Abstract
Background
Lewy body dementia (LBD) ranks second among prevalent neurodegenerative dementias. Previous studies have revealed associations of serum lipid measures with several neurodegenerative diseases. Nevertheless, the potential connection between serum lipids and LBD remains undetermined. In this study, Mendelian randomization (MR) analyses were carried out to assess the causal relationships of several serum lipid measures with the risk of developing LBD.
Methods
Genome-wide association study (GWAS) data for serum lipids and LBD in European descent individuals were acquired from publicly available genetic summary data. A series of filtering procedures were conducted to identify the genetic variant candidates that are related to serum lipids, including high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG). The causal effects were primarily determined through inverse-variance weighting (IVW)-based analyses.
Results
Neither TG (odds ratio [OR] = 1.149; 95% confidence interval [CI], 0.887–1.489; P = 0.293) nor HDL-C (OR = 0.864; 95% CI, 0.718–1.041; P = 0.124) had causal effects on LBD. However, a causal relationship was identified between LDL-C and LBD (OR = 1.343; 95% CI, 1.094–1.649; P = 0.005), which remained significant (OR = 1.237; 95% CI, 1.015–1.508; P = 0.035) following adjustment for HDL-C and TG in multivariable MR.
Conclusions
Elevated serum LDL-C increases the risk of LBD, while HDL-C and TG have no significant causal effects on LBD.
Similar content being viewed by others
Introduction
LBD patients often exhibit several histopathological and clinical symptoms that are similar to those of both Alzheimer’s disease (AD) and Parkinson’s disease (PD) patients. The lack of specific biomarkers for precise diagnosis frequently leads to misdiagnosis or underdiagnosis of LBD [1]. Currently, there is no curative treatment available for LBD, and the primary focus of clinical management is symptoms alleviation. However, it is important to noted that several pharmacologic agents commonly used for other forms of dementia may actually exacerbate LBD symptoms [2]. As a result, LBD imposes a significant social and economic burden, surpassing that of AD [3]. Given these circumstances, identifying potential risk factors associated with LBD for preventative measures could be a feasible approach to controlling the disease.
HDL-C, LDL-C, and TG are commonly utilized clinical indicators and are readily obtainable. Serum lipids have been shown to be associated with multiple neurodegenerative diseases (e.g., AD [4] and PD [5]). Nevertheless, few studies have examined the relationships among serum lipids and LBD. A case-control study enrolling 65 LBD patients and 110 adult controls revealed associations between LBD development and levels of LDL-C and HDL-C [6]. However, conventional observational studies are inherently flawed due to their nonrandomized designs, making them susceptible to both reverse causality and residual confounding [7]. As of now, there are no large-scale, multicentre randomized controlled trials (RCTs) available. Therefore, based on existing evidence, the exact relationship between serum lipids and LBD cannot be determined.
Mendelian randomization (MR) involves the use of single-nucleotide polymorphisms (SNPs) as genetic variants. Genotype formation, occurring prior to disease onset, is usually unaffected by clinical factors. This characteristic makes MR designs highly reliable, as they are largely independent of reverse causality and confounding factors [8]. As a result, MR designs are broadly utilized to examine the causal relationships among exposures and clinical outcomes [9]. Considering the uncertain relationship between serum lipids and LBD, multivariable MR (MVMR) and univariable MR (UVMR) analyses were performed using summary-level statistics of GWASs. This study assessed causal effects of three different exposures (HDL-C, LDL-C, and TG) on LBD. Findings obtained from this study have the potential to offer novel insights into the risk factors associated with LBD, which can contribute to the improvement of LBD screening, prevention, and the optimization of clinical management strategies for LBD patients.
Materials and methods
Study design
The causal relationships among HDL-C, LDL-C, TG and LBD were evaluated through MR method. The robust design of MR design was built on three fundamental assumptions [10]: (I) strong associations among genetic variants and target exposures; (II) no associations among genetic variants and potential confounding factors; (III) genetic variants influence outcomes exclusively via the exposures of interest.
Sources of GWAS data
The GWAS summary data for HDL-C, LDL-C, and TG in individuals of European descent were obtained from the OpenGWAS database. Exposure GWAS included LDL-C data for 70,814 participants, HDL-C data for 77,409 participants, and TG data for 78,700 participants. Each of the three exposure datasets had approximately 7.89 million SNPs.
LBD GWAS data were obtained from a multicentre case-control study [11] comprising 6618 individuals of European descent, including 2591 LBD patients and 4027 neurologically healthy control individuals. This study includes approximately 7.59 million SNPs. Detailed demographic characteristics, study sites/consortia, diagnostic criteria, and quality control are also available. For more detailed information on the GWAS datasets, please refer to Supplementary Table 1.
Selection of genetic instruments
Multiple steps were executed to identify the eligible genetic variants. First, SNPs associated with three exposure factors (TG, HDL-C, LDL-C) were identified by applying a rigorous threshold of P < 5 × 10− 8. Subsequently, SNPs in linkage disequilibrium (LD, window size = 10,000 kilobase and r2 threshold = 0.001) were discarded. Second, the F statistics were computed to prevent weak instrument involvement. The SNPs were retained if they had F statistics greater than 10. SNP candidates were then extracted from LBD GWAS data excluding those with P < 5 × 10− 6. Proxy SNPs were determined by utilizing the “TwoSampleMR” package at the LD threshold r2 > 0.80. Third, SNPs absent in the outcome or lacking proper proxy SNPs were excluded from further analysis. The fourth step involved a harmonization process to exclude the SNPs that are palindromic or have inconsistent alleles between the outcome and exposure GWAS data. Finally, outlier SNPs were eliminated using the MR pleiotropy residual sum and outlier (MR-PRESSO) method [12]. Detailed information about the SNPs utilized as genetic instruments is provided in Supplementary Tables 2–5.
MR analyses
“MendelianRandomization” (v.0.6.0) and “TwoSampleMR” (v.0.5.6) packages were used in R (v.4.2.2) for statistical analyses. Four MR methods were employed for UVMR analyses: weighted median, MR Egger, inverse-variance weighting (IVW), and weighted mode. IVW served as the primary analyses [13]. The other three MR analytical methods were conducted to complement the IVW estimates. Considering the clinical associations among the three exposures, MVMR analyses were conducted to evaluate their independent effects on LBD. IVW and MR Egger methods were used. Similarly, IVW served as the primary method. P < 0.05 was considered significant. Statistical power was calculated using an online tool [14] (https://shiny.cnsgenomics.com/mRnd/).
Quality control of MR estimation
Various methods were employed to assess possible violation of the MR assumptions. Heterogeneity was identified through the Cochran Q-test [15] and funnel plot. A symmetric funnel plot is indicative of a low risk of heterogeneity. MR‒Egger intercepts [16] were utilized for directional pleiotropy detection. Leave-one-out analyses were carried out to explore the influences of any individual SNP on the overall MR estimate. In addition, MR Steiger directionality test [17] was used to explore reverse causation.
This study also explored the genetic instruments associated with several common risk factors for LBD, such as smoking [18], cancer, stroke, and coffee consumption [19]. To achieve this, the PhenoScanner database was employed, which provides comprehensive information on human genotype-phenotype associations. Following this, additional MR analyses were performed after removing these SNPs to ensure robust results.
Results
Genetic instruments
After rigorous filtration steps, a total of 38, 65, and 36 SNPs were used in the UVMR analysis to genetically predict LDL-C, HDL-C, and TG, respectively. Notably, SNP rs28456 has associations with both HDL-C and LDL-C. Five SNPs (rs144503444, rs145947882, rs116843064, rs11231693, and rs147233090) have associations with both TG and HDL-C. Moreover, SNP rs112875651 has associations with both TG and LDL-C (Fig. 1). No F statistics were below 10. After clumping and harmonizing candidate SNPs of three exposure factors together, a total of 92 SNPs were utilized in the MVMR analyses (Supplementary Table 5). Proxy SNPs used in this study were shown in Table 1. No outlier SNPs were detected.
UVMR estimates
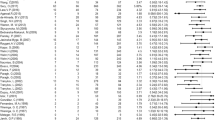
A causal relationship between LBD and LDL-C was identified with strong evidence. IVW analysis revealed that the increased LDL-C level could significantly elevate LBD risk (OR = 1.343; 95% CI, 1.094–1.649; P = 0.005). Causal estimates of UVMR were broadly consistent in magnitude and direction across various MR models (Figs. 2 and 3A). The MR Steiger directionality test did not indicate any evidence of reverse causality (Supplementary Table 6). Therefore, the causal direction from LDL-C to LBD is reliable. Conversely, the causal effects of TG (OR = 1.149; 95% CI, 0.887–1.489; P = 0.293) and HDL-C (OR = 0.864; 95% CI, 0.718–1.041; P = 0.124) on LBD were not statistically significant across all MR models (Figs. 2 and 3B-C). Statistical power was presented in Supplementary Table 7. MR analyses in this study exhibited neither heterogeneity nor pleiotropy (Table 2). Additionally, the funnel plot was basically symmetrical for all analyses (Fig. 3D-F). Furthermore, leave-one-out analyses reaffirmed the reliability of the causal effects (Supplementary Fig. 1).
MVMR estimates
In MVMR analyses, the detrimental effects of LDL-C on LBD remained significant after adjustment for TG and HDL-C, with consistent estimates across IVW (OR = 1.237; 95% CI, 1.015–1.508; P = 0.035) and MR Egger (OR = 1.236; 95% CI, 1.012–1.510; P = 0.038) (Fig. 4). Causal effects of TG and HDL-C on LBD were not observed in MVMR analyses (Fig. 4). No heterogeneity was detected (P = 0.637). The MR‒Egger intercept (intercept < 0.001; SE = 0.007; P = 0.993) suggest no directional pleiotropy exists in MVMR analyses.
Confounding analyses
Although no heterogeneity or pleiotropy was detected, the secondary traits (cancer, stroke, coffee consumption, and smoking) of SNPs utilized in this MR analyses were further manually checked. The HDL-C-associated SNPs had no associations with any confounders. For LDL-C, rs635634 was associated with invasive ovarian cancer and ischaemic stroke; rs140244541 was associated with smoking. For TG, rs1260326 was associated with coffee consumption. After removing these SNPs, the causality between the three exposure factors (LDL-C, HDL-C, and TG) and LBD remained unchanged (Supplementary Table 8).
Discussion
The aetiology and risk factors for LBD remain unclear, hindering the development of prevention strategies. Serum lipids are commonly used as indicators in health screenings, and accumulating evidence has revealed their associations with the potential risk of dementia, particularly AD [20,21,22]. However, limited evidence exists regarding the causal roles of serum lipids in LBD. To further examine whether serum lipids influence the LBD risk, MR design was applied in this study to assess their causal effects, and the results demonstrated a causal relationship between higher serum LDL-C levels and an increased risk of LBD, while HDL-C or TG did not impact the risk of LBD.
LBD, AD, and PD are prevalent neurodegenerative diseases. They exhibit overlapping symptom profiles, similar pathological manifestations of the deposition of α-synuclein, and even share potential genomic risk loci [23, 24]. However, the risk factors for these diseases are not consistently aligned. Smoking can significantly increase the risk of AD through smoking-related cerebral oxidative mechanisms [25]. Conversely, research suggests that smoking may have protective effects on PD [26] and is associated with a reduced risk of Lewy-related pathology [18]. Education exhibits opposing effects on the risk of AD and PD [27, 28], but shows no correlation with the risk of LBD [19]. Regarding serum lipids, some multicentre cohort studies with large sample sizes have reported that increased LDL-C attenuates the risk of PD, while HDL-C and TG show no association with PD risk [5, 29]. In contrast, multiple meta-analyses have revealed that high LDL-C levels increase the AD risk [4, 30]. These results highlight the diverse roles of LDL-C in neurodegenerative diseases. However, research on the roles of LDL-C in LBD is limited. A single-centre observational study reported the association of elevated serum LDL-C and reduced HDL-C with an increased LBD risk [6], which aligns with the MR analysis results of LDL-C in this study but not those of HDL-C. The relationship between HDL-C and LBD was not statistically significant in this study, although the OR values of HDL-C were less than 1 and demonstrated consistent estimations across various MR methods. The MR methods in this study, in comparison with conventional observational designs, could effectively minimize bias and enhance the credibility of the findings.
The underlying mechanisms of the causality between serum LDL-C and LBD are complex. In the periphery, serum cholesterol typically binds to circulating lipoproteins, facilitating its solubility and transportation to various tissues. Low-density lipoprotein (LDL) carries the majority of cholesterol. A vital role for cholesterol is to maintain neuronal structure and function. Under normal circumstances, blood-brain barrier (BBB) restricts the passage of serum cholesterol [31]. However, elevated serum cholesterol increases BBB permeability, allowing peripheral cholesterol, particularly LDL-C, to enter the brain and disrupt cholesterol metabolism [32]. Moreover, LDL binds to the LDL receptor on the BBB and is transported into the central nervous system via transcellular processes, suggesting a potential mechanism for the transportation of LDL from the periphery to the brain [33].
Evidence indicates that dysfunction in central cholesterol metabolism is closely linked to neurodegenerative pathologies [34]. Brain cholesterol plays a role in facilitating interactions between α-synuclein oligomers [35] and initiates their clustering [36]. Cholesterol-rich regions can serve as sites for the aggregation of α-synuclein [37]. Despite numerous studies investigating the possible involvement of cholesterols in the pathological process of dementia, the exact mechanisms underlying the causality between serum LDL-C and LBD remain unclear and demand further investigation.
Strengths and limitations
The current study has several noteworthy strengths. First, it is the first comprehensive MR study examining the causal relationships between serum lipids and LBD, providing a valuable reference for subsequent research in this area. Second, in the absence of RCTs, this MR analysis serves as a significant alternative study method, capitalizing on the inherent advantages of the MR design. Third, rigorous quality control measures were employed, and no evidence of heterogeneity, pleiotropy, or violation of MR assumptions was found, ensuring the reliability of the study.
Certain limitations are noted in this study. First, the GWAS data utilized are derived from participants of European ancestry, limiting the direct generalization of findings in this study to other populations. Second, while a causal relationship between LBD and LDL-C is indicated, the underlying molecular mechanisms remain incompletely understood. Third, due to the absence of detailed information on variables such as sex, age, LBD subtypes, and other clinical features in the summary-level data, subgroup analysis to stratify the population into different subgroups was not feasible.
Conclusions
This MR study offers compelling evidence that elevated serum LDL-C increases the risk of LBD. However, HDL-C and TG exhibit no significant causal effects on LBD. The findings of this study underscore the need to pay more attention to individuals with high serum LDL-C during the process of LBD screening and prevention, and contribute to the identification of feasible clinical management strategies for LBD patients.
Data availability
The datasets generated or analysed during the current study are available in OpenGWAS database (https://gwas.mrcieu.ac.uk/).
Abbreviations
- AD:
-
Alzheimer’s disease
- CI:
-
confidence interval
- HDL-C:
-
high-density lipoprotein cholesterol
- IVW:
-
Inverse-variance weighting
- LBD:
-
Lewy body dementia
- LDL-C:
-
low-density lipoprotein cholesterol
- MR:
-
Mendelian randomization
- OR:
-
odds ratio
- PD:
-
Parkinson’s disease
- TG:
-
triglycerides
References
Lopez OL, Kuller LH. Epidemiology of aging and associated cognitive disorders: prevalence and incidence of Alzheimer’s disease and other dementias. Handb Clin Neurol. 2019;167:139–48. https://doi.org/10.1016/b978-0-12-804766-8.00009-1.
Armstrong MJ. Lewy Body Dementias. Continuum (Minneap Minn). 2019;25(1):128–46. https://doi.org/10.1212/con.0000000000000685.
Chen Y, Wilson L, Kornak J, Dudley RA, Merrilees J, Bonasera SJ, et al. The costs of dementia subtypes to California Medicare fee-for-service, 2015. Alzheimers Dement. 2019;15(7):899–906. https://doi.org/10.1016/j.jalz.2019.03.015.
Sáiz-Vazquez O, Puente-Martínez A, Ubillos-Landa S, Pacheco-Bonrostro J, Santabárbara J. Cholesterol and Alzheimer’s Disease Risk: A Meta-Meta-Analysis. Brain Sci. 2020;10(6). https://doi.org/10.3390/brainsci10060386.
Hurh K, Park M, Jang SI, Park EC, Jang SY. Association between serum lipid levels over time and risk of Parkinson’s disease. Sci Rep. 2022;12(1):21020. https://doi.org/10.1038/s41598-022-25180-8.
Dou Y, Liu S, Li Y, Wu H, Chen H, Ji Y. Plasma cholesterol levels as potential nutritional biomarkers for Lewy Body Dementia. J Alzheimers Dis. 2022;86(2):779–86. https://doi.org/10.3233/jad-215295.
Boyko EJ. Observational research–opportunities and limitations. J Diabetes Complications. 2013;27(6):642–8. https://doi.org/10.1016/j.jdiacomp.2013.07.007.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–65. https://doi.org/10.1002/gepi.21758.
Richmond RC, Davey Smith G. Mendelian randomization: concepts and scope. Cold Spring Harb Perspect Med. 2022;12(1). https://doi.org/10.1101/cshperspect.a040501.
Boef AG, Dekkers OM, le Cessie S. Mendelian randomization studies: a review of the approaches used and the quality of reporting. Int J Epidemiol. 2015;44(2):496–511. https://doi.org/10.1093/ije/dyv071.
Chia R, Sabir MS, Bandres-Ciga S, Saez-Atienzar S, Reynolds RH, Gustavsson E, et al. Genome sequencing analysis identifies new loci associated with Lewy body dementia and provides insights into its genetic architecture. Nat Genet. 2021;53(3):294–303. https://doi.org/10.1038/s41588-021-00785-3.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–8. https://doi.org/10.1038/s41588-018-0099-7.
Pierce BL, Burgess S. Efficient design for mendelian randomization studies: subsample and 2-sample instrumental variable estimators. Am J Epidemiol. 2013;178(7):1177–84. https://doi.org/10.1093/aje/kwt084.
Brion MJ, Shakhbazov K, Visscher PM. Calculating statistical power in mendelian randomization studies. Int J Epidemiol. 2013;42(5):1497–501. https://doi.org/10.1093/ije/dyt179.
Greco MF, Minelli C, Sheehan NA, Thompson JR. Detecting pleiotropy in mendelian randomisation studies with summary data and a continuous outcome. Stat Med. 2015;34(21):2926–40. https://doi.org/10.1002/sim.6522.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–25. https://doi.org/10.1093/ije/dyv080.
Hemani G, Tilling K, Davey Smith G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 2017;13(11):e1007081. https://doi.org/10.1371/journal.pgen.1007081.
Tsuang D, Larson EB, Li G, Shofer JB, Montine KS, Thompson ML, et al. Association between lifetime cigarette smoking and lewy body accumulation. Brain Pathol. 2010;20(2):412–8. https://doi.org/10.1111/j.1750-3639.2009.00296.x.
Boot BP, Orr CF, Ahlskog JE, Ferman TJ, Roberts R, Pankratz VS, et al. Risk factors for dementia with Lewy bodies: a case-control study. Neurology. 2013;81(9):833–40. https://doi.org/10.1212/WNL.0b013e3182a2cbd1.
Dutta S, Rahman S, Ahmad R, Kumar T, Dutta G, Banerjee S, et al. An evidence-based review of neuronal cholesterol role in dementia and statins as a pharmacotherapy in reducing risk of dementia. Expert Rev Neurother. 2021;21(12):1455–72. https://doi.org/10.1080/14737175.2021.2003705.
Kjeldsen EW, Thomassen JQ, Juul Rasmussen I, Nordestgaard BG, Tybjærg-Hansen A, Frikke-Schmidt R. Plasma high-density lipoprotein cholesterol and risk of dementia: observational and genetic studies. Cardiovasc Res. 2022;118(5):1330–43. https://doi.org/10.1093/cvr/cvab164.
Anstey KJ, Ashby-Mitchell K, Peters R. Updating the evidence on the Association between Serum Cholesterol and risk of late-life dementia: review and Meta-analysis. J Alzheimers Dis. 2017;56(1):215–28. https://doi.org/10.3233/jad-160826.
Coughlin DG, Hurtig HI, Irwin DJ. Pathological influences on clinical heterogeneity in Lewy Body Diseases. Mov Disord. 2020;35(1):5–19. https://doi.org/10.1002/mds.27867.
Guo P, Gong W, Li Y, Liu L, Yan R, Wang Y, et al. Pinpointing novel risk loci for Lewy body dementia and the shared genetic etiology with Alzheimer’s disease and Parkinson’s disease: a large-scale multi-trait association analysis. BMC Med. 2022;20(1):214. https://doi.org/10.1186/s12916-022-02404-2.
Durazzo TC, Mattsson N, Weiner MW. Smoking and increased Alzheimer’s disease risk: a review of potential mechanisms. Alzheimers Dement. 2014;10(3 Suppl):122–45. https://doi.org/10.1016/j.jalz.2014.04.009.
Gallo V, Vineis P, Cancellieri M, Chiodini P, Barker RA, Brayne C, et al. Exploring causality of the association between smoking and Parkinson’s disease. Int J Epidemiol. 2019;48(3):912–25. https://doi.org/10.1093/ije/dyy230.
Frigerio R, Elbaz A, Sanft KR, Peterson BJ, Bower JH, Ahlskog JE, et al. Education and occupations preceding Parkinson disease: a population-based case-control study. Neurology. 2005;65(10):1575–83. https://doi.org/10.1212/01.wnl.0000184520.21744.a2.
Ngandu T, von Strauss E, Helkala EL, Winblad B, Nissinen A, Tuomilehto J, et al. Education and dementia: what lies behind the association? Neurology. 2007;69(14):1442–50. https://doi.org/10.1212/01.wnl.0000277456.29440.16.
Rozani V, Gurevich T, Giladi N, El-Ad B, Tsamir J, Hemo B, et al. Higher serum cholesterol and decreased Parkinson’s disease risk: a statin-free cohort study. Mov Disord. 2018;33(8):1298–305. https://doi.org/10.1002/mds.27413.
Zhou Z, Liang Y, Zhang X, Xu J, Lin J, Zhang R, et al. Low-Density Lipoprotein Cholesterol and Alzheimer’s Disease: a systematic review and Meta-analysis. Front Aging Neurosci. 2020;12:5. https://doi.org/10.3389/fnagi.2020.00005.
Pfrieger FW. Cholesterol homeostasis and function in neurons of the central nervous system. Cell Mol Life Sci. 2003;60(6):1158–71. https://doi.org/10.1007/s00018-003-3018-7.
Xue-Shan Z, Juan P, Qi W, Zhong R, Li-Hong P, Zhi-Han T, et al. Imbalanced cholesterol metabolism in Alzheimer’s disease. Clin Chim Acta. 2016;456:107–14. https://doi.org/10.1016/j.cca.2016.02.024.
Dehouck B, Fenart L, Dehouck MP, Pierce A, Torpier G, Cecchelli R. A new function for the LDL receptor: transcytosis of LDL across the blood-brain barrier. J Cell Biol. 1997;138(4):877–89. https://doi.org/10.1083/jcb.138.4.877.
Li D, Zhang J, Liu Q. Brain cell type-specific cholesterol metabolism and implications for learning and memory. Trends Neurosci. 2022;45(5):401–14. https://doi.org/10.1016/j.tins.2022.01.002.
García-Sanz P, Moratalla JMFGA. The role of cholesterol in α-Synuclein and Lewy Body Pathology in GBA1 Parkinson’s Disease. Mov Disord. 2021;36(5):1070–85. https://doi.org/10.1002/mds.28396.
Jakubec M, Bariås E, Furse S, Govasli ML, George V, Turcu D, et al. Cholesterol-containing lipid nanodiscs promote an α-synuclein binding mode that accelerates oligomerization. Febs j. 2021;288(6):1887–905. https://doi.org/10.1111/febs.15551.
Mahapatra A, Mandal N, Chattopadhyay K. Cholesterol in synaptic vesicle membranes regulates the Vesicle-Binding, function, and aggregation of α-Synuclein. J Phys Chem B. 2021;125(40):11099–111. https://doi.org/10.1021/acs.jpcb.1c03533.
Acknowledgements
We acknowledge the investigators and participants of the MRC-IEU Consortium and the Within family GWAS consortium. We are grateful to Ruth Chia et al. for the LBD GWAS summary data.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81801121) and the Key Research and Development Programs of Shaanxi Province, China (2016KTCL03-08).
Author information
Authors and Affiliations
Contributions
Conceptualization: P.L., X.Y., and X.X. Data Curation: J.L. and L.Z. Methodology: P.L., Y.Z., and X.X. Supervision: X.Y. and J.Q. Validation: Y.Z. and J.Q. Visualization: P.L. and J.L. Writing – Original Draft Preparation: P.L. and J.L. Writing – Review & Editing: L.Z. and X.Y.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Supplementary Fig. 1
Leave-one-out analyses of MR estimates of genetic risk of LDL-C (A), HDL-C (B), and TG (C) on LBD
Supplementary Material 2: Supplementary Table 1
Detailed information of GWAS datasets in the current study.
Supplementary Material 3: Supplementary Table 2
Eligible genetic instruments associated with LDL-C.
Supplementary Material 4: Supplementary Table 3
Eligible genetic instruments associated with HDL-C.
Supplementary Material 5: Supplementary Table 4
Eligible genetic instruments associated with TG.
Supplementary Material 6: Supplementary Table 5
Eligible genetic instruments used in MVMR.
Supplementary Material 7: Supplementary Table 6
Steiger direction test from LDL-C to LBD.
Supplementary Material 8: Supplementary Table 7
Statistical power calculation for MR analyses.
Supplementary Material 9: Supplementary Table 8
IVW MR analyses after removing SNPs with secondary traits.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, P., Liu, J., Zhang, Y. et al. Elevated serum LDL-C increases the risk of Lewy body dementia: a two-sample mendelian randomization study. Lipids Health Dis 23, 42 (2024). https://doi.org/10.1186/s12944-024-02032-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02032-0