who had stopped smoking at least 28 days before the interview. Data on alcohol consumption were based on the WHO step survey tool. The body mass index (BMI) was calculated as a ratio of the weight in kilograms and the square of the height in meters. BMI-based body habitus was classified as obese (BMI ≥ 30 kg/m2), and abdominal obesity was defined as WC > 88 cm for women and 102 cm for men. Diabetes mellitus was defined as a fasting blood glucose (FPG) level of 7.0 mmol/L or greater, HbA1c ≥ 6.5%, or using insulin or an oral hypoglycaemic agent. Pre-diabetes was defined as FPG between 6.1 mmol/L and 6.9 mmol/L. The blood tests included analysis for total TC, TG, HDL-C, and LDL-C levels. TC calculated Non-HDL-C minus HDL-C. All lipid profile were grouped according to the interquartile method. LVMI was calculated by dividing Left ventricular mass by body surface area.
Statistical analyses
SPSS (Version 25.0), GraphPad Prism (Version 9.5.0), and R (Version 4.3.0) were used for data analysis. Univariate analysis was performed for all variables using SPSS. Categorical variables were presented as percentages and compared using a chi-square test. Continuous variables perform a Kolmogorov-Smirnov test, The T-test was used for normal distribution, and the Mann-Whitney U was used for non-normal distribution. The correlation between LVMI and other variables was analyzed using Spearman correlation analysis. Depending on whether LVH or not, PCA was performed on a dataset containing continuous variables using R to reduce variable number. Lipid quartiles were treated as a categorical variable, with the lowest quartile as the reference category. The logistic regression test was performed to investigate the correlation between lipids and LVH using Graphpad. Three adjusted models were constructed to reduced confounders. Model I adjusted for age and income, and model II further adjusted for hypertension, alcohol consumption history, and smoking history. Model III was further adjusted for waist circumference and estimated glomerular filtration rate (eGFR). ROC curves were used to analyze the sensitivity and heterogeneity of the model and calculate the cut-off values. P < 0.05 were considered statistically significant.
Sensitivity analysis
A series of stratified analyses were conducted to evaluate the potential modification of classical risk factors, namely gender and HbA1c. Additionally, BMI adjustments will be made to mitigate the confounding effects of metabolic syndrome. Considering hypertension is an independent risk factor for LVH, its confounding effect will be further examined in the subgroup analysis stratified by hypertension (HTN).
Results
Comparison of characteristics of the LVH and Non-LVH group
Univariate analysis was performed for all variables based on the presence or absence of LVH, and the results are presented in Table 1. A significant increase in TC, TG, Non-HDL-C, and TC/HDL-C levels was observed in the LVH group when compared to the non-LVH group (P < 0.001) (Fig. 2). However, compared to the non-LVH group, patients with LVH group exhibited a significant decrease in HDL-C levels (P < 0.01). The two groups had no significant differences regarding LDL-C, TG/HDL-C, and LDL-C/HDL-C.
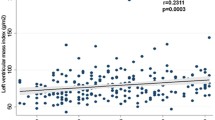
Correlation between LVH and potential risk factors
The Spearman-correlation analysis revealed positive correlations between LVMI and age (r = 0.18, P = 0.001), alcohol consumption history(r = 0.07, P = 0.001), hypertension history(r = 0.52, P = 0.001), eGFR(r = 0.35, P = 0.001), TC(r = 0.57, P = 0.001), Non-HDL-C (r = 0.59, P = 0.001), TG(r = 0.72, P = 0.001), TC/HDL-C ratio(r = 0.44, P = 0.001), and Non-HDL-C/HDL-C ratio(r = 0.31, P = 0.001). Conversely, negative correlations were observed with income(r=-0.6, P = 0.001), smoking history(r=-0.09, P = 0.001), waist circumstance(r=-2.2, P = 0.03), LDL-C(r=-0.35, P = 0.001), HDL-C(r=-0.44, P = 0.001), TG/HDL-C (r=-0.5, P = 0.001), and LDL-C/HDL-C(r=-0.6, P = 0.001) (Table 2).
PCA was conducted with all continuous variables to reduce the dimensionality potentially influencing LVH; the results indicated that LVH and non-LVH populations show significant separation in the principal component space. The first principal component explained 36.8% of the variance in whether LVH occurs, suggesting that this component was the most important in distinguishing between the two groups (Fig. 3A). In the first principal component, the variables making significant contributions were the TC/HDL-C ratio, Non-HDL-C/HDL-C ratio, TG/HDL-C ratio, LDL-C/HDL-C ratio, and Non-HDL-C, each contributing around 15%. The contribution of HDL-C was slightly lower but still close to 15%, indicating it also significantly contributed to the first principal component. The contributions of LDL-C were relatively small. These results suggested lipid profile were essential in distinguishing individuals with and without LVH (Fig. 3B).
Relationship between the levels of lipids and LVH
Univariate analysis, correlation analysis, and PCA results showed a moderate correlation between lipid levels and LVMI. Participants were categorized into quartiles based on their lipid levels. In the unadjusted model, participants in the highest quartile, as compared to those in the lowest quartile, exhibited a higher risk of LVH in the TC, Non-HDL-C, TG, TC/HDL-C ratio, Non-HDL-C/HDL-C ratio, and TG/HDL-C ratio groups (TC, OR = 2.9646, 95%CI: 2.0868–4.2115; Non-HDL-C, OR = 2.833, 95%CI: 1.982–4.049; TG, OR: 1.908, 95%CI: 1.367–2.661; TC/HDL-C, OR = 2.2182, 95%CI: 1.5445–3.1856; Non-HDL-C/HDL-C, OR = 2.1952, 95%CI: 1.5532–3.1025; TG/HDL-C, OR = 1.9166, 95%CI: 1.3831–2.6558) (Fig. 4). Adjusting for confounding factors: Model I was adjusted for age and income (Fig. 5); Model II further adjusted for hypertension, alcohol history, and smoking history (Fig. 6); Model III additionally adjusted for waist circumference and eGFR (Fig. 7). The results of Model III indicated that TC (OR = 2.773, 95%CI: 1.805–4.26), Non-HDL-C (OR = 2.74, 95%CI: 1.7723–4.236), TC/HDL-C ratio (OR = 2.237, 95%CI: 1.445–3.463), Non-HDL-C/HDL-C ratio (OR = 2.357, 95%CI: 1.548–3.588), TG/HDL-C ratio (OR = 1.513, 95%CI: 1.02–2.245) adjusted for confounding factors, the risk of LVH in participants in the highest quartile is increased compared to those in the lowest quartile.
Discrimination of lipids on LVH
The ROC curve analysis revealed the predictive ability of blood lipid profile for LVH (Fig. 8), with Non-HDL-C (AUC = 0.6109) exhibiting the highest area under the curve, followed by TC (AUC = 0.6084), and the weakest predictor being TG/HDL-C ratio (AUC = 0.5787). Youden’s index was utilized to identify the best threshold value of 4.9 for TC and 3.575 for Non-HDL-C in predicting LVH, with a specificity of 47.74% and a sensitivity of 74.4%, a specificity of 50.52% and a sensitivity of 70.86%, respectively (Table 3).
Sensibility analysis
After further adjustment for sex and HbA1c, the results remained consistent with those before adjustment (Supplement 1). Similarly, after adjusting for BMI, the results remained consistent (Supplement 2). Upon stratification analysis for hypertension, the results were consistent among hypertensive patients (Supplement 3).
Discussion
This study is the first to delve into the relationship between lipid components such as TC, Non-HDL-C, TG, TC/HDL-C ratio, Non-HDL-C/HDL-C ratio, TG/HDL-C ratio, and LVH in non-diabetic populations. Our result showed that Non-HDL-C, TC, TC/HDL-C ratio, Non-HDL-C/HDL-C ratio, and TG/HDL-C ratio can serve as independent risk factors for predicting the preservation of LVH in non-diabetic individuals. Additionally, Non-HDL-C and TC can be utilized as predictive markers due to their higher area beneath the curve. Furthermore, this correlation exhibited notable strength and consistency across correction groups for gender and HbA1c, BMI correction group, and stratified analysis of hypertension.
LVH, characterized by thickening of the myocardial wall of the left ventricle or dilation of the left ventricular chamber, poses a significant risk, with individuals displaying consistently high LVH showing the highest mortality risk [16]. Early detection and intervention and reducing the independent risk factors for LVH can serve as early preventive and intervention measures for the disease [18, 20]. Hypertension, diabetes, and renal insufficiency are major known risk factors for LVH [21]. A study in Mauritius found a higher prevalence of LVH among individuals with hypertension [22]. In pre-dialysis patients, the ratio of HDL-C to c-reactive protein and LVMI have been linked to baseline renal function and have shown an independent correlation with the progression of chronic kidney disease [23]. Additionally, African Americans with non-glomerular chronic kidney disease showed a higher prevalence of ambulatory hypertension and increased LVMI [24].
LVH is characterized by progressive impairment in β-oxidation, resulting in dysregulated fatty acid oxidation and significant metabolic remodeling of the heart [25]. Several studies suggest that alterations in lipid profile play a role in the pathophysiology of LVH. However, a consensus regarding the relationship between dyslipidemia and LVH is yet to be reached. Elevated HDL-C levels in mice models have been shown to impede LVH progression, evidenced by reduced left ventricular weight in mice fed a high-fat diet [26]. Change in leptin-signal transducer and activator of transcription three pathway signaling is related to the occurrence of LVH in Rats [27]. While drug interventions targeting lipid profile have shown promise in alleviating LVH by reducing TC, TG, and LDL-C while increasing HDL-C, the exact relationship between lipid regulation and LVH improvement remains uncertain [28]. Evidence suggests that individuals with dyslipidemia, defined by non-traditional lipid indices such as high atherosclerosis index and high TC/HDL-C, along with hypertension, are at higher risk of developing LVH [29]. A 7-year longitudinal and mediation study on increased lipids with risk of worsening cardiac damage in 1595 adolescents recognized that increased TC, Non-HDL-C, and TG were associated with worsening diastolic function and higher LV filling pressure [30]. In non-diabetic patients, the elevated TG in males with hypertension is independently associated with LVH [31]. This may be related to high TG causing myocardial steatosis, leading to left ventricular hypertrophy [32]. Increased TG/HDL-C ratio in obese children has been associated with eccentric LVH development [33]. The uncertainty of the effect of blood lipids on LVH may be related to insulin resistance and abnormal blood pressure caused by metabolic syndrome caused by dyslipidemia [27].
Furthermore, the most significant discovery in this study is that a comprehensive lipid profile has varying degrees of impact on the increase in LVH in the non-diabetic population. While lipids are affected by factors such as glucose metabolism, insulin resistance, and obesity, their influence on LVH remains notable [34]. Meanwhile, due to the variety of lipid types, they become an undeniable independent influencing factor in LVH. This study provides new evidence for the direct correlation between blood lipids and LVH and a new direction for managing and treating this disease.
Study strengths and limitations
This study is the first to investigate the risk determinant linked to LVH in a non-diabetic Sierra Leone population. PCA was used to determine the relative importance of blood lipids in the study, an innovation. Multiple corrections were performed to remove confounding factors and demonstrate the correlation between lipids and LVH. But it has some limitations. First, data focuses on individuals in Africa, which is constricted. It is better to enlarge samples and include other regions. Second, if participants are tracked and followed up, monitoring blood lipids will provide a more comprehensive understanding of the impact of blood lipids on LVH. Finally, conducting lipidomics analysis on the population to focus on the effect of the lipid profile on LVH would be even more convincing.
Conclusion
Lipid profile, represented by TC, Non-HDL-C, TC/HDL-C, Non-HDL-C/HDL-C ratio, and TG/HDL-C ratio, are independent risk factors of LVH in non-diabetic people. In addition, Non-HDL-C, with a cutoff value of 3.575, and TC, with a cutoff value of 4.9, were found to be an essential indicator for predicting the prevalence LVH disease with specific predictive values.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- BMI:
-
Body mass index
- eGFR:
-
Estimated glomerular filtration rate
- FPG:
-
Fasting blood glucose
- HbA1c:
-
Glycated hemoglobin
- HDL:
-
C-High-density lipoprotein
- HF:
-
Heart failure
- LDL:
-
C-Low-density lipoprotein cholesterol
- LVH:
-
Left ventricular hypertrophy
- LVMI:
-
Left Ventricular Mass Index
- Non:
-
HDL-C-Non-high-density lipoprotein
- PCA:
-
Principal component analysis
- TC:
-
Total cholesterols
- TG:
-
Triglycerides
References
Martin SS, Aday AW, Almarzooq ZI, et al. 2024 Heart Disease and Stroke statistics: a report of US and Global Data from the American Heart Association. Circulation. 2024;149(8):e347–913.
Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GM, Coats AJ. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. 2022;118(17):3272–87.
Myokines and Heart Failure: Challenging Role in Adverse Cardiac Remodeling, Myopathy, and Clinical Outcomes - Berezin – 2021 - Disease Markers - Wiley Online Library. Accessed July 8. 2024. https://onlinelibrary.wiley.com/doi/full/https://doi.org/10.1155/2021/6644631
Chudý M, Goncalvesová E. Prediction of left ventricular reverse remodelling: a mini review on clinical aspects. Cardiology. 2022;147(5–6):521–8.
Feng P, Huang Y, Wang S, et al. Analysis of the associations between obesity indices and left ventricular mass. Cardiology. 2019;141(4):183–9.
Hou W, Wang Z, Huang J, et al. Early diagnostic and prognostic value of myocardial strain derived from cardiovascular magnetic resonance in patients with cardiac amyloidosis. Cardiovasc Diagn Ther. 2023;13(6):979.
Rouhana S, Farah C, Roy J, et al. Early calcium handling imbalance in pressure overload-induced heart failure with nearly normal left ventricular ejection fraction. Biochim Biophys Acta BBA-Mol Basis Dis. 2019;1865(1):230–42.
The heart, a secondary organ in the control of blood circulation - Furst - Experimental Physiology - Wiley Online Library. Accessed July 8. 2024. https://physoc.onlinelibrary.wiley.com/doi/full/10.1113/EP091387
Schwinger RH. Pathophysiology of heart failure. Cardiovasc Diagn Ther. 2021;11(1):263.
Dhalla NS, Mota KO, de Vasconcelos CML, Adameova A. Behavior of Hypertrophied Right ventricle during the development of left ventricular failure due to myocardial infarction. Int J Mol Sci. 2024;25(5):2610.
Implication of Different ECG Left Ventricular Hypertrophy in Patients Undergoing Transcatheter Aortic Valve Replacement | Journal of the American Heart Association. Accessed July 8. 2024. https://www.ahajournals.org/doi/full/https://doi.org/10.1161/JAHA.121.023647
Sayin BY, Oto A. Left ventricular hypertrophy: etiology-based therapeutic options. Cardiol Ther. 2022;11(2):203–30.
Hookana I, Holmström L, Eskuri MAE, et al. Characteristics of women with ischemic sudden cardiac death. Ann Med. 2023;55(2):2258911.
Chetty RR, Pillay S. Electrocardiogram (ECG) diagnosis of left ventricular hypertrophy and its associations in patients living with diabetes. Indian J Endocrinol Metab. 2022;26(5):465–70.
Huang X, Deng K, Qin J, et al. Association between lipid profiles and left ventricular hypertrophy: new evidence from a retrospective study. Chin Med Sci J. 2022;37(2):103–17.
Singh GK, McClenaghan C, Aggarwal M, et al. A unique high-output Cardiac Hypertrophy phenotype arising from low systemic vascular resistance in Cantu Syndrome. J Am Heart Assoc. 2022;11(24):e027363.
Yeung AM, Huang J, Pandey A, et al. Biomarkers for the diagnosis of heart failure in people with diabetes: a consensus report from Diabetes Technology Society. Prog Cardiovasc Dis. 2023;79:65–79.
Wong ND, Budoff MJ, Ferdinand K, et al. Atherosclerotic cardiovascular disease risk assessment: an American Society for Preventive Cardiology clinical practice statement. Am J Prev Cardiol. 2022;10:100335.
Russell JBW, Koroma TR, Sesay S, et al. Burden of cardiometabolic risk factors and preclinical target organ damage among adults in Freetown, Sierra Leone: a community-based health-screening survey. BMJ Open. 2023;13(5):e067643.
Zhou D, Huang Y, Cai A, et al. Longitudinal study of left ventricular mass index trajectories and risk of mortality in hypertension: a cohort study. J Am Heart Assoc. 2023;12(9):e028568.
Nitta K, Iimuro S, Imai E, et al. Risk factors for increased left ventricular hypertrophy in patients with chronic kidney disease: findings from the CKD-JAC study. Clin Exp Nephrol. 2019;23:85–98.
Taki H, Tuomilehto J, Zimmet P, et al. Left ventricular hypertrophy: an ECG-based study of prevalence and risk factors in a multiethnic population. Open Heart. 2023;10(2):e002495.
Tang L, Li S, Guo X, et al. Combinative predictive effect of left ventricular mass index, ratio of HDL and CRP for progression of chronic kidney disease in non-dialysis patient. Int Urol Nephrol. 2024;56(1):205–15.
Sgambat K, Roem J, Brady TM, et al. Social determinants of cardiovascular health in African American children with CKD: an analysis of the chronic kidney disease in children (CKiD) study. Am J Kidney Dis. 2021;78(1):66–74.
Pal N, Acharjee A, Ament Z et al. Metabolic profiling of aortic stenosis and hypertrophic cardiomyopathy identifies mechanistic contrasts in substrate utilisation. bioRxiv. Published online 2019:715680.
Martins ÂM, Silva Sarto DAQ, de Caproni K. Grape juice attenuates left ventricular hypertrophy in dyslipidemic mice. PLoS ONE. 2020;15(9):e0238163.
Combined superposition effect of hypertension and dyslipidemia on left ventricular hypertrophy - Zhang – 2022 - Animal Models and Experimental Medicine - Wiley Online Library. Accessed July 4. 2024. https://onlinelibrary.wiley.com/doi/full/https://doi.org/10.1002/ame2.12249
Mercurio V, Pucci G, Bosso G, et al. A nutraceutical combination reduces left ventricular mass in subjects with metabolic syndrome and left ventricular hypertrophy: a multicenter, randomized, double-blind, placebo-controlled trial. Clin Nutr. 2020;39(5):1379–84.
Chuang SM, Liu SC, Leung CH, Lee YT, Chien KL. High left ventricular mass associated with increased risk of incident diabetes. Sci Rep. 2024;14(1):250.
Li Q. Using metabolomics to Profile older individuals with Frailty and Cardiac Dysfunction. Hong Kong University of Science and Technology (Hong Kong); 2020.
Pietri P, Georgiopoulos G, Tsiachris D, et al. Triglycerides are related to left ventricular mass in hypertensive patients independently of other cardiometabolic risk factors: the effect of gender. Sci Rep. 2020;10(1):13253.
Bednarski TK, Duda MK, Dobrzyn P. Alterations of lipid metabolism in the heart in spontaneously hypertensive rats precedes left ventricular hypertrophy and cardiac dysfunction. Cells. 2022;11(19):3032.
Bjelakovic B, Stefanutti C, Vukovic V, et al. Lipid profile and left ventricular geometry pattern in obese children. Lipids Health Dis. 2020;19:1–7.
Kojta I, Chacińska M, Błachnio-Zabielska A. Obesity, bioactive lipids, and adipose tissue inflammation in insulin resistance. Nutrients. 2020;12(5):1305.
Funding
This work was supported by a grant from the Health Commission Science and Technology Plan of Heilongjiang Province (20230303060318) to Yuanxin Xu.
Author information
Authors and Affiliations
Contributions
YX contributed to conceptualization, data curation, formal analysis, visualization, and writing original draft. YCJ contributed to validation, visualization, and software. LX contributed to investigation, WZ and ZZ contributed to methodology. YQ contributed to project administration, resources, supervision and writing review and editing. HK and SY contributed to funding acquisition and final writing review and editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
In the previously published article, all participants signed informed consent forms.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, Y., Jiang, Y.C., Xu, L. et al. Independent risk factors of left ventricular hypertrophy in non-diabetic individuals in Sierra Leone - a cross-sectional study. Lipids Health Dis 23, 259 (2024). https://doi.org/10.1186/s12944-024-02232-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02232-8