Abstract
Background
Observational studies have suggested an association between birth weight and type 2 diabetes mellitus, but the causality between them has not been established. We aimed to obtain the causal relationship between birth weight with T2DM and quantify the mediating effects of potential modifiable risk factors.
Methods
Two-step, two-sample Mendelian randomization (MR) techniques were applied using SNPs as genetic instruments for exposure and mediators. Summary data from genome-wide association studies (GWAS) for birth weight, T2DM, and a series of fatty acids traits and their ratios were leveraged. The inverse variance weighted (IVW) method was the main analysis approach. In addition, the heterogeneity test, horizontal pleiotropy test, Mendelian randomization pleiotropy residual sum and outlier (MR-PRESSO) test, and leave-one-out analysis were carried out to assess the robustness.
Results
The IVW method showed that lower birth weight raised the risk of T2DM (β: −1.113, 95% CI: −1.573 ∼ −0.652). Two-step MR identified 4 of 17 candidate mediators partially mediating the effect of lower birth weight on T2DM, including ratio of polyunsaturated fatty acids to monounsaturated fatty acids (proportion mediated: 7.9%), ratio of polyunsaturated fatty acids to total fatty acids (7.2%), ratio of omega-6 fatty acids to total fatty acids (8.1%) and ratio of linoleic acid to total fatty acids ratio (6.0%).
Conclusions
Our findings supported a potentially causal effect of birth weight against T2DM with considerable mediation by modifiable risk factors. Interventions that target these factors have the potential to reduce the burden of T2DM attributable to low birth weight.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is a clinical syndrome primarily characterized by a disturbance in glucose metabolism, which comprises a significant burden for public health. According to a recent systematic analysis, the global age-standardised prevalence of T2DM was 5.9% (95% uncertainty interval [UI] 5.5–6.3) in 2021. By 2050, the rate is estimated to reach 9.5% (9.0-9.9), affecting more than 1.27 billion (1.19–1.35) people [1]. T2DM is the result of a complex interaction between genetic and environmental factors, including dietary intake. Identification of potential pathogenic risk factors would help guide the prevention of the disease.
The fetal development in utero contributes to susceptibility to T2DM, as suggested by the Developmental Origin of Health and Disease (DOHaD) theory. This theory proposes that major risk factors for many adult diseases are established during fertilization, embryonic, fetal, and neonatal stages [2]. Previous studies have indicated that low birth weight is associated with an increased risk of T2DM compared to normal birth weight [3,4,5]. However, the mechanisms underlying the relationship between birth weight and T2DM remain unclear. Xiaoqiong Zhu et al. [6] demonstrated that fatty acids are risk factors for T2DM. Researchers have reported that fatty acids can regulate gene expression by altering epigenetic mechanisms, leading to either positive or negative outcomes [7, 8]. Based on these facts, we hypothesize that birth weight has a causal relationship with T2DM and glycemic quantitative traits (such as fasting glucose, fasting insulin, HbA1c, and two-hour glucose) through mediating factors (fatty acids traits) (Fig. 1).
Classification of fatty acids. Abbreviations: AA, arachidonic acid; DHA, docosahexaenoic acid; DTA, docosatetraenoic acid; EDA, eicosadienoic acid; GLA, gamma-linolenic acid; LA, linoleic acid; MUFA, monounsaturated fatty acid; Omega-3 FA, omega-3 fatty acid; Omega-6 FA, omega-6 fatty acid; PUFA, polyunsaturated fatty acid; SFA, saturated fatty acid; TFA, total fatty acid; UFA, unsaturated fatty acid
Mendelian randomization (MR) is an epidemiological method that uses genetic variants as instrumental variables (IVs) to investigate the causal effects of exposures on disease outcomes [9, 10]. MR is less susceptible to confounding, measurement errors, and reverse causation compared to observational epidemiologic studies because genetic variants are randomly assigned at conception. These strengths also apply to mediation analysis. Previous MR studies suggested a potential causal relationship between birth weight and T2DM. However, these studies did not assess the potential mediators [11,12,13]. Therefore, we conducted an MR analysis to assess the impact of birth weight on T2DM and quantify the role of fatty acids traits as mediators.
Methods
Study design
Overview of the MR study design. Abbreviations A-FABP, fatty acid-binding protein, adipocyte levels; bisallylic groups/TFA ratio, ratio of bisallylic groups to total fatty acids; DHA, docosahexaenoic acid levels; DHA/TFA ratio, ratio of docosahexaenoic acid to total fatty acid levels; LA, linoleic acid levels; LA/TFA ratio, ratio of linoleic acid to total fatty acids; MUFA, monounsaturated fatty acid levels; MUFA/TFA ratio, ratio of monounsaturated fatty acids to total fatty acids; Omega-3 FA, omega-3 fatty acid levels; Omega-3/TFA ratio, ratio of omega-3 fatty acids to total fatty acids; Omega-6 FA, omega-6 fatty acid levels; Omega-6/Omega-3 FA ratio, ratio of omega-6 fatty acids to omega-3 fatty acids; Omega-6/TFA ratio, ratio of omega-6 fatty acids to total fatty acids; PUFA, polyunsaturated fatty acid levels; PUFA/MUFA ratio, ratio of polyunsaturated fatty acids to monounsaturated fatty acids; PUFA/TFA ratio, ratio of polyunsaturated fatty acids to total fatty acids; SFA, saturated fatty acid levels; SFA/TFA ratio, ratio of saturated fatty acids to total fatty acids; TFA, total fatty acid levels
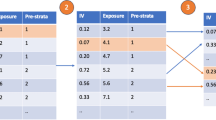
We reported the MR study in adherence to the Strengthening the Reporting of Observational Studies in Epidemiology using Mendelian Randomization (STROBE-MR). In MR analysis, we extracted single nucleotide polymorphisms (SNPs) from the GWAS database as genetic IVs to clarify the causal association between risk factors and outcomes. MR analysis can yield valid causal estimates if the following assumptions are met: [1] the IVs must be significantly closely related to exposures; [2] the IVs must be free of confounders; and [3] the IVs must be unrelated to the outcomes and only affect the outcomes through the exposure (Fig. S1). Two-sample MR analyses were first performed to assess the associations between birth weight and T2DM, and two-step MR analysis was then performed to investigate the mediating effects of fatty acids traits on these associations (Fig. 2).
Ethics committee approval and participant informed consent were obtained in the original studies.
Data sources
SNPs associated with birth weight were obtained from UK Biobank, which contained 261,932 participants. For each birth weight instrument, the genetic effect of the corresponding SNP on T2DM was obtained from a GWAS study with a total of 298,957 Europeans (48,286 diabetes cases and 250,671 controls) [14]. Glycemic quantitative traits (fasting glucose, fasting insulin, HbA1c, and two-hour glucose) were also collected as secondary outcomes. Finally, the summary statistics for intermediate phenotypes (fatty acids) were selected.
All the GWAS summary data applied in the present analysis can be obtained from the IEU open GWAS project (https://gwas.mrcieu.ac.uk/). The above GWAS data are from the European origin population, and their information is shown in Table 1.
Instrumental variable selection and data harmonization
For all analyses, genetic instruments with p-value < 5 × 10− 8 were defined as SNPs. In addition, we selected independent SNPs according to the removal of linkage disequilibrium (LD, R2 > 0.001 and within 10,000 kb). We calculated the F-statistic to quantify the strength of associations between genetic IVs and exposure, and discarded those with an F statistic < 10. The F statistic was calculated using the following formula: F = R2 (N − K − 1)/(K (1 − R2). R2 was calculated using the formula R2 = (2 × EAF × (1 − EAF) × β2)/[(2 × EAF × (1 − EAF) × β2) + (2 × EAF × (1 − EAF) × N × SE2)], where R2, N, EAF, β, SE, and K refer to the cumulative explained variance of selected SNPs in the exposure, the sample size, the effect allele frequency, the estimated effect on the exposure, the standard error of the estimated effect, and the number of IVs, respectively.
MR analyses and mediation analysis
We used the inverse variance weighted (IVW) method as the principal MR analytical approach; due to its high statistical power when the selected IVs were valid [15]. The MR-Egger [16], weighted median method, simple mode, weighted mode, and robust adjusted profile score (RAPS) were used in the two-sample MR analyses as complementary approaches to obtain MR estimates.
Two-sample MR was conducted to estimate the overall effect of birth weight on diabetes (β0) and the effect of birth weight on each mediator (β1) using publicly available GWAS. We further carried out multivariable MR (MVMR) to assess the effect of each mediator on diabetes (β2), adjusting for birth weight.
The total effect of birth weight was decomposed into direct (not acting through the mediators) and indirect (acting through the mediators) effects. The indirect effect of each mediator was calculated by the product of coefficients method (β1*β2) [17]. And the direct effects were estimated by subtracting the indirect effect of birth weight from the total effect. Then we calculated the proportion of the mediated as indirect effect divided by total effect. The 95% confidence intervals were calculated using the delta method.
Sensitivity analyses
To evaluate the robustness of the findings, several sensitivity analyses were conducted. Firstly, the presence of heterogeneity was evaluated using Cochran’s Q statistic (MR-IVW) and Rucker’s Q statistic (MR Egger). Secondly, we used MR-Egger regression intercept test to assess the horizontal pleiotropy of valid IVs. Thirdly, the MR-PRESSO method detected and excluded for outliers, thereby eliminating detected pleiotropy. Finally, a leave-one-out (LOO) sensitivity analysis was conducted by sequentially omitting one SNP at a time to evaluate the possibility of results being driven by a single SNP [18].
The adjusted p-value threshold was set to 0.05 using the Benjamini-Hochberg (BH) method [19]. All statistical analyses were conducted using the TwoSampleMR (version 0.5.8, https://mrcieu.github.io/TwoSampleMR) and MRPRESSO (version 1.0) packages in R (version 4.2.2).
Results
Total effect of birth weight on T2DM and glycemic quantitative traits
We found strong evidence of a causal relationship between birth weight and T2DM. Figure 3a illustrates the overall effect of birth weight on T2DM, fasting glucose, fasting insulin, HbA1c, and two-hour glucose. The IVW method showed that lower birth weight was associated with a higher risk of T2DM (β: −1.113, 95% CI: −1.573 ∼ −0.652), higher fasting insulin (β: −0.080, −0.108 ∼ −0.052) and higher two-hour glucose (β: −0.250, −0.360 ∼ −0.140).
Horizontal pleiotropy was detected for fasting glucose (ER intercept = 0.003; P = 0.028) and HbA1c (ER intercept = 0.008; P = 0.038). Potentially pleiotropic SNPs were excluded using MR-PRESSO. After removing 13 outliers (rs7854962, rs76895963, rs74932341, rs351776, rs329121, rs2934844, rs28378473, rs2747503, rs2159778, rs1522811, rs13266210, rs11708067 and rs10769199), we found that a lower birth weight indicated higher fasting glucose (β: −0.061, −0.091 ∼ −0.032), and no horizontal pleiotropy was detected (ER intercept = 0.001; P = 0.384). However, ER still indicated significant pleiotropy (ER intercept = 0.008; P = 0.048) for HbA1c after removing rs72790949, rs2551402, rs2395668, rs1776270, rs11222084(Table S14).
Effect of birth weight on fatty acids traits
Genetically predicted each 1-SD lower birth weight was associated with higher TFA (β: −0.101, −0.160 ∼ −0.042), SFA (β: −0.096, −0.151 ∼ −0.041) and MUFA (β: −0.117, −0.175 ∼ −0.058). Besides, IVW results also showed that genetically predicted each 1-SD decrease in birth weight was associated with lower PUFA/MUFA ratio (β: 0.107, 0.056 ∼ 0.159), PUFA/TFA ratio (β: 0.095, 0.045 ∼ 0.145), Omega-6/TFA ratio (β: 0.106, 0.052 ∼ 0.160) and LA/TFA ratio (β: 0.082, 0.033 ∼ 0.132), but higher MUFA/TFA ratio (β: −0.109, −0.160 ∼ −0.057) (Fig. 4).
In addition, reverse MR suggested that there was no evidence for a causal effect of fatty acids traits on birth weight. (Table S12) The presence of heterogeneity and pleiotropic effect are shown in Table S14-16.
MR estimates derived from the IVW method to assess the causal effect of birth weight on fatty acids traits. A-FABP, fatty acid-binding protein, adipocyte levels; bisallylic groups/TFA ratio, ratio of bisallylic groups to total fatty acids; CI, confidence interval; DHA, docosahexaenoic acid levels; DHA/TFA ratio, ratio of docosahexaenoic acid to total fatty acid levels; LA, linoleic acid levels; LA/TFA ratio, ratio of linoleic acid to total fatty acids; MUFA, monounsaturated fatty acid levels; MUFA/TFA ratio, ratio of monounsaturated fatty acids to total fatty acids; Omega-3 FA, omega-3 fatty acid levels; Omega-3/TFA ratio, ratio of omega-3 fatty acids to total fatty acids; Omega-6 FA, omega-6 fatty acid levels; Omega-6/Omega-3 FA ratio, ratio of omega-6 fatty acids to omega-3 fatty acids; Omega-6/TFA ratio, ratio of omega-6 fatty acids to total fatty acids; PUFA, polyunsaturated fatty acid levels; PUFA/MUFA ratio, ratio of polyunsaturated fatty acids to monounsaturated fatty acids; PUFA/TFA ratio, ratio of polyunsaturated fatty acids to total fatty acids; SFA, saturated fatty acid levels; SFA/TFA ratio, ratio of saturated fatty acids to total fatty acids; TFA, total fatty acid levels
Effects of fatty acids traits on T2DM and glycemic quantitative traits
In MVMR, TFA (β: −0.839, 95% CI: −1.315 ∼ −0.364), SFA (β: −0.930, −1.404 ∼ −0.455), and MUFA (β: −0.864, −1.353 ∼ −0.375) were negatively associated with T2DM after adjusting for birth weight. Besides, lower MUFA/TFA ratio (β: −0.852, −1.332 ∼ −0.372), PUFA/MUFA ratio (β: −0.819, −1.301 ∼ −0.336), PUFA/TFA ratio (β: −0.846, −1.344 ∼ −0.349), Omega-6/TFA ratio (β: −0.850, −1.349 ∼ −0.350), and LA/TFA ratio (β: −0.807, −1.319 ∼ −0.296) were in relation to an increased risk of T2DM after adjusting for birth weight (Fig. 5a).
Genetically determined each 1-SD higher fatty acids traits with adjustment for birth weight showed consistently causal associations with fasting glucose, fasting insulin and two-hour glucose (Fig. 5b).
a MR estimates derived from the IVW method to assess the causal effect of fatty acids traits on T2DM after adjusting for birth weight. b MR estimates derived from the IVW method to assess the causal effect of fatty acids traits on fasting glucose, fasting insulin and two-hour glucose after adjusting for birth weight. BW, birth weight; CI, confidence interval; LA/TFA ratio, ratio of linoleic acid to total fatty acids; MUFA, monounsaturated fatty acid levels; MUFA/TFA ratio, ratio of monounsaturated fatty acids to total fatty acids; Omega-6/TFA ratio, ratio of omega-6 fatty acids to total fatty acids; OR, odds ratio; PUFA/MUFA ratio, ratio of polyunsaturated fatty acids to monounsaturated fatty acids; PUFA/TFA ratio, ratio of polyunsaturated fatty acids to total fatty acids; SFA, saturated fatty acid levels; TFA, total fatty acid levels
Mediation effects of fatty acids traits on T2DM and glycemic quantitative traits
For the causal effect of birth weight on T2DM, the percentage mediated by PUFA/MUFA ratio, PUFA/TFA ratio, Omega-6/TFA ratio and LA/TFA ratio was 7.9% (95%CI: 1.1%∼14.7%), 7.2% (0.8%∼13.7%), 8.1% (0.9%∼15.2%) and 6.0% (0.2%∼11.7%), respectively. The mediation effects of PUFA/MUFA ratio, PUFA/TFA ratio, Omega-6/TFA ratio and LA/TFA ratio on fasting glucose, fasting insulin, and two-hour glucose were estimated to account for 7.6%∼13.9%. Table 2 shows the mediated effect of birth weight on T2DM, fasting glucose, fasting insulin and two-hour glucose explained by each mediator separately.
Discussion
In this study, we conducted a series of two-sample MR and two-step MR analyses to assess the independent impact of birth weight on T2DM and glycemic quantitative traits, identify potential metabolic mediators and quantify the mediation effects. Our findings provided robust evidence supporting the negative causal effect of birth weight on T2DM. Furthermore, the two-step MR analysis indicated that 4 of 17 candidate mediators were identified to partially mediate the causal effect of low birth weight on T2DM, including PUFA/MUFA ratio, PUFA/TFA ratio, Omega-6/TFA ratio, and LA/TFA ratio. These mediators also exhibited corresponding mediating effects on fasting glucose, fasting insulin, and two-hour glucose. Therefore, interventions targeted at these factors could potentially reduce the risk of T2DM among individuals with low birth weight.
T2DM is a significant societal burden [20, 21]. Our study indicated that a lower birth weight was associated with a higher risk of T2DM, fasting insulin, fasting glucose, and two-hour glucose. A recent systematic review involving 152,084 individuals supported a negative correlation between birth weight and T2DM [22]. However, Tamarra M. James-Todd’s study suggested that low birth weight did not significantly increase the risk of T2DM [23]. The increased incidence of impaired glucose tolerance and T2DM in adulthood with low birth weight can be explained from two perspectives. Firstly, from the genetic aspect, the fetal insulin hypothesis proposes that low birth weight and T2DM in adulthood are two phenotypes of the same gene. The loci that primarily affect pancreatic β-cell function, such as ADCY5 and CDKAL1, show the strongest associations between T2DM risk alleles and lower birth weight. Utilizing genome-wide data, common variants can explain 36% of the negative correlation between birth weight and T2DM. Secondly, we explained this result from the maternal impact. During pregnancy, the mother transmits relevant environmental information (such as nutritional status) to the fetus through the placenta [24]. The Developmental Origins of Health and Disease (DOHaD) suggests that various adverse early-life conditions, including nutrition imbalance, maternal conditions or diseases, maternal chemical exposure, and medication use can lead to vulnerability to later metabolic disorders [25]. Lumey LH’s investigation found that individuals born in famine areas in Ukraine exhibited decreased glucose tolerance about 50 years later [26]. Additionally, low birth weight reflects poor intrauterine nutritional status, which could lead to alterations in pancreatic β-cell structure and function [27], skeletal muscle abnormalities [28], and hypothalamus-pituitary-adrenal axis dysfunction [29], further influencing the occurrence of T2DM.
Infants with low birth weight often experience catch-up growth under nutrient sufficient conditions [30]. Due to parental concerns, they tend to consume more fatty acids, including TFA, SFA, MUFA, PUFA, Omega-3 FA, and Omega-6 FA. However, we observed a decrease in the ratios of PUFA/MUFA, PUFA/TFA, Omega-6/TFA, and LA/TFA, which could be associated with factors such as the types of fatty acids consumed and metabolic processes. When exposed to a metabolic challenge of high-fat overfeeding, low birth weight subjects could lead to peripheral insulin resistance and T2DM, possibly associated with decreased expression of OXPHOS genes and mitochondrial dysfunction [31, 32]. Furthermore, a mouse experiment suggested that catch-up growth in fetuses leads to severe impairment of insulin sensitivity [33].
TFA includes SFA and UFA. High SFA content in diets could adversely affect insulin sensitivity, potentially leading to the development of T2DM [34]. The potential mechanism involves the loss of β-cell fat storage-inducing transmembrane protein 2 (FIT2) and lipid droplet (LD), leading to β cell dysfunction and subsequently causing T2DM [35]. The role of SFA in T2DM remains controversial, with some studies indicating no association [36,37,38]. The lack of correlation between SFA and T2DM is due to the varying effects of SFA from different food sources. Consuming red meat, which is a primary source of SFA in the European and American diet, is associated with a higher risk of T2DM [39]. In contrast, a negative correlation is observed between the consumption of SFA and T2DM when dairy products, low-fat dairy, and cheese are the primary SFA sources [40].
UFA encompasses MUFA and PUFA. The substitution of carbohydrates with MUFA correlates with an increased T2DM (HR 1.10, [95% CI 1.01, 1.19]) [41]. Oleic acid, the most abundant MUFA, is implicated in lipotoxicity of pancreatic β-cells, thereby promoting the progression of T2DM. Islets exposed to oleic acid elevate the expression of PPI, PDX-1, and GLUT2, potentially contributing to increased basal insulin secretion [42]. Additionally, excessive oleic acid intake induces DNA methylation, which most likely accounts for the decrease of glucose-stimulated insulin secretion (GSIS) [43].
Our study indicated a negative correlation between PUFA/SFA and PUFA/MUFA ratios with T2DM. A study exploring complete data on plasma fatty acids from 95,854 participants in the UK Biobank between 2006 and 2010 revealed a positive association of SFA (OR: 1.03) and MUFA (OR: 1.03) with T2DM, while PUFA (OR: 0.62) showed a negative association with T2DM [44]. Substituting dietary SFA with PUFA improved insulin sensitivity within just 5 weeks, thereby decreasing the risk of developing T2DM [45]. Fumiaki et al. [46] suggested that replacing SFA or MUFA with PUFA leads to significant reductions in blood glucose levels. The findings of the previous studies mentioned above are consistent with our results. In animal studies, PUFA primarily enhanced insulin sensitivity in skeletal muscle and adipose tissue, thereby improving glucose homeostasis [47, 48].
In our study, Omega-6/SFA showed a negative correlation with T2DM. Omega-6 fatty acids are a class of PUFA, and their impact on T2DM remains controversial. Specifically, LA and eicosadienoic acid (EDA) exhibit a negative correlation with T2DM, while arachidonic acid (AA) shows no significant correlation. Additionally, gamma-linolenic acid (GLA), dihomo-GLA, docosatetraenoic acid (DTA), and n6-docosapentaenoic acid (n6-DPA) are significantly positively correlated with T2DM [49].
LA, as an essential fatty acid, is the most abundant Omega-6 FA [50]. Studies suggested a negative correlation between LA intake and T2DM [51, 52], although some studies found no significant association [53]. In a multivariable-adjusted pooled analysis, a higher LA/TFA ratio was associated with an overall lower risk of T2DM, which was in agreement with our study [54].
The primary component of vegetable oils is Omega-6 FA, in particular LA. And nuts are nutrition-dense foods, abundant in PUFA and some bioactive compounds, providing benefits for glycemic regulation [55]. Therefore, increasing the proportion of vegetable oils and nuts consumed may be beneficial in preventing T2DM, particularly in individuals with low birth weight.
Our study possesses several strengths. Firstly, to our knowledge, it is the first MR analysis to assess the association between low birth weight with T2DM risk and glycemic traits, exploring fatty acids traits as intermediaries. Secondly, we investigated not only the content of fatty acids but also the ratio of a series of fatty acids in mediating the impact of low birth weight on T2DM. Thirdly, leveraging large-sample GWAS data enables a more reliable assessment of the relationship between risk factors and disease outcomes compared to observational studies at the individual level. Finally, we employed a variety of MR methods, including weighted median regression, MR-Egger method, simple mode, weighted mode, and robust adjusted profile score, and the consistently estimated associations support the robustness of our study findings.
However, our study has some limitations. Firstly, we assessed the linear effect association between birth weight and T2DM using two-sample MR analysis, lacking exploration into non-linear associations [5, 56,57,58]. Secondly, we employed the MVMR method to estimate the individual mediating effects of each fatty acid factor. Nevertheless, interactions among these mediators could exist, complicating the precision of individual effects as one mediator could influence others. Thirdly, a random effect model was adopted, taking into consideration the high heterogeneity. Fourthly, considering the limitations in the GWAS summary data, the MR analyses with age, sex or education stratification are unavailable. Fifthly, it is important to note that MR findings only reflect lifetime exposure levels and cannot easily provide information on acute changes in exposure levels. Lastly, it should be noted that the participants in our study were of European descent, so caution should be exercised when generalizing our results to populations of Asian or African descent.
In conclusion, our results supported a potential causal role of low birth weight in T2DM. Additionally, individual fatty acid mediating effects were modest, while their ratios (PUFA/MUFA ratio, PUFA/TFA ratio, Omega-6/TFA ratio, and LA/TFA ratio) demonstrated substantial mediating effects. Therefore, interventions targeting these factors could significantly alleviate the burden of T2DM associated with low birth weight.
Conclusions
In conclusion, this two-step MR study presented genetic evidence of a causal relationship between low birth weight and T2DM, with PUFA/MUFA ratio, PUFA/TFA ratio, Omega-6/TFA ratio, and LA/TFA ratio serving as mediators. This finding provided novel insights into the underlying mechanisms of the occurrence and development of T2DM and suggested potential avenues for developing preventive and therapeutic strategies.
Data availability
All data used in the current study were obtained from public genome-wide association study summary statistics which were publicly released by genetic consortia. All data is obtained from OpenGWAS (https://gwas.mrcieu.ac.uk/).
Abbreviations
- A-FABP:
-
fatty acid-binding protein adipocyte levels
- bisallylic groups/TFA ratio:
-
ratio of bisallylic groups to total fatty acids
- CI:
-
confidence interval
- DHA:
-
docosahexaenoic acid levels
- DHA/TFA ratio:
-
ratio of docosahexaenoic acid to total fatty acid levels
- GWAS:
-
genome-wide association study
- LA:
-
linoleic acid levels
- LA/TFA ratio:
-
ratio of linoleic acid to total fatty acids
- MUFA:
-
monounsaturated fatty acid levels
- MUFA/TFA ratio:
-
ratio of monounsaturated fatty acids to total fatty acids
- Omega-3 FA:
-
omega-3 fatty acid levels
- Omega-3/TFA ratio:
-
ratio of omega-3 fatty acids to total fatty acids
- Omega-6 FA:
-
omega-6 fatty acid levels
- Omega-6/Omega-3 FA ratio:
-
ratio of omega-6 fatty acids to omega-3 fatty acids
- Omega-6/TFA ratio:
-
ratio of omega-6 fatty acids to total fatty acids
- OR:
-
odds ratio
- PUFA:
-
polyunsaturated fatty acid levels
- PUFA/MUFA ratio:
-
ratio of polyunsaturated fatty acids to monounsaturatedfatty acids
- PUFA/TFA ratio:
-
ratio of polyunsaturated fatty acids to total fatty acids
- SD:
-
standard deviation
- SFA:
-
saturated fatty acid levels
- SFA/TFA ratio:
-
ratio of saturated fatty acids to total fatty acids
- TFA:
-
total fatty acid levels
References
Collaborators GBDD. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of Disease Study 2021. Lancet. 2023;402(10397):203–34.
Barker DJ. The fetal and infant origins of adult disease. BMJ. 1990;301(6761):1111.
Jornayvaz FR, Vollenweider P, Bochud M, Mooser V, Waeber G, Marques-Vidal P. Low birth weight leads to obesity, diabetes and increased leptin levels in adults: the CoLaus study. Cardiovasc Diabetol. 2016;15:73.
Mi D, Fang H, Zhao Y, Zhong L. Birth weight and type 2 diabetes: a meta-analysis. Exp Ther Med. 2017;14(6):5313–20.
Tian G, Guo C, Li Q, Liu Y, Sun X, Yin Z, et al. Birth weight and risk of type 2 diabetes: a dose-response meta-analysis of cohort studies. Diabetes Metab Res Rev. 2019;35(5):e3144.
Zhu X, Chen L, Lin J, Ba M, Liao J, Zhang P, et al. Association between fatty acids and the risk of impaired glucose tolerance and type 2 diabetes mellitus in American adults: NHANES 2005–2016. Nutr Diabetes. 2023;13(1):8.
Gonzalez-Becerra K, Ramos-Lopez O, Barron-Cabrera E, Riezu-Boj JI, Milagro FI, Martinez-Lopez E, et al. Fatty acids, epigenetic mechanisms and chronic diseases: a systematic review. Lipids Health Dis. 2019;18(1):178.
Zhang M, Zhu Y-H, Zhu Z-Q. Research advances in the influence of lipid metabolism on cognitive impairment. Ibrain.n/a(n/a).8.
Emdin CA, Khera AV, Kathiresan S, Mendelian Randomization. JAMA. 2017;318(19):1925–6.
Xiong Y, Zhang F, Zhang Y, Wang W, Ran Y, Wu C et al. Insights into modifiable risk factors of erectile dysfunction, a wide-angled mendelian randomization study. J Adv Res. 2023.
Group B-GSW, Huang T, Wang T, Zheng Y, Ellervik C, Li X, et al. Association of Birth Weight with Type 2 diabetes and glycemic traits: a mendelian randomization study. JAMA Netw Open. 2019;2(9):e1910915.
Wang T, Huang T, Li Y, Zheng Y, Manson JE, Hu FB, et al. Low birthweight and risk of type 2 diabetes: a mendelian randomisation study. Diabetologia. 2016;59(9):1920–7.
Zanetti D, Tikkanen E, Gustafsson S, Priest JR, Burgess S, Ingelsson E, Birthweight. Type 2 diabetes Mellitus, and Cardiovascular Disease: addressing the Barker Hypothesis with mendelian randomization. Circ Genom Precis Med. 2018;11(6):e002054.
Mahajan A, Wessel J, Willems SM, Zhao W, Robertson NR, Chu AY, et al. Refining the accuracy of validated target identification through coding variant fine-mapping in type 2 diabetes. Nat Genet. 2018;50(4):559–71.
Lin Z, Deng Y, Pan W. Combining the strengths of inverse-variance weighting and Egger regression in mendelian randomization using a mixture of regressions model. PLoS Genet. 2021;17(11):e1009922.
Burgess S, Thompson SG. Interpreting findings from mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32(5):377–89.
MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614.
Brion MJ, Shakhbazov K, Visscher PM. Calculating statistical power in mendelian randomization studies. Int J Epidemiol. 2013;42(5):1497–501.
Benjamini Y, Hochberg Y. Controlling the false Discovery rate: a practical and powerful Approach to multiple testing. J Royal Stat Soc Ser B: Methodological. 1995;57(1):289–300.
Zhuo X, Zhang P, Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013;45(3):253–61.
Yu YY, Lei D, He Q, Chen W. A cohort study on the relationship between education level and high-risk population of stroke. Ibrain. 2021;7(3):181–91.
Wibaek R, Andersen GS, Linneberg A, Hansen T, Grarup N, Thuesen ACB, et al. Low birthweight is associated with a higher incidence of type 2 diabetes over two decades independent of adult BMI and genetic predisposition. Diabetologia. 2023;66(9):1669–79.
James-Todd TM, Karumanchi SA, Hibert EL, Mason SM, Vadnais MA, Hu FB, et al. Gestational age, infant birth weight, and subsequent risk of type 2 diabetes in mothers: nurses’ Health Study II. Prev Chronic Dis. 2013;10:E156.
Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359(1):61–73.
Hsu CN, Hou CY, Hsu WH, Tain YL. Early-Life origins of metabolic syndrome: mechanisms and preventive aspects. Int J Mol Sci. 2021;22:21.
Lumey LH, Khalangot MD, Vaiserman AM. Association between type 2 diabetes and prenatal exposure to the Ukraine famine of 1932-33: a retrospective cohort study. Lancet Diabetes Endocrinol. 2015;3(10):787–94.
Fowden AL, Hill DJ. Intra-uterine programming of the endocrine pancreas. Br Med Bull. 2001;60:123–42.
Merz KE, Thurmond DC. Role of skeletal muscle in insulin resistance and glucose uptake. Compr Physiol. 2020;10(3):785–809.
Ward AM, Syddall HE, Wood PJ, Chrousos GP, Phillips DI. Fetal programming of the hypothalamic-pituitary-adrenal (HPA) axis: low birth weight and central HPA regulation. J Clin Endocrinol Metab. 2004;89(3):1227–33.
Gat-Yablonski G, Phillip M. Nutritionally-induced catch-up growth. Nutrients. 2015;7(1):517–51.
Brons C, Jacobsen S, Hiscock N, White A, Nilsson E, Dunger D, et al. Effects of high-fat overfeeding on mitochondrial function, glucose and fat metabolism, and adipokine levels in low-birth-weight subjects. Am J Physiol Endocrinol Metab. 2012;302(1):E43–51.
Gillberg L, Perfilyev A, Brons C, Thomasen M, Grunnet LG, Volkov P, et al. Adipose tissue transcriptomics and epigenomics in low birthweight men and controls: role of high-fat overfeeding. Diabetologia. 2016;59(4):799–812.
Pericuesta E, Gutierrez-Arroyo JL, Sanchez-Calabuig MJ, Gutierrez-Adan A. Postnatal Catch-Up Growth Programs Telomere dynamics and glucose intolerance in low Birth Weight mice. Int J Mol Sci. 2021;22(7).
Tierney AC, McMonagle J, Shaw DI, Gulseth HL, Helal O, Saris WH, et al. Effects of dietary fat modification on insulin sensitivity and on other risk factors of the metabolic syndrome–LIPGENE: a European randomized dietary intervention study. Int J Obes (Lond). 2011;35(6):800–9.
Zheng X, Ho QWC, Chua M, Stelmashenko O, Yeo XY, Muralidharan S, et al. Destabilization of beta cell FIT2 by saturated fatty acids alter lipid droplet numbers and contribute to ER stress and diabetes. Proc Natl Acad Sci U S A. 2022;119(11):e2113074119.
Neuenschwander M, Barbaresko J, Pischke CR, Iser N, Beckhaus J, Schwingshackl L, et al. Intake of dietary fats and fatty acids and the incidence of type 2 diabetes: a systematic review and dose-response meta-analysis of prospective observational studies. PLoS Med. 2020;17(12):e1003347.
Gaeini Z, Bahadoran Z, Mirmiran P. Saturated fatty acid intake and risk of type 2 diabetes: an updated systematic review and dose-response Meta-analysis of Cohort studies. Adv Nutr. 2022;13(6):2125–35.
de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015;351:h3978.
Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94(4):1088–96.
Aune D, Norat T, Romundstad P, Vatten LJ. Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr. 2013;98(4):1066–83.
Quality of dietary fat. And genetic risk of type 2 diabetes: individual participant data meta-analysis. BMJ. 2019;367:l5612.
Zhang Y, Xiao M, Niu G, Tan H. Mechanisms of oleic acid deterioration in insulin secretion: role in the pathogenesis of type 2 diabetes. Life Sci. 2005;77(17):2071–81.
Zhou Z, Sun B, Li X, Zhu C. DNA methylation landscapes in the pathogenesis of type 2 diabetes mellitus. Nutr Metab (Lond). 2018;15:47.
Zhuang P, Liu X, Li Y, Li H, Zhang L, Wan X, et al. Circulating fatty acids and genetic predisposition to type 2 diabetes: Gene-Nutrient Interaction Analysis. Diabetes Care. 2022;45(3):564–75.
Summers LK, Fielding BA, Bradshaw HA, Ilic V, Beysen C, Clark ML, et al. Substituting dietary saturated fat with polyunsaturated fat changes abdominal fat distribution and improves insulin sensitivity. Diabetologia. 2002;45(3):369–77.
Imamura F, Micha R, Wu JH, de Oliveira Otto MC, Otite FO, Abioye AI, et al. Effects of Saturated Fat, Polyunsaturated Fat, Monounsaturated Fat, and Carbohydrate on glucose-insulin homeostasis: a systematic review and Meta-analysis of Randomised Controlled feeding trials. PLoS Med. 2016;13(7):e1002087.
Calonne J, Marcelino H, Veyrat-Durebex C, Scerri I, Dulloo AG. Countering impaired glucose homeostasis during catch-up growth with essential polyunsaturated fatty acids: is there a major role for improved insulin sensitivity? Nutr Diabetes. 2021;11(1):4.
Lamping KG, Nuno DW, Coppey LJ, Holmes AJ, Hu S, Oltman CL, et al. Modification of high saturated fat diet with n-3 polyunsaturated fat improves glucose intolerance and vascular dysfunction. Diabetes Obes Metab. 2013;15(2):144–52.
Forouhi NG, Imamura F, Sharp SJ, Koulman A, Schulze MB, Zheng J, et al. Association of Plasma Phospholipid n-3 and n-6 polyunsaturated fatty acids with type 2 diabetes: the EPIC-InterAct case-cohort study. PLoS Med. 2016;13(7):e1002094.
Russo GL. Dietary n-6 and n-3 polyunsaturated fatty acids: from biochemistry to clinical implications in cardiovascular prevention. Biochem Pharmacol. 2009;77(6):937–46.
Schwab U, Lauritzen L, Tholstrup T, Haldorssoni T, Riserus U, Uusitupa M et al. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food Nutr Res. 2014;58.
Zong G, Liu G, Willett WC, Wanders AJ, Alssema M, Zock PL, et al. Associations between Linoleic Acid Intake and Incident Type 2 diabetes among U.S. men and women. Diabetes Care. 2019;42(8):1406–13.
Dow C, Mangin M, Balkau B, Affret A, Boutron-Ruault MC, Clavel-Chapelon F, et al. Fatty acid consumption and incident type 2 diabetes: an 18-year follow-up in the female E3N (etude Epidemiologique aupres des femmes de la Mutuelle Generale De l’Education Nationale) prospective cohort study. Br J Nutr. 2016;116(10):1807–15.
Wu JHY, Marklund M, Imamura F, Tintle N, Ardisson Korat AV, de Goede J, et al. Omega-6 fatty acid biomarkers and incident type 2 diabetes: pooled analysis of individual-level data for 39 740 adults from 20 prospective cohort studies. Lancet Diabetes Endocrinol. 2017;5(12):965–74.
Telle-Hansen VH, Gaundal L, Myhrstad MCW. Polyunsaturated fatty acids and Glycemic Control in Type 2 diabetes. Nutrients. 2019;11(5).
Hu C, Mu Y, Wan Q, Qin Y, Hu R, Shi L, et al. Association between birth weight and diabetes: role of body mass index and lifestyle in later life. J Diabetes. 2020;12(1):10–20.
Knop MR, Geng TT, Gorny AW, Ding R, Li C, Ley SH, et al. Birth weight and risk of type 2 diabetes Mellitus, Cardiovascular Disease, and hypertension in adults: a Meta-analysis of 7 646 267 participants from 135 studies. J Am Heart Assoc. 2018;7(23):e008870.
Franks PW, McCarthy MI. Exposing the exposures responsible for type 2 diabetes and obesity. Science. 2016;354(6308):69–73.
Acknowledgements
We are grateful for the suggestions of the editor and anonymous reviewers. We also thank for the open data set OpenGWAS.
Funding
This work was supported by Department of Human Resources and Social Security of Shanxi Province (No.20200043) and the College Students’ Innovative Entrepreneurial Training Plan Program of Shanxi Province (No.20230296 and No. 20230294).
Author information
Authors and Affiliations
Contributions
LMC is responsible for data analysis and article writing. YHW, KYF, QWW, YCZ, ZLL and NW collected and assembled the data. XHZ is responsible for giving constructive suggestions for the revision of the article. All authors have contributed to the interpretation of the results and have critically revised the content of the manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
All data sources in this study were based on publicly available summary-level data, and all the original articles had previously undergone ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cao, L., Wen, Y., Fan, K. et al. Association of birth weight with type 2 diabetes mellitus and the mediating role of fatty acids traits: a two-step mendelian randomization study. Lipids Health Dis 23, 97 (2024). https://doi.org/10.1186/s12944-024-02087-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02087-z